Fear of Cancer Recurrence and Coping Strategies among Prostate Cancer Survivors: A Qualitative Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Design and Participants
2.2. Ethics Considerations
2.3. Data Collection
2.4. Data Analysis
2.5. Trustworthiness of Data
3. Results
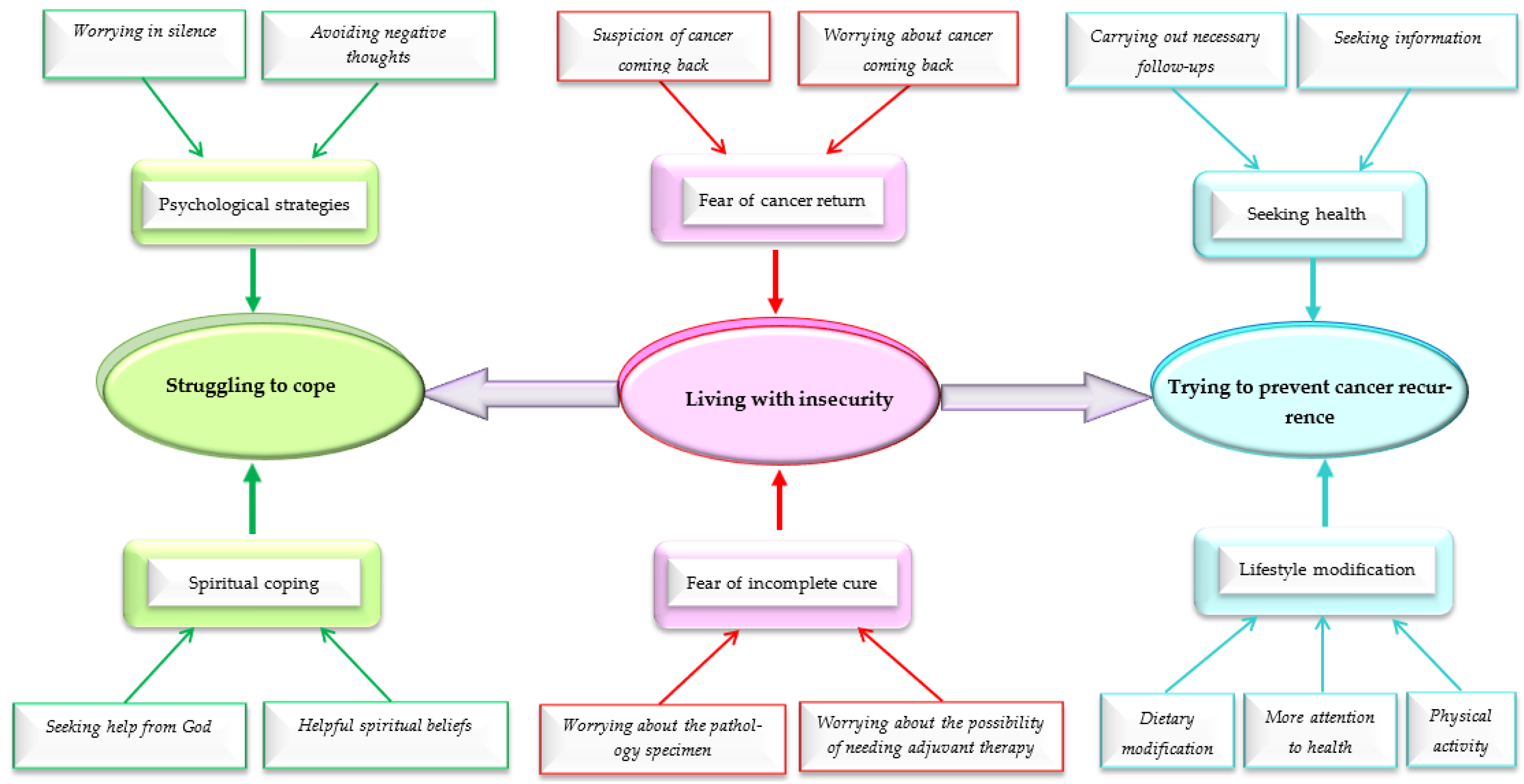
3.1. Living with Insecurity
3.1.1. Fear of Incomplete Cure
- (1)
- Worrying about the pathology specimen.
“Ever since the doctor talked to me about the pathology specimen, I was worried about the answer and I was thinking about what was going to happen.”(Participant 4)
“When we wanted to go to the doctor’s office to show the pathology result, I did not look at the result, I mean, I did not dare to look at it at all, I asked my wife to show it to the doctor.”(Participant 2)
“When the doctor saw the pathology result, he said that there are still cancer cells. When I heard this, I felt that my death was near and that my cancer would not be cured.”(Participant 13)
- (2)
- Worrying about the possibility of needing adjuvant therapy.
“My own father had stomach cancer and he received radiotherapy and chemotherapy…he became weak little by little and then passed away after a year…when I heard that chemotherapy or radiotherapy should be done If the pathology specimen result be unfavorable… I was worried that my situation would be like him.”(Participant 9)
“Chemotherapy or radiation therapy itself is one side of the issue, and the fact that it implicates the whole family and causes the family to suffer is another side of the issue.”.(Participant 12)
3.1.2. Fear of Cancer Return
- (1)
- Worrying about cancer coming back.
“When I went to perform this test [PSA] and even close to the time of the test, I was very worried about what the result of this test would be… this worry between taking this test and awaiting to get the result and show it to the doctor became much more and I had stress.”(Participant 4)
“The doctor said that my cancer score was 8 and ‘if you had come a little later, it was not clear what would happen to you.’ The fact that my cancer is advanced at the time of diagnosis makes me more worried about that my cancer might come back one day.”(Participant 8)
“I always think that if my cancer returns what will happen to me, my children are girls; I think about these things.”(Participant 9)
- (2)
- Suspicion of cancer coming back.
“About one month after that I was discharged from the hospital, I do not know what was the problem that caused my urination to be drop by drop. During that month, I was very bothered when urinating, which made me suspect that my cancer has relapsed.”(Participant 8)
“It was 10 months after my surgery that I had severe back pain. I had already read on the Internet about the recurrence of prostate cancer and its metastasis, and I knew that prostate cancer might give metastasis to bones and vertebrae of my back. I thought that cancer had spread in my body.”(Participant 11)
3.2. Struggling to Cope
3.2.1. Psychological Strategies
- (1)
- Worrying in silence.
“I did not want my wife and children to know my concern about the possibility of cancer recurrence and they would also become worried.”(Participant 10)
- (2)
- Avoiding negative thoughts.
“I try not to think about it at all; there is a law called the law of attraction, and in my opinion, whatever you think about, you attract it… if I think about cancer returning, I think this issue will happen. That is why I do not think about it at all.”(Participant 13)
“When the thought of cancer recurrence comes to me, I try not to give too much attention to it… At such times, I make myself busy with other things, for example, I go to watch the TV or read a book.”(Participant 12)
3.2.2. Spiritual Coping
- (1)
- Seeking help from God.
“When I was waiting for the PSA test result, I was very stressed, I talked to God and asked for his help, and this was relaxing for me down.”(Participant 1)
“I ask God to take care of me and I still have a lot of work to do and I have three daughters that I have to take care of, just talking to God helps me a lot to deal with this worry.”(Participant 9)
- (2)
- Helpful spiritual beliefs.
“The world is a place of passage, and this world is a passage and not for permanent residency; after all, we will all leave this world one day and I have to leave one day. Therefore, I am not too worried about cancer recurrence.”(Participant 6)
“I always tell God that I will accept whatever you decide for me and I have no complaints against you. I believe that God wanted to give me this cancer and nothing will happen until God wills and this belief helps me to better deal with this worry of recurrence.”(Participant 4)
“I left everything to God and I think this is the best thing that will reduce my worries about cancer recurrence.” .(Participant 5)
3.3. Trying to Prevent Cancer Recurrence
3.3.1. Seeking Health
- (1)
- Seeking information.
“I read a lot on the internet about the things that should be done to prevent cancer recurrence, and I tried to incorporate them into my life if they made sense.”(Participant 11)
“One of the issues I expected to get information about was the issue of cancer relapse and what I need to do to prevent it from coming back, but no one talked to me about that.”(Participant 13)
- (2)
- Carrying out necessary follow-ups.
“The doctor told me that this test (PSA) could show the state of my cancer and I performed this test based on the doctor’s advice.”(Participant 1)
“Pain in my pelvic bones occurred about 5 to 6 months after the end of radiotherapy. I thought that my cancer had metastasized to my pelvic bones, so I immediately informed my doctor.”(Participant 13)
3.3.2. Lifestyle Modification
- (1)
- Physical activity.
“I know that regular physical activity can reduce the risk of cancer recurrence, so I walk every day. Also, sometimes when I have something to do, I try not to use my car or taxi and go on foot.”(Participant 9)
- (2)
- More attention to health.
“I do not stress myself for trivial issues anymore, because I know that stress is the cause of many diseases and may even cause my cancer to come back.”(Participant 11)
“Perhaps the most important change that I made in my life after cancer was related to smoking. I had been smoking for more than 30 years. When I was in the hospital, I asked the doctor if smoking would have an effect on my cancer. He said that it is better not to smoke and that it may affect the return of your cancer or even other cancers, so after the surgery, I reduced the amount of smoking and I stopped smoking completely three months after the surgery.”(Participant 9)
- (3)
- Dietary modification.
“I include fruit three times a day in my diet, one in the morning, one in the evening, and one at night, or for example, I read somewhere that some types of tea have additives that may be related to cancer, and after that, I only use organic tea without additives.”(Participant 12)
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. International Agency for Research on Cancer. Global Cancer Observatory. 2018. Available online: https://gco.iarc.fr/ (accessed on 15 October 2020).
- Fitch, M.I. Transition to survivorship: Can there be improvement? Curr. Opin. Support Palliat. Care 2018, 12, 74–79. [Google Scholar] [CrossRef]
- Siegel, R.L.; Miller, K.D.; Fuchs, H.E.; Jemal, A. Cancer statistics, 2022. CA Cancer J. Clin. 2022, 72, 7–33. [Google Scholar] [CrossRef]
- Drummond, F.J.; Kinnear, H.; O’Leary, E.; Gavin, A.; Sharp, L. Long-term health-related quality of life of prostate cancer survivors varies by primary treatment. Results from the PiCTure (Prostate Cancer Treatment, your experience) study. J. Cancer Surviv. 2015, 9, 361–372. [Google Scholar] [CrossRef]
- Mardani, A.; Razi, S.P.; Mazaheri, R.; Dianatinasab, M.; Vaismoradi, M. Health-related quality of life in prostate cancer survivors: Implications for nursing care. Int. J. Caring Sci. 2020, 13, 1322. [Google Scholar]
- Hart, S.L.; Latini, D.M.; Cowan, J.E.; Carroll, P.R. Fear of recurrence, treatment satisfaction, and quality of life after radical prostatectomy for prostate cancer. Support. Care Cancer Off. J. Multinatl. Assoc. Support. Care Cancer 2008, 16, 161–169. [Google Scholar] [CrossRef]
- Bellizzi, K.M.; Latini, D.M.; Cowan, J.E.; DuChane, J.; Carroll, P.R. Fear of recurrence, symptom burden, and health-related quality of life in men with prostate cancer. Urology 2008, 72, 1269–1273. [Google Scholar] [CrossRef]
- Butow, P.N.; Fardell, J.E.; Smith, A. Fear of cancer recurrence: An overview and Australian perspective. Cancer Forum 2015, 39, 95–100. [Google Scholar]
- Meissner, V.H.; Olze, L.; Schiele, S.; Ankerst, D.P.; Jahnen, M.; Gschwend, J.E.; Herkommer, K.; Dinkel, A. Fear of cancer recurrence and disease progression in long-term prostate cancer survivors after radical prostatectomy: A longitudinal study. Cancer 2021, 127, 4287–4295. [Google Scholar] [CrossRef] [PubMed]
- Lebel, S.; Ozakinci, G.; Humphris, G.; Mutsaers, B.; Thewes, B.; Prins, J.; Dinkel, A.; Butow, P.; University of Ottawa Fear of Cancer Recurrence Colloquium, A. From normal response to clinical problem: Definition and clinical features of fear of cancer recurrence. Support. Care Cancer Off. J. Multinatl. Assoc. Support. Care Cancer 2016, 24, 3265–3268. [Google Scholar] [CrossRef]
- van de Wal, M.; van Oort, I.; Schouten, J.; Thewes, B.; Gielissen, M.; Prins, J. Fear of cancer recurrence in prostate cancer survivors. Acta Oncol. 2016, 55, 821–827. [Google Scholar] [CrossRef] [PubMed]
- Marzouk, K.; Assel, M.; Ehdaie, B.; Vickers, A. Long-term cancer specific anxiety in men undergoing active surveillance of prostate cancer: Findings from a large prospective cohort. J. Urol. 2018, 200, 1250–1255. [Google Scholar] [CrossRef] [PubMed]
- James, C.; Brunckhorst, O.; Eymech, O.; Stewart, R.; Dasgupta, P.; Ahmed, K. Fear of cancer recurrence and PSA anxiety in patients with prostate cancer: A systematic review. Support. Care Cancer Off. J. Multinatl. Assoc. Support. Care Cancer 2022, 30, 5577–5589. [Google Scholar] [CrossRef] [PubMed]
- Hong, Y.M.; Hu, J.C.; Paciorek, A.T.; Knight, S.J.; Carroll, P.R. Impact of radical prostatectomy positive surgical margins on fear of cancer recurrence: Results from CaPSURE. Urol. Oncol. 2010, 28, 268–273. [Google Scholar] [CrossRef] [PubMed]
- Anderson, K.; Smith, A.B.; Diaz, A.; Shaw, J.; Butow, P.; Sharpe, L.; Girgis, A.; Lebel, S.; Dhillon, H.; Burhansstipanov, L. A systematic review of fear of cancer recurrence among indigenous and minority peoples. Front. Psychol. 2021, 12, 621850. [Google Scholar] [CrossRef]
- Nilsson, R.; Næss-Andresen, T.F.; Myklebust, T.Å.; Bernklev, T.; Kersten, H.; Haug, E.S. Fear of recurrence in prostate cancer patients: A cross-sectional study after radical prostatectomy or active surveillance. Eur. Urol. Open Sci. 2021, 25, 44–51. [Google Scholar] [CrossRef]
- Vaismoradi, M.; Snelgrove, S. Theme in qualitative content analysis and thematic analysis. Forum Qual. Sozialforschung/Forum Qual. Soc. Res. 2019, 20, 1–14. [Google Scholar] [CrossRef]
- O’Brien, B.C.; Harris, I.B.; Beckman, T.J.; Reed, D.A.; Cook, D.A. Standards for reporting qualitative research: A synthesis of recommendations. Aca. Med. 2014, 89, 1245–1251. [Google Scholar] [CrossRef]
- Mardani, A.; Pedram Razi, S.; Mazaheri, R.; Haghani, S.; Vaismoradi, M. Effect of the exercise programme on the quality of life of prostate cancer survivors: A randomized controlled trial. Int. J. Nurs. Pract. 2021, 27, e12883. [Google Scholar] [CrossRef]
- Maleki, M.; Mardani, A.; Ghafourifard, M.; Vaismoradi, M. Qualitative exploration of sexual life among breast cancer survivors at reproductive age. BMC Women’s Health 2021, 21, 1–10. [Google Scholar] [CrossRef]
- Maleki, M.; Mardani, A.; Ghafourifard, M.; Vaismoradi, M. Changes and challenges in sexual life experienced by the husbands of women with breast cancer: A qualitative study. BMC Women’s Health 2022, 22, 326. [Google Scholar] [CrossRef]
- Vaismoradi, M.; Turunen, H.; Bondas, T. Content analysis and thematic analysis: Implications for conducting a qualitative descriptive study. Nurs. Health Sci. 2013, 15, 398–405. [Google Scholar] [CrossRef]
- Graneheim, U.H.; Lundman, B. Qualitative content analysis in nursing research: Concepts, procedures and measures to achieve trustworthiness. Nurse Educ. Today 2004, 24, 105–112. [Google Scholar] [CrossRef] [PubMed]
- Thomas, E.; Magilvy, J.K. Qualitative rigor or research validity in qualitative research. J. Spec. Pediatr. Nurs. 2011, 16, 151–155. [Google Scholar] [CrossRef] [PubMed]
- Plage, S.; Olson, R.E. Surprise reveals the affective-moral economies in cancer illness narratives. Qual. Health Res. 2021, 31, 2730–2742. [Google Scholar] [CrossRef]
- Sajjadi, M.; Rassouli, M.; Abbaszadeh, A.; Brant, J.; Majd, H.A. Lived experiences of “illness uncertainty” of Iranian cancer patients: A phenomenological hermeneutic study. Cancer Nurs. 2016, 39, E1–E9. [Google Scholar] [CrossRef] [PubMed]
- Maheu, C.; Hébert, M.; Louli, J.; Yao, T.R.; Lambert, S.; Cooke, A.; Black, A.; Kyriacou, J. Revision of the fear of cancer recurrence cognitive and emotional model by Lee-Jones et al with women with breast cancer. Cancer Rep. 2019, 2, e1172. [Google Scholar] [CrossRef]
- Cai, Y.-J. Supportive care needs of Chinese women with newly diagnosed breast cancer prior to adjuvant chemotherapy. Oncol. Nurs. Forum 2021, 48, 341–349. [Google Scholar] [CrossRef]
- Vyas, N.; Brunckhorst, O.; Fox, L.; Van Hemelrijck, M.; Muir, G.; Stewart, R.; Dasgupta, P.; Ahmed, K. Undergoing radical treatment for prostate cancer and its impact on wellbeing: A qualitative study exploring men’s experiences. PLoS ONE 2022, 17, e0279250. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Sun, D.; Wang, Z.; Qin, N. Triggers and Coping Strategies for Fear of Cancer Recurrence in Cancer Survivors: A Qualitative Study. Curr. Oncol. 2022, 29, 9501–9510. [Google Scholar] [CrossRef]
- Tauber, N.M.; O’Toole, M.S.; Dinkel, A.; Galica, J.; Humphris, G.; Lebel, S.; Maheu, C.; Ozakinci, G.; Prins, J.; Sharpe, L. Effect of psychological intervention on fear of cancer recurrence: A systematic review and meta-analysis. J. Clin. Oncol. 2019, 37, 2899. [Google Scholar] [CrossRef]
- Maguire, R.; Hanly, P.; Drummond, F.J.; Gavin, A.; Sharp, L. Regret and fear in prostate cancer: The relationship between treatment appraisals and fear of recurrence in prostate cancer survivors. Psycho-Oncology 2017, 26, 1825–1831. [Google Scholar] [CrossRef] [PubMed]
- Anderson, J.; Burney, S.; Brooker, J.E.; Ricciardelli, L.A.; Fletcher, J.M.; Satasivam, P.; Frydenberg, M. Anxiety in the management of localised prostate cancer by active surveillance. BJU Int. 2014, 114, 55–61. [Google Scholar] [CrossRef] [PubMed]
- van den Bergh, R.C.N.; Essink-Bot, M.L.; Roobol, M.J.; Wolters, T.; Schröder, F.H.; Bangma, C.H.; Steyerberg, E.W. Anxiety and distress during active surveillance for early prostate cancer. Cancer 2009, 115, 3868–3878. [Google Scholar] [CrossRef] [PubMed]
- Lai, W.S.; Shu, B.C.; Hou, W.L. A qualitative exploration of the fear of recurrence among Taiwanese breast cancer survivors. Eur. J. Cancer 2019, 28, e13113. [Google Scholar] [CrossRef]
- Ghasemi, Z. A comparative study of the role and function of fathers in family and satisfaction of their situation. Sociol. Stud. 2012, 4, 91–110. [Google Scholar]
- Shiri, F.H.; Mohtashami, J.; Nasiri, M.; Manoochehri, H.; Rohani, C. Stigma and related factors in Iranian people with cancer. Asian Pac. J. Cancer Prev. 2018, 19, 2285. [Google Scholar]
- Valizadeh, L.; Zamanzadeh, V.; Rahmani, A.; Howard, F.; Nikanfar, A.R.; Ferguson, C. Cancer disclosure: Experiences of Iranian cancer patients. Nurs. Health Sci. 2012, 14, 250–256. [Google Scholar] [CrossRef]
- Koral, L.; Cirak, Y. The relationships between fear of cancer recurrence, spiritual wellbeing and psychological resilience in non-metastatic breast cancer survivors during the COVID-19 outbreak. Psycho-Oncology 2021, 30, 1765–1772. [Google Scholar] [CrossRef]
- Simard, S.; Thewes, B.; Humphris, G.; Dixon, M.; Hayden, C.; Mireskandari, S.; Ozakinci, G. Fear of cancer recurrence in adult cancer survivors: A systematic review of quantitative studies. J. Cancer Surviv. 2013, 7, 300–322. [Google Scholar]
- Almeida, S.N.; Elliott, R.; Silva, E.R.; Sales, C.M.D. Fear of cancer recurrence: A qualitative systematic review and meta-synthesis of patients’ experiences. Clin. Psychol. Rev. 2019, 68, 13–24. [Google Scholar] [CrossRef] [PubMed]
- Séguin Leclair, C.; Lebel, S.; Westmaas, J.L. Can physical activity and healthy diet help long-term cancer survivors manage their fear of recurrence? Front. Psychol. 2021, 12, 647432. [Google Scholar] [CrossRef]
- Li, M.-Y.; Yang, Y.-L.; Liu, L.; Wang, L. Effects of social support, hope and resilience on quality of life among Chinese bladder cancer patients: A cross-sectional study. Health Qual. Life Outcomes 2016, 14, 73. [Google Scholar] [CrossRef] [PubMed]
- Lee-Jones, C.; Humphris, G.; Dixon, R.; Bebbington Hatcher, M. Fear of cancer recurrence—A literature review and proposed cognitive formulation to explain exacerbation of recurrence fears. Psychooncology 1997, 6, 95–105. [Google Scholar] [CrossRef]
- Leventhal, H.; Diefenbach, M.; Leventhal, E.A. Illness cognition: Using common sense to understand treatment adherence and affect cognition interactions. Cogn. Ther. Res. 1992, 16, 143–163. [Google Scholar] [CrossRef]
| Participant | Age (Year) | Marital Status | Education Level | Occupation | Economic Status (Self-Report) | Gleason Score /ISUP 1 Grade | Treatment | Time Passed from Cancer Treatment (Months) |
|---|---|---|---|---|---|---|---|---|
| 1 | 62 | Married | Under diploma | Employed | Relatively sufficient | 8/4 | RT 2 + CT 3 | 2 |
| 2 | 56 | Married | Academic | Retired | Relatively sufficient | 4 + 3/3 | RP 4 | 24 |
| 3 | 70 | Married | Under diploma | Retired | Relatively sufficient | 4 + 3/3 | RP | 19 |
| 4 | 57 | Married | Diploma | Employed | Not sufficient | 3 + 4/2 | RP | 6 |
| 5 | 73 | Married | Diploma | Employed | Not sufficient | 6/1 | RP | 20 |
| 6 | 53 | Married | Under diploma | Employed | Sufficient | 4 + 3/3 | RP | 8 |
| 7 | 64 | Married | Academic | Retired | Sufficient | 3 + 4/2 | RP | 22 |
| 8 | 73 | Married | Academic | Retired | Sufficient | 8/4 | RP | 16 |
| 9 | 62 | Married | Diploma | Employed | Not sufficient | 4 + 3/3 | RP | 17 |
| 10 | 58 | Married | Illiterate | Retired | Relatively sufficient | 4 + 3/3 | RP | 15 |
| 11 | 61 | Married | Academic | Retired | Sufficient | 3 + 4/2 | RP | 14 |
| 12 | 67 | Married | Under diploma | Retired | Sufficient | 4 + 3/3 | RP + HT 5 | 13 |
| 13 | 48 | Married | Academic | Employed | Not sufficient | 8/4 | RT + RT + HT | 23 |
| Subcategory | Category | Theme |
|---|---|---|
| Fear of incomplete cure | Living with insecurity |
| Fear of cancer return | |
| Psychological strategies | Struggling to cope |
| Spiritual coping | |
| Seeking health | Trying to prevent cancer recurrence |
| Lifestyle modification |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mardani, A.; Farahani, M.A.; Khachian, A.; Vaismoradi, M. Fear of Cancer Recurrence and Coping Strategies among Prostate Cancer Survivors: A Qualitative Study. Curr. Oncol. 2023, 30, 6720-6733. https://doi.org/10.3390/curroncol30070493
Mardani A, Farahani MA, Khachian A, Vaismoradi M. Fear of Cancer Recurrence and Coping Strategies among Prostate Cancer Survivors: A Qualitative Study. Current Oncology. 2023; 30(7):6720-6733. https://doi.org/10.3390/curroncol30070493
Chicago/Turabian StyleMardani, Abbas, Mansoureh Ashghali Farahani, Alice Khachian, and Mojtaba Vaismoradi. 2023. "Fear of Cancer Recurrence and Coping Strategies among Prostate Cancer Survivors: A Qualitative Study" Current Oncology 30, no. 7: 6720-6733. https://doi.org/10.3390/curroncol30070493
APA StyleMardani, A., Farahani, M. A., Khachian, A., & Vaismoradi, M. (2023). Fear of Cancer Recurrence and Coping Strategies among Prostate Cancer Survivors: A Qualitative Study. Current Oncology, 30(7), 6720-6733. https://doi.org/10.3390/curroncol30070493







