Assessing the Functional Accessibility, Actionability, and Quality of Patient Education Materials from Canadian Cancer Agencies
Abstract
1. Introduction
2. Materials and Methods
2.1. Sample Collection
2.2. Document Readability Analysis
2.3. Difficult Word Analysis
2.4. Quality, Actionability, and Understandability Analysis
2.5. Statistics
3. Results
3.1. Document Readability Analysis
3.2. Difficult Word Analysis
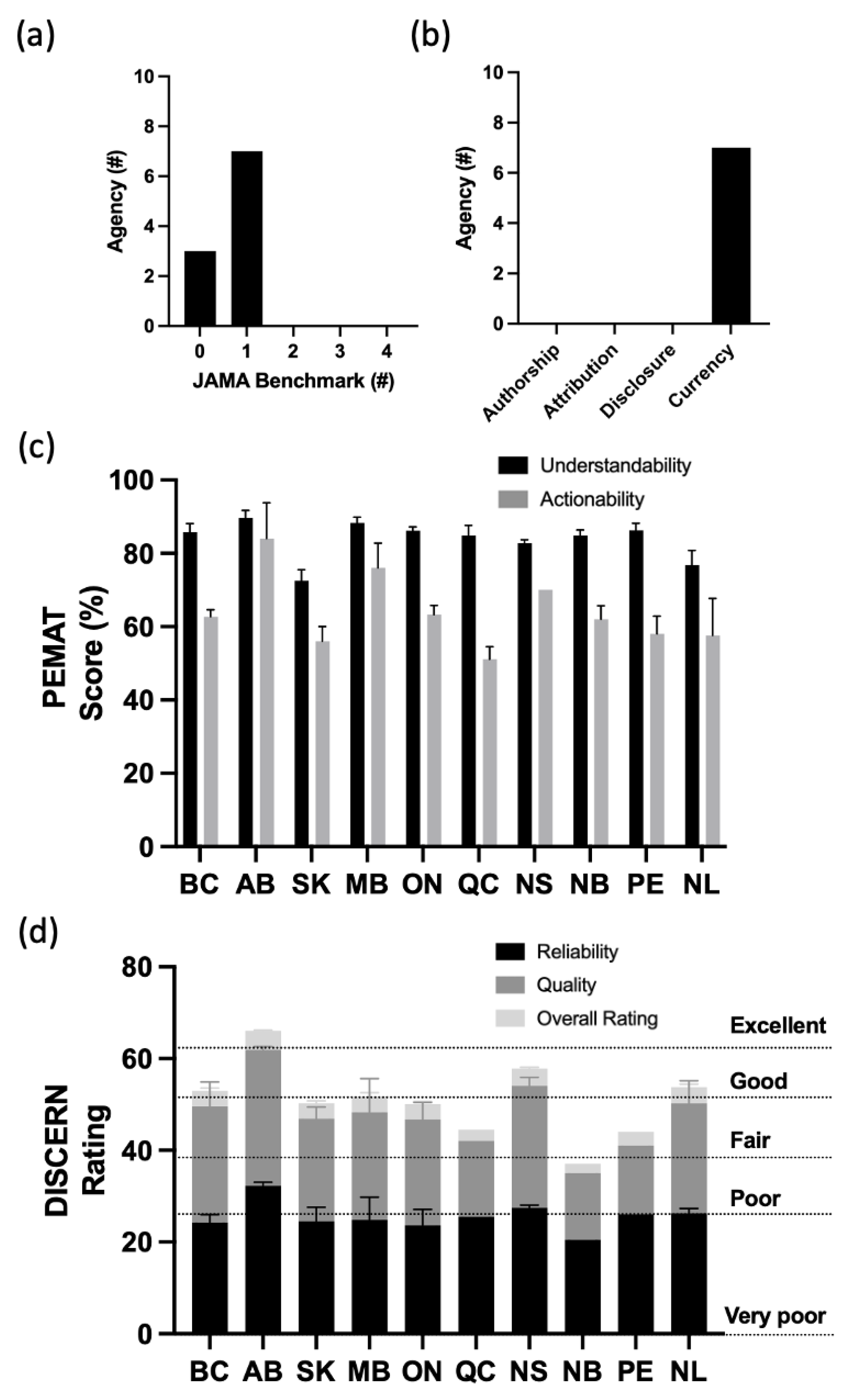
3.3. Quality, Actionability, and Understandability Analysis
4. Discussion
4.1. Implications
4.2. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AB | Alberta |
| ANOVA | Analysis of Variance |
| BC | British Columbia |
| CDC | Centers for Disease Control and Prevention |
| CLI | Coleman–Liau Index |
| COVID | Coronavirus |
| DRP | Degrees of Reading Power |
| FK | Flesch–Kincaid Grade Level |
| FORCAST | Ford, Caylor, Sticht |
| FRG | Fry Readability Graph |
| GR | Grade Equivalent |
| GRL | Grade reading level |
| GF | Gunning Fog Index |
| MB | Manitoba |
| NIH | National Institutes of Health |
| NB | New Brunswick |
| NDC | New Dale–Chall |
| NFC | New Fog Count |
| NL | Newfoundland and Labrador |
| NS | Nova Scotia |
| ON | Ontario |
| PEM | Patient education materials |
| PEMAT | Patient Education Materials Assessment Tool |
| PEI | Prince Edward Island |
| Portal Document Format | |
| QC | Québec |
| SK | Saskatchewan |
| SMOG | Simple Measure of Gobbledygook Index |
| RREG | Raygor Readability Estimate Graph |
References
- Centers for Disease Control, Health Literacy Page. Available online: https://www.cdc.gov/healthliteracy/learn/index.html (accessed on 31 October 2022).
- Wolf, M.S.; Gazmararian, J.A.; Baker, D.W. Health Literacy and Functional Health Status Among Older Adults. Arch. Intern. Med. 2005, 165, 1946–1952. [Google Scholar] [CrossRef] [PubMed]
- Berkman, N.D.; Sheridan, S.L.; Donahue, K.E.; Halpern, D.J.; Crotty, K. Low Health Literacy and Health Outcomes: An Updated Systematic Review. Ann. Intern. Med. 2011, 155, 97–107. [Google Scholar] [CrossRef] [PubMed]
- Silva, M.J.; Santos, P. The Impact of Health Literacy on Knowledge and Attitudes towards Preventive Strategies against COVID-19: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2021, 18, 5421. [Google Scholar] [CrossRef] [PubMed]
- Funnell, M.M.; Donnelly, M.B.; Anderson, R.M.; Johnson, P.D.; Oh, M.S. Perceived Effectiveness, Cost, and Availability of Patient Education Methods and Materials. Diabetes Educ. 1992, 18, 139–145. [Google Scholar] [CrossRef]
- Vanderpool, R.C.; Huang, G.C.; Mollica, M.; Gutierrez, A.I.; Maynard, C.D. Cancer Information-seeking in an Age of COVID-19: Findings from the National Cancer Institute’s Cancer Information Service. Health Commun. 2021, 36, 89–97. [Google Scholar] [CrossRef]
- OECD Skills Outlook 2013. Available online: https://escholarship.org/uc/item/4b75m4tj (accessed on 10 November 2022).
- Simply Put; a Guide for Creating Easy-to-Understand Materials. Strategic and Proactive Communication. Available online: https://stacks.cdc.gov/view/cdc/11938 (accessed on 11 November 2022).
- Man, A.; van Ballegooie, C. Assessment of the Readability of Web-Based Patient Education Material from Major Canadian Pediatric Associations: Cross-sectional Study. JMIR Pediatr. Parent. 2022, 5, e31820. [Google Scholar] [CrossRef]
- Stossel, L.M.; Segar, N.; Gliatto, P.; Fallar, R.; Karani, R. Readability of Patient Education Materials Available at the Point of Care. J. Gen. Intern. Med. 2012, 27, 1165–1170. [Google Scholar] [CrossRef] [PubMed]
- Hoang, P.M.; van Ballegooie, C. Assessment of the Readability and Quality of Online Patient Education Material for Chronic Medical Conditions. Healthcare 2022, 10, 234. [Google Scholar] [CrossRef]
- Agarwal, N.; Hansberry, D.R.; Sabourin, V.; Tomei, K.L.; Prestigiacomo, C.J. A Comparative Analysis of the Quality of Patient Education Materials from Medical Specialties. JAMA Intern. Med. 2013, 173, 1257–1259. [Google Scholar] [CrossRef]
- Friedman, D.; Hoffman-Goetz, L.; Arocha, J. Readability of Cancer Information on the Internet. J. Cancer Educ. 2004, 19, 117–122. [Google Scholar] [CrossRef]
- Perni, S.; Rooney, M.K.; Horowitz, D.P.; Golden, D.W.; McCall, A.R.; Einstein, A.J.; Jagsi, R. Assessment of Use, Specificity, and Readability of Written Clinical Informed Consent Forms for Patients With Cancer Undergoing Radiotherapy. JAMA Oncol. 2019, 5, e190260. [Google Scholar] [CrossRef] [PubMed]
- van Ballegooie, C.; Hoang, P. Health Services: A Mixed Methods Assessment of Canadian Cancer Patient Education Materials Related to the 2019 Novel Coronavirus. Cancer Control. 2021, 28, 1073274821989709. [Google Scholar] [CrossRef] [PubMed]
- van Ballegooie, C. Assessment of Canadian patient education material for oncology pharmaceutics. J. Oncol. Pharm. Pr. 2020, 27, 1578–1587. [Google Scholar] [CrossRef] [PubMed]
- Friedman, D.B.; Hoffman-Goetz, L.; Arocha, J.F. Health literacy and the World Wide Web: Comparing the readability of leading incident cancers on the Internet. Med Informatics Internet Med. 2006, 31, 67–87. [Google Scholar] [CrossRef]
- van Ballegooie, C.; Hoang, P. Assessment of the Readability of Online Patient Education Material from Major Geriatric Associations. J. Am. Geriatr. Soc. 2021, 69, 1051–1056. [Google Scholar] [CrossRef]
- Charnock, D.; Shepperd, S.; Needham, G.; Gann, R. DISCERN: An instrument for judging the quality of written consumer health information on treatment choices. J. Epidemiol. Community Health 1999, 53, 105–111. [Google Scholar] [CrossRef]
- Silberg, W.M.; Lundberg, G.D.; Musacchio, R.A. Assessing, Controlling, and Assuring the Quality of Medical Information on the Internet: Caveant Lector et Viewor—Let the Reader and Viewer Beware. JAMA 1997, 277, 1244–1245. [Google Scholar] [CrossRef]
- Shoemaker, S.J.; Wolf, M.S.; Brach, C. Development of the Patient Education Materials Assessment Tool (PEMAT): A new measure of understandability and actionability for print and audiovisual patient information. Patient Educ. Couns. 2014, 96, 395–403. [Google Scholar] [CrossRef]
- Sobota, A.; Ozakinci, G. The Quality and Readability of Online Consumer Information About Gynecologic Cancer. Int. J. Gynecol. Cancer 2015, 25, 537–541. [Google Scholar] [CrossRef]
- López-Jornet, P.; Camacho-Alonso, F. The quality of internet sites providing information relating to oral cancer. Oral Oncol. 2009, 45, e95–e98. [Google Scholar] [CrossRef]
- Ni Riordain, R.; McCreary, C. Head and neck cancer information on the internet: Type, accuracy and content. Oral Oncol. 2009, 45, 675–677. [Google Scholar] [CrossRef] [PubMed]
- Kobes, K.; Harris, I.B.; Regehr, G.; Tekian, A.; Ingledew, P.-A. Malignant websites? Analyzing the quality of prostate cancer education web resources. Can. Urol. Assoc. J. 2018, 12, 344–350. [Google Scholar] [CrossRef]
- Alsaiari, A.; Joury, A.; Aljuaid, M.; Wazzan, M.; Pines, J.M. The Content and Quality of Health Information on the Internet for Patients and Families on Adult Kidney Cancer. J. Cancer Educ. 2017, 32, 878–884. [Google Scholar] [CrossRef] [PubMed]
- Chlebowski, R.T.; Geller, M.L. Adherence to Endocrine Therapy for Breast Cancer. Oncology 2006, 71, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Ekinci, E.; Nathoo, S.; Korattyil, T.; Vadhariya, A.; Zaghloul, H.A.; Niravath, P.A.; Abughosh, S.M.; Trivedi, M.V. Interventions to improve endocrine therapy adherence in breast cancer survivors: What is the evidence? J. Cancer Surviv. 2018, 12, 348–356. [Google Scholar] [CrossRef]
- Chalela, P.; Muñoz, E.; Inupakutika, D.; Kaghyan, S.; Akopian, D.; Kaklamani, V.; Lathrop, K.; Ramirez, A. Improving adherence to endocrine hormonal therapy among breast cancer patients: Study protocol for a randomized controlled trial. Contemp. Clin. Trials Commun. 2018, 12, 109–115. [Google Scholar] [CrossRef]
- Miller, T.A. Health literacy and adherence to medical treatment in chronic and acute illness: A meta-analysis. Patient Educ. Couns. 2016, 99, 1079–1086. [Google Scholar] [CrossRef]
- Ethan, D.; Basch, C.H.; MacLean, S.A.; Garcia, P.; Basch, E.C. Readability of colorectal cancer online information: A brief report. Int. J. Prev. Med. 2018, 9, 77. [Google Scholar] [CrossRef]
- Mbanda, N.; Dada, S.; Bastable, K.; Ingalill, G.-B. A scoping review of the use of visual aids in health education materials for persons with low-literacy levels. Patient Educ. Couns. 2020, 104, 998–1017. [Google Scholar] [CrossRef]
- Pratt, M.; Searles, G.E. Using Visual Aids to Enhance Physician-Patient Discussions and Increase Health Literacy. J. Cutan. Med. Surg. 2017, 21, 497–501. [Google Scholar] [CrossRef]
- Pentz, R.D.; Lohani, M.; Hayban, M.; Switchenko, J.M.; Dixon, M.D.; De Feo, R.J.D., Jr.; Orloff, G.M.; Jani, A.B.; Master, V.A. Videos improve patient understanding of misunderstood chemotherapy terminology. Cancer 2019, 125, 4011–4018. [Google Scholar] [CrossRef] [PubMed]
- Hibbard, J.H.; Stockard, J.; Mahoney, E.R.; Tusler, M. Development of the Patient Activation Measure (PAM): Conceptualizing and Measuring Activation in Patients and Consumers. Health Serv. Res. 2004, 39, 1005–1026. [Google Scholar] [CrossRef] [PubMed]
- Katz, M.L.; Fisher, J.L.; Fleming, K.; Paskett, E.D. Patient Activation Increases Colorectal Cancer Screening Rates: A Randomized Trial among Low-Income Minority Patients. Cancer Epidemiol. Biomark. Prev. 2012, 21, 45–52. [Google Scholar] [CrossRef] [PubMed]
- Papadakos, J.K.; Giannopoulos, E.; McBain, S.; Forbes, L.; Jain, P.; Samoil, D.; Wang, J.; Zwicker, V.; Fox, C.; Moody, L.; et al. Quality Assessment of Cancer Patient Education Materials: The Current State of Systemic Therapy Patient Education in Fourteen Cancer Centres across Ontario, Canada. Support. Care Cancer 2021, 29, 3513–3519. [Google Scholar] [CrossRef] [PubMed]
- Tae, J.W.; Lee, J.C.; Hong, S.J.; Han, J.P.; Lee, Y.H.; Chung, J.H.; Yoon, H.G.; Ko, B.M.; Cho, J.Y.; Lee, J.S.; et al. Impact of Patient Education with Cartoon Visual Aids on the Quality of Bowel Preparation for Colonoscopy. Gastrointest. Endosc. 2012, 76, 804–811. [Google Scholar] [CrossRef] [PubMed]
- Hansen, H.; Nielsen, B.K.; Boejen, A.; Vestergaard, A. Teaching Cancer Patients the Value of Correct Positioning During Radiotherapy Using Visual Aids and Practical Exercises. J. Cancer Educ. 2018, 33, 680–685. [Google Scholar] [CrossRef]
- Hofmann, S.; Vetter, J.; Wachter, C.; Henne-Bruns, D.; Porzsolt, F.; Kornmann, M. Visual Aids for Multimodal Treatment Options to Support Decision Making of Patients with Colorectal Cancer. BMC Med. Inform. Decis. Mak. 2012, 12, 118. [Google Scholar] [CrossRef] [PubMed]
- Choi, J. Development and pilot test of pictograph-enhanced breast health-care instructions for community-residing immigrant women. Int. J. Nurs. Pract. 2012, 18, 373–378. [Google Scholar] [CrossRef]
- Institute of Medicine (US) Committee on Health Literacy. Health Literacy: A Prescription to End Confusion; Nielsen-Bohlman, L., Panzer, A.M., Kindig, D.A., Eds.; The National Academies Press: Washington, DC, USA, 2004; Volume 1. [Google Scholar] [CrossRef]
| Cancer Agency | Province | Number of Unique PEMs |
|---|---|---|
| BC Cancer | British Columbia (BC) | 184 |
| Cancer Control Alberta | Alberta (AB) | 110 |
| Sask Cancer Agency | Saskatchewan (SK) | 59 |
| Cancer Care Manitoba | Manitoba (MB) | 70 |
| Cancer Care Ontario | Ontario (ON) | 64 |
| Ministry of Health and Social Services | Quebec (QC) | 40 |
| Cancer Care Eastern Health | Newfoundland and Labrador (NL) | 68 |
| New Brunswick Cancer Network | New Brunswick (NB) | 17 |
| Health PEI | Prince Edward Island (PE) | 25 |
| Nova Scotia Health Authority | Nova Scotia (NS) | 149 |
| CLI | NDC | DRP GE | FK | FORCAST | GF | NFC | SMOG | Average | |
|---|---|---|---|---|---|---|---|---|---|
| BC | 10.6 ± 1.9 | 9.4 ± 2.2 | 9.6 ± 2.5 | 8.4 ± 1.9 | 10.9 ± 0.9 | 9.5 ± 1.6 | 4.9 ± 1.5 | 10.9 ± 1.3 | 9.29 ± 1.8 |
| AB | 9.8 ± 2.6 | 8.3 ± 3.1 | 8.5 ± 3.7 | 7.8 ± 2.5 | 10.5 ± 1.2 | 9.3 ± 2.2 | 5.4 ± 2.0 | 10.4 ± 1.8 | 8.75 ± 2.5 |
| SK | 11.7 ± 2.0 | 9.5 ± 2.1 | 10.5 ± 3.2 | 9.8 ± 2.0 | 11.0 ± 0.9 | 10.3 ± 1.9 | 6.3 ± 2.0 | 11.8 ± 1.4 | 10.1 ± 2.0 |
| MB | 10.5 ± 2.3 | 9.0 ± 2.7 | 9.5 ± 3.3 | 8.5 ± 2.3 | 10.8 ± 0.9 | 9.7 ± 2.2 | 5.3 ± 1.7 | 10.9 ± 1.8 | 9.3 ± 2.2 |
| ON | 11.4 ± 2.4 | 10.0 ± 2.7 | 11.3 ± 3.3 | 10.0 ± 2.8 | 10.7 ± 1.1 | 10.8 ± 2.6 | 8.1 ± 2.7 | 12.0 ± 2.2 | 10.5 ± 2.5 |
| QC | 11.0 ± 1.6 | 9.6 ± 2.1 | 10.1 ± 2.2 | 8.9 ± 1.6 | 11.3 ± 0.8 | 10.3 ± 1.6 | 5.6 ± 1.4 | 11.1 ± 1.2 | 9.7 ± 1.6 |
| NS | 9.0 ± 1.8 | 7.4 ± 2.0 | 7.4 ± 2.2 | 7.2 ± 1.6 | 10.3 ± 0.8 | 8.3 ± 1.6 | 4.6 ± 1.6 | 9.8 ± 1.4 | 8.0 ± 1.7 |
| NB | 11.0 ± 1.7 | 9.6 ± 1.7 | 10.6 ± 2.1 | 9.7 ± 1.5 | 11.1 ± 0.8 | 10.8 ± 1.4 | 7.0 ± 1.5 | 12.0 ± 1.2 | 10.2 ± 1.5 |
| PE | 11.6 ± 1.6 | 9.9 ± 1.6 | 11.4 ± 2.2 | 10.3 ± 1.1 | 11.1 ± 0.9 | 10.7 ± 1.5 | 6.5 ± 1.9 | 12.3 ± 1.0 | 10.5 ± 1.3 |
| NL | 11.6 ± 2.6 | 9.6 ± 2.3 | 11.1 ± 3.7 | 9.7 ± 2.5 | 11.3 ± 0.9 | 10.4 ± 2.4 | 5.5 ± 0.4 | 11.6 ± 2.1 | 10.1 ± 2.4 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
van Ballegooie, C.; Heroux, D.; Hoang, P.; Garg, S. Assessing the Functional Accessibility, Actionability, and Quality of Patient Education Materials from Canadian Cancer Agencies. Curr. Oncol. 2023, 30, 1439-1449. https://doi.org/10.3390/curroncol30020110
van Ballegooie C, Heroux D, Hoang P, Garg S. Assessing the Functional Accessibility, Actionability, and Quality of Patient Education Materials from Canadian Cancer Agencies. Current Oncology. 2023; 30(2):1439-1449. https://doi.org/10.3390/curroncol30020110
Chicago/Turabian Stylevan Ballegooie, Courtney, Devon Heroux, Peter Hoang, and Sarthak Garg. 2023. "Assessing the Functional Accessibility, Actionability, and Quality of Patient Education Materials from Canadian Cancer Agencies" Current Oncology 30, no. 2: 1439-1449. https://doi.org/10.3390/curroncol30020110
APA Stylevan Ballegooie, C., Heroux, D., Hoang, P., & Garg, S. (2023). Assessing the Functional Accessibility, Actionability, and Quality of Patient Education Materials from Canadian Cancer Agencies. Current Oncology, 30(2), 1439-1449. https://doi.org/10.3390/curroncol30020110





