Coaxial Drainage versus Standard Chest Tube after Pulmonary Lobectomy: A Randomized Controlled Study
Abstract
:1. Introduction
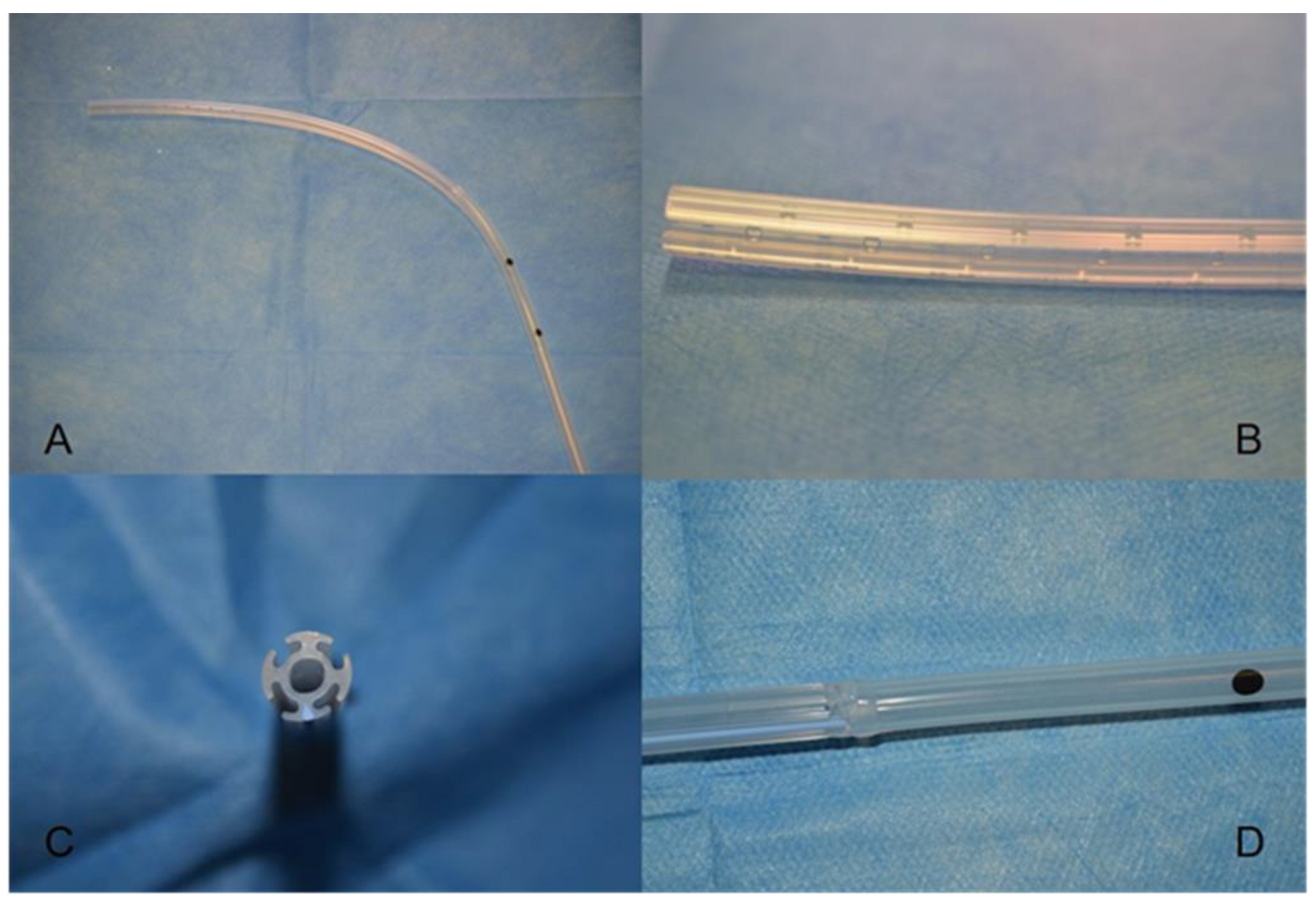
2. Materials and Methods
2.1. Study Population
2.2. Clinical Data
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| SDC | Smart Drain Coaxial |
| ST | Standard tubes |
| ICU | Intensive care unit |
| VAS | Visual analogue scale |
| CXR | Chest X-ray |
| POD | Postoperative day |
| IQR | Inter-quartile range |
| SD | Standard deviation |
| PALs | Prolonged air leaks |
| ERAS | Enhanced recovery after surgery |
References
- Alex, J.; Ansari, J.; Bahalkar, P.; Agarwala, S.; Rehman, M.U.; Saleh, A.; Cowen, M. Comparison of the immediate postoperative outcome of using the conventional two drains versus a single drain after lobectomy. Ann. Thorac. Surg. 2003, 76, 1046–1049. [Google Scholar] [CrossRef]
- Gómez-Caro, A.; Roca, M.J.; Torres, J.; Cascales, P.; Terol, E.; Castañer, J.; Piñero, A.; Parrilla, P. Successful use of a single chest drain postlobectomy instead of two classical drains: A randomized study. Eur. J. Cardiothorac Surg. 2006, 29, 562–566. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Okur, E.; Baysungur, V.; Tezel, C.; Sevilgen, G.; Ergene, G.; Gokce, M.; Halezeroglu, S. Comparison of the single or double chest tube applications after pulmonary lobectomies. Eur. J. Cardiothorac Surg. 2009, 35, 32–35. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, M.; Sagawa, M.; Usuda, K.; Machida, Y.; Ueno, M.; Motono, N.; Sakuma, T. Postoperative drainage with one chest tube is appropriate for pulmonary lobectomy: A randomized trial. Tohoku J. Exp. Med. 2014, 232, 55–61. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rena, O.; Parini, S.; Papalia, E.; Massera, F.; Turello, D.; Baietto, G.; Casadio, C. The Redax (®) Coaxial Drain in pulmonary lobectomy: A study of efficacy. J. Thorac. Dis. 2017, 9, 3215–3221. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mammarappallil, J.G.; Anderson, S.A.; Danelson, K.A.; Stitzel, J.A.; Chiles, C. Estimation of Pleural Fluid Volumes on Chest Radiography Using Computed Tomography Volumetric Analysis: An Update of the Visual Prediction Rule. J. Thorac. Imaging 2015, 30, 336–339. [Google Scholar] [CrossRef] [PubMed]
- Hickey, G.L.; Dunning, J.; Seifert, B.; Sodeck, G.; Carr, M.J. Beyersdorf F on behalf of the EJCTS and ICVTS Editorial Committees Editor’s Choice: Statistical and data reporting guidelines for the European Journal of Cardio-Thoracic Surgery and the Interactive CardioVascular and Thoracic Surgery. Eur. J. Cardiothorac Surg. 2015, 48, 180–193. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Available online: https://www.rgs.mef.gov.it/_Documenti/VERSIONE-I/Attivit--i/Bilancio_di_previsione/Missioni_e_programmi_delle_ACdS/LaPrecedentestrutturadelbilancio468/Libro-verde-sulla-spesa-pubblica/Sanit-.pdf (accessed on 18 May 2022).
- Fell, S.C.; DeCamp, M.M. Technical aspects of lobectomy. In General Thoracic Surgery; Shields, T.W., LoCicero, J., III, Reed, C.E., Eds.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2009; pp. 421–444. [Google Scholar]
- Khan, I.H.; Vaughan, R. A national survey of thoracic surgical practice in the UK. Int. J. Clin. Pract. 1999, 53, 252–256. [Google Scholar] [PubMed]
- Brunelli, A.; Beretta, E.; Cassivi, S.D.; Cerfolio, R.; Detterbeck, F.; Kiefer, T.; Miserocchi, G.; Shrager, J.; Singhal, S.; Van Raemdonck, D.; et al. Consensus definitions to promote an evidence-based approach to management of the pleural space. A collaborative proposal by ESTS, AATS, STS, and GTSC. Eur. J. Cardiothorac Surg. 2011, 40, 291–297. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhou, N.; Deng, X.-F.; Liu, Q.-X.; Chen, Q.; Min, J.-X.; Dai, J.-G. Single chest tube drainage is superior to double chest tube drainage after lobectomy: A meta-analysis. J. Cardiothorac Surg. 2016, 11, 88. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- You, J.; Zhang, H.; Li, W.; Dai, N.; Zheng, Z. Single versus double chest drains after pulmonary lobectomy: A systematic review and meta-analysis. World J. Surg. Oncol. 2020, 18, 175. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.; Zhang, X.; Lv, D.; Li, M.; Sun, G. The single chest tube versus double chest tube application after pulmonary lobectomy: A systematic review and meta-analysis. J. Cancer Res. Ther. 2016, 12, C309–C316. [Google Scholar] [CrossRef] [PubMed]
- Filosso, P.L.; Sandri, A.; Guerrera, F.; Roffinella, M.; Bora, G.; Solidoro, P. Management of Chest Drains After Thoracic Resections. Thorac. Surg. Clin. 2017, 27, 7–11. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.S.; Khalpey, Z.; Daugherty, S.L.; Torabim, M.; Little, A.G. Factors in the Selection and Management of Chest Tubes After Pulmonary Lobectomy: Results of a National Survey of Thoracic Surgeons. Ann. Thorac. Surg. 2016, 101, 1082–1088. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shalli, S.; Saeed, D.; Fukamachi, K.; Gillinov, A.M.; Cohn, W.E.; Perrault, L.P.; Boyle, E.M. Chest tube selection in cardiac and thoracic surgery: A survey of chest tube-related complications and their management. J. Card. Surg. 2009, 24, 503–509. [Google Scholar] [CrossRef] [PubMed]
- Guerrera, F.; Filosso, P.L.; Pompili, C.; Olivetti, S.; Roffinella, M.; Imperatori, A.; Brunelli, A. Application of the coaxial smart drain in patients with a large air leak following anatomic lung resection: A prospective multicenter phase II analysis of efficacy and safety. J. Vis. Surg. 2018, 4, 26. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cerfolio, R.J.; Bryant, A.S. The management of chest tubes after pulmonary resection. Thorac. Surg. Clin. 2010, 20, 399–405. [Google Scholar] [CrossRef] [PubMed]
- Rogers, L.J.; Bleetmanm, D.; Messenger, D.E.; Joshi, N.A.; Wood, L.; Rasburn, N.J.; Batchelor, T.J.P. The impact of enhanced recovery after surgery (ERAS) protocol compliance on morbidity from resection for primary lung cancer. J. Thorac. Cardiovasc Surg. 2018, 155, 1843–1852. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Overall | Standard | Coaxial | p-Value | |
|---|---|---|---|---|
| n | 98 | 50 | 48 | |
| Age | 68.3 ± 7.4 | 69.0 ± 7.1 | 67.6 ± 7.8 | 0.21 |
| Male | 57 (58.2%) | 28 (56%) | 29 (60%) | 0.69 |
| Active Smokers | 73 (74.5%) | 38 (76.0%) | 35 (72.9%) | 0.66 |
| Lobe | 0.54 | |||
| Left lower lobe | 19 (19.4%) | 10 (10.2%) | 9 (9.2%) | |
| Left upper lobe | 20 (20.4%) | 8 (8.2%) | 12 (12.2%) | |
| Right lower lobe | 25 (25.5%) | 15 (15.3%) | 10 (10.2%) | |
| Right upper lobe | 34 (34.7%) | 17 (17.3%) | 17 (17.3%) | |
| Histology | 0.09 | |||
| Adenocarcinoma | 71 (72.5%) | 34 (34.7%) | 37 (37.8%) | |
| Squamous cell cancer | 11 (11.2%) | 9 (9.2%) | 2 (2.0%) | |
| Others | 16 (16.3%) | 7 (7.1%) | 9 (9.2%) | |
| Stage | ||||
| IA | 35 (35.7%) | 13 (13.3%) | 22 (22.4%) | 0.29 |
| IB | 23 (23.5%) | 13 (13.3%) | 10 (10.2%) | |
| IIA | 6 (6.1%) | 3 (3.1%) | 3 (3.1%) | |
| IIB | 15 (15.3%) | 11 (11.2%) | 4 (4.1%) | |
| IIIA | 10 (10.2%) | 4 (4.1%) | 6 (6.1%) | |
| IIIB | 2 (2.0%) | 1 (1.0%) | 1 (1.0%) | |
| IVa | 2 (2.0%) | 2 (2.0%) | 0 (0.0%) |
| Overall | Standard | Coaxial | p-Value | |
|---|---|---|---|---|
| Length of stay (days) | 6.7 ± 2.6 | 7.3 ± 3.1 | 6.1 ± 2.0 | 0.02 |
| Tube stay (days) | 5.0 ± 2.0 | 5.3 ± 2.2 | 4.7 ± 1.9 | 0.04 |
| Postoperative complications | ||||
| Overall | 18 (18.4%) | 10 (10.2%) | 8 (8.2%) | 0.67 |
| Persistent air leaks | 9 (9.2%) | 5 (5.1%) | 4 (4.0%) | 0.76 |
| Sputum retention | 4 (4.0%) | 2 (2.0%) | 2 (2.0%) | |
| Atrial Fibrillation | 2 (2.0%) | 2 (2.0%) | 0 (0.0%) | |
| Others | 3 (3.1%) | 1 (1.0%) | 2 (2.0%) | |
| ICU admission | 36 (100%) (36.7%) | 22 (22.4%) | 14 (14.3%) | 0.13 |
| ICU stay (days) | 1.2 ± 0.7 | 1.2 ± 0.6 | 1.1 ± 0.3 | 0.30 |
| Air leaks detection | ||||
| POD 1 | 27 (27.5%) | 15 (15.3%) | 12 (12.2%) | 0.58 |
| POD 3 | 14 (14.3%) | 9 (9.2%) | 5 (5.1%) | |
| Amount of drainage (mL) | ||||
| Overall | 1624.9 ± 718.5 | 1363.5 ± 692.2 | 0.07 | |
| POD 1 | 464.4 ± 143.0 | 407.9 ± 141.4 | 0.04 | |
| POD ≤ 3 | 374.2 ± 96.1 | 323.9 ± 94.5 | 0.01 | |
| Chest X-ray scale (grade) | ||||
| POD1 | 1.3 ± 0.8 | 1.1 ± 0.8 | 0.34 | |
| POD3 | 1.0 ± 0.9 | 0.9 ± 1.0 | 0.76 | |
| Post-removal | 1.3 ± 0.8 | 1.2 ± 1.1 | 0.65 | |
| Fluid retention rate (scale) | ||||
| POD1 | 16 (16.3%) | 9 (9.2%) | 0.13 | |
| POD3 | 13 (13.3%) | 13 (13.3%) | 0.90 | |
| Post-removal | 20 (20.4%) | 18 (18.4%) | 0.80 | |
| Pain (Visual Analogue Scale) | ||||
| POD 1 | 5.5 ± 1.9 | 4.6 ± 1.7 | 0.02 | |
| POD 3 | 4,0 ± 1.5 | 4.2 ± 1.8 | 0.70 | |
| POD 5 | 2.8 ± 1.6 | 2.4 ± 1.2 | 0.14 | |
| Tube Removal Complications | ||||
| Overall | 22 (22.4%) | 13 (13.3%) | 9 (9.2%) | 0.47 |
| Pneumothorax | 14 (14.3)%) | 8 (8.2%) | 6 (6.1%) | |
| Pleural Effusion | 5 (5.1%) | 3 (3.1%) | 2 (2.0%) | |
| Hydro-pneumothorax | 2 (2.0%) | 1 (1.0%) | 1 (1.0%) | |
| Subcutaneous emphysema | 1 (1.0%) | 1 (1.0%) | 0 (0.0%) | |
| Standard | Coaxial | Mean Difference | p-Value | |
|---|---|---|---|---|
| Chest tubes cost | 21.7 | 64.5 | 42.8 | |
| Drugs cost (mean) | 16 | 15.9 | 0.1 | |
| Hospital cost per days [8] | 674 | 674 | 0 | |
| Mean length of stay (days) | 7.3 | 6.1 | 1.2 | |
| Total cost | 5059 | 4273 | 786 | 0.04 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bassi, M.; Mottola, E.; Mantovani, S.; Amore, D.; Pagini, A.; Diso, D.; Vannucci, J.; Poggi, C.; De Giacomo, T.; Rendina, E.A.; et al. Coaxial Drainage versus Standard Chest Tube after Pulmonary Lobectomy: A Randomized Controlled Study. Curr. Oncol. 2022, 29, 4455-4463. https://doi.org/10.3390/curroncol29070354
Bassi M, Mottola E, Mantovani S, Amore D, Pagini A, Diso D, Vannucci J, Poggi C, De Giacomo T, Rendina EA, et al. Coaxial Drainage versus Standard Chest Tube after Pulmonary Lobectomy: A Randomized Controlled Study. Current Oncology. 2022; 29(7):4455-4463. https://doi.org/10.3390/curroncol29070354
Chicago/Turabian StyleBassi, Massimiliano, Emilia Mottola, Sara Mantovani, Davide Amore, Andreina Pagini, Daniele Diso, Jacopo Vannucci, Camilla Poggi, Tiziano De Giacomo, Erino Angelo Rendina, and et al. 2022. "Coaxial Drainage versus Standard Chest Tube after Pulmonary Lobectomy: A Randomized Controlled Study" Current Oncology 29, no. 7: 4455-4463. https://doi.org/10.3390/curroncol29070354
APA StyleBassi, M., Mottola, E., Mantovani, S., Amore, D., Pagini, A., Diso, D., Vannucci, J., Poggi, C., De Giacomo, T., Rendina, E. A., Venuta, F., & Anile, M. (2022). Coaxial Drainage versus Standard Chest Tube after Pulmonary Lobectomy: A Randomized Controlled Study. Current Oncology, 29(7), 4455-4463. https://doi.org/10.3390/curroncol29070354






