Abstract
Second primary malignancies (SPM) are described as any primary, not synchronous, malignancy arising in a different anatomical district, with confirmed histological diagnosis. Age at diagnosis, previous non-thyroidal primary malignancy, and radioactive iodine (RAI) therapy have been proposed as independent risk factors for SPM. RAI therapy is a standard treatment for moderate-high risk differentiated thyroid cancer (DTC), and its effect on the development of SPM has become a critical topic in DTC treatment. The purpose of this retrospective single-center study was to investigate the occurrence and the possible association of non-thyroidal SPM diagnosed after DTC and RAI therapy in a cohort of 1326 consecutive DTC patients referred at our Institution for RAI treatment from 1993 to 2009. Eighty-nine patients with ages ≤ 18 years at the time of DTC diagnosis or with a follow-up of ≤12 months were excluded from the final analysis. All patients underwent a complete clinical and hematological follow-up every 6 months for a minimum of 12 months. During follow-up (mean 89 ± 73 months), 25 patients (2%) had an SPM diagnosis (mean 133 ± 73 months). The most common site of the second malignancy was the breast, accounting for 32% of all SPM, followed by colon-rectal cancer (16%), leukemia, and gynecological and kidney cancer (4%). At Cox univariable regression analysis, age at DTC diagnosis (p < 0.001), age ≥55 years (p < 0.001) and follow-up duration (p < 0.004) were associated with SPM onset, while no significant association was observed with the administered activity of radioiodine. In conclusion, our data suggest that the older a person gets, the more sharply the likelihood of developing additional diseases, such as PMS, increases. Similarly, for follow-up, the more a patient is followed up clinically over time, the higher the risk of new diagnoses increases.
1. Introduction
Differentiated thyroid cancer (DTC) is estimated to be the sixth most common cancer in 2021, with incidence rates of 10.1 per 100,000 women and 3.1 per 100,000 men and mortality rates of 0.5 per 100,000 women and 0.3 per 100,000 men [1,2,3,4,5,6]. The diagnosis of DTC is rapidly rising with small papillary thyroid carcinoma, with an improved prognosis [1,2,3,4,5,6]. The survival rate of DTC in Italy improved from 91% to 99% (from 1970 to 2004) [5].
Second primary malignancies (SPM), described as any primary, not synchronous, malignancy arising in a different anatomical district with confirmed histological diagnosis, is reported in patients with DTC [5]. Actually, different incidences of SPM have been previously reported, ranging from 0.5% to 22% [7,8,9,10,11,12,13,14,15,16,17,18,19,20]. Moreover, several factors can influence the incidence of SPM in patients with DTC. The time elapsed between DTC diagnosis and SPM has proved to be relevant, varying from 2 months up to over 2 years of follow-up, with the risk of SPM being higher in DTC survivors compared to the cancer risk in the general population [5]. Age at diagnosis, previous non-thyroidal primary malignancy, and radioactive iodine (RAI) therapy have been proposed as independent risk factors for SPM [5]. RAI therapy is a standard treatment for moderate-high-risk DTC [21,22,23], and its effect on the development of SPM has become a critical topic in DTC treatment. An increased risk of SPM was reported in a large-scale cohort study, but the development of SPM after RAI administration was not clearly demonstrable [24]. While some studies report that a higher SPM risk is associated particularly with high cumulative 131I doses [7,8,9,10], in other studies, no association between RAI therapy and the risk of SPM was found [13,25,26]. Hence, the relationship between RAI therapy and SPM remains controversial.
The purpose of this study was to investigate the occurrence and the possible association of non-thyroidal SPM diagnosed after DTC and RAI therapy in a retrospective cohort study.
2. Materials and Methods
2.1. Study Cohort
We performed a retrospective single-center study in a cohort of 1326 consecutive DTC patients who were referred to our Institution for RAI treatment and follow-up of DTC from 1993 to 2009. Demographic, clinical, surgical, and pathological data were noted from clinical records, including the age at the time of DTC diagnosis, the extent of surgery, the administered RAI dose, and the latest date of follow-up. According to the American Thyroid Association risk stratification [6], the activity administered in low-risk patients ranged from 1110 to 2220 MBq, in intermediate-risk patients from 2479 to 3700 MBq and in high-risk patients from 4440 to 7400 MBq.
2.2. Follow-Up
All patients underwent a complete clinical and hematological follow-up every 6 months for a minimum of 12 months (mean 89 ± 73 months). SPM was described as any primary, not synchronous, malignancy arising in a different anatomical district with a confirmed histological diagnosis. The timing of SPM occurrence with respect to DTC diagnosis was chosen to be more than 12 months after DTC. The SPM diagnosed within 12 months of RAI administration was considered synchronous and excluded from our analysis. The date of recurrence, SPM diagnosis and most recent outpatient visit were recorded as follow-up duration. If patient death occurred during follow-up, it was noted.
2.3. Statistical Analysis
Continuous data are expressed as mean ± standard deviation and categorical data as a percentage. Comparison between groups was performed with unpaired t-test and Chi-square test as appropriate. A p-value < 0.05 was considered statistically significant. Univariable Cox regression analysis was performed for each variable. Only variables showing a p-value < 0.05 at univariable analysis were considered statistically significant. Statistical analysis was performed with Stata 15.1 software (StataCorp, College Station, TX, USA).
3. Results
None of the patients potentially eligible for the study refused to participate, and all patients were able to sustain the examination. From the 1326 patients available from the analysis, 89 subjects with age ≤ 18 years at the time of DTC diagnosis or with a follow-up ≤12 months were excluded from the final analysis leaving 1237 patients (985 women, 252 men; mean age of 45 ± 14) for the final analysis (Figure 1).
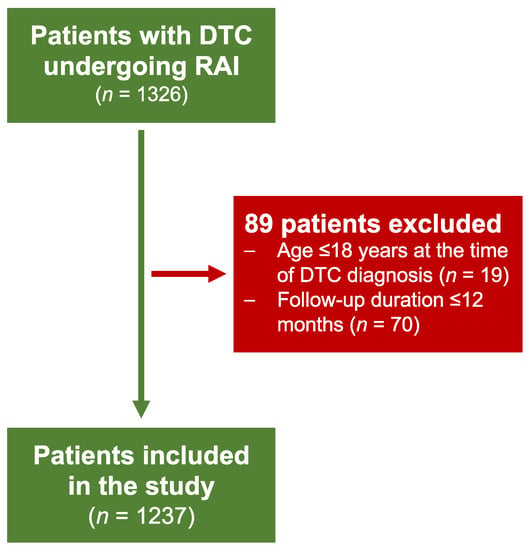
Figure 1.
Studied population.
Baseline characteristics of the patient population, histological characteristics, follow-up duration and dose administration, are summarized in Table 1.

Table 1.
Clinical characteristics in the overall patient population according to SPM occurrence.
The mean initial RAI dose is 3552 ± 1110 MBq The mean number of treatments is 1.44 ± 1.067, and the average treatment interval is 25 ± 2 months.
As shown in Table 1, during follow-up (mean 89 ± 73 months), 25 patients (2%) had an SPM diagnosis (mean 133 ± 73 months). The mean age of these patients (55 ± 16 years) was lower compared to those without SPM (45 ± 14, p < 0.0001), while no differences in gender and in histological type were found (Table 1). Moreover, no significant difference was observed in the total administered 131I activity (6364 ± 5176 MBq vs. 5710 ± 5820 MBq). Interestingly, follow-up duration was significantly longer in patients experiencing SPM compared to those without documented SPM (133 ± 73 MBq vs. 89 ± 73, p = 0.003).
SPM histology and number are described in Table 2, along with the 131I activity administered. The most common site of the SPM was the breast, accounting for 32% of all SPM, followed by colon-rectal cancer (16%), leukemia, and gynecological and kidney cancer (4%). To note, only one out of the eight female patients developing breast cancer was of childbearing age, while the other seven were in postmenopausal age at the time of RAI, further supporting data that excludes a potential relationship between RAI and breast cancer development.

Table 2.
Observed second primary malignancies and RAI activity in 25 patients.
At Cox univariable regression analysis, as described in Table 3, increasing age at the DTC diagnosis (p < 0.001) and follow-up duration (p < 0.005) were the only factors significantly associated with SPM onset.

Table 3.
Univariable predictors of SPM.
Of note, only 11 out of 25 patients showed SPM. By mean, 44% of the subjects with the event had the secondary malignancy diagnosis within five years of RAI therapy.
At the end of the follow-up, 25 patients had died. Among these, 2 patients died due to SPM, and 23 patients died due to non-oncological reasons. There were 20 patients who died from cardiovascular events and 3 patients who died from infection accidents.
4. Discussion
In the present study, a relatively low percentage of patients (2%) showed SPM during follow-up. According to data available from the Italian Tumor Registry Association (AIRTUM) on https://www.registri-tumori.it/cms (accessed on 1 September 2022), it has been reported that the number of observed second cancers in patients with DTC in the Italian population is 404/12,866 patients overall, with a frequency of 3% of patients showing an SPM after DTC. Our findings are thus in line with Italian data. Age at DTC diagnosis and duration of follow-up were the only significant factors associated with the development of SPM after RAI. This finding is not surprising given the excellent long-life expectancy of the investigated population. It becomes clear that a longer follow-up certainly has a better chance of bringing out new diagnoses such as SPMs, especially in patients on surveillance programs, as in the case of patients with DTC [12,13,15].
Discordant data regarding the development of SPM in patients treated with RAI have been reported [7,8,9,10,11,12,13,14,15,16,17,18,19,20,27]. Undeniably, the body of evidence provided by literature on this topic shows a wide heterogeneity in methods and results [7,8,9,10,11,12,13,14,15,16,17,18,19,20,27]. To date, the risk of developing SPM after an RAI cannot be excluded a priori, but it is expected to be low [10,11,12,17,18,20].
Our findings are consistent with those from Cappagli et al. [13], who retrospectively evaluated the risk of developing SPM in 1096 consecutive DTC patients after RAI treatment, observing that only 7% of patients experienced an SPM. This investigation demonstrates that while the cumulative dose of 131I is not significantly associated with the development of an SPM, only the duration of follow-up shows a significant relationship with the risk of an SPM after DTC supporting the idea that a long follow-up determines more effective health surveillance including SPM diagnosis. Likewise, Mei et al. [12] found that 4% of 104,026 DTC survivors developed SPM during the follow-up. The overall risk of SPM associated with RAI increased with age at DTC diagnosis and decreased after two years from RAI [12].
Furthermore, a recent meta-analysis evaluated the risk of breast cancer in patients with DTC receiving RAI taking into consideration 14 studies [26] and reported that the pooled risk of primary breast cancer after a long-term follow-up is not higher than the risk observed in those not treated with RAI. [26].
Crocetti et al. [25], found that the standardized incidence ratio of SPM on an Italian cohort of 276,100 patients with DTC not treated with RAI was 1.16. This finding is consistent with the results of the present investigation carried out in a population who underwent RAI therapy, suggesting that this treatment does not influence the risk of SPM.
On the other hand, Brown et al. [15] evaluated a total of 30,278 DTC patients, for a median follow-up of 103 months, with 2158 (7%) showing SPM. A greater significant risk of SPM was found for patients treated with RAI as compared to those not treated. Similarly, Rubino et al. [8] evaluated a European cohort of 6841 DTC patients with a mean age of 44 years, with an overall increased risk of SPM of 27% as compared to the general population. An increased risk of SPM was associated with the increasing cumulative activity of 131I administered.
Thus, on the one hand, our data demonstrate a low number of SPM. On the other, larger cohort studies have reported higher rates of SPM. However, given the observational retrospective nature of the present analysis, some events would have been missed on follow-up, explaining a slight underestimation of SMPs in our investigation. Indeed, within DTC follow-up, the enrolled patients were not routinely referred to clinical and imaging tests that were not directly related to DTC surveillance.
Hong et al. [27], in a multicenter retrospective study, analyzed a total of 3106 DTC patients who underwent RAI. A total of 183 SPM, which included 162 solid and 21 hematologic cancers, occurred in 173 patients (5.6%). A multivariate analysis identified independent prognostic factors for the development of SPM, including age at RAI, male gender, and total cumulative dose over 200 mCi.
The incidence of SPM in the present study is very low compared to that found in some studies described in the literature [7,8,13,14,15,19]. This difference could be explained by considering the characteristics of the current study population, such as the exclusion of pediatric patients, with a more aggressive tumor phenotype and the follow-up length.
For some authors [12,13,15], the latency time is an important factor that influences SPM development. However, in our sample, only 44% of the subjects with SPM had the secondary malignancy diagnosis within five years of the RAI therapy.
Another factor worth considering is the 131I cumulative activity dose. The present investigation demonstrates that 131I cumulative activity dose is not associated with SPM development in DTC patients after RAI therapy, even considering different administered activity categories. This finding is in agreement with numerous prior studies [5,11,12,13,14,19,20,27,28,29,30]. However, in the study by Hong et al. [27] total cumulative dose over 200 mCi was significantly associated with SPM development. In the same way, Lang et al. [7] and Rubino et al. [8] found an increased risk of SPM with the growing cumulative activity of 131I administered. Therefore, the association between RAI and the risk of SPM development in DTC patients is still controversial. It is certainly very important that every patient must be contextualized and deserves a personal medical evaluation based on their genetic and clinical background [5,7,8,9,10,11,12,13,14,15,16,17,18,19,20]. With regard to women, in the studied population, only one out of the eight female patients developing breast cancer was of childbearing age, while the other seven were in postmenopausal age at the time of RAI, further supporting data that excludes a potential relationship between RAI and breast cancer development. This finding is consistent with a recent meta-analysis [26] demonstrating that patients with DTC treated with RAI do not have a higher risk of primary breast cancer compared to those not treated with RAI.
The results of our study suggest that the older a person gets, the more sharply the likelihood of developing additional diseases, such as SPM, increases.
In this context, it should be considered that the pediatric population has been excluded from the final analysis in light of known differences between adult and pediatric DTC regarding clinical, molecular, and pathological characteristics [31]. Thus, specific investigations for the pediatric population are needed. We excluded such a population that will be the object of a different study to avoid any bias in the results interpretation.
Similarly, for follow-up, the more a patient is followed up clinically over time, the higher the risk of new diagnoses increases.
5. Conclusions
In the present study, only increasing age at the DTC diagnosis and follow-up length were significantly associated with SPM onset. On the contrary, 131I cumulative activity was not associated with SPM development. Breast cancer was the most common secondary non-thyroid cancer. Our data can also be read in light of the long-life expectancy of patients with DTC, making the malignancy rate of this patient category like general population findings. The high incidence of breast cancer in our cohort of patients can be explained by the high prevalence (i.e., 80%) of women enrolled.
Author Contributions
All authors attest that they meet the current International Committee of 278 Medical Journal Editors (ICMJE) criteria for Authorship. L.P. (Leandra Piscopo), C.N., E.Z., M.M., P.T., L.P. (Leonardo Pace), F.M., S.M., A.C. and M.K. conceptualized the paper; L.P. (Leandra Piscopo), C.N., F.V. and M.K. drafted the manuscript; and all the authors revised and commented on the paper and approved the final version of the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki. Approval Code: 270109/09; Approval Date: 27 January 2009.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to privacy restrictions.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Vaccarella, S.; Lortet-Tieulent, J.; Colombet, M.; Davies, L.; Stiller, C.A.; Schüz, J.; Togawa, K.; Bray, F.; Franceschi, S.; Maso, L.D.; et al. Global Patterns and Trends in Incidence and Mortality of Thyroid Cancer in Children and Adolescents: A Population-Based Study. Lancet Diabetes Endocrinol. 2021, 9, 144–152. [Google Scholar] [CrossRef] [PubMed]
- Pizzato, M.; Li, M.; Vignat, J.; Laversanne, M.; Singh, D.; La Vecchia, C.; Vaccarella, S. The Epidemiological Landscape of Thyroid Cancer Worldwide: GLOBOCAN Estimates for Incidence and Mortality Rates in 2020. Lancet Diabetes Endocrinol. 2022, 10, 264–272. [Google Scholar] [CrossRef] [PubMed]
- Mao, Y.; Xing, M. Recent Incidences and Differential Trends of Thyroid Cancer in the USA. Endocr. Relat. Cancer 2016, 23, 313–322. [Google Scholar] [CrossRef] [PubMed]
- Elisei, R.; Molinaro, E.; Agate, L.; Bottici, V.; Masserini, L.; Ceccarelli, C.; Lippi, F.; Grasso, L.; Basolo, F.; Bevilacqua, G.; et al. Are the Clinical and Pathological Features of Differentiated Thyroid Carcinoma Really Changed over the Last 35 Years? Study on 4187 Patients from a Single Italian Institution to Answer This Question. J. Clin. Endocrinol. Metab. 2010, 95, 1516–1527. [Google Scholar] [CrossRef] [PubMed]
- Reinecke, M.J.; Ahlers, G.; Burchert, A.; Eilsberger, F.; Flux, G.D.; Marlowe, R.J.; Mueller, H.-H.; Reiners, C.; Rohde, F.; van Santen, H.M.; et al. Second Primary Malignancies Induced by Radioactive Iodine Treatment of Differentiated Thyroid Carcinoma—A Critical Review and Evaluation of the Existing Evidence. Eur. J. Nucl. Med. Mol. Imaging 2022, 49, 3247–3256. [Google Scholar] [CrossRef]
- Haugen, B.R.; Alexander, E.K.; Bible, K.C.; Doherty, G.M.; Mandel, S.J.; Nikiforov, Y.E.; Pacini, F.; Randolph, G.W.; Sawka, A.M.; Schlumberger, M.; et al. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid 2016, 26, 1–133. [Google Scholar] [CrossRef]
- Lang, B.H.-H.; Wong, I.O.L.; Wong, K.P.; Cowling, B.J.; Wan, K.-Y. Risk of Second Primary Malignancy in Differentiated Thyroid Carcinoma Treated with Radioactive Iodine Therapy. Surgery 2012, 151, 844–850. [Google Scholar] [CrossRef]
- Rubino, C.; de Vathaire, F.; Dottorini, M.E.; Hall, P.; Schvartz, C.; Couette, J.E.; Dondon, M.-G.; Abbas, M.T.; Langlois, C.; Schlumberger, M. Second Primary Malignancies in Thyroid Cancer Patients. Br. J. Cancer 2003, 89, 1638–1644. [Google Scholar] [CrossRef]
- Silva-Vieira, M.; Carrilho Vaz, S.; Esteves, S.; Ferreira, T.C.; Limbert, E.; Salgado, L.; Leite, V. Second Primary Cancer in Patients with Differentiated Thyroid Cancer: Does Radioiodine Play a Role? Thyroid 2017, 27, 1068–1076. [Google Scholar] [CrossRef]
- Khang, A.R.; Cho, S.W.; Choi, H.S.; Ahn, H.Y.; Yoo, W.S.; Kim, K.W.; Kang, K.W.; Yi, K.H.; Park, D.J.; Lee, D.S.; et al. The Risk of Second Primary Malignancy Is Increased in Differentiated Thyroid Cancer Patients with a Cumulative 131I Dose over 37 GBq. Clin. Endocrinol. 2015, 83, 117–123. [Google Scholar] [CrossRef]
- Al-Qahtani, K.H.; Al-Asiri, M.; Tunio, M.A.; Aljohani, N.J.; Bayoumi, Y.; Al-Hussain, H.; Maklad, A.M. Prevalence and Treatment Outcomes of Second Primary Malignancies in Saudi Patients with Differentiated Thyroid Cancers. Saudi Med. J. 2015, 36, 442–448. [Google Scholar] [CrossRef]
- Mei, X.; Yao, X.; Feng, F.; Cheng, W.; Wang, H. Risk and Outcome of Subsequent Malignancies after Radioactive Iodine Treatment in Differentiated Thyroid Cancer Patients. BMC Cancer 2021, 21, 543. [Google Scholar] [CrossRef]
- Cappagli, V.; Caldarella, A.; Manneschi, G.; Piaggi, P.; Bottici, V.; Agate, L.; Molinaro, E.; Bianchi, F.; Elisei, R. Nonthyroidal Second Primary Malignancies in Differentiated Thyroid Cancer Patients: Is the Incidence Increased Comparing to the General Population and Could It Be a Radioiodine Therapy Consequence? Int. J. Cancer 2020, 147, 2838–2846. [Google Scholar] [CrossRef]
- Hakala, T.T.; Sand, J.A.; Jukkola, A.; Huhtala, H.S.; Metso, S.; Kellokumpu-Lehtinen, P.-L. Increased Risk of Certain Second Primary Malignancies in Patients Treated for Well-Differentiated Thyroid Cancer. Int. J. Clin. Oncol. 2016, 21, 231–239. [Google Scholar] [CrossRef]
- Brown, A.; Chen, J.; Hitchcock, Y.; Szabo, A.; Shrieve, D.C.; Tward, J. The Risk of Second Primary Malignancies up to Three Decades after the Treatment of Differentiated Thyroid Cancer. J. Clin. Endocrinol. Metab. 2008, 93, 504–515. [Google Scholar] [CrossRef]
- Iyer, N.G.; Morris, L.G.; Tuttle, R.M.; Shaha, A.R.; Ganly, I. Rising incidence of second cancers in patients with low-risk (T1N0) thyroid cancer who receive radioactive iodine therapy. Cancer 2011, 117, 4439–4446. [Google Scholar] [CrossRef]
- Molenaar, R.J.; Sidana, S.; Radivoyevitch, T.; Advani, A.S.; Gerds, A.; Carraway, H.E.; Angelini, D.; Kalaycio, M.; Nazha, A.; Adelstein, D.J.; et al. Risk of Hematologic Malignancies After Radioiodine Treatment of Well-Differentiated Thyroid Cancer. J. Clin. Oncol. 2018, 36, 1831–1839. [Google Scholar] [CrossRef]
- Molenaar, R.J.; Pleyer, C.; Radivoyevitch, T.; Sidana, S.; Godley, A.; Advani, A.S.; Gerds, A.T.; Carraway, H.E.; Kalaycio, M.; Nazha, A.; et al. Risk of developing chronic myeloid neoplasms in well-differentiated thyroid cancer patients treated with radioactive iodine. Leukemia 2018, 32, 952–959. [Google Scholar] [CrossRef]
- Berthe, E.; Henry-Amar, M.; Michels, J.-J.; Rame, J.-P.; Berthet, P.; Babin, E.; Icard, P.; Samama, G.; Mahoudeau, J. Risk of Second Primary Cancer Following Differentiated Thyroid Cancer. Eur. J. Nucl. Med. Mol. Imaging 2004, 31, 685–691. [Google Scholar] [CrossRef]
- Kim, S.; Bang, J.-I.; Boo, D.; Kim, B.; Choi, I.Y.; Ko, S.; Yoo, I.R.; Kim, K.; Kim, J.; Joo, Y.; et al. Second Primary Malignancy Risk in Thyroid Cancer and Matched Patients with and without Radioiodine Therapy Analysis from the Observational Health Data Sciences and Informatics. Eur. J. Nucl. Med. Mol. Imaging 2022, 49, 3547–3556. [Google Scholar] [CrossRef]
- Pacini, F.; Basolo, F.; Bellantone, R.; Boni, G.; Cannizzaro, M.A.; De Palma, M.; Durante, C.; Elisei, R.; Fadda, G.; Frasoldati, A.; et al. Italian Consensus on Diagnosis and Treatment of Differentiated Thyroid Cancer: Joint Statements of Six Italian Societies. J. Endocrinol. Investig. 2018, 41, 849–876. [Google Scholar] [CrossRef] [PubMed]
- Klain, M.; Nappi, C.; Zampella, E.; Cantoni, V.; Green, R.; Piscopo, L.; Volpe, F.; Manganelli, M.; Caiazzo, E.; Petretta, M.; et al. Ablation Rate after Radioactive Iodine Therapy in Patients with Differentiated Thyroid Cancer at Intermediate or High Risk of Recurrence: A Systematic Review and a Meta-Analysis. Eur. J. Nucl. Med. Mol. Imaging 2021, 48, 4437–4444. [Google Scholar] [CrossRef] [PubMed]
- Klain, M.; Ricard, M.; Leboulleux, S.; Baudin, E.; Schlumberger, M. Radioiodine Therapy for Papillary and Follicular Thyroid Carcinoma. Eur. J. Nucl. Med. Mol. Imaging 2002, 29, S479–S485. [Google Scholar] [CrossRef] [PubMed]
- Schonfeld, S.J.; Morton, L.M.; de González, A.B.; Curtis, R.E.; Kitahara, C.M. Risk of Second Primary Papillary Thyroid Cancer among Adult Cancer Survivors in the United States, 2000–2015. Cancer Epidemiol. 2020, 64, 101664. [Google Scholar] [CrossRef] [PubMed]
- Crocetti, E.; Mattioli, V.; Buzzoni, C.; Franceschi, S.; Serraino, D.; Vaccarella, S.; Ferretti, S.; Busco, S.; Fedeli, U.; Varvarà, M.; et al. Risk of thyroid as a first or second primary cancer. A population-based study in Italy, 1998–2012. Cancer Med. 2021, 10, 6855–6867. [Google Scholar] [CrossRef]
- Nappi, C.; Klain, M.; Cantoni, V.; Green, R.; Piscopo, L.; Volpe, F.; Maurea, S.; Petretta, M.; Cuocolo, A. Risk of Primary Breast Cancer in Patients with Differentiated Thyroid Cancer Undergoing Radioactive Iodine Therapy: A Systematic Review and Meta-Analysis. Eur. J. Nucl. Med. Mol. Imaging 2022, 49, 1630–1639. [Google Scholar] [CrossRef]
- Hong, C.M.; Shin, J.-Y.; Kim, B.I.; Song, H.-C.; Yoon, J.-K.; Won, K.S.; Kim, S.-M.; Cho, I.H.; Jeong, S.Y.; Lee, S.-W. Incidence rate and factors associated with the development of secondary cancers after radioiodine therapy in differentiated thyroid cancer: A multicenter retrospective study. Eur. J. Nucl. Med. Mol. Imaging 2022, 49, 1661–1670. [Google Scholar] [CrossRef]
- Sawka, A.; Thabane, L.; Parlea, L.; Ibrahim-Zada, I.; Tsang, R.; Brierley, J.D.; Straus, S.; Ezzat, S.; Goldstein, D.P. Second Primary Malignancy Risk After Radioactive Iodine Treatment for Thyroid Cancer: A Systematic Review and Meta-Analysis. Thyroid 2009, 19, 451–457. [Google Scholar] [CrossRef]
- Verburg, F.A.; Hoffmann, M.; Iakovou, I.; Konijnenberg, M.W.; Mihailovic, J.; Gabina, P.M.; Ovčariček, P.P.; Reiners, C.; Vrachimis, A.; Zerdoud, S.; et al. Errare humanum est, sed in errare perseverare diabolicum: Methodological errors in the assessment of the relationship between I-131 therapy and possible increases in the incidence of malignancies. Eur. J. Nucl. Med. Mol. Imaging 2020, 47, 519–522. [Google Scholar] [CrossRef]
- Tulchinsky, M.; Binse, I.; Campennì, A.; Dizdarevic, S.; Giovanella, L.; Jong, I.; Kairemo, K.; Kim, C.K. Radioactive Iodine Therapy for Differentiated Thyroid Cancer: Lessons from Confronting Controversial Literature on Risks for Secondary Malignancy. J. Nucl. Med. 2018, 59, 723–725. [Google Scholar] [CrossRef]
- Lebbink, C.A.; Links, T.P.; Czarniecka, A.; Dias, R.P.; Elisei, R.; Izatt, L.; Krude, H.; Lorenz, K.; Luster, M.; Newbold, K.; et al. 2022 European Thyroid Association Guidelines for the management of pediatric thyroid nodules and differentiated thyroid carcinoma. Eur. Thyroid. Thyroid. Thyroid. J. 2022, 11, e220146. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).