Prognostic Factors for Patients with Small-Cell Lung Cancer Treated with Chemoimmunotherapy: A Retrospective Multicenter Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethical Approval
2.2. Patients and Data Collection
2.3. Statistical Analysis
3. Results
3.1. Patient Characteristics and Efficacy
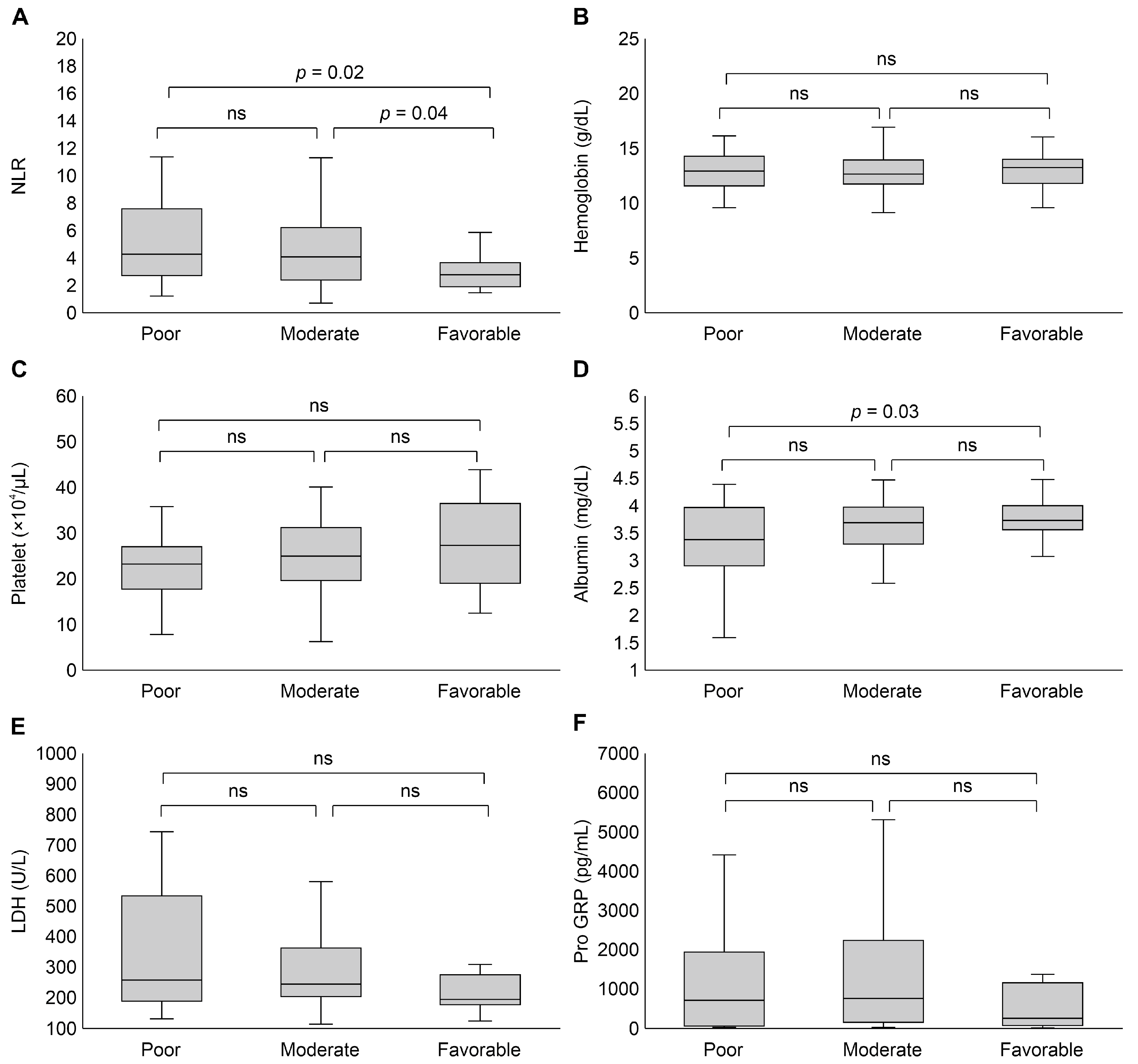
3.2. Laboratory Data at Baseline
3.3. Univariate and Multivariate Analyses
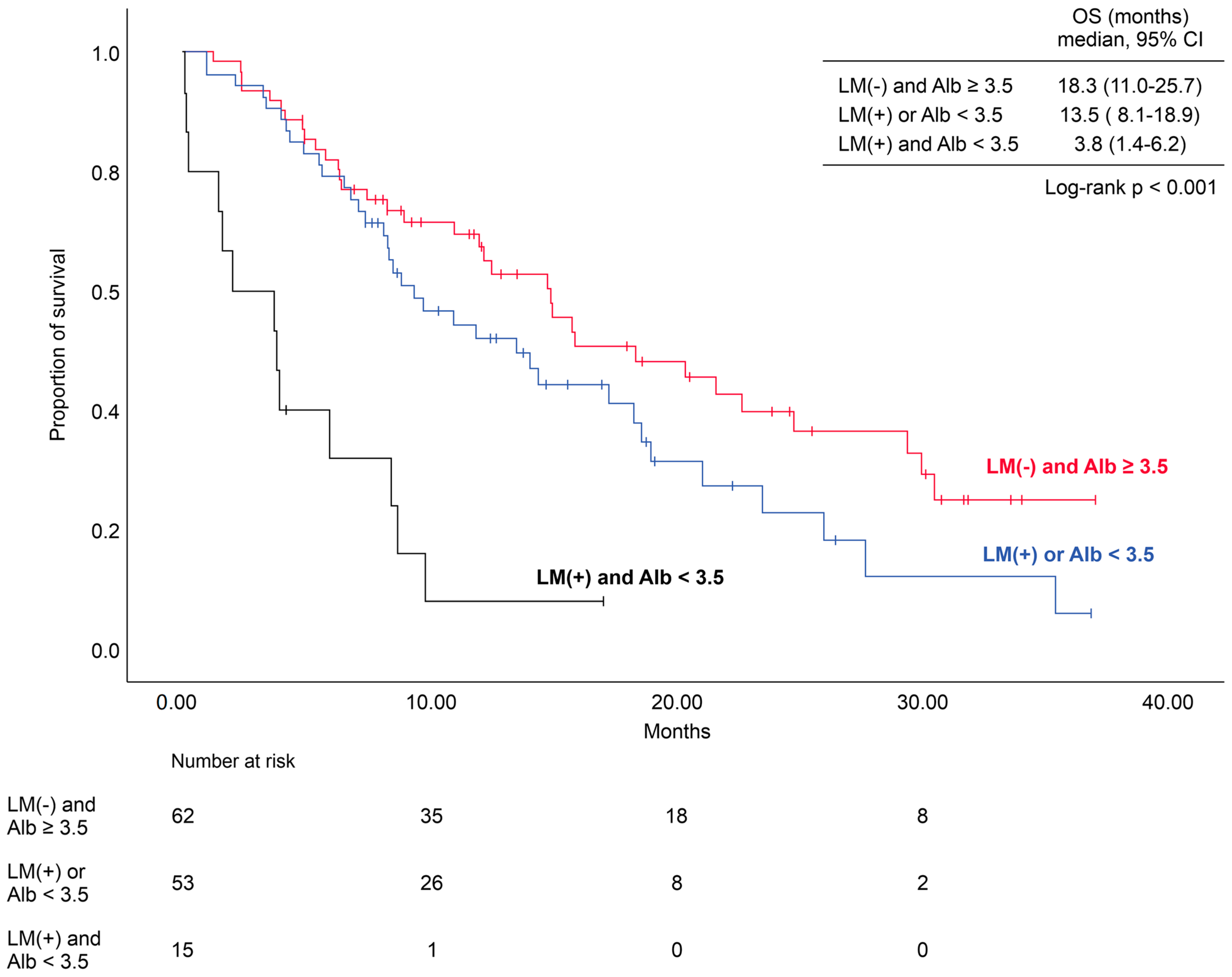
3.4. Number of Prognostic Factors and the Impact on Survival
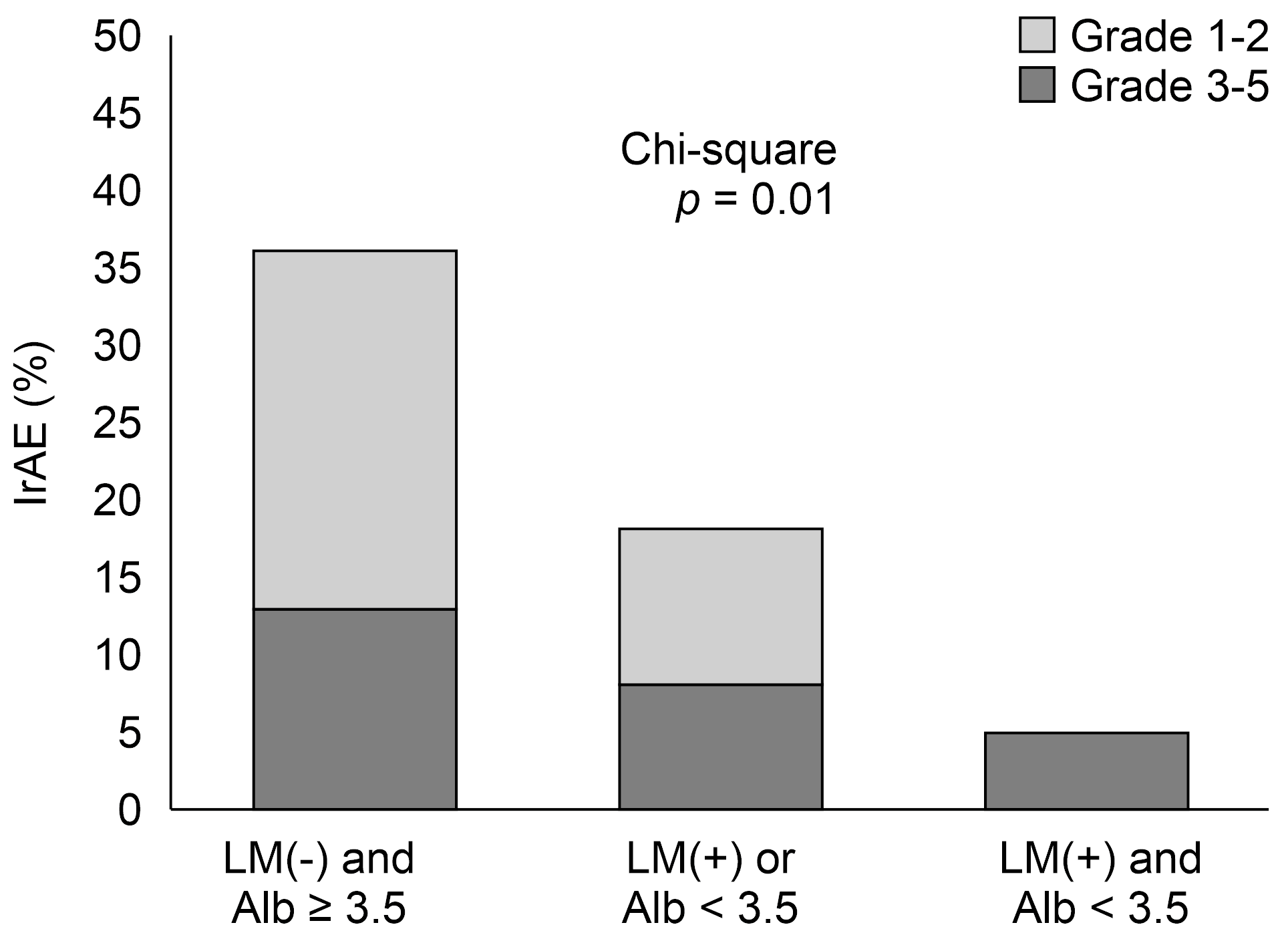
3.5. Number of Prognostic Factors and the Impact on Immune-Related Adverse Event (irAE) Incidence
3.6. Subsequent Chemotherapy
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rudin, C.M.; Brambilla, E.; Faivre-Finn, C.; Sage, J. Small-cell lung cancer. Nat. Rev. Dis. Primers 2021, 7, 3. [Google Scholar] [CrossRef] [PubMed]
- Farago, A.F.; Keane, F.K. Current standards for clinical management of small cell lung cancer. Transl. Lung Cancer Res. 2018, 7, 69–79. [Google Scholar] [CrossRef] [PubMed]
- O’sullivan, D.E.; Cheung, W.Y.; Syed, I.A.; Moldaver, D.; Shanahan, M.K.; Bebb, D.G.; Sit, C.; Brenner, D.R.; Boyne, D.J. Real-World Treatment Patterns, Clinical Outcomes, and Health Care Resource Utilization in Extensive-Stage Small Cell Lung Cancer in Canada. Curr. Oncol. 2021, 28, 3091–3103. [Google Scholar] [CrossRef] [PubMed]
- Horn, L.; Mansfield, A.S.; Szczesna, A.; Havel, L.; Krzakowski, M.; Hochmair, M.J.; Huemer, F.; Losonczy, G.; Johnson, M.L.; Nishio, M.; et al. First-Line Atezolizumab plus Chem-otherapy in Extensive-Stage Small-Cell Lung Cancer. N. Engl. J. Med. 2018, 379, 2220–2229. [Google Scholar] [CrossRef] [PubMed]
- Paz-Ares, L.; Dvorkin, M.; Chen, Y.; Reinmuth, N.; Hotta, K.; Trukhin, D.; Statsenko, G.; Hochmair, M.J.; Özgüroğlu, M.; Ji, J.H.; et al. Durvalumab plus platinum-etoposide versus platinum-etoposide in first-line treatment of extensive-stage small-cell lung cancer (CASPIAN): A randomised, controlled, open-label, phase 3 trial. Lancet 2019, 39, 1929–1939. [Google Scholar] [CrossRef]
- Liu, S.V.; Reck, M.; Mansfield, A.S.; Mok, T.; Scherpereel, A.; Reinmuth, N.; Garassino, M.C.; De Castro Carpeno, J.; Califano, R.; Nishio, M.; et al. Updated Overall Survival and PD-L1 Subgroup Analysis of Patients with Extensive-Stage Small-Cell Lung Cancer Treated with Atezolizumab, Carboplatin, and Etoposide (IMpower133). J. Clin. Oncol. 2021, 39, 619–630. [Google Scholar] [CrossRef]
- Paz-Ares, L.; Chen, Y.; Reinmuth, N.; Hotta, K.; Trukhin, D.; Statsenko, G.; Hochmair, M.; Özgüroğlu, M.; Ji, J.; Garassino, M.; et al. Durvalumab, with or without tremelimumab, plus platinum-etoposide in first-line treatment of extensive-stage small-cell lung cancer: 3-year overall survival update from CASPIAN. ESMO Open 2022, 7, 100408. [Google Scholar] [CrossRef]
- Yi, M.; Jiao, D.; Xu, H.; Liu, Q.; Zhao, W.; Han, X.; Wu, K. Biomarkers for predicting efficacy of PD-1/PD-L1 inhibitors. Mol. Cancer 2018, 17, 129. [Google Scholar] [CrossRef]
- Mino-Kenudson, M.; Schalper, K.; Cooper, W.; Dacic, S.; Hirsch, F.R.; Jain, D.; Lopez-Rios, F.; Tsao, M.S.; Yatabe, Y.; Beasley, M.B.; et al. Predictive Biomarkers for Immunotherapy in Lung Cancer: Perspective from the International Association for the Study of Lung Cancer Pathology Committee. J. Thorac. Oncol. 2022, 17, 1335–1354. [Google Scholar] [CrossRef]
- Russano, M.; La Cava, G.; Cortellini, A.; Citarella, F.; Galletti, A.; Di Fazio, G.R.; Santo, V.; Brunetti, L.; Vendittelli, A.; Fioroni, I.; et al. Immunotherapy for Metastatic Non-Small Cell Lung Cancer: Therapeutic Advances and Biomarkers. Curr. Oncol. 2023, 30, 2366–2387. [Google Scholar] [CrossRef]
- Paz-Ares, L.; Garassino, M.C.; Chen, Y.; Reinmuth, N.; Hotta, K.; Poltoratskiy, A.; Trukhin, D.; Hochmair, M.J.; Özgüroğlu, M.; Ji, J.H.; et al. Durvalumab +/- tremelimumab + platinum-etoposide in extensive-stage small-cell lung cancer (CASPIAN): Outcomes by PD-L1 expression and tissue tumor mutational burden. Clin. Cancer Res. 2023, 30, 824–835. [Google Scholar] [CrossRef] [PubMed]
- El Sayed, R.; Blais, N. Immunotherapy in Extensive-Stage Small Cell Lung Cancer. Curr. Oncol. 2021, 28, 4093–4108. [Google Scholar] [CrossRef] [PubMed]
- Plaja, A.; Moran, T.; Carcereny, E.; Saigi, M.; Hernández, A.; Cucurull, M.; Domènech, M. Small-Cell Lung Cancer Long-Term Survivor Patients: How to Find a Needle in a Haystack? Int. J. Mol. Sci. 2021, 16, 13508. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.; Zhang, J.; Zhou, W.; Yuan, Z.; Wang, H. Prognostic factors in extensive-stage small cell lung cancer patients with or-gan-specific metastasis: Unveiling commonalities and disparities. J. Cancer Res. Clin. Oncol. 2024, 150, 74. [Google Scholar] [CrossRef]
- Imai, H.; Wasamoto, S.; Tsuda, T.; Nagai, Y.; Kishikawa, T.; Masubuchi, K.; Osaki, T.; Miura, Y.; Umeda, Y.; Ono, A.; et al. Using the neutrophil-to-lymphocyte ratio to predict the outcome of individuals with nonsquamous non-small cell lung cancer receiving pembrolizumab plus platinum and pemetrexed. Thorac. Cancer 2023, 14, 2567–2578. [Google Scholar] [CrossRef]
- Mirili, C.; Guney, I.B.; Paydas, S.; Seydaoglu, G.; Kapukaya, T.K.; Ogul, A.; Gokcay, S.; Buyuksimsek, M.; Yetisir, A.E.; Karaalioglu, B.; et al. Prognostic significance of neutrophil/lymphocyte ratio (NLR) and correlation with PET–CT metabolic parameters in small cell lung cancer (SCLC). Int. J. Clin. Oncol. 2018, 24, 168–178. [Google Scholar] [CrossRef]
- Tumeh, P.C.; Hellmann, M.D.; Hamid, O.; Tsai, K.K.; Loo, K.L.; Gubens, M.A.; Rosenblum, M.; Harview, C.L.; Taube, J.M.; Handley, N.; et al. Liver Metastasis and Treatment Outcome with Anti-PD-1 Monoclonal Antibody in Patients with Melanoma and NSCLC. Cancer Immunol. Res. 2017, 5, 417–424. [Google Scholar] [CrossRef]
- Takeuchi, E.; Kondo, K.; Okano, Y.; Kunishige, M.; Kondo, Y.; Kadota, N.; Machida, H.; Hatakeyama, N.; Naruse, K.; Ogino, H.; et al. Early mortality factors in immune checkpoint inhibitor monotherapy for advanced or metastatic non-small cell lung cancer. J. Cancer Res. Clin. Oncol. 2022, 149, 3139–3147. [Google Scholar] [CrossRef]
- Campos-Balea, B.; Carpeño, J.d.C.; Massutí, B.; Vicente-Baz, D.; Parente, D.P.; Ruiz-Gracia, P.; Crama, L.; Dols, M.C. Prognostic factors for survival in patients with metastatic lung adenocarcinoma: An analysis of the SEER database. Thorac. Cancer 2020, 11, 3357–3364. [Google Scholar] [CrossRef]
- Wang, Q.; Fang, Y.; Li, C.; Leong, T.L.; Provencio, M.; Oh, I.-J.; Zhang, Z.; Su, C. Differential organ-specific tumor response to first-line immune checkpoint inhibitor therapy in non-small cell lung cancer—A retrospective cohort study. Transl. Lung Cancer Res. 2023, 12, 312–321. [Google Scholar] [CrossRef]
- Ma, X.; Zhang, Z.; Chen, X.; Zhang, J.; Nie, J.; Da, L.; Hu, W.; Tian, G.; Wu, D.; Han, J.; et al. Prognostic factor analysis of patients with small cell lung cancer: Real-world data from 988 patients. Thorac. Cancer 2021, 12, 1841–1850. [Google Scholar] [CrossRef] [PubMed]
- Zhou, S.; Wang, H.; Jiang, W.; Yu, Q.; Zeng, A. Prognostic Value of Pretreatment Albumin-to-Alkaline Phosphatase Ratio in Extensive-Disease Small-Cell Lung Cancer: A Retrospective Cohort Study. Cancer Manag. Res. 2020, 12, 2015–2024. [Google Scholar] [CrossRef] [PubMed]
- Li, Q.; Li, L.; Wang, Y.; Xu, C.; Zou, J. The prognostic value of pretreatment albumin-to-fibrinogen ratio in small cell lung cancer patients receiving first-line platinum-based chemotherapy. Heliyon 2023, 9, e19225. [Google Scholar] [CrossRef] [PubMed]
- Nakanishi, Y.; Masuda, T.; Yamaguchi, K.; Sakamoto, S.; Horimasu, Y.; Mimae, T.; Nakashima, T.; Miyamoto, S.; Tsutani, Y.; Iwamoto, H.; et al. Albumin–globulin ratio is a predictive biomarker of antitumor effect of anti-PD-1 antibody in patients with non-small cell lung cancer. Int. J. Clin. Oncol. 2019, 25, 74–81. [Google Scholar] [CrossRef] [PubMed]
- Nasu, I.; Kondo, M.; Uozumi, R.; Takada, S.; Nawata, S.; Iihara, H.; Okumura, Y.; Takemoto, M.; Mino, K.; Sasaki, T.; et al. Prognostic Model of Baseline Medications plus Neutrophil-to-lymphocyte Ratio in Patients with Advanced Non-small-cell Lung Cancer Receiving Immune Checkpoint In-hibitor plus Platinum Doublet: A Multicenter Retrospective Study. J. Cancer 2023, 14, 676–688. [Google Scholar] [CrossRef]
- Bi, H.; Ren, D.; Xiao, Y.; Zhou, Y.; Yi, B.; Han, W.; Shao, Y.; Wang, J.; Zhang, C.; Wang, H. Prognostic implications of neutrophil-to-lymphocyte ratio in patients with extensive-stage small cell lung cancer receiving chemoimmunotherapy: A multicenter, real-world study. Thorac. Cancer 2024, 15, 559–569. [Google Scholar] [CrossRef]
- Haratani, K.; Hayashi, H.; Chiba, Y.; Kudo, K.; Yonesaka, K.; Kato, R.; Kaneda, H.; Hasegawa, Y.; Tanaka, K.; Takeda, M.; et al. Association of Immune-Related Adverse Events with Nivolumab Efficacy in Non–Small-Cell Lung Cancer. JAMA Oncol. 2018, 4, 374–378. [Google Scholar] [CrossRef]
- Cook, S.; Samuel, V.; Meyers, D.E.; Stukalin, I.; Litt, I.; Sangha, R.; Morris, D.G.; Heng, D.Y.C.; Pabani, A.; Dean, M.; et al. Immune-Related Adverse Events and Survival Among Patients with Metastatic NSCLC Treated with Immune Checkpoint Inhibitors. JAMA Netw. Open 2024, 7, e2352302. [Google Scholar] [CrossRef]
- Capella, M.P.; Pang, S.A.; Magalhaes, M.A.; Esfahani, K. A Review of Immunotherapy in Non-Small-Cell Lung Cancer. Curr. Oncol. 2024, 31, 3495–3512. [Google Scholar] [CrossRef]
- Yokoo, K.; Kitamura, Y.; Suzuki, K.; Morikawa, K.; Sawai, T.; Honda, H.; Kudo, S.; Yamada, G. Relationship between immune-related adverse events and treatment effectiveness in extensive disease small cell lung cancer. Thorac. Cancer 2023, 14, 2251–2258. [Google Scholar] [CrossRef]
- Nishimura, T.; Fujimoto, H.; Fujiwara, T.; Ito, K.; Fujiwara, A.; Yuda, H.; Itani, H.; Naito, M.; Kodama, S.; Furuhashi, K.; et al. Impact of immune-related adverse events on survival outcomes in extensive-stage small cell lung cancer patients treated with immune checkpoint inhibitors. Cancer Med. 2024, 13, e7188. [Google Scholar] [CrossRef] [PubMed]
| Total (n = 130) | Poor (n = 35) | Moderate (n = 77) | Favorable (n = 18) | p Value | |
|---|---|---|---|---|---|
| Age | 71 (42–85) | 73 (46–82) | 69 (42–84) | 70 (62–85) | 0.67 |
| Gender | |||||
| Male | 103 | 29 | 61 | 13 | |
| Female | 27 | 6 | 16 | 5 | 0.67 |
| Smoking status | |||||
| Never | 4 | 1 | 3 | 0 | |
| Former or current | 126 | 34 | 74 | 18 | 0.69 |
| Performance status | |||||
| 0 | 27 | 1 | 22 | 4 | |
| 1 | 71 | 19 | 41 | 11 | |
| 2 | 23 | 9 | 12 | 2 | |
| 3–4 | 9 | 6 | 2 | 1 | 0.02 |
| Clinical stage | |||||
| IIIB-IIIC | 10 | 3 | 6 | 1 | |
| IVA | 36 | 6 | 22 | 8 | |
| IVB | 80 | 26 | 47 | 7 | |
| Recurrent | 4 | 0 | 2 | 2 | 0.10 |
| Metastatic site | |||||
| Brain | 29 | 12 | 13 | 4 | 0.12 |
| Liver | 40 | 17 | 20 | 3 | 0.03 |
| Bone | 25 | 5 | 15 | 5 | 0.73 |
| Prior radiotherapy | |||||
| Yes | 27 | 6 | 16 | 5 | |
| No | 103 | 29 | 61 | 13 | 0.67 |
| Platinum doublet regimen | |||||
| Cisplatin and etoposide | 6 | 1 | 5 | 0 | |
| Carboplatin and etoposide | 124 | 34 | 72 | 18 | 0.56 |
| Immune checkpoint inhibitors | |||||
| Atezolizumab | 98 | 25 | 57 | 16 | |
| Durvalumab | 32 | 10 | 20 | 2 | 0.34 |
| Univariate | Multivariate | |||
|---|---|---|---|---|
| HR (95% CI) | p Value | HR (95% CI) | p Value | |
| Age (≥75 vs. <75) | 1.43 (0.87–2.35) | 0.16 | 1.66 (1.01–2.76) | 0.06 |
| PS (0–1 vs. 2–3) | 0.89 (0.53–1.43) | 0.59 | 0.79 (0.71–2.00) | 0.50 |
| Liver metastasis | 1.81 (1.13–2.91) | 0.01 | 2.03 (1.25–3.30) | 0.002 |
| NLR (<5.0 vs. ≥5.0) | 0.60 (0.37–0.97) | 0.04 | 0.97 (0.68–2.55) | 0.07 |
| Alb (<3.5 vs. ≥3.5) | 2.02 (1.30–3.14) | <0.001 | 1.84 (1.14–2.96) | 0.02 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hatori, T.; Numata, T.; Shiozawa, T.; Taguchi, M.; Sakurai, H.; Tamura, T.; Kanazawa, J.; Tachi, H.; Kondo, K.; Miyazaki, K.; et al. Prognostic Factors for Patients with Small-Cell Lung Cancer Treated with Chemoimmunotherapy: A Retrospective Multicenter Study. Curr. Oncol. 2024, 31, 6502-6511. https://doi.org/10.3390/curroncol31110482
Hatori T, Numata T, Shiozawa T, Taguchi M, Sakurai H, Tamura T, Kanazawa J, Tachi H, Kondo K, Miyazaki K, et al. Prognostic Factors for Patients with Small-Cell Lung Cancer Treated with Chemoimmunotherapy: A Retrospective Multicenter Study. Current Oncology. 2024; 31(11):6502-6511. https://doi.org/10.3390/curroncol31110482
Chicago/Turabian StyleHatori, Takashi, Takeshi Numata, Toshihiro Shiozawa, Manato Taguchi, Hirofumi Sakurai, Tomohiro Tamura, Jun Kanazawa, Hiroaki Tachi, Kyoko Kondo, Kunihiko Miyazaki, and et al. 2024. "Prognostic Factors for Patients with Small-Cell Lung Cancer Treated with Chemoimmunotherapy: A Retrospective Multicenter Study" Current Oncology 31, no. 11: 6502-6511. https://doi.org/10.3390/curroncol31110482
APA StyleHatori, T., Numata, T., Shiozawa, T., Taguchi, M., Sakurai, H., Tamura, T., Kanazawa, J., Tachi, H., Kondo, K., Miyazaki, K., Kikuchi, N., Kurishima, K., Satoh, H., & Hizawa, N. (2024). Prognostic Factors for Patients with Small-Cell Lung Cancer Treated with Chemoimmunotherapy: A Retrospective Multicenter Study. Current Oncology, 31(11), 6502-6511. https://doi.org/10.3390/curroncol31110482





