Is It Safe to Switch from a Standard Anterior to Retzius-Sparing Approach in Robot-Assisted Radical Prostatectomy?
Abstract
1. Introduction
2. Materials and Methods
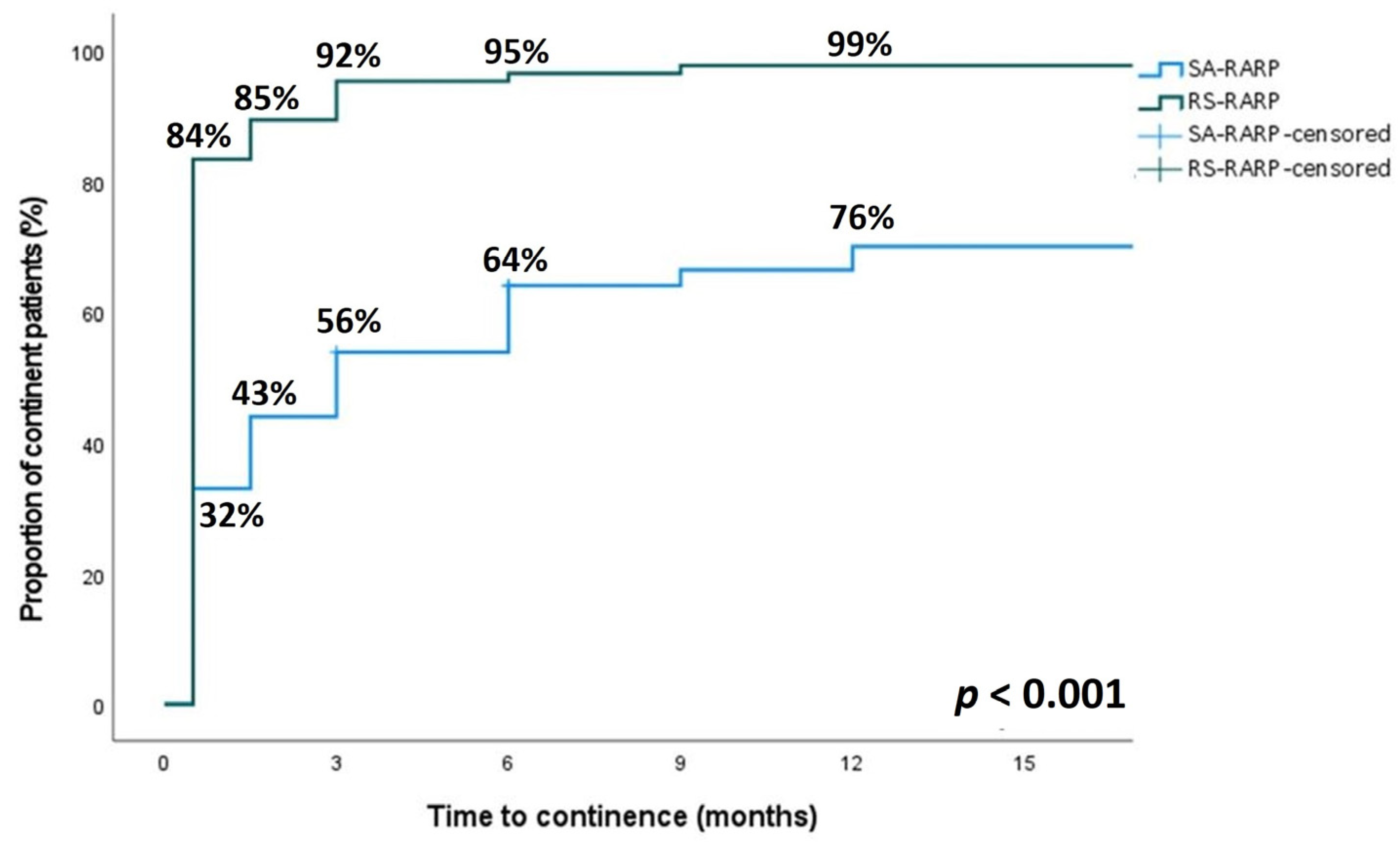
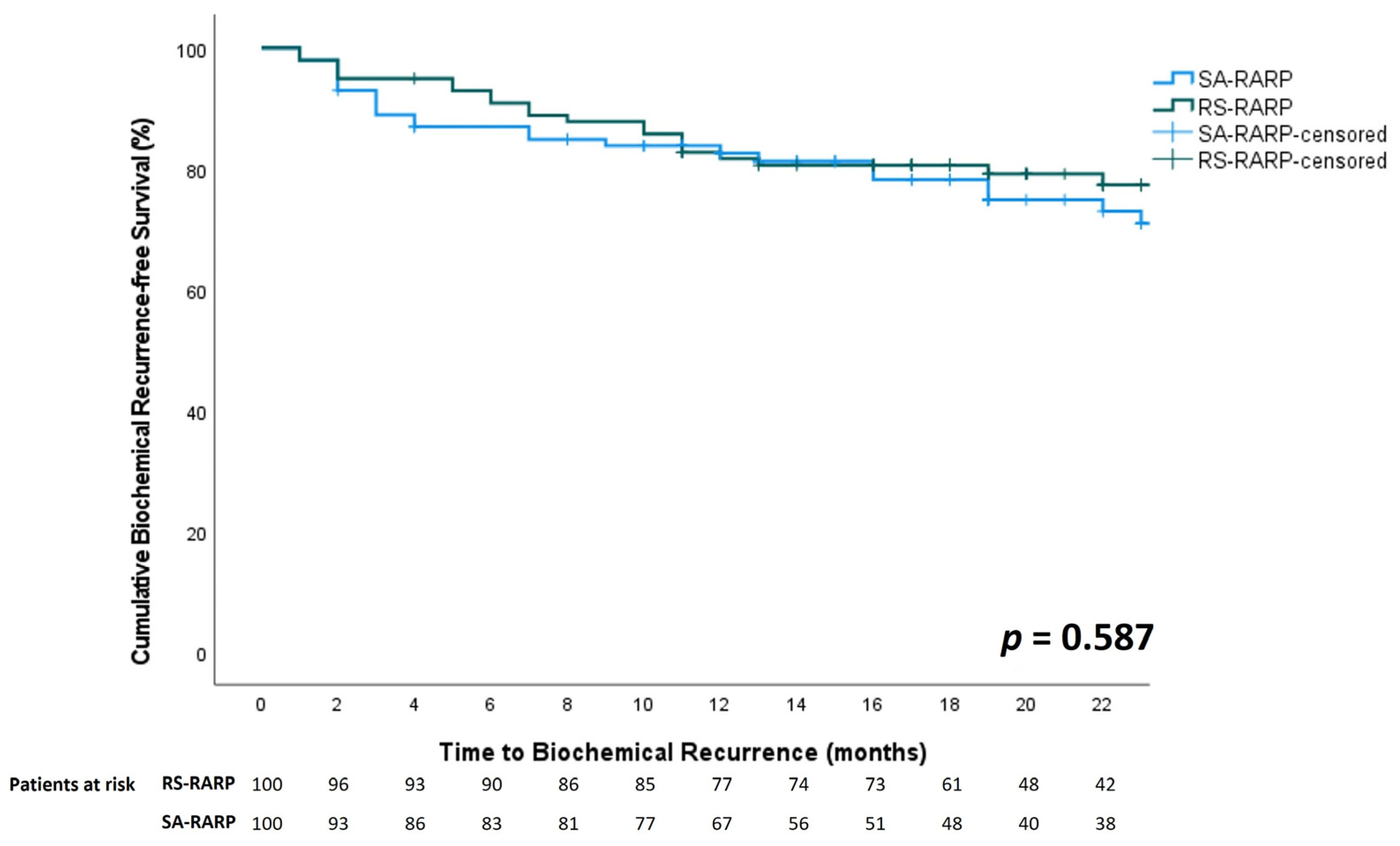
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Ilic, D.; Evans, S.M.; Allan, C.A.; Jung, J.H.; Murphy, D.; Frydenberg, M. Laparoscopic and Robotic-Assisted versus Open Radical Prostatectomy for the Treatment of Localised Prostate Cancer. Cochrane Database Syst. Rev. 2017, 9, CD009625. [Google Scholar] [CrossRef] [PubMed]
- Zahid, A.; Ayyan, M.; Farooq, M.; Cheema, H.A.; Shahid, A.; Naeem, F.; Ilyas, M.A.; Sohail, S. Robotic Surgery in Comparison to the Open and Laparoscopic Approaches in the Field of Urology: A Systematic Review. J. Robot. Surg. 2022, 17, 11–29. [Google Scholar] [CrossRef] [PubMed]
- Menon, M.; Shrivastava, A.; Bhandari, M.; Satyanarayana, R.; Siva, S.; Agarwal, P.K. Vattikuti Institute Prostatectomy: Technical Modifications in 2009. Eur. Urol. 2009, 56, 89–96. [Google Scholar] [CrossRef]
- Galfano, A.; Ascione, A.; Grimaldi, S.; Petralia, G.; Strada, E.; Bocciardi, A.M. A New Anatomic Approach for Robot-Assisted Laparoscopic Prostatectomy: A Feasibility Study for Completely Intrafascial Surgery. Eur. Urol. 2010, 58, 457–461. [Google Scholar] [CrossRef]
- Galfano, A.; Secco, S.; Dell’Oglio, P.; Rha, K.; Eden, C.; Fransis, K.; Sooriakumaran, P.; De La Muela, P.S.; Kowalczyk, K.; Miyagawa, T.; et al. Retzius-Sparing Robot-Assisted Radical Prostatectomy: Early Learning Curve Experience in Three Continents. BJU Int. 2021, 127, 412–417. [Google Scholar] [CrossRef]
- Asimakopoulos, A.D.; Topazio, L.; De Angelis, M.; Agrò, E.F.; Pastore, A.L.; Fuschi, A.; Annino, F. Retzius-Sparing versus Standard Robot-Assisted Radical Prostatectomy: A Prospective Randomized Comparison on Immediate Continence Rates. Surg. Endosc. 2019, 33, 2187–2196. [Google Scholar] [CrossRef]
- Umari, P.; Eden, C.; Cahill, D.; Rizzo, M.; Eden, D.; Sooriakumaran, P. Retzius-Sparing versus Standard Robot-Assisted Radical Prostatectomy: A Comparative Prospective Study of Nearly 500 Patients. J. Urol. 2021, 205, 780–790. [Google Scholar] [CrossRef]
- Menon, M.; Dalela, D.; Jamil, M.; Diaz, M.; Tallman, C.; Abdollah, F.; Sood, A.; Lehtola, L.; Miller, D.; Jeong, W. Functional Recovery, Oncologic Outcomes and Postoperative Complications after Robot-Assisted Radical Prostatectomy: An Evidence-Based Analysis Comparing the Retzius Sparing and Standard Approaches. J. Urol. 2018, 199, 1210–1217. [Google Scholar] [CrossRef]
- Rosenberg, J.E.; Jung, J.H.; Edgerton, Z.; Lee, H.; Lee, S.; Bakker, C.J.; Dahm, P. Retzius-Sparing versus Standard Robot-Assisted Laparoscopic Prostatectomy for the Treatment of Clinically Localized Prostate Cancer. BJU Int. 2021, 128, 12–20. [Google Scholar] [CrossRef]
- Lumen, N.; Lambert, E.; Poelaert, F.; Wirtz, M.; Verbeke, S.; Van Praet, C. Retzius-Sparing Robot-Assisted Radical Prostatectomy. J. Vis. Exp. 2022, 183, e63592. [Google Scholar] [CrossRef]
- Bianchi, L.; Turri, F.M.; Larcher, A.; De Groote, R.; De Bruyne, P.; De Coninck, V.; Goossens, M.; D’Hondt, F.; De Naeyer, G.; Schatteman, P.; et al. A Novel Approach for Apical Dissection During Robot-Assisted Radical Prostatectomy: The “Collar” Technique. Eur. Urol. Focus 2018, 4, 677–685. [Google Scholar] [CrossRef]
- Clavien, P.A.; Barkun, J.; de Oliveira, M.L.; Vauthey, J.N.; Dindo, D.; Schulick, R.D.; de Santibañes, E.; Pekolj, J.; Slankamenac, K.; Bassi, C.; et al. The Clavien-Dindo Classification of Surgical Complications. Ann. Surg. 2009, 250, 187–196. [Google Scholar] [CrossRef]
- Barakat, B.; Othman, H.; Gauger, U.; Wolff, I.; Hadaschik, B.; Rehme, C. Retzius Sparing Radical Prostatectomy Versus Robot-Assisted Radical Prostatectomy: Which Technique Is More Beneficial for Prostate Cancer Patients (MASTER Study)? A Systematic Review and Meta-Analysis. Eur. Urol. Focus 2022, 8, 1060–1071. [Google Scholar] [CrossRef] [PubMed]
- Galfano, A.; Di Trapani, D.; Sozzi, F.; Strada, E.; Petralia, G.; Bramerio, M.; Ascione, A.; Gambacorta, M.; Bocciardi, A.M. Beyond the Learning Curve of the Retzius-Sparing Approach for Robot-Assisted Laparoscopic Radical Prostatectomy: Oncologic and Functional Results of the First 200 Patients with ≥1 Year of Follow-Up. Eur. Urol. 2013, 64, 974–980. [Google Scholar] [CrossRef]
- Umari, P.; Fossati, N.; Gandaglia, G.; Pokorny, M.; De Groote, R.; Geurts, N.; Goossens, M.; Schatterman, P.; De Naeyer, G.; Mottrie, A. Robotic Assisted Simple Prostatectomy versus Holmium Laser Enucleation of the Prostate for Lower Urinary Tract Symptoms in Patients with Large Volume Prostate: A Comparative Analysis from a High Volume Center. J. Urol. 2017, 197, 1108–1114. [Google Scholar] [CrossRef]
- Qiu, X.; Li, Y.; Chen, M.; Xu, L.; Guo, S.; Marra, G.; Elliot Rosenberg, J.; Ma, H.; Li, X.; Guo, H. Retzius-Sparing Robot-Assisted Radical Prostatectomy Improves Early Recovery of Urinary Continence: A Randomized, Controlled, Single-Blind Trial with a 1-Year Follow-Up. BJU Int. 2020, 126, 633–640. [Google Scholar] [CrossRef] [PubMed]
- Lim, S.K.; Kim, K.H.; Shin, T.Y.; Han, W.K.; Chung, B.H.; Hong, S.J.; Choi, Y.D.; Rha, K.H. Retzius-Sparing Robot-Assisted Laparoscopic Radical Prostatectomy: Combining the Best of Retropubic and Perineal Approaches. BJU Int. 2014, 114, 236–244. [Google Scholar] [CrossRef] [PubMed]
- Dalela, D.; Jeong, W.; Prasad, M.A.; Sood, A.; Abdollah, F.; Diaz, M.; Karabon, P.; Sammon, J.; Jamil, M.; Baize, B.; et al. A Pragmatic Randomized Controlled Trial Examining the Impact of the Retzius-Sparing Approach on Early Urinary Continence Recovery After Robot-Assisted Radical Prostatectomy. Eur. Urol. 2017, 72, 677–685. [Google Scholar] [CrossRef]
- Sayyid, R.K.; Simpson, W.G.; Lu, C.; Terris, M.K.; Klaassen, Z.; Madi, R. Retzius-Sparing Robotic-Assisted Laparoscopic Radical Prostatectomy: A Safe Surgical Technique with Superior Continence Outcomes. J. Endourol. 2017, 31, 1244–1250. [Google Scholar] [CrossRef]
- Egan, J.; Marhamati, S.; Carvalho, F.L.F.; Davis, M.; O’Neill, J.; Lee, H.; Lynch, J.H.; Hankins, R.A.; Hu, J.C.; Kowalczyk, K.J. Retzius-Sparing Robot-Assisted Radical Prostatectomy Leads to Durable Improvement in Urinary Function and Quality of Life Versus Standard Robot-Assisted Radical Prostatectomy Without Compromise on Oncologic Efficacy: Single-Surgeon Series and Step-by-Step. Eur. Urol. 2021, 79, 839–857. [Google Scholar] [CrossRef] [PubMed]
- Stonier, T.; Simson, N.; Davis, J.; Challacombe, B. Retzius-Sparing Robot-Assisted Radical Prostatectomy (RS-RARP) vs Standard RARP: It’s Time for Critical Appraisal. BJU Int. 2019, 123, 5–7. [Google Scholar] [CrossRef]
- Chang, L.-W.; Hung, S.-C.; Hu, J.-C.; Chiu, K.-Y. Retzius-Sparing Robotic-Assisted Radical Prostatectomy Associated with Less Bladder Neck Descent and Better Early Continence Outcome. Anticancer Res. 2018, 38, 345–351. [Google Scholar] [CrossRef]
- Abdel Raheem, A.; Hagras, A.; Ghaith, A.; Alenzi, M.J.; Elghiaty, A.; Gameel, T.; Alowidah, I.; Ham, W.S.; Choi, Y.D.; El-Bahnasy, A.H.; et al. Retzius-Sparing Robot-Assisted Radical Prostatectomy versus Open Retropubic Radical Prostatectomy: A Prospective Comparative Study with 19-Month Follow-Up. Minerva Urol. Nefrol. 2020, 72, 586–594. [Google Scholar] [CrossRef]
- Nyberg, M.; Sjoberg, D.D.; Carlsson, S.V.; Wilderäng, U.; Carlsson, S.; Stranne, J.; Wiklund, P.; Steineck, G.; Haglind, E.; Hugosson, J.; et al. Surgeon Heterogeneity Significantly Affects Functional and Oncological Outcomes after Radical Prostatectomy in the Swedish LAPPRO Trial. BJU Int. 2021, 127, 361–368. [Google Scholar] [CrossRef] [PubMed]
- Lantz, A.; Bock, D.; Akre, O.; Angenete, E.; Bjartell, A.; Carlsson, S.; Modig, K.K.; Nyberg, M.; Kollberg, K.S.; Steineck, G.; et al. Functional and Oncological Outcomes After Open Versus Robot-Assisted Laparoscopic Radical Prostatectomy for Localised Prostate Cancer: 8-Year Follow-Up. Eur. Urol. 2021, 80, 650–660. [Google Scholar] [CrossRef] [PubMed]
- Phukan, C.; Mclean, A.; Nambiar, A.; Mukherjee, A.; Somani, B.; Krishnamoorthy, R.; Sridhar, A.; Rajan, P.; Sooriakumaran, P.; Rai, B.P. Retzius Sparing Robotic Assisted Radical Prostatectomy vs. Conventional Robotic Assisted Radical Prostatectomy: A Systematic Review and Meta-Analysis. World J. Urol. 2020, 38, 1123–1134. [Google Scholar] [CrossRef]
- Checcucci, E.; Veccia, A.; Fiori, C.; Amparore, D.; Manfredi, M.; Di Dio, M.; Morra, I.; Galfano, A.; Autorino, R.; Bocciardi, A.M.; et al. Retzius-Sparing Robot-Assisted Radical Prostatectomy vs the Standard Approach: A Systematic Review and Analysis of Comparative Outcomes. BJU Int. 2020, 125, 8–16. [Google Scholar] [CrossRef]
- Tai, T.E.; Wu, C.C.; Kang, Y.N.; Wu, J.C. Effects of Retzius Sparing on Robot-Assisted Laparoscopic Prostatectomy: A Systematic Review with Meta-Analysis. Surg. Endosc. 2020, 34, 4020–4029. [Google Scholar] [CrossRef]
- Abdel Raheem, A.; Chang, K.D.; Alenzi, M.J.; Ham, W.S.; Han, W.K.; Choi, Y.D.; Rha, K.H. Predictors of Biochemical Recurrence after Retzius-Sparing Robot-Assisted Radical Prostatectomy: Analysis of 359 Cases with a Median Follow-up Period of 26 Months. Int. J. Urol. 2018, 25, 1006–1014. [Google Scholar] [CrossRef]
- Menon, M.; Bhandari, M.; Gupta, N.; Lane, Z.; Peabody, J.O.; Rogers, C.G.; Sammon, J.; Siddiqui, S.A.; Diaz, M. Biochemical Recurrence Following Robot-Assisted Radical Prostatectomy: Analysis of 1384 Patients with a Median 5-Year Follow-Up. Eur. Urol. 2010, 58, 838–846. [Google Scholar] [CrossRef]
- Galfano, A.; Tappero, S.; Eden, C.; Dell’Oglio, P.; Fransis, K.; Guo, H.; Kowalczyk, K.; Longoni, M.; Madi, R.; Rha, K.H.; et al. Multicentric Experience in Retzius-Sparing Robot-Assisted Radical Prostatectomy Performed by Expert Surgeons for High-Risk Prostate Cancer. Minerva Urol. Nephrol. 2022, 74, 607–614. [Google Scholar] [CrossRef]
- Lee, J.; Kim, H.Y.; Goh, H.J.; Heo, J.E.; Almujalhem, A.; Alqahtani, A.A.; Chung, D.Y.; Chang, K.; Choi, Y.D.; Rha, K.H. Retzius Sparing Robot-Assisted Radical Prostatectomy Conveys Early Regain of Continence over Conventional Robot-Assisted Radical Prostatectomy: A Propensity Score Matched Analysis of 1,863 Patients. J. Urol. 2020, 203, 137–144. [Google Scholar] [CrossRef] [PubMed]
- Anil, H.; Karamik, K.; Yildiz, A.; Savaş, M. Does Transition from Standard to Retzius-Sparing Technique in Robot-Assisted Radical Prostatectomy Affect the Functional and Oncological Outcomes? Arch. Ital. Urol. Androl. 2021, 93, 399–403. [Google Scholar] [CrossRef] [PubMed]
- Kates, M.; Sopko, N.A.; Han, M.; Partin, A.W.; Epstein, J.I. Importance of Reporting the Gleason Score at the Positive Surgical Margin Site: Analysis of 4,082 Consecutive Radical Prostatectomy Cases. J. Urol. 2016, 195, 337–342. [Google Scholar] [CrossRef] [PubMed]
| SA-RARP (N = 100) | RS-RARP (N = 100) | p | ||
|---|---|---|---|---|
| Age (years) | 67 (62–73) | 66 (61–70) | 0.166 | |
| BMI (kg/m²) | 26.3 (24.1–28.5) | 26.3 (24.3–29.0) | 0.713 | |
| ASA-score | 2 (2–2) | 2 (2–2) | 0.766 | |
| Prostate volume (mL) | 45 (34–56) | 44 (34–65) | 0.756 | |
| PSA (ng/mL) | 8.62 (6.16–10.79) | 7.38 (5.37–10.60) | 0.09 | |
| Previous prostate surgery | 0.009 | |||
| None | 91 (91%) | 100 (100%) | ||
| TURP | 8 (8%) | 0 (0%) | ||
| Other | 1 (1%) | 0 (0%) | ||
| Biopsy ISUP Grade Group | 0.176 | |||
| 1 | 18 (18%) | 15 (15%) | ||
| 2 | 35 (35%) | 34 (34%) | ||
| 3 | 19 (19%) | 32 (32%) | ||
| 4 | 15 (15%) | 13 (13%) | ||
| 5 | 13 (13%) | 6 (6%) | ||
| cT | 0.005 | |||
| T1c | 26 (26%) | 39 (39%) | ||
| T2 | 30 (30%) | 29 (29%) | ||
| T3 | 3 (3%) | 12 (12%) | ||
| T4 | 1 (1%) | 0 (0%) | ||
| Missing | 39 (39%) | 18 (18%) | ||
| cN | 0.32 | |||
| N0 | 94 (94%) | 98 (98%) | ||
| N1 | 3 (3%) | 2 (2%) | ||
| Nx | 2 (2%) | 0 (0%) | ||
| Missing | 1 (1%) | 0 (0%) | ||
| cM | 0.059 | |||
| M0 | 66 (66%) | 78 (78%) | ||
| Mx | 34 (34%) | 22 (22%) | ||
| MRI | 0.063 | |||
| PIRADS 1–2 | 4 (4%) | 9 (9%) | ||
| PIRADS 3 | 12 (12%) | 13 (13%) | ||
| PIRADS 4–5 | 78 (78%) | 77 (77%) | ||
| Not performed/Missing | 6 (6%) | 1 (1%) | ||
| iT | 0.155 | |||
| T2 | 70 (70%) | 63 (63%) | ||
| T3 | 18 (18%) | 26 (26%) | ||
| No tumor | 4 (4%) | 10 (10%) | ||
| Not performed/missing | 8 (8%) | 1 (1%) | ||
| Index Lesion Location | <0.001 | |||
| Peripheral zone | 63 (63%) | 83 (83%) | ||
| Anterior zone | 20 (20%) | 4 (4%) | ||
| Multifocal (anterior and posterior) | 5 (5%) | 2 (2%) | ||
| No MRI or no index lesion | 12 (12%) | 11 (11%) | ||
| SA-RARP (N = 100) | RS-RARP (N = 100) | p | ||
|---|---|---|---|---|
| Surgeon | <0.001 | |||
| NL | 96 (96%) | 71 (71%) | ||
| CVP | 4 (4%) | 28 (28%) | ||
| Missing | 0 (0%) | 1 (1%) | ||
| Operative time (mins) | 147.5 (125–175) | 160 (145–180) | 0.005 | |
| Estimated blood loss (mL) | 400 (150–400) | 225 (100–300) | 0.096 | |
| Positive lymph nodes | 0 (0–0) | 0 (0–0) | <0.001 | |
| Nerve-sparing (%) | 0.005 | |||
| None | 9 (9%) | 6 (6%) | ||
| Unilateral | 22 (22%) | 43 (43%) | ||
| Bilateral | 69 (69%) | 50 (50%) | ||
| Missing | 0 (0%) | 1 (1%) | ||
| Intraoperative leak test | 0.028 | |||
| No leakage | 93 (93%) | 82 (82%) | ||
| Leakage | 7 (7%) | 17 (17%) | ||
| Missing | 0 (0%) | 1 (1%) | ||
| Duration of urinary catheter stay (days) | 3 (3–3) | 3 (3–3) | 0.382 | |
| Length of stay (days) | 3 (3–3) | 3 (3–3) | 0.268 | |
| Clavien-Dindo | SA-RARP (N = 100) | RS-RARP (N = 100) | p | |||
|---|---|---|---|---|---|---|
| 0 | 79 | 88 | 0.028 | |||
| 1 | 12 | Urinary retention (11) Abdominal wall hematoma (1) | 9 | Urinary retention (7) Prolonged suprapubic pain (1) Prolonged hematuria (1) | ||
| 2 | 9 | Wound infection (1) Urinary tract infection (7) Anastomotic leakage (1) | 1 | Infected lymfocele (1) | ||
| 3A | 0 | 1 | Infected lymfocele (1) | 0.292 | ||
| 3B | 4 | Cholecystitis (1) Hemoperitoneum (1) Anastomotic leakage (1) Obstructive pyelonephritis (1) | 1 | Gastrointestinal obstruction (1) | ||
| 4A | 1 | Hypovolemic shock (1) | 0 | |||
| 4B | 1 | Urosepsis (1) | 0 | |||
| SA-RARP (N = 100) | RS-RARP (N = 100) | p | |||
|---|---|---|---|---|---|
| Preoperative potency (N = 200) | <0.001 | ||||
| Impotent | 31 (31%) | 27 (27%) | |||
| Potent | 48 (48%) | 63 (63%) | |||
| Missing | 21 (21%) | 9 (9%) | |||
| Postoperative potency in preoperatively potent men (N = 111) | 0.608 | ||||
| Impotent | 21 (44%) | 25 (40%) | |||
| Potent | 25 (52%) | 37 (59%) | |||
| Missing | 2 (4%) | 1 (1%) | |||
| Pathology T stage | 0.38 | ||||
| T2 | 52 (52%) | 51 (51%) | |||
| T3a | 32 (32%) | 38 (38%) | |||
| T3b | 16 (16%) | 10 (10%) | |||
| Missing | 0 (0%) | 1 (1%) | |||
| Pathology N stage | <0.001 | ||||
| pN0 | 49 (49%) | 34 (34%) | |||
| pN1 | 10 (10%) | 0 (0%) | |||
| pNx | 41 (41%) | 65 (65%) | |||
| Missing | 0 (0%) | 1 (1%) | |||
| Pathology ISUP Grade Group | 0.344 | ||||
| 1 | 5 (5%) | 5 (5%) | |||
| 2 | 43 (43%) | 41 (41%) | |||
| 3 | 24 (24%) | 34 (34%) | |||
| 4 | 13 (13%) | 6 (6%) | |||
| 5 | 15 (15%) | 13 (13%) | |||
| Missing | 0 (0%) | 1 (1%) | |||
| Surgical margins | |||||
| T2 | R0 | 44 (84.6%) | 39 (76.5%) | 0.329 | |
| R1 | 8 (15.4%) | 12 (23.5%) | |||
| T3 | R0 | 27 (56.3%) | 17 (35.4%) | 0.041 | |
| R1 | 21 (43.8%) | 31 (64.6%) | |||
| Overall | R0 | 71 (71%) | 56 (56%) | 0.034 | |
| R1 | 29 (29%) | 43 (43%) | |||
| Missing | 0 (0%) | 1 (1%) | |||
| Patients with undetectable PSA at 3 months postoperatively (ng/mL) | 85 (85%) | 85 (85%) | 1.000 | ||
| Biochemical recurrence | 0.540 | ||||
| No | 73 (73%) | 76 (76%) | |||
| Yes | 27 (27%) | 23 (23%) | |||
| Missing | 0 (0%) | 1 (1%) | |||
| Postoperative radiotherapy | 0.605 | ||||
| No | 77 (77%) | 78 (78%) | |||
| Adjuvant | 1 (1%) | 0 (0%) | |||
| Salvage | 21 (21%) | 21 (21%) | |||
| Missing | 1 (1%) | 1 (1%) | |||
| Development of metastatic PCa | 2 (2%) | 0 (0%) | 0.157 | ||
| Follow-up (months) | 24.5 (17–35) | 22 (18–27) | 0.008 | ||
| Variable | Odds Ratio | 95% CI | p | |
|---|---|---|---|---|
| Univariate Logistic Regression | ||||
| iPSA | 1.14 | 1.03–1.26 | 0.011 | |
| pT | ||||
| pT2 | Ref | |||
| pT3 | 19.06 | 4.15–87.53 | <0.001 | |
| Lymphovascular invasion | ||||
| No | Ref | |||
| Yes | 11.25 | 1.11–114.05 | 0.041 | |
| Surgical margin status | ||||
| R0 | Ref | |||
| R1 | 3.21 | 1.21–8.53 | 0.019 | |
| ISUP Grade Group | ||||
| 1 | Ref | |||
| 2–3 | 3.39 × 108 | / | 1.00 | |
| 4–5 | 1.79 × 109 | / | 1.00 | |
| Multivariate Logistic Regression | ||||
| iPSA | 1.13 | 1.00–1.28 | 0.054 | |
| pT | ||||
| pT2 | Ref | |||
| pT3 | 14.99 | 2.77–81.11 | 0.002 | |
| Lymphovascular invasion | ||||
| No | Ref | |||
| Yes | 13.52 | 0.85–216.28 | 0.066 | |
| Surgical margin status | ||||
| R0 | Ref | |||
| R1 | 2.05 | 0.56–7.54 | 0.281 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lambert, E.; Allaeys, C.; Berquin, C.; De Visschere, P.; Verbeke, S.; Vanneste, B.; Fonteyne, V.; Van Praet, C.; Lumen, N. Is It Safe to Switch from a Standard Anterior to Retzius-Sparing Approach in Robot-Assisted Radical Prostatectomy? Curr. Oncol. 2023, 30, 3447-3460. https://doi.org/10.3390/curroncol30030261
Lambert E, Allaeys C, Berquin C, De Visschere P, Verbeke S, Vanneste B, Fonteyne V, Van Praet C, Lumen N. Is It Safe to Switch from a Standard Anterior to Retzius-Sparing Approach in Robot-Assisted Radical Prostatectomy? Current Oncology. 2023; 30(3):3447-3460. https://doi.org/10.3390/curroncol30030261
Chicago/Turabian StyleLambert, Edward, Charlotte Allaeys, Camille Berquin, Pieter De Visschere, Sofie Verbeke, Ben Vanneste, Valerie Fonteyne, Charles Van Praet, and Nicolaas Lumen. 2023. "Is It Safe to Switch from a Standard Anterior to Retzius-Sparing Approach in Robot-Assisted Radical Prostatectomy?" Current Oncology 30, no. 3: 3447-3460. https://doi.org/10.3390/curroncol30030261
APA StyleLambert, E., Allaeys, C., Berquin, C., De Visschere, P., Verbeke, S., Vanneste, B., Fonteyne, V., Van Praet, C., & Lumen, N. (2023). Is It Safe to Switch from a Standard Anterior to Retzius-Sparing Approach in Robot-Assisted Radical Prostatectomy? Current Oncology, 30(3), 3447-3460. https://doi.org/10.3390/curroncol30030261





