Achieving a Textbook Outcome in Colon Cancer Surgery Is Associated with Improved Long-Term Survival
Abstract
1. Introduction
2. Materials and Methods
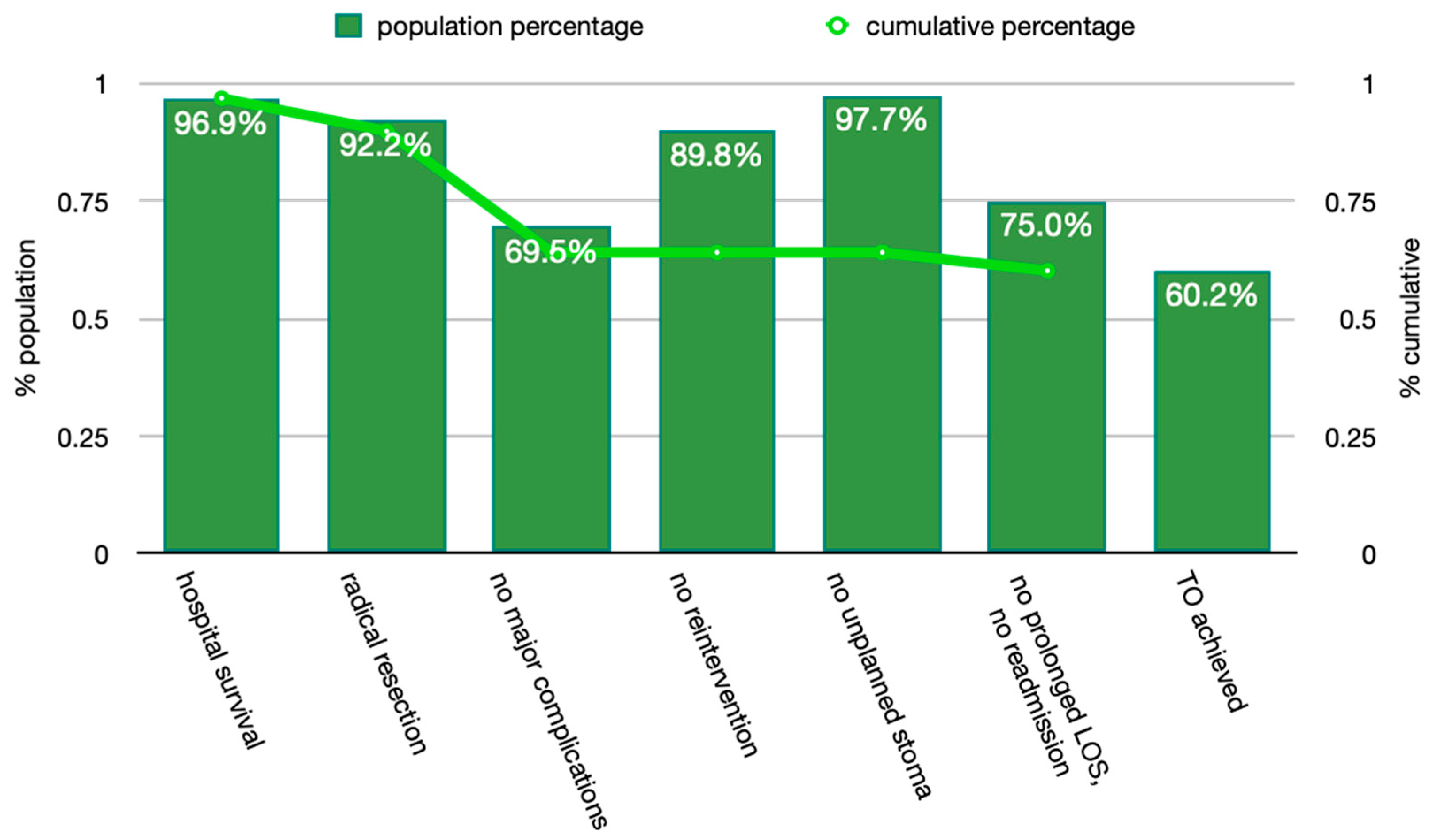
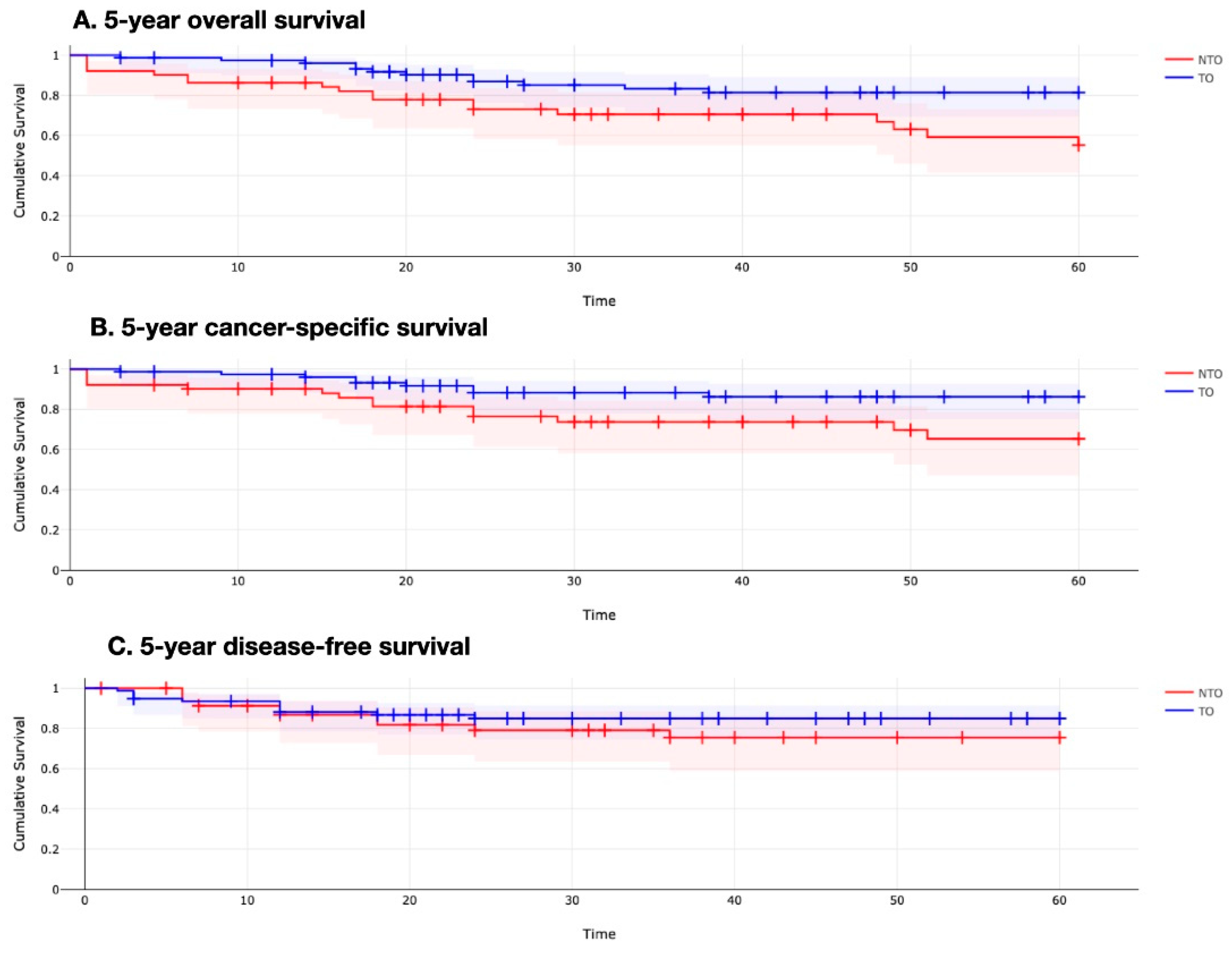
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Yang, C.C.; Tian, Y.F.; Liu, W.S.; Chou, C.L.; Cheng, L.C.; Chu, S.S.; Lee, C.C. The association between the composite quality measure “textbook outcome” and long term survival in operated colon cancer. Medicine 2020, 99, e22447. [Google Scholar] [CrossRef] [PubMed]
- Busweiler, L.A.; Schouwenburg, M.G.; van Berge Henegouwen, M.I.; Kolfschoten, N.E.; de Jong, P.C.; Rozema, T.; Wijnhoven, B.P.; van Hillegersberg, R.; Wouters, M.W.; van Sandick, J.W.; et al. Textbook outcome as a composite measure in oesophagogastric cancer surgery. Br. J. Surg. 2017, 104, 742–750. [Google Scholar] [CrossRef] [PubMed]
- Oesophago-Gastric Anastomotic Audit (OGAA) Collaborative. Textbook outcome following oesophagectomy for cancer: International cohort study. Br. J. Surg. 2022, 109, 439–449. [Google Scholar] [CrossRef]
- Van Roessel, S.; Mackay, T.M.; van Dieren, S.; van der Schelling, G.P.; Nieuwenhuijs, V.B.; Bosscha, K.; van der Harst, E.; van Dam, R.M.; Liem, M.S.; Festen, S.; et al. Textbook outcome: Nationwide analysis of a novel quality measure in pancreatic surgery. Ann. Surg. 2020, 271, 155–162. [Google Scholar] [CrossRef] [PubMed]
- De Graaff, M.R.; Elfrink, A.K.; Buis, C.I.; Swijnenburg, R.J.; Erdmann, J.I.; Kazemier, G.; Verhoef, C.; Mieog, J.S.; Derksen, W.J.; van den Boezem, P.B.; et al. Defining textbook outcome in liver surgery and assessment of hospital variation: A nationwide population-based study. Eur. J. Surg. Oncol. 2022, 48, 2414–2423. [Google Scholar] [CrossRef]
- Sweigert, P.J.; Eguia, E.; Baker, M.S.; Link, C.M.; Hyer, J.M.; Paredes, A.Z.; Tsilimigras, D.I.; Husain, S.; Pawlik, T.M. Assessment of cancer center variation in textbook oncologic outcomes following colectomy for adenocarcinoma. J. Gastrointest. Surg. 2021, 25, 775–785. [Google Scholar] [CrossRef]
- Warps, A.K.; Detering, R.; Tollenaar, R.A.E.M.; Tanis, P.J.; Dekker, J.W.T.; Dutch, C.A.G. Textbook outcome after rectal cancer surgery as a composite measure for quality of care: A population-based study. Eur. J. Surg. Oncol. 2021, 47, 2821–2829. [Google Scholar] [CrossRef]
- Kolfschoten, N.E.; Kievit, J.; Gooiker, G.A.; Van Leersum, N.J.; Snijders, H.S.; Eddes, E.H.; Tollenaar, R.A.; Wouters, M.W.; Marang-Van De Mheen, P.J. Focusing on desired outcomes of care after colon cancer resections; hospital variations in ‘textbook outcome’. Eur. J. Surg. Oncol. 2013, 39, 156–163. [Google Scholar] [CrossRef]
- Hohenberger, W.; Weber, K.; Matzel, K.; Papadopoulos, T.; Merkel, S. Standardized surgery for colonic cancer: Complete mesocolic excision and central ligation--technical notes and outcome. Colorectal Dis. 2009, 11, 354–364. [Google Scholar] [CrossRef]
- Xynos, E.; Gouvas, N.; Triantopoulou, C.; Al, E. Clinical practice guidelines for the surgical management of colon cancer: A consensus statement of the Hellenic and Cypriot Colorectal Cancer Study Group by the HESMO. Ann. Gastroenterol. 2016, 29, 3–17. [Google Scholar]
- Dindo, D.; Demartines, N.; Clavien, P.A. Classification of surgical complications: A new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann. Surg. 2004, 240, 205–213. [Google Scholar] [CrossRef]
- Aiken, T.; Abbott, D.E. Textbook oncologic outcome: A promising summary metric of high-quality care, but are we on the same page. J. Surg. Oncol. 2020, 121, 923–924. [Google Scholar] [CrossRef]
- van Groningen, J.T.; Ceyisakar, I.E.; Gietelink, L.; Henneman, D.; van der Harst, E.; Westerterp, M.; Marang-van de Mheen, P.J.; Tollenaar, R.A.; Lingsma, H.; Wouters, M.W. Identifying best performing hospitals in colorectal cancer care; is it possible. Eur. J. Surg. Oncol. 2020, 46, 1144–1150. [Google Scholar] [CrossRef]
- Mehta, R.; Tsilimigras, D.I.; Paredes, A.Z.; Sahara, K.; Moro, A.; Farooq, A.; White, S.; Ejaz, A.; Tsung, A.; Dillhoff, M.; et al. Comparing textbook outcomes among patients undergoing surgery for cancer at US News & World Report ranked hospitals. J. Surg. Oncol. 2020, 121, 927–935. [Google Scholar]
- Aquina, C.T.; Hamad, A.; Becerra, A.Z.; Cloyd, J.M.; Tsung, A.; Pawlik, T.M.; Ejaz, A. Is textbook oncologic outcome a valid hospital-quality metric after high-risk surgical oncology procedures. Ann. Surg. Oncol. 2021, 28, 8028–8045. [Google Scholar] [CrossRef]
- GlobalSurg Collaborative and NIHR Global Health Research Unit on Global Surgery. Global variation in postoperative and complications after cancer surgery: A multicentre, prospective cohort study in 82 countries. Lancet 2021, 397, 387–397. [Google Scholar] [CrossRef]
- GlobalSurg Collaborative and NIHR Global Health Research Unit on Global Surgery. Effects of hospital facilities on patient outcomes after cancer surgery: An international, prospective, observational study. Lancet Glob. Health 2022, 10, e1003–e1011. [Google Scholar] [CrossRef]
- Barclay, M.; Dixon-Woods, M.; Lyratzopoulos, G. The problem with composite indicators. BMJ Qual. Saf. 2019, 28, 338–344. [Google Scholar] [CrossRef]
- Kalff, M.C.; Van Berge Henegouwen, M.I.; Gisbertz, S.S. Textbook outcome for esophageal cancer surgery: An international consensus-based update of a quality measure. Dis. Esophagus. 2021, 34, doab011. [Google Scholar] [CrossRef]
- Görgec, B.; Cacciaguerra, A.B.; Pawlik, T.M.; Aldrighetti, L.A.; Alseidi, A.A.; Cillo, U.; Kokudo, N.; Geller, D.A.; Wakabayashi, G.; Asbun, H.J.; et al. An international expert delphi consensus on defining textbook outcome in liver surgery (TOLS). Ann. Surg. 2022, 10–97, Online ahead of print. [Google Scholar] [CrossRef]
- Glasbey, J.C.; Nepogodiev, D.; Simoes, J.F.; Omar, O.; Li, E.; Venn, M.L.; Abou Chaar, M.K.; Capizzi, V.; Chaudhry, D.; Desai, A.; et al. Elective cancer surgery in COVID-19-free surgical pathways during the SARS-CoV-2pandemic: An international, multicenter, comparative cohort study. J. Clin. Oncol. 2021, 39, 66–78. [Google Scholar] [CrossRef] [PubMed]
- CovidSurg. Collaborative; Glasbey, J.C.; Nepogodiev, D.; Simoes, J.F.; Omar, O.M.; Venn, M.L.; Evans, J.P.; Futaba, K.; Knowles, C.H.; Minaya-Bravo, A.; et al. Outcomes from elective colorectal cancer surgery during the SARS-CoV-2 pandemic. Colorectal Dis. 2020, 23, 732–749. [Google Scholar]
- CovidSurg. Collaborative. Effect of COVID-19 pandemic lockdowns on planned cancer surgery for 15 tumour types in 61 countries: An international, prospective, cohort study. Lancet Oncol. 2021, 22, 1507–1517. [Google Scholar] [CrossRef] [PubMed]
- CovidSurg. Collaborative; Adamina, M.; Ademuyiwa, A.; Adisa, A.; Bhangu, A.A.; Bravo, A.M.; Cunha, M.F.; Emile, S.; Ghosh, D.; Glasbey, J.C.; et al. The impact of surgical delay on resectability of colorectal cancer: An international prospective cohort study. Colorectal Dis. 2022, 24, 708–726. [Google Scholar]
| N | % | |
|---|---|---|
| Age (years) | 70.7 ± 11.4 | range 36–93 |
| Sex | ||
| male | 78 | 60.9% |
| female | 50 | 39.1% |
| ASA class | ||
| II | 92 | 71.9% |
| III | 36 | 28.1% |
| Surgical setting | ||
| elective | 118 | 92.2% |
| emergency | 10 | 7.8% |
| Surgical approach | ||
| open | 78 | 60.9% |
| laparoscopic | 47 | 36.7% |
| conversion | 3 | 2.4% |
| Type of resection | ||
| right hemicolectomy | 58 | 45.3% |
| extended right | 19 | 14.9% |
| left hemicolectomy | 16 | 12.5% |
| high anterior resection | 35 | 27.3% |
| 30-day post-operative mortality | 4 | 3.1% |
| 30-day post-operative morbidity | 43 | 33.6% |
| Length of hospital stay (days) | 9.9 ± 7.7 | range 3–49 |
| 30-day readmission | 4 | 3.1% |
| N | % | |
|---|---|---|
| Quality of resection | ||
| R0 | 124 | 96.9% |
| R1 | 4 | 3.1% |
| Mean lymph node yield | 25.5 ± 11.4 | range 6–74 |
| ≥12 lymph nodes | 122 | 95.3% |
| pT stage | ||
| pT1 | 22 | 17.2% |
| pT2 | 16 | 12.5% |
| pT3 | 73 | 57% |
| pT4 | 17 | 13.3% |
| pN stage | ||
| pN0 | 84 | 65.6% |
| pN (+) | 44 | 34.4% |
| pN1 (1–3 lymph nodes) | 23 | 18% |
| pN2 (≥4 lymph nodes) | 21 | 16.4% |
| TNM stage | ||
| stage I | 37 | 28.9% |
| stage II | 47 | 36.7% |
| stage III | 44 | 34.4% |
| TO | NTO | p Value | |
|---|---|---|---|
| Age (years) | 68.5 ± 11.1 | 73.9 ± 11.3 | 0.005 |
| Sex | |||
| male | 46 (59.7%) | 32 (62.7%) | |
| female | 31 (40.3%) | 19 (37.3%) | 0.733 |
| ASA class | |||
| II | 57 (74%) | 35 (68.6%) | |
| III | 20 (26%) | 16 (31.4%) | 0.506 |
| Tumour location | |||
| right-sided | 53 (68.8%) | 24 (47.1%) | |
| left-sided | 24 (31.2%) | 27 (52.9%) | 0.013 |
| Surgical setting | |||
| elective | 73 (94.8%) | 45 (88.2%) | |
| emergency | 4 (5.2%) | 6 (11.8%) | 0.195 |
| Surgical approach | |||
| open + conversion | 48 (62.3%) | 33 (64.7%) | |
| laparoscopic | 29 (37.7%) | 18 (35.3%) | 0.785 |
| TNM stage | |||
| stage I | 28 (36.3%) | 9 (17.6%) | |
| stage II | 27 (35.1%) | 20 (39.3%) | |
| stage III | 22 (28.6%) | 22 (43.1%) | 0.056 |
| pT stage | |||
| pT1 + pT2 | 29 (37.7%) | 9 (17.6%) | |
| pT3 | 42 (54.5%) | 31 (60.8%) | |
| pT4 | 6 (7.8%) | 11 (21.6%) | 0.012 |
| pN stage | |||
| pN0 | 55 (71.4%) | 29 (56.9%) | |
| pN(+) | 22 (28.6%) | 22 (43.1%) | 0.089 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Manatakis, D.K.; Tzardi, M.; Souglakos, J.; Tsiaoussis, J.; Agalianos, C.; Kyriazanos, I.D.; Pechlivanides, G.; Kordelas, A.; Tasis, N.; Gouvas, N.; et al. Achieving a Textbook Outcome in Colon Cancer Surgery Is Associated with Improved Long-Term Survival. Curr. Oncol. 2023, 30, 2879-2888. https://doi.org/10.3390/curroncol30030220
Manatakis DK, Tzardi M, Souglakos J, Tsiaoussis J, Agalianos C, Kyriazanos ID, Pechlivanides G, Kordelas A, Tasis N, Gouvas N, et al. Achieving a Textbook Outcome in Colon Cancer Surgery Is Associated with Improved Long-Term Survival. Current Oncology. 2023; 30(3):2879-2888. https://doi.org/10.3390/curroncol30030220
Chicago/Turabian StyleManatakis, Dimitrios K., Maria Tzardi, John Souglakos, John Tsiaoussis, Christos Agalianos, Ioannis D. Kyriazanos, George Pechlivanides, Athanasios Kordelas, Nikolaos Tasis, Nikolaos Gouvas, and et al. 2023. "Achieving a Textbook Outcome in Colon Cancer Surgery Is Associated with Improved Long-Term Survival" Current Oncology 30, no. 3: 2879-2888. https://doi.org/10.3390/curroncol30030220
APA StyleManatakis, D. K., Tzardi, M., Souglakos, J., Tsiaoussis, J., Agalianos, C., Kyriazanos, I. D., Pechlivanides, G., Kordelas, A., Tasis, N., Gouvas, N., & Xynos, E. (2023). Achieving a Textbook Outcome in Colon Cancer Surgery Is Associated with Improved Long-Term Survival. Current Oncology, 30(3), 2879-2888. https://doi.org/10.3390/curroncol30030220






