Twenty Years of Advancements in a Radiotherapy Facility: Clinical Protocols, Technology, and Management
Abstract
1. Introduction
2. Materials and Methods
- (1)
- Standard Delivery: 3D CRT and Portal Imaging IGRT
- (2)
- Advanced Delivery: IMRT-VMAT irradiation
- (3)
- CBCT IGRT: Cone beam CT IGRT capability
- (4)
- FFF: Flattening Filter Free Beams capability
- (5)
- 6DOF: Six Degrees of Freedom Couch
- (6)
- SGRT: Surface Guided Radiotherapy System
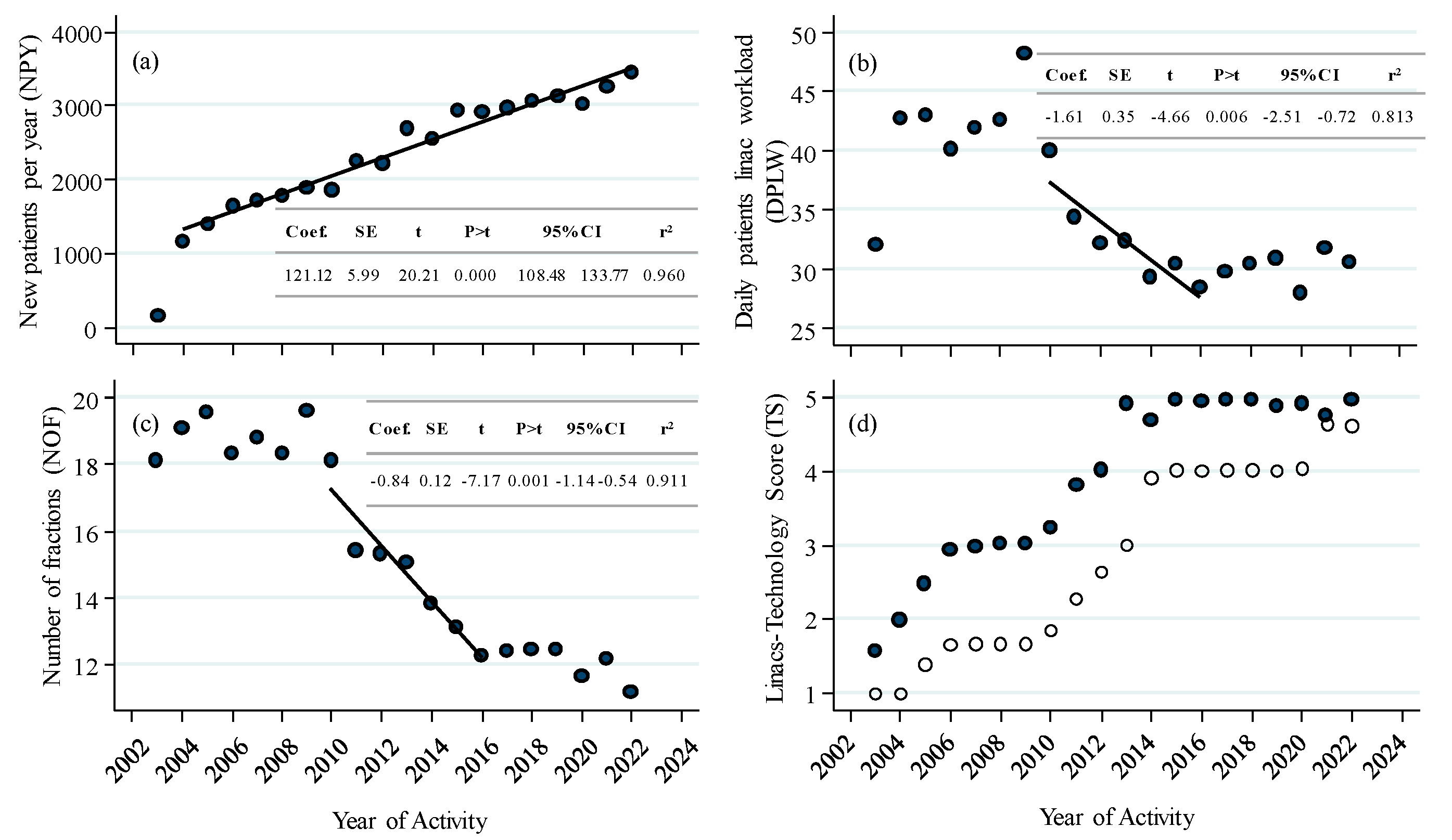
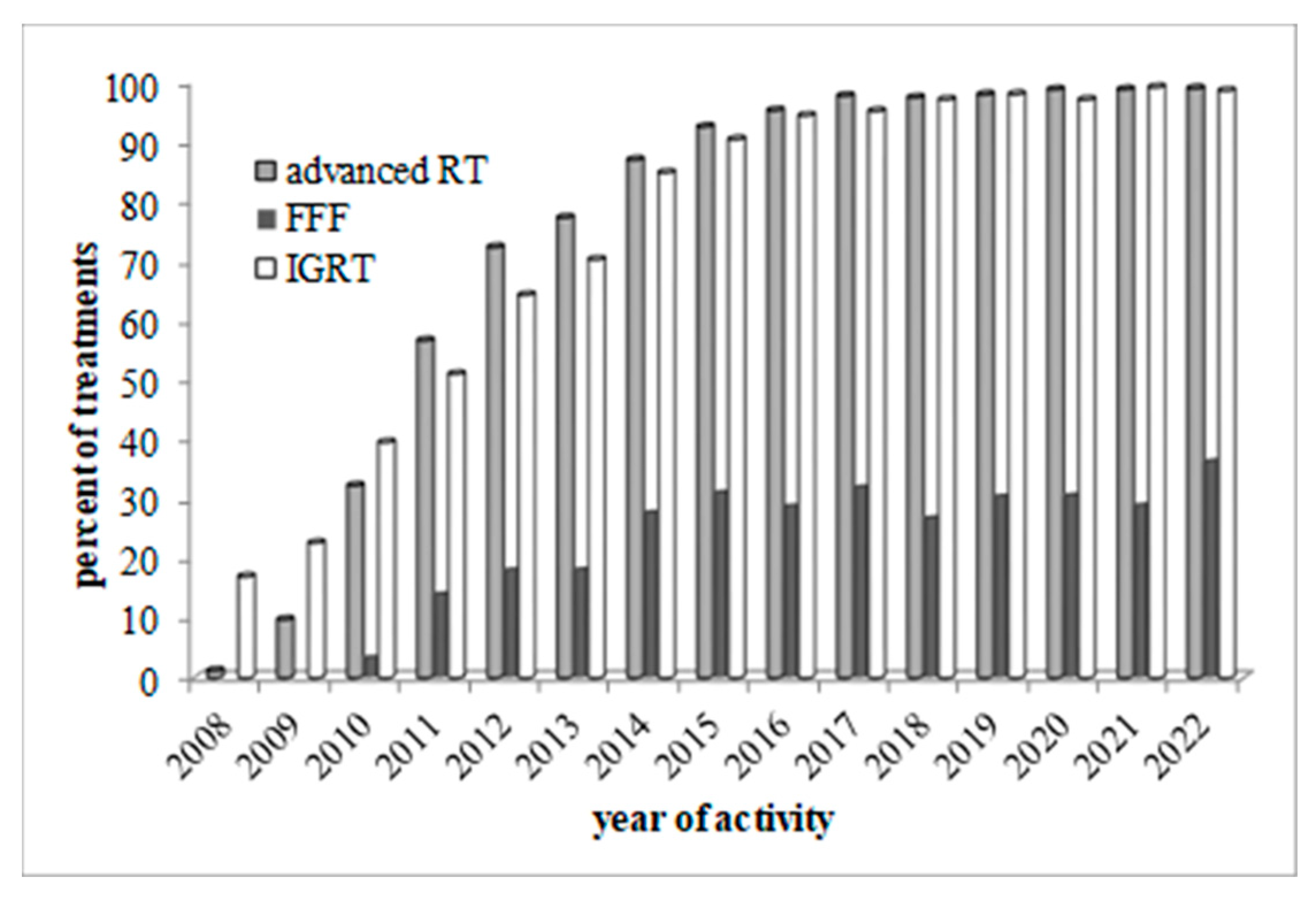
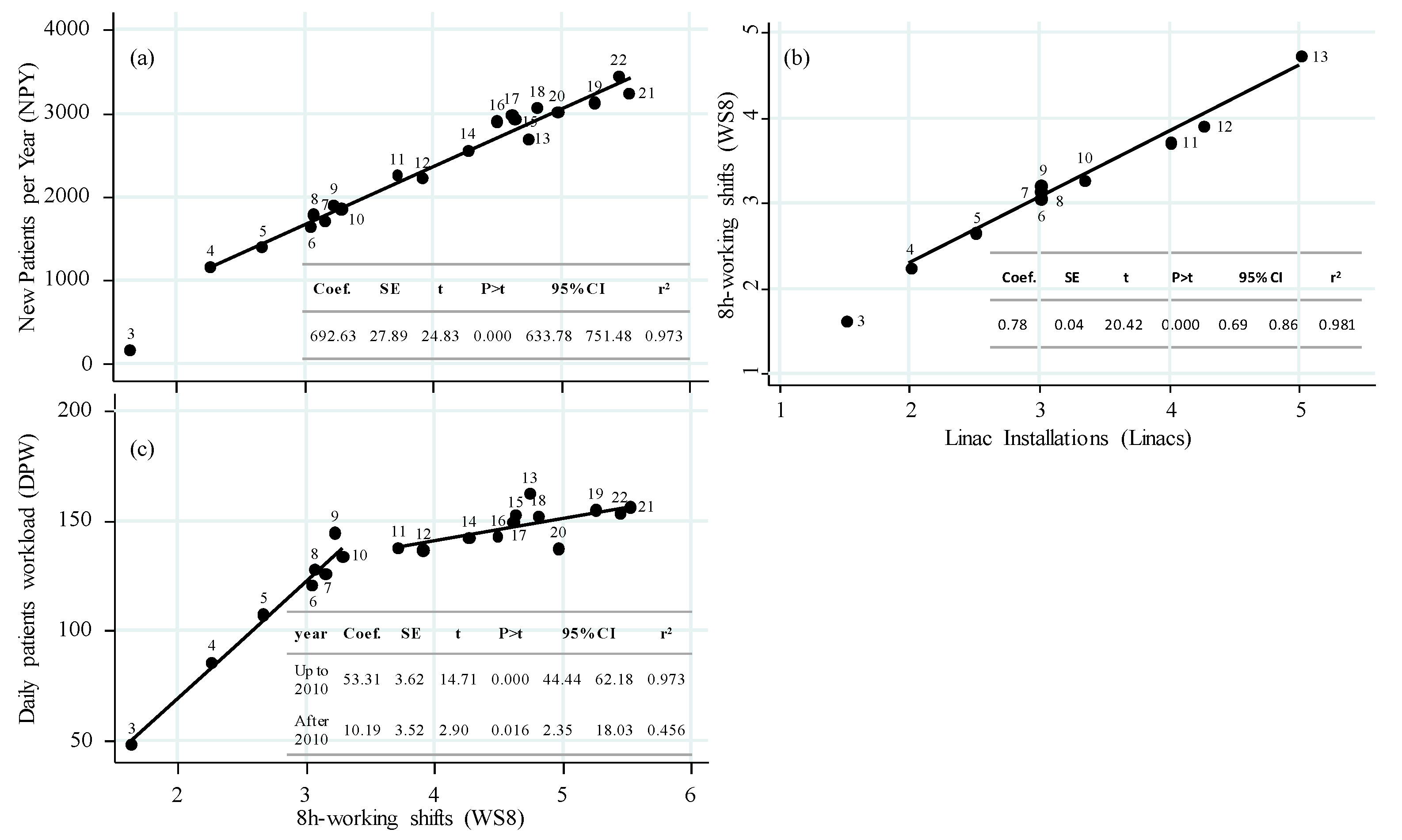
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Chetty, I.J.; Martel, M.K.; Jaffray, D.A.; Benedict, S.H.; Hahn, S.M.; Berbeco, R.; Deye, J.; Jeraj, R.; Kavanagh, B.; Krishnan, S.; et al. Technology for Innovation in Radiation Oncology. Int. J. Radiat. Oncol. Biol. Phys. 2015, 93, 485–492. [Google Scholar] [CrossRef] [PubMed]
- Smith, G.L.; Ganz, P.A.; Bekelman, J.E.; Chmura, S.J.; Dignam, J.J.; Efstathiou, J.A.; Jagsi, R.; Johnstone, P.A.; Steinberg, M.L.; Williams, S.B.; et al. Promoting the Appropriate Use of Advanced Radiation Technologies in Oncology: Summary of a National Cancer Policy Forum Workshop. Int. J. Radiat. Oncol. Biol. Phys. 2017, 97, 450–461. [Google Scholar] [CrossRef] [PubMed]
- Atun, R.; Jaffray, D.A.; Barton, M.B.; Bray, F.; Baumann, M.; Vikram, B.; Hanna, T.P.; Knaul, F.M.; Lievens, Y.; Lui, T.Y.M.; et al. Expanding Global Access to Radiotherapy. Lancet Oncol. 2015, 16, 1153–1186. [Google Scholar] [CrossRef]
- Franceschini, D.; Cozzi, L.; De Rose, F.; Navarria, P.; Franzese, C.; Comito, T.; Iftode, C.; Tozzi, A.; Di Brina, L.; Ascolese, A.M.; et al. Role of Stereotactic Body Radiation Therapy for Lung Metastases from Radio-Resistant Primary Tumours. J. Cancer Res. Clin. Oncol. 2017, 143, 1293–1299. [Google Scholar] [CrossRef]
- Chi, A.; Liao, Z.; Nguyen, N.P.; Xu, J.; Stea, B.; Komaki, R. Systemic Review of the Patterns of Failure Following Stereotactic Body Radiation Therapy in Early-Stage Non-Small-Cell Lung Cancer: Clinical Implications. Radiother. Oncol. 2010, 94, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Franceschini, D.; De Rose, F.; Fogliata, A.; Navarria, P.; Ascolese, A.M.; Franzese, C.; Comito, T.; Tozzi, A.; Iftode, C.; Di Brina, L.; et al. Volumetric Modulated Arc Therapy for Thoracic Node Metastases: A Safe and Effective Treatment for a Neglected Disease. Oncotarget 2016, 7, 53321–53329. [Google Scholar] [CrossRef]
- Comito, T.; Cozzi, L.; Zerbi, A.; Franzese, C.; Clerici, E.; Tozzi, A.; Iftode, C.; Navarria, P.; D’Agostino, G.; Fogliata, A.; et al. Clinical Results of Stereotactic Body Radiotherapy (SBRT) in the Treatment of Isolated Local Recurrence of Pancreatic Cancer after R0 Surgery: A Retrospective Study. Eur. J. Surg. Oncol. 2017, 43, 735–742. [Google Scholar] [CrossRef]
- Franzese, C.; Franceschini, D.; Cozzi, L.; D’Agostino, G.; Comito, T.; De Rose, F.; Navarria, P.; Mancosu, P.; Tomatis, S.; Fogliata, A.; et al. Minimally Invasive Stereotactical Radio-Ablation of Adrenal Metastases as an Alternative to Surgery. Cancer Res. Treat. 2017, 49, 20–28. [Google Scholar] [CrossRef] [PubMed]
- Hawkins, P.G.; Kadam, A.S.; Jackson, W.C.; Eisbruch, A. Organ-Sparing in Radiotherapy for Head-and-Neck Cancer: Improving Quality of Life. Semin. Radiat. Oncol. 2018, 28, 46–52. [Google Scholar] [CrossRef]
- Mishra, M.V.; Louie, A.V.; Gondi, V.; Slotman, B. The Evolving Role of Radiotherapy in the Management of Small Cell Lung Cancer. J. Thorac. Dis. 2018, 10, S2545–S2554. [Google Scholar] [CrossRef]
- Grimm, J.; Marks, L.B.; Jackson, A.; Kavanagh, B.D.; Xue, J.; Yorke, E. High Dose per Fraction, Hypofractionated Treatment Effects in the Clinic (HyTEC): An Overview. Int. J. Radiat. Oncol. Biol. Phys. 2021, 110, 1–10. [Google Scholar] [CrossRef]
- Fransson, P.; Nilsson, P.; Gunnlaugsson, A.; Beckman, L.; Tavelin, B.; Norman, D.; Thellenberg-Karlsson, C.; Hoyer, M.; Lagerlund, M.; Kindblom, J.; et al. Ultra-Hypofractionated versus Conventionally Fractionated Radiotherapy for Prostate Cancer (HYPO-RT-PC): Patient-Reported Quality-of-Life Outcomes of a Randomised, Controlled, Non-Inferiority, Phase 3 Trial. Lancet Oncol. 2021, 22, 235–245. [Google Scholar] [CrossRef]
- Moon, D.H.; Efstathiou, J.A.; Chen, R.C. What Is the Best Way to Radiate the Prostate in 2016? Urol. Oncol. Semin. Orig. Investig. 2017, 35, 59–68. [Google Scholar] [CrossRef] [PubMed]
- Haviland, J.S.; Owen, J.R.; Dewar, J.A.; Agrawal, R.K.; Barrett, J.; Barrett-Lee, P.J.; Dobbs, H.J.; Hopwood, P.; Lawton, P.A.; Magee, B.J.; et al. The UK Standardisation of Breast Radiotherapy (START) Trials of Radiotherapy Hypofractionation for Treatment of Early Breast Cancer: 10-Year Follow-up Results of Two Randomised Controlled Trials. Lancet Oncol. 2013, 14, 1086–1094. [Google Scholar] [CrossRef]
- Perry, J.R.; Laperriere, N.; O’Callaghan, C.J.; Brandes, A.A.; Menten, J.; Phillips, C.; Fay, M.; Nishikawa, R.; Cairncross, J.G.; Roa, W.; et al. Short-Course Radiation plus Temozolomide in Elderly Patients with Glioblastoma. N. Engl. J. Med. 2017, 376, 1027–1037. [Google Scholar] [CrossRef] [PubMed]
- Navarria, P.; Pessina, F.; Tomatis, S.; Soffietti, R.; Grimaldi, M.; Lopci, E.; Chiti, A.; Leonetti, A.; Casarotti, A.; Rossi, M.; et al. Are Three Weeks Hypofractionated Radiation Therapy (HFRT) Comparable to Six Weeks for Newly Diagnosed Glioblastoma Patients? Results of a Phase II Study. Oncotarget 2017, 8, 67696–67708. [Google Scholar] [CrossRef]
- Nicholas, S.; Chen, L.; Choflet, A.; Fader, A.; Guss, Z.; Hazell, S.; Song, D.Y.; Tran, P.T.; Viswanathan, A.N. Pelvic Radiation and Normal Tissue Toxicity. Semin. Radiat. Oncol. 2017, 27, 358–369. [Google Scholar] [CrossRef]
- Grégoire, V.; Langendijk, J.A.; Nuyts, S. Advances in Radiotherapy for Head and Neck Cancer. J. Clin. Oncol. 2015, 33, 3277–3284. [Google Scholar] [CrossRef]
- Koontz, B.F.; Bossi, A.; Cozzarini, C.; Wiegel, T.; D’Amico, A. A Systematic Review of Hypofractionation for Primary Management of Prostate Cancer. Eur. Urol. 2015, 68, 683–691. [Google Scholar] [CrossRef]
- Scorsetti, M.; Comito, T.; Tozzi, A.; Navarria, P.; Fogliata, A.; Clerici, E.; Mancosu, P.; Reggiori, G.; Rimassa, L.; Torzilli, G.; et al. Final Results of a Phase II Trial for Stereotactic Body Radiation Therapy for Patients with Inoperable Liver Metastases from Colorectal Cancer. J. Cancer Res. Clin. Oncol. 2015, 141, 543–553. [Google Scholar] [CrossRef] [PubMed]
- Falkson, C.B.; Vella, E.T.; Yu, E.; El-Mallah, M.; Mackenzie, R.; Ellis, P.M.; Ung, Y.C. Radiotherapy With Curative Intent in Patients With Early-Stage, Medically Inoperable, Non–Small-Cell Lung Cancer: A Systematic Review. Clin. Lung Cancer 2017, 18, 105–121.e5. [Google Scholar] [CrossRef]
- De Los Santos, J.; Popple, R.; Agazaryan, N.; Bayouth, J.E.; Bissonnette, J.P.; Bucci, M.K.; Dieterich, S.; Dong, L.; Forster, K.M.; Indelicato, D.; et al. Image Guided Radiation Therapy (IGRT) Technologies for Radiation Therapy Localization and Delivery. Int. J. Radiat. Oncol. Biol. Phys. 2013, 87, 33–45. [Google Scholar] [CrossRef]
- Korreman, S.; Rasch, C.; McNair, H.; Verellen, D.; Oelfke, U.; Maingon, P.; Mijnheer, B.; Khoo, V. The European Society of Therapeutic Radiology and Oncology-European Institute of Radiotherapy (ESTRO-EIR) Report on 3D CT-Based in-Room Image Guidance Systems: A Practical and Technical Review and Guide. Radiother. Oncol. 2010, 94, 129–144. [Google Scholar] [CrossRef]
- Jaffray, D.A.; Das, S.; Jacobs, P.M.; Jeraj, R.; Lambin, P. How Advances in Imaging Will Affect Precision Radiation Oncology. Int. J. Radiat. Oncol. Biol. Phys. 2018, 101, 292–298. [Google Scholar] [CrossRef] [PubMed]
- Vaandering, A.; Jansen, N.; Weltens, C.; Moretti, L.; Stellamans, K.; Vanhoutte, F.; Scalliet, P.; Remouchamps, V.; Lievens, Y. Radiotherapy-Specific Quality Indicators at National Level: How to Make It Happen. Radiother. Oncol. 2023, 178, 109433. [Google Scholar] [CrossRef]
- McNutt, T.R.; Bowers, M.; Cheng, Z.; Han, P.; Hui, X.; Moore, J.; Robertson, S.; Mayo, C.; Voong, R.; Quon, H. Practical Data Collection and Extraction for Big Data Applications in Radiotherapy. Med. Phys. 2018, 45, e863–e869. [Google Scholar] [CrossRef]
- Skripcak, T.; Belka, C.; Bosch, W.; Brink, C.; Brunner, T.; Budach, V.; Büttner, D.; Debus, J.; Dekker, A.; Grau, C.; et al. Creating a Data Exchange Strategy for Radiotherapy Research: Towards Federated Databases and Anonymised Public Datasets. Radiother. Oncol. 2014, 113, 303–309. [Google Scholar] [CrossRef] [PubMed]
- D’Agostino, G.R.; Mancosu, P.; Di Brina, L.; Franzese, C.; Pasini, L.; Iftode, C.; Comito, T.; De Rose, F.; Guazzoni, G.F.; Scorsetti, M. Stereotactic Body Radiation Therapy for Intermediate-Risk Prostate Cancer with VMAT and Real-Time Electromagnetic Tracking: A Phase II Study. Am. J. Clin. Oncol. Cancer Clin. Trials 2020, 43, 628–635. [Google Scholar] [CrossRef]
- Scorsetti, M.; Comito, T.; Clerici, E.; Franzese, C.; Tozzi, A.; Iftode, C.; Di Brina, L.; Navarria, P.; Mancosu, P.; Reggiori, G.; et al. Phase II Trial on SBRT for Unresectable Liver Metastases: Long-Term Outcome and Prognostic Factors of Survival after 5 Years of Follow-Up. Radiat. Oncol. 2018, 13, 234. [Google Scholar] [CrossRef]
- Scorsetti, M.; Alongi, F.; Fogliata, A.; Pentimalli, S.; Navarria, P.; Lobefalo, F.; Garcia-Etienne, C.; Clivio, A.; Cozzi, L.; Mancosu, P.; et al. Phase I-II Study of Hypofractionated Simultaneous Integrated Boost Using Volumetric Modulated Arc Therapy for Adjuvant Radiation Therapy in Breast Cancer Patients: A Report of Feasibility and Early Toxicity Results in the First 50 Treatments. Radiat. Oncol. 2012, 7, 145. [Google Scholar] [CrossRef] [PubMed]
- Schmitt, D.; Blanck, O.; Gauer, T.; Fix, M.K.; Brunner, T.B.; Fleckenstein, J.; Loutfi-Krauss, B.; Manser, P.; Werner, R.; Wilhelm, M.L.; et al. Technological Quality Requirements for Stereotactic Radiotherapy: Expert Review Group Consensus from the DGMP Working Group for Physics and Technology in Stereotactic Radiotherapy. Strahlentherapie Onkol. 2020, 196, 421–443. [Google Scholar] [CrossRef] [PubMed]
- Guckenberger, M.; Baus, W.W.; Blanck, O.; Combs, S.E.; Debus, J.; Engenhart-Cabillic, R.; Gauer, T.; Grosu, A.L.; Schmitt, D.; Tanadini-Lang, S.; et al. Definition and Quality Requirements for Stereotactic Radiotherapy: Consensus Statement from the DEGRO/DGMP Working Group Stereotactic Radiotherapy and Radiosurgery. Strahlentherapie Onkol. 2020, 196, 417–420. [Google Scholar] [CrossRef] [PubMed]
- Franzese, C.; Tomatis, S.; Bianchi, S.P.; Pelizzoli, M.; Teriaca, M.A.; Badalamenti, M.; Comito, T.; Clerici, E.; Franceschini, D.; Navarria, P.; et al. Adaptive Volumetric-Modulated Arc Radiation Therapy for Head and Neck Cancer: Evaluation of Benefit on Target Coverage and Sparing of Organs at Risk. Curr. Oncol. 2023, 30, 3344–3354. [Google Scholar] [CrossRef]
- Borras, J.M.; Grau, C.; Corral, J.; Wong, K.; Barton, M.B.; Ferlay, J.; Bray, F.; Lievens, Y. Estimating the Number of Fractions by Tumour Site for European Countries in 2012 and 2025: An ESTRO-HERO Analysis. Radiother. Oncol. 2018, 126, 198–204. [Google Scholar] [CrossRef]
- Irabor, O.C.; Swanson, W.; Shaukat, F.; Wirtz, J.; Mallum, A.A.; Ngoma, T.; Elzawawy, A.; Nguyen, P.; Incrocci, L.; Ngwa, W. Can the Adoption of Hypofractionation Guidelines Expand Global Radiotherapy Access? An Analysis for Breast and Prostate Radiotherapy. JCO Glob. Oncol. 2020, 6, 667–678. [Google Scholar] [CrossRef]
- Spencer, K.; Defourny, N.; Tunstall, D.; Cosgrove, V.; Kirkby, K.; Henry, A.; Lievens, Y.; Hall, P. Variable and Fixed Costs in NHS Radiotherapy; Consequences for Increasing Hypo Fractionation. Radiother. Oncol. 2022, 166, 180–188. [Google Scholar] [CrossRef]
- Lievens, Y.; Borras, J.M.; Grau, C.; Aggarwal, A. Value-Based Radiotherapy: A New Chapter of the ESTRO-HERO Project. Radiother. Oncol. 2021, 160, 236–239. [Google Scholar] [CrossRef]
- Burnet, N.G.; Routsis, D.S.; Murrell, P.; Burton, K.E.; Taylor, P.J.; Thomas, S.J.; Williams, M.V.; Prevost, A.T. A Tool to Measure Radiotherapy Complexity and Workload: Derivation from the Basic Treatment Equivalent (BTE) Concept. Clin. Oncol. 2001, 13, 14–23. [Google Scholar] [CrossRef]
- Stewart, E.; Sun, I.; Kim, C.; Giddings, A.; Silverio, F.; Taruc, O.; Nica, L. Examining Radiation Treatment Appointment Times at a Canadian Cancer Centre: A Timing Study. J. Med. Imaging Radiat. Sci. 2019, 50, 536–542. [Google Scholar] [CrossRef]
- Lievens, Y. Access to Innovative Radiotherapy: How to Make It Happen from an Economic Perspective? Acta Oncol. 2017, 56, 1353–1358. [Google Scholar] [CrossRef]
- Gao, Y.; Liu, R.; Chang, C.W.; Charyyev, S.; Zhou, J.; Bradley, J.D.; Liu, T.; Yang, X. A Potential Revolution in Cancer Treatment: A Topical Review of FLASH Radiotherapy. J. Appl. Clin. Med. Phys. 2022, 23, e13790. [Google Scholar] [CrossRef] [PubMed]
- Mazal, A.; Vera Sanchez, J.A.; Sanchez-Parcerisa, D.; Udias, J.M.; España, S.; Sanchez-Tembleque, V.; Fraile, L.M.; Bragado, P.; Gutierrez-Uzquiza, A.; Gordillo, N.; et al. Biological and Mechanical Synergies to Deal With Proton Therapy Pitfalls: Minibeams, FLASH, Arcs, and Gantryless Rooms. Front. Oncol. 2021, 10, 613669. [Google Scholar] [CrossRef] [PubMed]
- Jereczek-Fossa, B.A.; Palazzi, M.F.; Tonoli, S.; Zaffaroni, M.; Marvaso, G.; Ivaldi, G.B.; Amadori, M.; Antognoni, P.; Arcangeli, S.; Buffoli, A.; et al. Almost One Year of COVID-19 Pandemic: How Radiotherapy Centers Have Counteracted Its Impact on Cancer Treatment in Lombardy, Italy. CODRAL/AIRO-L Study. Tumori J. 2022, 108, 177–181. [Google Scholar] [CrossRef] [PubMed]

| Parameter | Specification |
|---|---|
| Date | session date |
| Linac | treatment machine (linear accelerator) |
| WS8 | mean total operational hours per day of each linac normalized by 8 h (i.e., the standard working shift) |
| Treatment time (TRT) | total treatment irradiation time |
| Dose | prescribed treatment dose (Gy) |
| Number of fractions (NOF) | total number of fractions in a therapy course 1 |
| Technique | standard (3D CRT-rotational arc) or advanced (IMRT-VMAT) therapy |
| FFF | use of high intensity flattening filter free (FFF) beams |
| IGRT | use of Image Guided RT in a therapy session |
| Machine | Replacing 1 | Operation (Start–End) | Main Features | TS 2 |
|---|---|---|---|---|
| Linac 1 | (new) | November 2003–December 2011 | Standard Delivery | 1 |
| Linac 2 | (new) | November 2003–December 2013 | Standard Delivery | 1 |
| Linac 3 | (new) | July 2005 | Standard Delivery, Advanced Delivery, CBCT IGRT 3 | 3 |
| Linac 4 | (new) | September 2010 | Standard Delivery, Advanced Delivery, CBCT IGRT, FFF | 4 |
| Linac 5 | Linac 1 | January 2012–November 2020 | Standard Delivery, Advanced Delivery | 2 |
| Linac 6 | (new) | October 2012 | Standard Delivery, Advanced Delivery, CBCT IGRT, FFF, 6DOF | 5 |
| Linac 7 | Linac 2 | March 2014 | Standard Delivery, Advanced Delivery, CBCT IGRT, FFF, 6DOF, SGRT | 6 |
| Linac 8 | Linac 5 | February 2021 | Standard Delivery, Advanced Delivery, CBCT IGRT, FFF, 6DOF | 5 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tomatis, S.; Mancosu, P.; Reggiori, G.; Lobefalo, F.; Gallo, P.; Lambri, N.; Paganini, L.; La Fauci, F.; Bresolin, A.; Parabicoli, S.; et al. Twenty Years of Advancements in a Radiotherapy Facility: Clinical Protocols, Technology, and Management. Curr. Oncol. 2023, 30, 7031-7042. https://doi.org/10.3390/curroncol30070510
Tomatis S, Mancosu P, Reggiori G, Lobefalo F, Gallo P, Lambri N, Paganini L, La Fauci F, Bresolin A, Parabicoli S, et al. Twenty Years of Advancements in a Radiotherapy Facility: Clinical Protocols, Technology, and Management. Current Oncology. 2023; 30(7):7031-7042. https://doi.org/10.3390/curroncol30070510
Chicago/Turabian StyleTomatis, Stefano, Pietro Mancosu, Giacomo Reggiori, Francesca Lobefalo, Pasqualina Gallo, Nicola Lambri, Lucia Paganini, Francesco La Fauci, Andrea Bresolin, Sara Parabicoli, and et al. 2023. "Twenty Years of Advancements in a Radiotherapy Facility: Clinical Protocols, Technology, and Management" Current Oncology 30, no. 7: 7031-7042. https://doi.org/10.3390/curroncol30070510
APA StyleTomatis, S., Mancosu, P., Reggiori, G., Lobefalo, F., Gallo, P., Lambri, N., Paganini, L., La Fauci, F., Bresolin, A., Parabicoli, S., Pelizzoli, M., Navarria, P., Franzese, C., Lenoci, D., & Scorsetti, M. (2023). Twenty Years of Advancements in a Radiotherapy Facility: Clinical Protocols, Technology, and Management. Current Oncology, 30(7), 7031-7042. https://doi.org/10.3390/curroncol30070510






