Sex-Related Differences in Immunotherapy Outcomes of Patients with Advanced Non-Small Cell Lung Cancer
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Data Sources
2.2. Study Population
2.3. Outcomes
2.4. Data Analysis and Statistical Methods
3. Results
3.1. Study Population
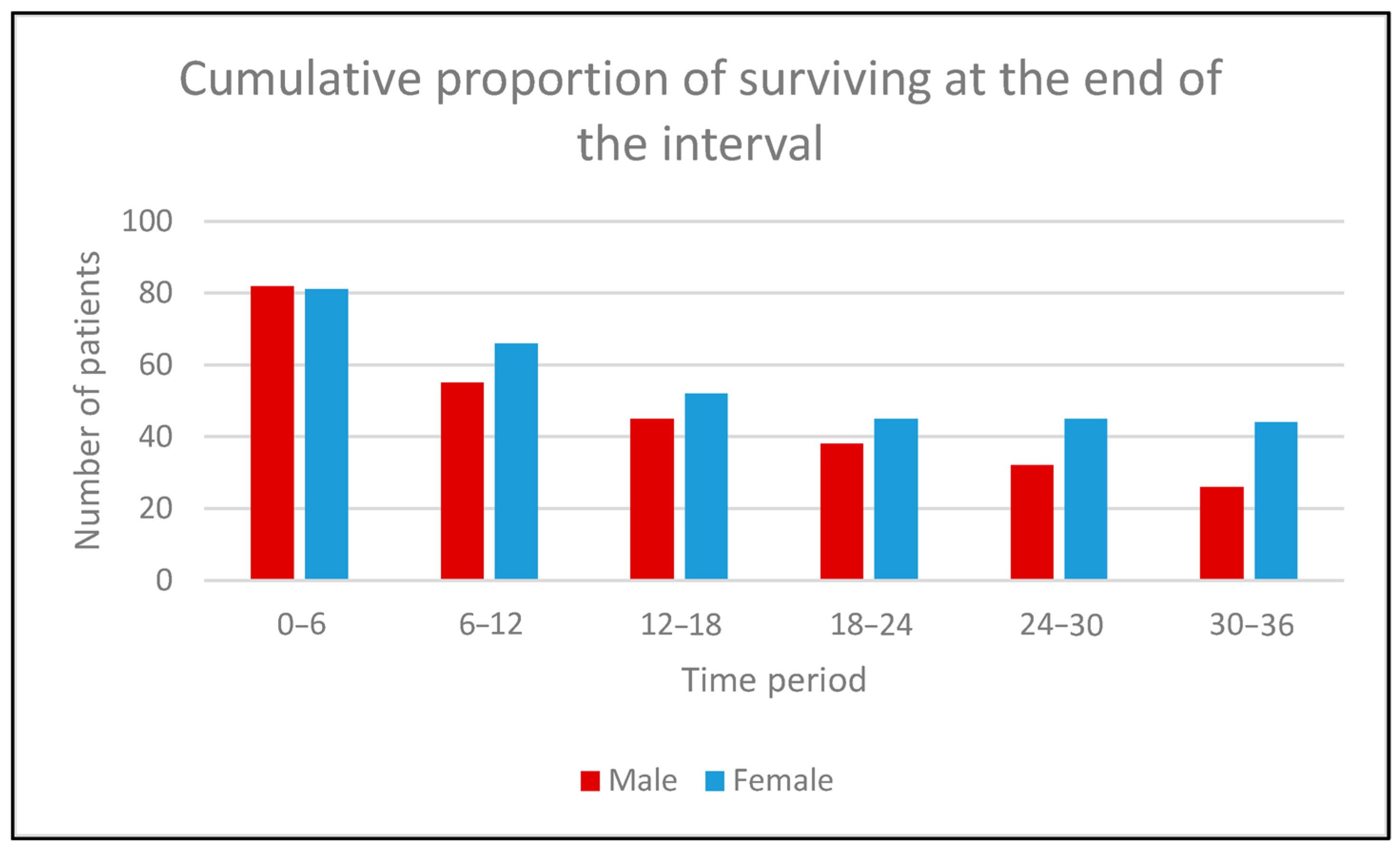
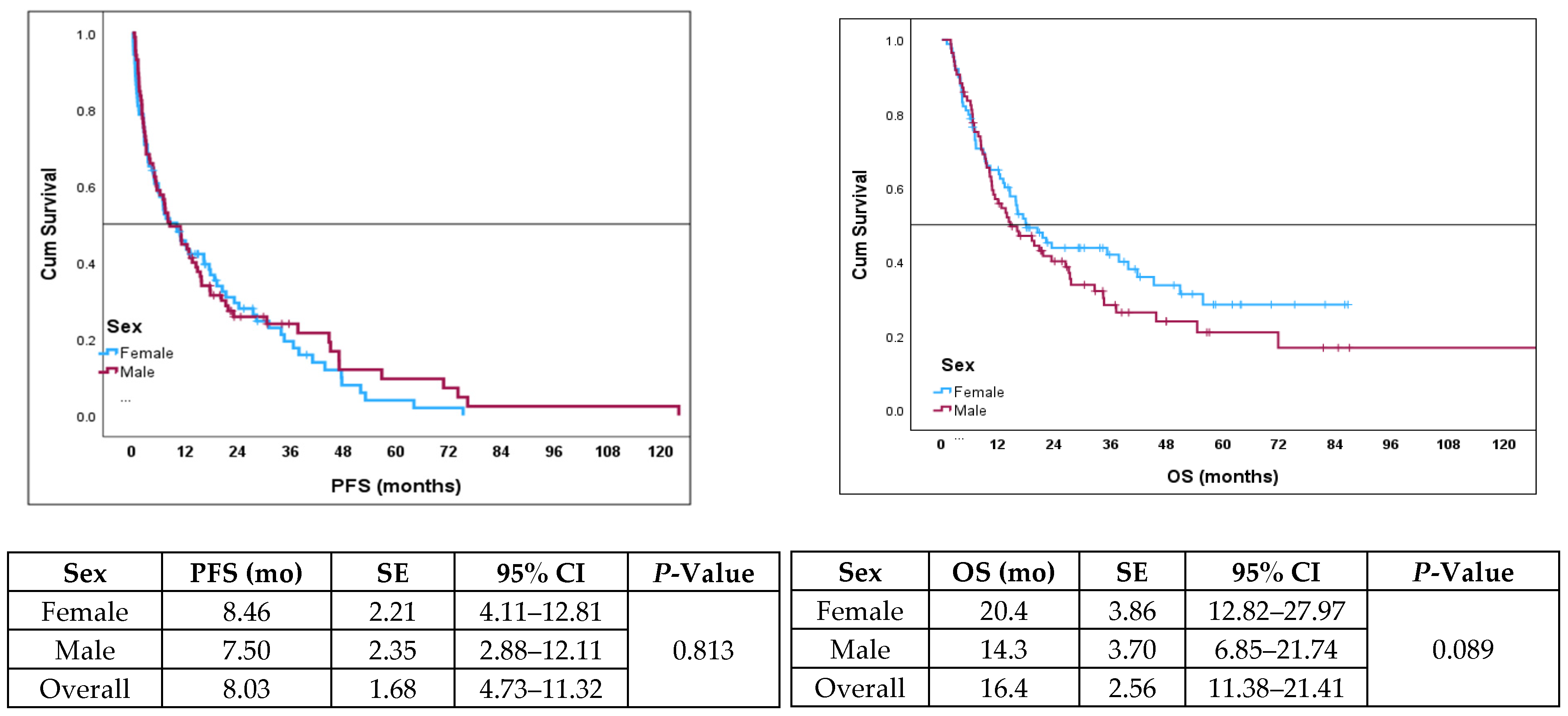
3.2. Efficacy Outcomes Based on Gender
3.3. Prognostic Factors for PFS and OS
3.4. Treatment Details and AE Data
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ma, J.; Yao, Y.; Tian, Y.; Chen, K.; Liu, B. Advances in sex disparities for cancer immunotherapy: Unveiling the dilemma of Yin and Yang. Biol. Sex. Differ. 2022, 13, 58. [Google Scholar] [CrossRef] [PubMed]
- Jaillon, S.; Berthenet, K.; Garlanda, C. Sexual Dimorphism in Innate Immunity. Clin. Rev. Allergy Immunol. 2019, 56, 308–321. [Google Scholar] [CrossRef] [PubMed]
- Klein, S.L.; Flanagan, K.L. Sex differences in immune responses. Nat. Rev. Immunol. 2016, 16, 626–638. [Google Scholar] [CrossRef] [PubMed]
- Haupt, S.; Caramia, F.; Klein, S.L.; Rubin, J.B.; Haupt, Y. Sex disparities matter in cancer development and therapy. Nat. Rev. Cancer 2021, 21, 393–407. [Google Scholar] [CrossRef]
- Meester, I.; Manilla-Munoz, E.; Leon-Cachon, R.B.R.; Paniagua-Frausto, G.A.; Carrion-Alvarez, D.; Ruiz-Rodriguez, C.O.; Rodriguez-Rangel, X.; Garcia-Martinez, J.M. SeXY chromosomes and the immune system: Reflections after a comparative study. Biol. Sex. Differ. 2020, 11, 3. [Google Scholar] [CrossRef]
- Ono, M. Control of regulatory T-cell differentiation and function by T-cell receptor signalling and Foxp3 transcription factor complexes. Immunology 2020, 160, 24–37. [Google Scholar] [CrossRef]
- Wallis, C.J.D.; Butaney, M.; Satkunasivam, R.; Freedland, S.J.; Patel, S.P.; Hamid, O.; Pal, S.K.; Klaassen, Z. Association of Patient Sex With Efficacy of Immune Checkpoint Inhibitors and Overall Survival in Advanced Cancers: A Systematic Review and Meta-analysis. JAMA Oncol. 2019, 5, 529–536. [Google Scholar] [CrossRef]
- Conforti, F.; Pala, L.; Bagnardi, V.; De Pas, T.; Martinetti, M.; Viale, G.; Gelber, R.D.; Goldhirsch, A. Cancer immunotherapy efficacy and patients’ sex: A systematic review and meta-analysis. Lancet Oncol. 2018, 19, 737–746. [Google Scholar] [CrossRef]
- Conforti, F.; Pala, L.; Bagnardi, V.; Viale, G.; De Pas, T.; Pagan, E.; Pennacchioli, E.; Cocorocchio, E.; Ferrucci, P.F.; De Marinis, F.; et al. Sex-Based Heterogeneity in Response to Lung Cancer Immunotherapy: A Systematic Review and Meta-Analysis. J. Natl. Cancer Inst. 2019, 111, 772–781. [Google Scholar] [CrossRef]
- Botticelli, A.; Onesti, C.E.; Zizzari, I.; Cerbelli, B.; Sciattella, P.; Occhipinti, M.; Roberto, M.; Di Pietro, F.; Bonifacino, A.; Ghidini, M.; et al. The sexist behaviour of immune checkpoint inhibitors in cancer therapy? Oncotarget 2017, 8, 99336–99346. [Google Scholar] [CrossRef]
- Takahashi, T.; Iwasaki, A. Sex differences in immune responses. Science 2021, 371, 347–348. [Google Scholar] [CrossRef]
- Chen, C.; Zhang, C.; Jin, Z.; Wu, B.; Xu, T. Sex differences in immune-related adverse events with immune checkpoint inhibitors: Data mining of the FDA adverse event reporting system. Int. J. Clin. Pharm. 2022, 44, 689–697. [Google Scholar] [CrossRef] [PubMed]
- Whitacre, C.C.; Reingold, S.C.; O’Looney, P.A. A gender gap in autoimmunity. Science 1999, 283, 1277–1278. [Google Scholar] [CrossRef]
- Conforti, F.; Pala, L.; Goldhirsch, A. Different effectiveness of anticancer immunotherapy in men and women relies on sex-dimorphism of the immune system. Oncotarget 2018, 9, 31167–31168. [Google Scholar] [CrossRef] [PubMed]
- Ortona, E.; Pierdominici, M.; Rider, V. Editorial: Sex Hormones and Gender Differences in Immune Responses. Front. Immunol. 2019, 10, 1076. [Google Scholar] [CrossRef] [PubMed]
- Vavala, T.; Catino, A.; Pizzutilo, P.; Longo, V.; Galetta, D. Gender Differences and Immunotherapy Outcome in Advanced Lung Cancer. Int. J. Mol. Sci. 2021, 22, 11942. [Google Scholar] [CrossRef] [PubMed]
- Gandhi, L.; Rodriguez-Abreu, D.; Gadgeel, S.; Esteban, E.; Felip, E.; De Angelis, F.; Domine, M.; Clingan, P.; Hochmair, M.J.; Powell, S.F.; et al. Pembrolizumab plus Chemotherapy in Metastatic Non-Small-Cell Lung Cancer. N. Engl. J. Med. 2018, 378, 2078–2092. [Google Scholar] [CrossRef] [PubMed]
- Paz-Ares, L.; Luft, A.; Vicente, D.; Tafreshi, A.; Gumus, M.; Mazieres, J.; Hermes, B.; Cay Senler, F.; Csoszi, T.; Fulop, A.; et al. Pembrolizumab plus Chemotherapy for Squamous Non-Small-Cell Lung Cancer. N. Engl. J. Med. 2018, 379, 2040–2051. [Google Scholar] [CrossRef]
- McAllister, S.S.; Weinberg, R.A. The tumour-induced systemic environment as a critical regulator of cancer progression and metastasis. Nat. Cell Biol. 2014, 16, 717–727. [Google Scholar] [CrossRef]
- Suzuki, K.; Terakawa, T.; Furukawa, J.; Harada, K.; Hinata, N.; Nakano, Y.; Fujisawa, M. C-reactive protein and the neutrophil-to-lymphocyte ratio are prognostic biomarkers in metastatic renal cell carcinoma patients treated with nivolumab. Int. J. Clin. Oncol. 2020, 25, 135–144. [Google Scholar] [CrossRef]
- Oya, Y.; Yoshida, T.; Kuroda, H.; Mikubo, M.; Kondo, C.; Shimizu, J.; Horio, Y.; Sakao, Y.; Hida, T.; Yatabe, Y. Predictive clinical parameters for the response of nivolumab in pretreated advanced non-small-cell lung cancer. Oncotarget 2017, 8, 103117–103128. [Google Scholar] [CrossRef] [PubMed]
- Riedl, J.M.; Barth, D.A.; Brueckl, W.M.; Zeitler, G.; Foris, V.; Mollnar, S.; Stotz, M.; Rossmann, C.H.; Terbuch, A.; Balic, M.; et al. C-Reactive Protein (CRP) Levels in Immune Checkpoint Inhibitor Response and Progression in Advanced Non-Small Cell Lung Cancer: A Bi-Center Study. Cancers 2020, 12, 2319. [Google Scholar] [CrossRef] [PubMed]
- Miceli, R.; Eriksson, H.; Lo Russo, G.; Alfieri, S.; Moksnes Bjaanaes, M.; Pietrantonio, F.; De Cecco, L.; Prelaj, A.; Proto, C.; Franzen, J.; et al. Gender Difference in sidE eFfects of ImmuNotherapy: A possible clue to optimize cancEr tReatment (G-DEFINER): Study protocol of an observational prospective multicenter study. Acta Oncol. 2024, 63, 213–219. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Male N = 85 | Female N = 89 | p-Value | ||
|---|---|---|---|---|---|
| Age (mean; range) | 71 (42–87) | 68 (41–89) | 0.097 | ||
| Smoking history (n/%) | Former/current smoker | n = 153 | 79 (92.9) | 74 (83.0) | 0.039 |
| Non-smoker | n = 21 | 6 (7.1) | 15 (17.0) | ||
| PD-L1: (n/%) 1 | ≥50 | n = 101 | 50 (61.0) | 51 (58.6) | 0.755 |
| <50 | n = 42 | 32 (39.0) | 36 (41.4) | ||
| Histology | Adenocarcinoma | n = 112 | 48 (56.0) | 64 (71.9) | 0.028 |
| Large cell carcinoma | n = 17 | 9 (11.1) | 8 (9.0) | ||
| Squamous | n = 45 | 28 (32.9) | 17 (19.1) | ||
| Genetic testing 4 | EGFR | n = 0/162 | 0 | 0 | 0.489 |
| Non(V600E) | n = 7/162 | 3 (3.6) | 4 (4.8) | ||
| KRAS (nonG12C) | n = 44/162 | 21 (25.7) | 23 (27.0) | ||
| Negative | n = 111/162 | 58 (70.7) | 53 (62.4) | ||
| Treatment type | Mono-ICI 2 | n = 80 | 40 (52.9) | 40 (44.9) | 0.449 |
| ICI+CTX 3 | n = 94 | 45 (47.1) | 49 (55.1) | ||
| Liver metastases at the baseline | Present | n = 10 | 5 (5.6) | 5 (5.6) | 0.597 |
| Absent | n = 164 | 80 (94.1) | 84 (94.4) | ||
| History of autoimmune disease | Present | n = 14 | 4 (4.7) | 16 (18.0) | 0.005 |
| Absent | n = 160 | 81 (95.3) | 73 (82.0) | ||
| CRP mean (SD) | n = 174 | 34.5 (40.9) | 50.8 (61.9) | 0.046 | |
| Treatment Outcomes | Males | Females | p-Value |
|---|---|---|---|
| Ongoing (n = 17) | All censored | All censored | n/a 1 |
| Completed 2 years (n = 20) | Not reached | Not reached | n/a |
| Discontinued due to PD (n = 86) | 9.40 (7.3–11.4) | 13.1 (7.4–18.7) | 0.140 |
| Discontinued due to irAEs (n = 51) | 16.4 (2.3–30.4) | 17.86 (9.7–25.9) | 0.984 |
| Variables of Interest | OS (mo) | SE | 95% CI | p-Value | |
|---|---|---|---|---|---|
| Sex | Female Male | 20.40 14.30 | 3.86 3.79 | 12.8–27.9 6.8–74 | 0.089 |
| Smoking | Never Ever | 16.13 16.4 | 8.21 2.85 | 0.03–32.2 10.7–22.0 | 0.971 |
| CRP at the start of IO | ≤10 mg/L >10 mg/L | 35.26 14.50 | 7.59 1.55 | 20.3–50.1 11.4–17.5 | 0.013 |
| CRP 1 at the end of treatment | ≤10 mg/L >10 mg/L | NR 2 14.53 | 1.43 | 11.7–17.3 | <0.001 |
| Age | ≤65 >65 | 18.03 16.40 | 5.71 2.67 | 6.8–29.23 11.1–21.6 | 0.057 |
| Treatment | IO+CTX 3 IO 4 | 15.83 20.80 | 2.56 5.80 | 10.7–20.8 9.41–32.2 | 0.137 |
| PD-L1 | ≥50 <50 | 18.03 20.80 | 3.87 6.22 | 10.4–25.6 0.0–24.36 | 0.464 |
| Histology 3 | Non-squamous Squamous | 18.03 13.86 | 2.52 3.08 | 13.1–22.9 7.82–19.9 | 0.418 |
| Liver metastases | Present Absent | 9.23 18.03 | 4.53 2.77 | 0.35–18.1 12.6–23.4 | 0.034 |
| Pre-existing liver disease | Present Absent | 15.77 20.40 | 3.46 8.67 | 8.9–22.5 3.4–37.48 | 0.210 |
| Variables (Reference) | Exp(B) | 95% CI | p-Value | Variable (Reference) | Exp(B) | 95% CI | p-Value |
|---|---|---|---|---|---|---|---|
| COX Model for PFS | COX Model for OS | ||||||
| CRP at the TD (<10 g/L) | 1.638 | 1.10–2.43 | 0.014 | CRP at the TD (<10g/L) | 2.68 | 1.58–4.78 | <0.001 |
| Liver metastases (absent) | 2.48 | 1.25–4.94 | 0.009 | Age (<65) | 1.43 | 0.92–2.19 | 0.106 |
| PD-L1 | 0.704 | 0.62–1.00 | 0.073 | ||||
| Pre-existing liver disease | 0.655 | 0.38–1.09 | 0.113 | ||||
| Treatment Outcomes | Mean CRP (SD) | p-Value | |
|---|---|---|---|
| Male | Female | ||
| Completed 2 years (n = 20) | 18.1 (35.7) | 14.3 (14.0) | 0.746 |
| Discontinued d/t PD 1 (n = 86) | 99.3 (93.5) | 53.2 (52.9) | 0.009 |
| Discontinued d/t irAEs 2 (n = 51) | 73.2 (96.8) | 57.9 (73.2) | 0.540 |
| Reason To Stop | Males | Females | RR 1 | 96% CI | p-Value |
|---|---|---|---|---|---|
| Ongoing (n = 17) | 9 (10.6) | 8 (9.0) | 1.03 | 0.50–2.13 | 0.926 |
| Completed 2 years (n = 20) | 9 (10.6) | 11 (12.4) | 0.95 | 0.41–2.17 | 0.913 |
| Discontinued d/t PD (n = 86) | 49 (57.6) | 37 (41.5) | 0.86 | 061–1.20 | 0.036 |
| Discontinued d/t irAEs (n = 51) | 18(21.2) | 33 (37.1) | 1.75 | 1.00–2.82 | 0.028 |
| Total | 85 (100) | 89 (100) |
| Incidence of irAEs in Males and Females | Male N = 85 | Female N = 89 |
|---|---|---|
| ir-pneumonitis | 8 (9.5) | 3 (3.4) |
| ir-colitis | 3 (3.6) | 11 (12.4) |
| ir-hepatitis | 2 (2.3) | 7 (7.9) |
| ir-thyroiditis | 2 (2.3) | 8 (8.9) |
| ir-miocarditis | 2 (2.3) | 1 (1.1) |
| other | 1 (1.2) | 3 (3.4) |
| No irAEs | 67 (78.9) | 56 (62.9) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cohen, S.F.; Cruiziat, D.; Naimer, J.; Cohen, V.; Kasymjanova, G.; Spatz, A.; Agulnik, J. Sex-Related Differences in Immunotherapy Outcomes of Patients with Advanced Non-Small Cell Lung Cancer. Curr. Oncol. 2024, 31, 7379-7389. https://doi.org/10.3390/curroncol31110544
Cohen SF, Cruiziat D, Naimer J, Cohen V, Kasymjanova G, Spatz A, Agulnik J. Sex-Related Differences in Immunotherapy Outcomes of Patients with Advanced Non-Small Cell Lung Cancer. Current Oncology. 2024; 31(11):7379-7389. https://doi.org/10.3390/curroncol31110544
Chicago/Turabian StyleCohen, Sara Frida, Diane Cruiziat, Jeremy Naimer, Victor Cohen, Goulnar Kasymjanova, Alan Spatz, and Jason Agulnik. 2024. "Sex-Related Differences in Immunotherapy Outcomes of Patients with Advanced Non-Small Cell Lung Cancer" Current Oncology 31, no. 11: 7379-7389. https://doi.org/10.3390/curroncol31110544
APA StyleCohen, S. F., Cruiziat, D., Naimer, J., Cohen, V., Kasymjanova, G., Spatz, A., & Agulnik, J. (2024). Sex-Related Differences in Immunotherapy Outcomes of Patients with Advanced Non-Small Cell Lung Cancer. Current Oncology, 31(11), 7379-7389. https://doi.org/10.3390/curroncol31110544








