Immune Checkpoint Inhibitors-Associated Thrombosis: Incidence, Risk Factors and Management
Abstract
1. Introduction
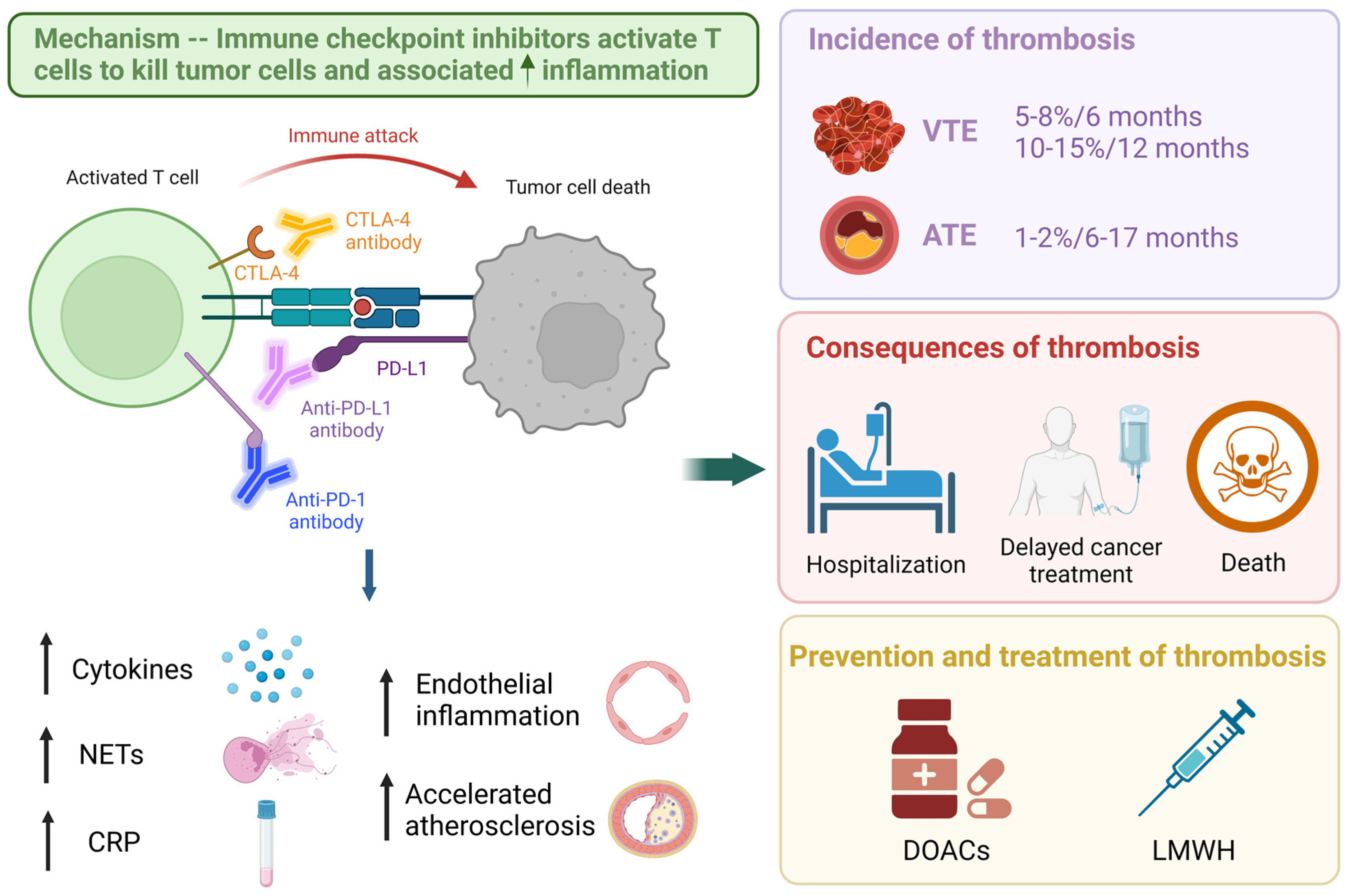
2. Mechanism of Thrombosis and Immunotherapy
3. Incidence of Thrombosis in Patients Receiving Immune Checkpoint Inhibitors
4. Biomarkers for Thrombosis in Patients on Immune Checkpoint Inhibitors
5. Risk Factors of Thrombosis in Patients on Immune Checkpoint Inhibitors
6. Consequences of Thrombosis in Patients on Immune Checkpoint Inhibitors
7. Prevention and Treatment of Thrombosis in Patients on Immune Checkpoint Inhibitors
8. Anticoagulation and Cancer Survival
9. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Haslam, A.; Prasad, V. Estimation of the Percentage of US Patients With Cancer Who Are Eligible for and Respond to Checkpoint Inhibitor Immunotherapy Drugs. JAMA Netw. Open. 2019, 2, e192535. [Google Scholar] [CrossRef] [PubMed]
- Himmel, M.E.; Saibil, S.D.; Saltman, A.P. Immune checkpoint inhibitors in cancer immunotherapy. CMAJ 2020, 192, E651. [Google Scholar] [CrossRef] [PubMed]
- Lyman, G.H.; Eckert, L.; Wang, Y.; Wang, H.; Cohen, A. Venous thromboembolism risk in patients with cancer receiving chemotherapy: A real-world analysis. Oncologists 2013, 18, 1321–1329. [Google Scholar] [CrossRef]
- Khorana, A.A.; Francis, C.W.; Culakova, E.; Kuderer, N.M.; Lyman, G.H. Thromboembolism is a leading cause of death in cancer patients receiving outpatient chemotherapy. J. Thromb. Haemost. 2007, 5, 632–634. [Google Scholar] [CrossRef]
- Lloyd, A.J.; Dewilde, S.; Noble, S.; Reimer, E.; Lee, A.Y.Y. What Impact Does Venous Thromboembolism and Bleeding Have on Cancer Patients’ Quality of Life? Value Health 2018, 21, 449–455. [Google Scholar] [CrossRef] [PubMed]
- Noble, S.; Nelson, A.; Scott, J.; Berger, A.; Schmidt, K.; Swarnkar, P.; Lee, A. Patient Experience of Living With Cancer-Associated Thrombosis in Canada (PELICANADA). Res. Pract. Thromb. Haemost. 2020, 4, 154–160. [Google Scholar] [CrossRef] [PubMed]
- Font, C.; Nelson, A.; Garcia-Fernandez, T.; Prout, H.; Gee, P.; Noble, S. Patients’ Experience of Living with Cancer-associated thrombosis in Spain (PELICANOS). Support Care Cancer 2018, 26, 3233–3239. [Google Scholar] [CrossRef]
- Wang, T.-F.; Khorana, A.A.; Carrier, M. Thrombotic Complications Associated with Immune Checkpoint Inhibitors. Cancers 2021, 13, 4606. [Google Scholar] [CrossRef]
- Jackson, S.P.; Darbousset, R.; Schoenwaelder, S.M. Thromboinflammation: Challenges of therapeutically targeting coagulation and other host defense mechanisms. Blood 2019, 133, 906–918. [Google Scholar] [CrossRef]
- Kunimasa, K.; Nishino, K.; Kimura, M.; Inoue, T.; Tamiya, M.; Kumagai, T.; Imamura, F. Pembrolizumab-induced acute thrombosis: A case report. Medicine 2018, 97, e10772. [Google Scholar] [CrossRef] [PubMed]
- Cochain, C.; Chaudhari, S.M.; Koch, M.; Wiendl, H.; Eckstein, H.H.; Zernecke, A. Programmed cell death-1 deficiency exacerbates T cell activation and atherogenesis despite expansion of regulatory T cells in atherosclerosis-prone mice. PLoS ONE 2014, 9, e93280. [Google Scholar] [CrossRef]
- McCrae, K.R.; Swaidani, S.; Diaz-Montero, C.M.; Khorana, A.A. Old is new again: Emergence of thromboembolic complications in cancer patients on immunotherapy. Thromb. Res. 2022, 213, S51–S57. [Google Scholar] [CrossRef]
- Solinas, C.; Saba, L.; Sganzerla, P.; Petrelli, F. Venous and arterial thromboembolic events with immune checkpoint inhibitors: A systematic review. Thromb. Res. 2020, 196, 444–453. [Google Scholar] [CrossRef]
- Giustozzi, M.; Becattini, C.; Roila, F.; Agnelli, G.; Mandala, M. Vascular events with immune checkpoint inhibitors in melanoma or non-small cell lung cancer: A systematic review and meta-analysis. Cancer Treat Rev. 2021, 100, 102280. [Google Scholar] [CrossRef]
- Ma, Z.; Sun, X.; Zhang, Y.; Li, H.; Sun, D.; An, Z.; Zhang, Y. Risk of Thromboembolic Events in Cancer Patients Treated with Immune Checkpoint Inhibitors: A Meta-analysis of Randomized Controlled Trials. Thromb. Haemost. 2022, 122, 1757–1766. [Google Scholar] [CrossRef] [PubMed]
- Chiasakul, T.; Patell, R.; Maraveyas, A.; Carrier, M.; Zwicker, J.I. Discordant reporting of VTE in pancreatic cancer: A systematic review and meta-analysis of thromboprophylaxis versus chemotherapeutic trials. J. Thromb. Haemost. 2021, 19, 489–501. [Google Scholar] [CrossRef] [PubMed]
- Ay, C.; Dunkler, D.; Marosi, C.; Chiriac, A.-L.; Vormittag, R.; Simanek, R.; Quehenberger, P.; Zielinski, C.; Pabinger, I. Prediction of venous thromboembolism in cancer patients. Blood 2010, 116, 5377–5382. [Google Scholar] [CrossRef] [PubMed]
- Sheng, I.Y.; Gupta, S.; Reddy, C.A.; Angelini, D.; Funchain, P.; Sussman, T.A.; Sleiman, J.; Ornstein, M.C.; McCrae, K.; Khorana, A.A. Thromboembolism in Patients with Metastatic Renal Cell Carcinoma Treated with Immunotherapy. Target Oncol. 2021, 16, 813–821. [Google Scholar] [CrossRef]
- Sheng, I.Y.; Gupta, S.; Reddy, C.A.; Angelini, D.; Funchain, P.; Sussman, T.A.; Sleiman, J.; Ornstein, M.C.; McCrae, K.; Khorana, A.A. Thromboembolism in Patients with Metastatic Urothelial Cancer Treated with Immune Checkpoint Inhibitors. Target Oncol. 2022, 17, 563–569. [Google Scholar] [CrossRef]
- Hegde, A.M.; Stroud, C.R.; Cherry, C.R.; Yogarajah, M.; Cherukuri, S.D.; Walker, P.R. Incidence and impact of thromboembolic events in lung cancer patients treated with nivolumab. J. Clin. Oncol. 2017, 35 (Suppl. 15), e20624. [Google Scholar] [CrossRef]
- Ibrahimi, S.; Machiorlatti, M.; Vesely, S.K.; Malla, M.; Modhia, F.; Jones, S.A.; Cherry, M.A. Incidence of Vascular Thromboembolic Events in Patients Receiving Immunotherapy: A Single Institution Experience. Blood 2017, 130, 4864. [Google Scholar]
- Bar, J.; Markel, G.; Gottfried, T.; Percik, R.; Leibowitz-Amit, R.; Berger, R.; Golan, T.; Daher, S.; Taliansky, A.; Dudnik, E.; et al. Acute vascular events as a possibly related adverse event of immunotherapy: A single-institute retrospective study. Eur. J. Cancer 2019, 120, 122–131. [Google Scholar] [CrossRef]
- Nichetti, F.; Ligorio, F.; Zattarin, E.; Signorelli, D.; Prelaj, A.; Proto, C.; Galli, G.; Marra, A.; Apollonio, G.; Porcu, L.; et al. Is There an Interplay between Immune Checkpoint Inhibitors, Thromboprophylactic Treatments and Thromboembolic Events? Mechanisms and Impact in Non-Small Cell Lung Cancer Patients. Cancers 2019, 12, 67. [Google Scholar] [CrossRef]
- Ando, Y.; Hayashi, T.; Sugimoto, R.; Nishibe, S.; Ito, K.; Kawada, K.; Ikeda, Y.; Yamada, S.; Imaizumi, K. Risk factors for cancer-associated thrombosis in patients undergoing treatment with immune checkpoint inhibitors. Investig. New Drugs 2020, 38, 1200–1206. [Google Scholar] [CrossRef]
- Drobni, Z.D.; Alvi, R.M.; Taron, J.; Zafar, A.; Murphy, S.P.; Rambarat, P.K.; Mosarla, R.C.; Lee, C.; Zlotoff, D.A.; Raghu, V.K.; et al. Association Between Immune Checkpoint Inhibitors With Cardiovascular Events and Atherosclerotic Plaque. Circulation 2020, 142, 2299–2311. [Google Scholar] [CrossRef]
- Deschênes-Simard, X.; Richard, C.; Galland, L.; Blais, F.; Desilets, A.; Malo, J.; Cvetkovic, L.; Belkaid, W.; Elkrief, A.; Gagné, A.; et al. Venous thrombotic events in patients treated with immune checkpoint inhibitors for non-small cell lung cancer: A retrospective multicentric cohort study. Thromb. Res. 2021, 205, 29–39. [Google Scholar] [CrossRef]
- Gong, J.; Drobni, Z.D.; Alvi, R.M.; Murphy, S.P.; Sullivan, R.J.; Hartmann, S.E.; Gilman, H.K.; Lee, H.; Zubiri, L.; Raghu, V.K.; et al. Immune checkpoint inhibitors for cancer and venous thromboembolic events. Eur. J. Cancer 2021, 158, 99–110. [Google Scholar] [CrossRef] [PubMed]
- Gutierrez-Sainz, L.; Martinez-Marin, V.; Viñal, D.; Martinez-Perez, D.; Pedregosa, J.; Garcia-Cuesta, J.A.; Feliu, J. Incidence of venous thromboembolic events in cancer patients receiving immunotherapy: A single-institution experience. Clin. Transl. Oncol. Off. Publ. Fed. Span. Oncol. Soc. Natl. Cancer Inst. Mex. 2021, 23, 1245–1252. [Google Scholar] [CrossRef]
- Guven, D.C.; Aksun, M.S.; Sahin, T.K.; Aktepe, O.H.; Yildirim, H.C.; Taban, H.; Ceylan, F.; Kertmen, N.; Arik, Z.; Dizdar, O.; et al. Poorer baseline performance status is associated with increased thromboembolism risk in metastatic cancer patients treated with immunotherapy. Support. Care Cancer Off. J. Multinatl. Assoc. Support. Care Cancer 2021, 29, 5417–5423. [Google Scholar] [CrossRef] [PubMed]
- Haist, M.; Stege, H.; Pemler, S.; Heinz, J.; Fleischer, M.I.; Graf, C.; Ruf, W.; Loquai, C.; Grabbe, S. Anticoagulation with Factor Xa Inhibitors Is Associated with Improved Overall Response and Progression-Free Survival in Patients with Metastatic Malignant Melanoma Receiving Immune Checkpoint Inhibitors-A Retrospective, Real-World Cohort Study. Cancers 2021, 13, 5103. [Google Scholar] [CrossRef] [PubMed]
- Hill, H.; Robinson, M.; Lu, L.; Slaughter, D.; Amin, A.; Mileham, K.; Patel, J.N. Venous thromboembolism incidence and risk factors in non-small cell lung cancer patients receiving first-line systemic therapy. Thromb. Res. 2021, 208, 71–78. [Google Scholar] [CrossRef] [PubMed]
- Icht, O.; Darzi, N.; Shimony, S.; Jacobi, O.; Reinhorn, D.; Landman, Y.; Leader, A. Venous thromboembolism incidence and risk assessment in lung cancer patients treated with immune checkpoint inhibitors. J. Thromb. Haemost. 2021, 19, 1250–1258. [Google Scholar] [CrossRef] [PubMed]
- Kewan, T.; Ko, T.; Flores, M.; Sallam, Y.; Haddad, A.; Daw, H. Prognostic impact and risk factors of cancer-associated thrombosis events in stage-IV cancer patients treated with immune checkpoint inhibitors. Eur. J. Haematol. 2021, 106, 682–688. [Google Scholar] [CrossRef]
- Madison, C.J.; Melson, R.A.; Conlin, M.J.; Gundle, K.R.; Thompson, R.F.; Calverley, D.C. Thromboembolic risk in patients with lung cancer receiving systemic therapy. Br. J. Haematol. 2021, 194, 179–190. [Google Scholar] [CrossRef]
- Moik, F.; Chan, W.-S.E.; Wiedemann, S.; Hoeller, C.; Tuchmann, F.; Aretin, M.-B.; Fuereder, T.; Zöchbauer-Müller, S.; Preusser, M.; Pabinger, I.; et al. Incidence, risk factors, and outcomes of venous and arterial thromboembolism in immune checkpoint inhibitor therapy. Blood 2021, 137, 1669–1678. [Google Scholar] [CrossRef]
- Alma, S.; Eloi, D.; Léa, V.; Julie, C.; Valérie, M.; Pierre, G.; Hilgers, W.; Philippe, G.; Christine, Z.; Philippe, D. Incidence of venous thromboembolism and discriminating capacity of Khorana score in lung cancer patients treated with immune checkpoint inhibitors. J. Thromb. Thrombolysis 2022, 54, 287–294. [Google Scholar] [CrossRef]
- Bjørnhart, B.; Kristiansen, C.; Asmussen, J.; Hansen, K.H.; Wedervang, K.; Jørgensen, T.L.; Herrstedt, J.; Schytte, T. Clinical impact of venous thromboembolism in non-small cell lung cancer patients receiving immunotherapy. Thromb. Res. 2023, 221, 164–172. [Google Scholar] [CrossRef]
- Cánovas, M.S.; Garay, D.F.; Moran, L.O.; Pérez, J.R.; Rubio, C.M.G.; de Mena, M.L.; Portero, B.O.; Castro, J.B.; Lage, Y.; Lavin, D.C.; et al. Immune checkpoint inhibitors-associated thrombosis in patients with lung cancer and melanoma: A study of the Spanish society of medical oncology (SEOM) thrombosis and cancer group. Clin. Transl. Oncol. 2022, 24, 2010–2020. [Google Scholar] [CrossRef]
- Endo, S.; Honda, T.; Kawahara, T.; Sakakibara, R.; Mitsumura, T.; Okamoto, T.; Miyazaki, Y. Profile of metastatic lung cancer patients susceptible to development of thromboembolism during immunotherapy. Cancer Treat. Res. Commun. 2022, 31, 100547. [Google Scholar] [CrossRef] [PubMed]
- Khorana, A.; Palaia, J.; Rosenblatt, L.; Pisupati, R.; Huang, N.; Nguyen, C.; Barron, J.; Gallagher, K.; Bond, T.C. Venous thromboembolism incidence and risk factors associated with immune checkpoint inhibitors among patients with advanced non-small cell lung cancer. J. Immunother. Cancer 2023, 11, e006072. [Google Scholar] [CrossRef] [PubMed]
- May, S.B.; La, J.; Milner, E.; Riaz, N.; Amos, C.; Garcia, D.A.; Carrier, M.; Zakai, N.; Do, N.V.; Brophy, M.; et al. Venous Thromboembolism Risk in Cancer Patients Receiving First-Line Immune Checkpoint Inhibitor Vs. Chemotherapy. Blood 2022, 140, 7968–7970. [Google Scholar] [CrossRef]
- Sanfilippo, K.M.; Luo, S.; Lyman, G.H.; Calverley, D.C.; Kuderer, N. Identification of Risk Factors for and Development of a Predictive Model for Immunotherapy-Associated Venous Thromboembolism (VTE) in Patients with Non-Small Cell Lung Cancer. Blood 2022, 140, 2803–2804. [Google Scholar] [CrossRef]
- Mulder, F.I.; Horváth-Puhó, E.; van Es, N.; van Laarhoven, H.W.M.; Pedersen, L.; Moik, F.; Ay, C.; Büller, H.R.; Sørensen, H.T. Venous thromboembolism in cancer patients: A population-based cohort study. Blood 2021, 137, 1959–1969. [Google Scholar] [CrossRef] [PubMed]
- Moik, F.; Ay, C.; Horváth-Puhó, E.; Pabinger, I.; Mulder, F.I.; van Es, N.; Sørensen, H.T. Risk of Venous and Arterial Thromboembolic Events in Patients Receiving Targeted Anti-cancer Therapy–A Nationwide Cohort Study. Available online: https://abstracts.isth.org/abstract/risk-of-venous-and-arterial-thromboembolic-events-in-patients-receiving-targeted-anti-cancer-therapy-a-nationwide-cohort-study/ (accessed on 2 February 2023).
- Overvad, T.F.; Skjøth, F.; Piazza, G.; Noble, S.; Ording, A.G.; Larsen, T.B.; Nielsen, P.B. The Khorana score and venous and arterial thrombosis in patients with cancer treated with immune checkpoint inhibitors: A Danish cohort study. J. Thromb. Haemost. JTH 2022, 20, 2921–2929. [Google Scholar] [CrossRef]
- Sussman, T.A.; Li, H.; Hobbs, B.; Funchain, P.; McCrae, K.R.; Khorana, A.A. Incidence of thromboembolism in patients with melanoma on immune checkpoint inhibitor therapy and its adverse association with survival. J. Immunother. Cancer 2021, 9, e001719. [Google Scholar] [CrossRef] [PubMed]
- Roopkumar, J.; Swaidani, S.; Kim, A.S.; Thapa, B.; Gervaso, L.; Hobbs, B.P.; Wei, W.; Alban, T.J.; Funchain, P.; Kundu, S.; et al. Increased Incidence of Venous Thromboembolism with Cancer Immunotherapy. Medicine 2021, 2, 423–434. [Google Scholar] [CrossRef] [PubMed]
- Fukuda, S.; Saito, K.; Yasuda, Y.; Kijima, T.; Yoshida, S.; Yokoyama, M.; Ishioka, J.; Matsuoka, Y.; Kageyama, Y.; Fujii, Y. Impact of C-reactive protein flare-response on oncological outcomes in patients with metastatic renal cell carcinoma treated with nivolumab. J. Immunother. Cancer 2021, 9, e001564. [Google Scholar] [CrossRef] [PubMed]
- Klümper, N.; Saal, J.; Berner, F.; Lichtensteiger, C.; Wyss, N.; Heine, A.; Bauernfeind, F.G.; Ellinger, J.; Brossart, P.; Diem, S.; et al. C reactive protein flare predicts response to checkpoint inhibitor treatment in non-small cell lung cancer. J. Immunother Cancer 2022, 10, e004024. [Google Scholar] [CrossRef]
- Moik, F.; Riedl, J.; Barth, D.; Chan, W.-S.E.; Wiedemann, S.; Höller, C.; Fuereder, T.; Jost, P.; Pabinger, I.; Preusser, M.; et al. Early Dynamics of C-Reactive Protein Predict Risk of Venous Thromboembolism in Patients with Cancer Treated with Immune Checkpoint Inhibitors. Blood 2022, 140, 1250–1251. [Google Scholar] [CrossRef]
- Petricciuolo, S.; Delle Donne, M.G.; Aimo, A.; Chella, A.; De Caterina, R. Pre-treatment high-sensitivity troponin T for the short-term prediction of cardiac outcomes in patients on immune checkpoint inhibitors. Eur. J. Clin. Investig. 2021, 51, e13400. [Google Scholar] [CrossRef]
- Waissengein, B.; Abu Ata, B.; Merimsky, O.; Shamai, S.; Wolf, I.; Arnold, J.H.; Bar-On, T.; Banai, S.; Khoury, S.; Laufer-Perl, M. The predictive value of high sensitivity troponin measurements in patients treated with immune checkpoint inhibitors. Clin. Res. Cardiol. Off. J. Ger. Card. Soc. 2022. ahead of print. [Google Scholar] [CrossRef] [PubMed]
- Lyon, A.R.; López-Fernández, T.; Couch, L.S.; Asteggiano, R.; Aznar, M.C.; Bergler-Klein, J.; Zamorano, J.L. 2022 ESC Guidelines on cardio-oncology developed in collaboration with the European Hematology Association (EHA), the European Society for Therapeutic Radiology and Oncology (ESTRO) and the International Cardio-Oncology Society (IC-OS). Eur. Heart J. 2022, 43, 4229–4361. [Google Scholar] [CrossRef] [PubMed]
- Khorana, A.A.; Kuderer, N.M.; Culakova, E.; Lyman, G.H.; Francis, C.W. Development and validation of a predictive model for chemotherapy-associated thrombosis. Blood 2008, 111, 4902–4907. [Google Scholar] [CrossRef] [PubMed]
- Mulder, F.I.; Candeloro, M.; Kamphuisen, P.; Di Nisio, M.; Bossuyt, P.M.; Guman, N.; Smit, K.; Büller, H.R.; Van Es, N. The Khorana score for prediction of venous thromboembolism in cancer patients: A systematic review and meta-analysis. Haematologica 2019, 104, 1277–1287. [Google Scholar] [CrossRef] [PubMed]
- Carrier, M.; Abou-Nassar, K.; Mallick, R.; Tagalakis, V.; Shivakumar, S.; Schattner, A.; Kuruvilla, P.; Hill, D.; Spadafora, S.; Marquis, K.; et al. Apixaban to Prevent Venous Thromboembolism in Patients with Cancer. N. Engl. J. Med. 2019, 380, 711–719. [Google Scholar] [CrossRef] [PubMed]
- Khorana, A.A.; Soff, G.A.; Kakkar, A.K.; Vadhan-Raj, S.; Riess, H.; Wun, T.; Streiff, M.B.; Garcia, D.A.; Liebman, H.A.; Belani, C.P.; et al. Rivaroxaban for Thromboprophylaxis in High-Risk Ambulatory Patients with Cancer. N. Engl. J. Med. 2019, 380, 720–728. [Google Scholar] [CrossRef] [PubMed]
- Key, N.S.; Khorana, A.A.; Kuderer, N.M.; Bohlke, K.; Lee, A.Y.; Arcelus, J.I.; Wong, S.L.; Balaban, E.P.; Flowers, C.R.; Francis, C.W.; et al. Venous Thromboembolism Prophylaxis and Treatment in Patients With Cancer: ASCO Clinical Practice Guideline Update. J. Clin. Oncol. 2020, 38, 496–520. [Google Scholar] [CrossRef]
- Lyman, G.H.; Carrier, M.; Ay, C.; Di Nisio, M.; Hicks, L.K.; Khorana, A.A.; Leavitt, A.D.; Lee, A.Y.Y.; Macbeth, F.; Morgan, R.L.; et al. American Society of Hematology 2021 guidelines for management of venous thromboembolism: Prevention and treatment in patients with cancer. Blood Adv. 2021, 5, 927–974. [Google Scholar] [CrossRef]
- Carrier, M.; Blais, N.; Crowther, M.; Kavan, P.; Le Gal, G.; Moodley, O.; Shivakumar, S.; Suryanarayan, D.; Tagalakis, V.; Wu, C.; et al. Treatment Algorithm in Cancer-Associated Thrombosis: Updated Canadian Expert Consensus. Curr. Oncol. 2021, 28, 5434–5451. [Google Scholar] [CrossRef]
- Graf, C.; Wilgenbus, P.; Pagel, S.; Pott, J.; Marini, F.; Reyda, S.; Kitano, M.; Macher-Göppinger, S.; Weiler, H.; Ruf, W. Myeloid cell-synthesized coagulation factor X dampens antitumor immunity. Sci. Immunol. 2019, 4, eaaw8405. [Google Scholar] [CrossRef]
- Ruf, W.; Graf, C. Coagulation signaling and cancer immunotherapy. Thromb. Res. 2020, 191 (Suppl. 1), S106–S111. [Google Scholar] [CrossRef] [PubMed]
- Johannet, P.; Sawyers, A.; Gulati, N.; Donnelly, D.; Kozloff, S.; Qian, Y.; Floristan, A.; Hernando, E.; Zhong, J.; Osman, I. Treatment with therapeutic anticoagulation is not associated with immunotherapy response in advanced cancer patients. J. Transl. Med. 2021, 19, 47. [Google Scholar] [CrossRef] [PubMed]
| Immune Checkpoint Inhibitors | Target | Approved Indication |
|---|---|---|
| Ipilimumab | CTLA-4 | Melanoma NSCLC RCC Colorectal cancer Malignant pleural mesothelioma |
| Pembrolizumab | PD-1 | Melanoma NSCLC Urothelial carcinoma RCC Bladder cancer Esophageal/esophagogastric junction cancer Colorectal cancer Endometrial cancer Cervical cancer Breast cancer Head and neck squamous cell carcinoma Hodgkin lymphoma Primary mediastinal B cell lymphoma |
| Nivolumab | PD-1 | Melanoma NSCLC RCC Head and neck squamous cell carcinoma Classical Hodgkin lymphoma Hepatocellular carcinoma |
| Cemiplimab | PD-1 | NSCLC Cutaneous squamous cell carcinoma Cutaneous basal cell carcinoma Cervical cancer |
| Atezolizumab | PD-L1 | NSCLC Small cell lung cancer Urothelial carcinoma |
| Avelumab | PD-L1 | Urothelial carcinoma Merkel cell carcinoma |
| Durvalumab | PD-L1 | NSCLC Urothelial carcinoma |
| Study | Country | N | Type of Cancer | Stage IV | Follow-up [Median (IQR)] | VTE Incidence % (95% CI) | ATE Incidence % (95% CI) |
|---|---|---|---|---|---|---|---|
| Hegde et al. 2017 [20] Abstract | USA | 76 | Lung | N/A | 10.8 mo | 18.4 | 2.6 |
| Ibrahimi et al. 2017 [21] Abstract | USA | 154 | Lung 20.8% Melanoma 20.1% Ovarian 12.3% | 92% | 7 mo (198 days) | 10.4 | 0 |
| Bar et al. 2019 [22] | Israel | 1215 | All cancers Melanoma 40.5% Lung 28.7% | N/A | 12 mo | AVE (MI, stroke, PE, DVT) 6 mo: 4.9 12 mo: 5.8 | |
| Nichetti et al. 2019 [23] | Italy | 217 | NSCLC | 95.4% | 37.8 mo | 7.4 | 6.5 |
| Ando et al. 2020 [24] | Japan | 122 | Lung, kidney, stomach, urothelial, melanoma | N/A | N/A Time to thrombosis 90 days (range 6–178) | 4.1 | 4.9 |
| Drobni et al. 2020 [25] | USA | 2842 | All cancers NSCLC 28.8% Melanoma 27.9% | N/A | 2 years | N/A | Composite: 5.35/100 person-yrs MI: 2.49 Stroke: 2.08 |
| Deschênes-Simard et al. 2021 [26] | Canada | 593 | NSCLC | 87.2% | 12.7 (4.9–22.7) mo | 9.9 (7.5–12.3) 76.5 (59.9–97.8) per 1000 person-years | 1.3 |
| Gong et al. 2021 [27] | USA | 2854 | All cancers NSCLC 28.4% Melanoma 28.2% | N/A | 194 days (IQR 65–412) | 6 mo: 7.4 12 mo: 13.8 | N/A |
| Gutierrez-Sainz et al. 2021 [28] | Spain | 229 | Lung 48% Melanoma 23.6% RCC 11.8% | 96.5% | 9.8 mo | 7 (4–10) | N/A |
| Guven et al. 2021 [29] | Turkey | 133 | RCC 26.3% Melanoma 24.1% NSCLC 18.8% | 100% | 10.1 (5.8–18.5) mo | 11.3 | N/A |
| Haist et al. 2021 [30] | Germany | 280 | Melanoma | 100% | 28 mo (95% CI 23.4–32.6) | 12.5 | 4.3 |
| Hill et al. 2021 [31] | USA | 435 (a) ICI: 171 (b) ICI+chemo: 157 (c) chemo then durvalumab: 107 | NSCLC | 47% | N/A | 6 mo: (a) 7.6 (4.3–12.2) (b) 9.9 (5.8–15.3) (c) 9.4 (4.8–15.8) 12 mo: (a) 9.0 (5.3–14.0) (b) 12.8 (7.8–19.0) (c) 12.2 (6.8–19.2) | N/A |
| Icht et al. 2021 [32] | Israel | 176 | NSCLC | 85.8% | 6 mo (187 days) | 4.5 (2.1–8.3) | N/A |
| Kewan et al. 2021 [33] | USA | 552 | All cancers NSCLC 47.3% | 100% | 12.1 mo | 12.1 | 1.3 |
| Madison et al. 2021 [34] ^ | USA | 6127 | Lung | N/A | 6 mo | 6.3 | 2.6 |
| Moik et al. 2021 [35] | Austria | 672 | Melanoma 30.4% NSCLC 24.1% RCC 11% | 85.8% | 8.5 mo | 6 mo: 5.0 (3.4–6.9) 12mo: 7.0 (5.1–9.3) Overall: 12.9 (8.2–18.5) | 6 mo: 1.0 (0.4–2.0) 12 mo: 1.8 (0.7–3.6) Overall 1.8 (0.7–3.6) |
| Roopkumar et al. 2021 | USA | 1686 | Lung 49.6% Melanoma 13.2% | 90.3% | 438 days (range 7–1971) | 6 mo: 7.1 12 mo: 10.9 Overall: 24 | N/A |
| Sheng et al. 2021 [18] | USA | 351 | RCC | 100% | 12.8 mo | 11 | 2 |
| Total thromboembolism: 6 mo: 4.4 (2.6–6.9) 12 mo: 9.8 (6.8–13.4) | |||||||
| Sussman et al. 2021 | USA | 228 | Melanoma | 81.1% | 27.3 mo | 6 mo: 8.0 (4.9–12.0) 12 mo: 12.9 (8.9–17.7) | 6 mo: 2.2 (0.8–4.8) 12 mo: 4.5 (2.3–7.8) |
| Alma et al. 2022 [36] | France | 481 | Lung | 86% | 9.8 mo | 9.8 | N/A |
| Bjornhart et al. 2022 [37] | Denmark | 146 prospective (A) * | NSCLC | 87% | 16.5 mo | 6 mo: 13.0 12 mo: 14.4 Overall: 14 | N/A |
| 426 retrospective (B) | 6 mo: 4.9 12 mo: 5.6 Overall: 6 | ||||||
| Canovas et al. 2022 [38] | Spain | 665 | Lung | 91.2% | 14 mo | 6.9 | 1.5 |
| All thrombosis: 8.4 (6.23–10.6) | |||||||
| 291 | Melanoma | 82.5% | 17 mo | 4.8 | 1.0 | ||
| All thrombosis: 5.8 (3.34–9.18) | |||||||
| Endo et al. 2022 [39] | Japan | 120 | Lung | 62.5% | within 6 mo | 2.5 | 4.2 |
| Khorana et al. 2023 [40] ^ | USA | (a) ICI: 605 (b) ICI+chemo: 602 | NSCLC | 100% | 9.1 mo | 6 mo: (a) 8.1 (b) 12.8 12 mo: (a) 13.5 (10.6–16.5) (b) 22.4 (20.2–24.5) | N/A |
| May et al. 2022 abstract [41] ^ | USA | 1823 | All cancers | N/A | 6 mo | 7.3 | N/A |
| Sanfilippo et al. 2022 abstract [42]^ | USA | 1754 | All cancers | 77.9% | 6 mo | 4.1 | N/A |
| Sheng et al. 2022 [19] | USA | 279 | Urothelial | 100% | 5.6 mo | 13 | 2 |
| Total thromboembolism: 6 mo: 9.1 (6.0–13.0) 12 mo: 13.6 (9.6–18.4) | |||||||
| Study | N | Type of cancer | Follow-up (mo) | VTE (%), (95% CI) | ATE (%), (95% CI) |
|---|---|---|---|---|---|
| Mulder et al. 2021 [44] | 370 | All cancers | 6 | 4.1 (2.3–6.7) | N/A |
| 12 | 7.1 (4.2–11.1) | ||||
| Moik et al. 2021 [44] Abstract | 3259 | All cancers | 6 | 3.9 (3.3–4.7) | 1.3 (0.9–1.8) |
| 12 | 5.7 (4.9–6.6) | 2.2 (1.7–2.8) | |||
| 24 | 7.3 (6.2–8.4) | 3.1 (2.4–3.8) | |||
| Overvad et al. 2022 [45] | 3946 | All cancers | 6 | 2.6 | 1.3 |
| 12 | 3.8 | 1.9 |
| Study | Risk factors for Thrombosis (Multivariable) | Risk Factors for Mortality |
|---|---|---|
| Hegde et al. 2017 [20] (Abstract) | Female | VTE before ICI |
| Bar et al. 2019 [22] | NSCLC H/o AVE Hypertension Dyslipidemia | AVE |
| Nichetti et al. 2019 [23] | Current smoker PD-L1 > 50% | TE |
| Ando et al. 2020 [24] | h/o thromboembolism | N/A |
| Drobni et al. 2020 [25] | Overall study: ICIs, age, h/o stroke, diabetes, hypertension, NSCLC, male, h/o radiation | N/A |
| Deschênes-Simard et al. 2021 [26] | Age < 65 Higher PD-L1 level Smoking <12 mo from diagnosis to ICIs | VTE is not correlated with survival |
| Gong et al. 2021 [27] | Age ≤ 65 Khorana score ≥ 2 h/o hypertension Strong trend: h/o VTE (HR 1.42, 95% CI 0.99–2.06) (melanoma is associated with decreased risks) | N/A |
| Gutierrez-Sainz et al. 2021 [28] | Female Melanoma | VTE is not an independent risk factor |
| Guven et al. 2021 [29] | ECOG ≥ 1 | VTE (trend, not significant) |
| Hill et al. 2021 [31] | Cancer treatment types (ICI-chemotherapy, targeted therapies) Smoking | VTE was not associated with significantly worsened survival |
| Icht et al. 2021 [32] | N/A | VTE |
| Kewan et al. 2021 [33] | Anticoagulation at the time of ICI (univariate) | Khorana score |
| Moik et al. 2021 [35] | h/o VTE | VTE after ICI |
| Roopkumar et al. 2021 [47] | Younger age Metastasis Biomarkers | VTE |
| Sheng et al. 2021 [18] | None | Thromboembolism, IMDC score, and/or Khorana score |
| Sussman et al. 2021 [46] | Combination ICI Khorana score ≥ 1 h/o CAD Anticoagulation at treatment start | VTE |
| Alma et al. 2022 [36] | Metastasis BMI | VTE |
| Bjornhart et al. 2022 [37] | h/o VTE ICI as first-line treatment Other mets (non-brain, liver, bone) | VTE |
| Canovas et al. 2022 [38] Lung cancer cohort | Hgb < 10.9 g/dL at the start of ICI NLR < 4.55 h/o thrombosis | Thrombosis |
| Canovas et al. 2022 [38] Melanoma cohort | LDH > 198 U/L NLR > 3.01 | Thrombosis |
| Endo et al. 2022 [39] | ECOG ≥ 2 and history of thromboembolism | N/A |
| Khorana et al. 2023 [40] | History of radiation Body mass index ≥ 40 kg/m2 | N/A |
| Sanfilippo et al. 2022 [42] (Abstract) | ICI-chemotherapy (vs ICI alone) Severe frailty by CA frailty index | N/A |
| Sheng et al. 2022 [19] | None | Thromboembolism, Bajorin score 1 and 2 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wang, T.-F.; Carrier, M. Immune Checkpoint Inhibitors-Associated Thrombosis: Incidence, Risk Factors and Management. Curr. Oncol. 2023, 30, 3032-3046. https://doi.org/10.3390/curroncol30030230
Wang T-F, Carrier M. Immune Checkpoint Inhibitors-Associated Thrombosis: Incidence, Risk Factors and Management. Current Oncology. 2023; 30(3):3032-3046. https://doi.org/10.3390/curroncol30030230
Chicago/Turabian StyleWang, Tzu-Fei, and Marc Carrier. 2023. "Immune Checkpoint Inhibitors-Associated Thrombosis: Incidence, Risk Factors and Management" Current Oncology 30, no. 3: 3032-3046. https://doi.org/10.3390/curroncol30030230
APA StyleWang, T.-F., & Carrier, M. (2023). Immune Checkpoint Inhibitors-Associated Thrombosis: Incidence, Risk Factors and Management. Current Oncology, 30(3), 3032-3046. https://doi.org/10.3390/curroncol30030230





