Health-Related Quality of Life following Total Thyroidectomy and Lobectomy for Differentiated Thyroid Carcinoma: A Systematic Review
Abstract
:1. Introduction
2. Methods
2.1. Literature Search
2.2. Screening and Eligibility Assessment of Articles
2.3. Inclusion Criteria
2.4. Exclusion Criteria
2.5. Quality Assessment and Risk of Bias
2.6. Definitions of TT vs. HT
2.7. HrQoL Model
3. Results
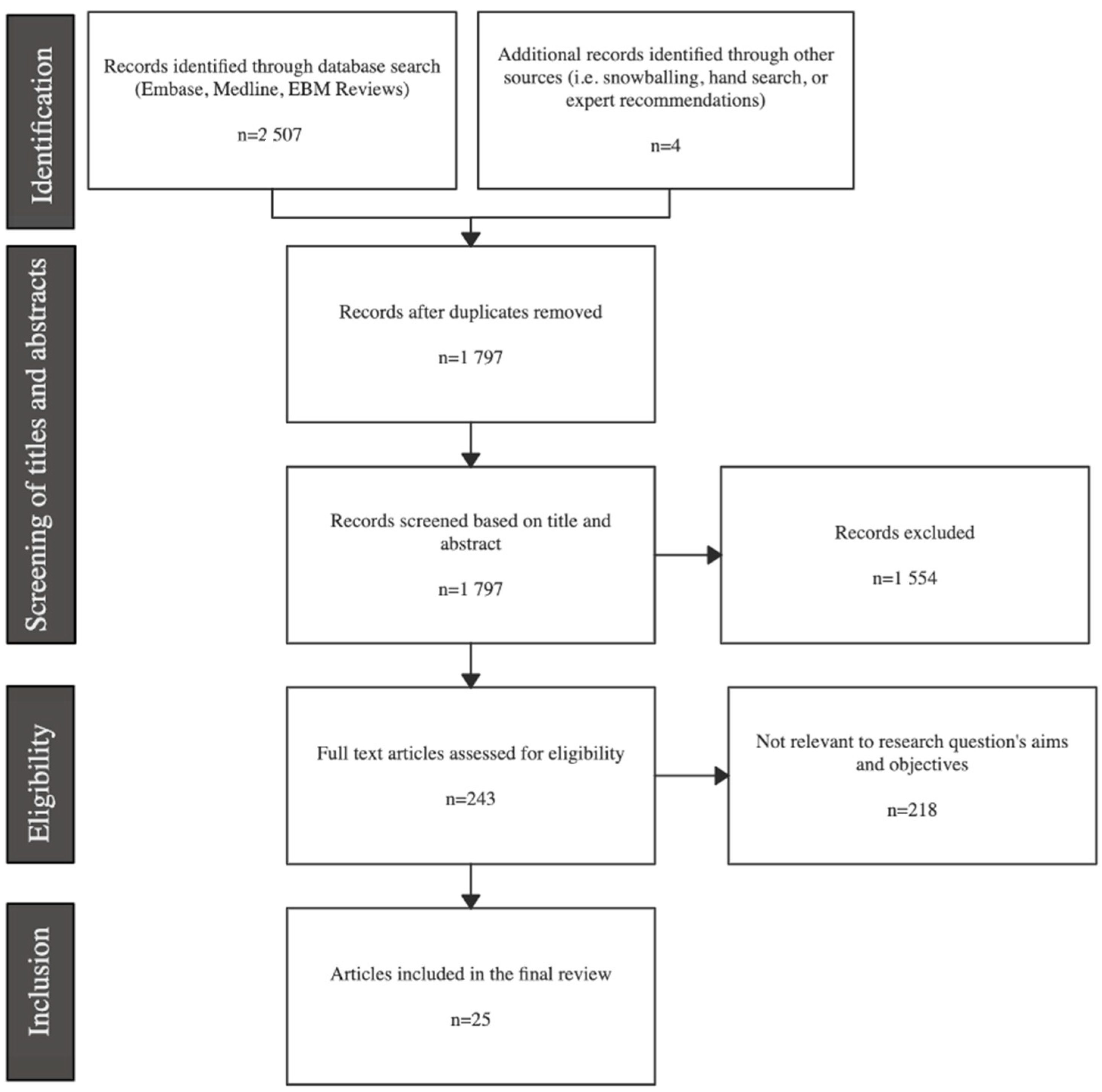
3.1. Search-Strategy Results
3.2. Study Characteristics
3.3. HrQoL Instruments
3.3.1. SF-36 (or RAND-36)
3.3.2. SF-12
3.3.3. SF-6D
3.3.4. EQ5D-5L
3.3.5. HUI2 and HUI 3
3.3.6. 15 D
3.3.7. FoP
3.3.8. FoP-Q-SF
3.3.9. ASC
3.3.10. EORTC QLQ-C30
3.3.11. EORTC QLQ-THY34
3.3.12. THYCA-QoL
3.3.13. KT-QoL
3.3.14. ThyPRO
3.3.15. Billewicz Score
3.3.16. MFI-20
3.3.17. PSQI
3.3.18. HADS
3.3.19. SDQ
3.3.20. State-Trait Anxiety Inventory
3.3.21. VHI
3.3.22. VAS
3.4. Quality Assessment
3.5. Physical HrQoL Component
3.6. Psychological HrQoL Component
3.7. Social HrQoL Component
3.8. Global HrQoL Component
3.9. Perspectives from Qualitative and Mixed Methods Studies
4. Discussion
4.1. Physical-Related HrQoL
4.2. Psychological-Related HrQoL
4.3. Social-Related HrQoL
4.4. Global HrQoL
4.5. Clinical Implications
4.6. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Davies, L.; Welch, H.G. Current thyroid cancer trends in the United States. JAMA Otolaryngol. Head Neck Surg. 2014, 140, 317–322. [Google Scholar] [CrossRef] [Green Version]
- La Vecchia, C.; Malvezzi, M.; Bosetti, C.; Garavello, W.; Bertuccio, P.; Levi, F.; Negri, E. Thyroid cancer mortality and incidence: A global overview. Int. J. Cancer 2015, 136, 2187–2195. [Google Scholar] [CrossRef] [PubMed]
- Sosa, J.A.; Hanna, J.W.; Robinson, K.A.; Lanman, R.B. Increases in thyroid nodule fine-needle aspirations, operations, and diagnoses of thyroid cancer in the United States. Surgery 2013, 154, 1420–1427. [Google Scholar] [CrossRef] [PubMed]
- Al-Qurayshi, Z.; Robins, R.; Hauch, A.; Randolph, G.W.; Kandil, E. Association of surgeon volume With outcomes and cost savings following thyroidectomy: A national forecast. JAMA Otolaryngol. Head Neck Surg. 2016, 142, 32–39. [Google Scholar] [CrossRef] [Green Version]
- National Cancer Institute Surveillance, Epidemiology and End Results Program. Cancer Stat Facts: Thyroid Cancer. Available online: https://seer.cancer.gov/statfacts/html/thyro.html (accessed on 26 February 2022).
- Tuttle, R.M.; Tala, H.; Shah, J.; Leboeuf, R.; Ghossein, R.; Gonen, M.; Brokhin, M.; Omry, G.; Fagin, J.A.; Shaha, A. Estimating risk of recurrence in differentiated thyroid cancer after total thyroidectomy and radioactive iodine remnant ablation: Using response to therapy variables to modify the initial risk estimates predicted by the new American Thyroid Association staging system. Thyroid 2010, 20, 1341–1349. [Google Scholar] [CrossRef]
- Chan, S.; Karamali, K.; Kolodziejczyk, A.; Oikonomou, G.; Watkinson, J.; Paleri, V.; Nixon, I.; Kim, D. Systematic review of recurrence rate after hemithyroidectomy for low-risk well-differentiated thyroid cancer. Eur. Thyr. J. 2020, 9, 73–84. [Google Scholar] [CrossRef] [PubMed]
- Haugen, B.R.; Alexander, E.K.; Bible, K.C.; Doherty, G.M.; Mandel, S.J.; Nikiforov, Y.E.; Pacini, F.; Randolph, G.W.; Sawka, A.M.; Schlumberger, M.; et al. 2015 american thyroid association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: The american thyroid association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid 2016, 26, 1–133. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Perros, P.; Boelaert, K.; Colley, S.; Evans, C.; Evans, R.M.; Gerrard Ba, G.; Gilbert, J.; Harrison, B.; Johnson, S.J.; Giles, T.E.; et al. Guidelines for the management of thyroid cancer. Clin. Endocrinol. 2014, 81 (Suppl. 1), 1–122. [Google Scholar] [CrossRef] [PubMed]
- Adam, M.A.; Pura, J.; Gu, L.; Dinan, M.A.; Tyler, D.S.; Reed, S.D.; Scheri, R.; Roman, S.A.; Sosa, J.A. Extent of surgery for papillary thyroid cancer is not associated with survival: An analysis of 61,775 patients. Ann. Surg. 2014, 260, 601–605. [Google Scholar] [CrossRef] [Green Version]
- Barney, B.M.; Hitchcock, Y.J.; Sharma, P.; Shrieve, D.C.; Tward, J.D. Overall and cause-specific survival for patients undergoing lobectomy, near-total, or total thyroidectomy for differentiated thyroid cancer. Head Neck 2011, 33, 645–649. [Google Scholar] [CrossRef]
- Mendelsohn, A.H.; Elashoff, D.A.; Abemayor, E.; St John, M.A. Surgery for papillary thyroid carcinoma: Is lobectomy enough? Arch. Otolaryngol. Head Neck Surg. 2010, 136, 1055–1061. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Haigh, P.I.; Urbach, D.R.; Rotstein, L.E. Extent of thyroidectomy is not a major determinant of survival in low- or high-risk papillary thyroid cancer. Ann. Surg. Oncol. 2005, 12, 81–89. [Google Scholar] [CrossRef] [PubMed]
- Hsiao, V.; Light, T.J.; Adil, A.A.; Tao, M.; Chiu, A.S.; Hitchcock, M.; Arroyo, N.; Fernandes-Taylor, S.; Francis, D.O. Complication rates of total thyroidectomy vs hemithyroidectomy for treatment of papillary thyroid microcarcinoma: A systematic review and meta-analysis. JAMA Otolaryngol. Head Neck Surg. 2022, 148, 531–539. [Google Scholar] [CrossRef] [PubMed]
- Rogers, S.N.; Mepani, V.; Jackson, S.; Lowe, D. Health-related quality of life, fear of recurrence, and emotional distress in patients treated for thyroid cancer. Br. J. Oral Maxillofac. Surg. 2017, 55, 666–673. [Google Scholar] [CrossRef]
- Singer, S.; Lincke, T.; Gamper, E.; Bhaskaran, K.; Schreiber, S.; Hinz, A.; Schulte, T. Quality of life in patients with thyroid cancer compared with the general population. Thyroid 2012, 22, 117–124. [Google Scholar] [CrossRef]
- Husson, O.; Haak, H.R.; Buffart, L.M.; Nieuwlaat, W.A.; Oranje, W.A.; Mols, F.; Kuijpens, J.L.; Coebergh, J.W.; van de Poll-Franse, L.V. Health-related quality of life and disease specific symptoms in long-term thyroid cancer survivors: A study from the population-based PROFILES registry. Acta Oncol. 2013, 52, 249–258. [Google Scholar] [CrossRef] [Green Version]
- Hoftijzer, H.C.; Heemstra, K.A.; Corssmit, E.P.; van der Klaauw, A.A.; Romijn, J.A.; Smit, J.W. Quality of life in cured patients with differentiated thyroid carcinoma. J. Clin. Endocrinol. Metab. 2008, 93, 200–203. [Google Scholar] [CrossRef] [Green Version]
- Applewhite, M.K.; James, B.C.; Kaplan, S.P.; Angelos, P.; Kaplan, E.L.; Grogan, R.H.; Aschebrook-Kilfoy, B. Quality of Life in Thyroid Cancer is Similar to That of Other Cancers with Worse Survival. World J. Surg. 2016, 40, 551–561. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ 2009, 339, b2535. [Google Scholar] [CrossRef] [Green Version]
- Strings Attached: CADTH Database Search Filters; CADTH: Ottawa, ON, Canada, 2021; Available online: https://www.cadth.ca/strings-attached-cadth-search-filters-database (accessed on 30 March 2022).
- Joanna Briggs Institute. Critical Appraisal Tools. Available online: https://jbi.global/critical-appraisal-tools (accessed on 30 March 2022).
- Bakas, T.; McLennon, S.M.; Carpenter, J.S.; Buelow, J.M.; Otte, J.L.; Hanna, K.M.; Ellett, M.L.; Hadler, K.A.; Welch, J.L. Systematic review of health-related quality of life models. Health Qual. Life Outcomes 2012, 10, 134. [Google Scholar] [CrossRef] [Green Version]
- Wilson, I.B.; Cleary, P.D. Linking clinical variables with health-related quality of life. A conceptual model of patient outcomes. JAMA 1995, 273, 59–65. [Google Scholar] [CrossRef] [PubMed]
- Lins, L.; Carvalho, F.M. SF-36 total score as a single measure of health-related quality of life: Scoping review. SAGE Open Med. 2016, 4, 2050312116671725. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- 36-Item Short Form Survey (SF-36) Scoring Instructions. Available online: https://www.rand.org/health-care/surveys_tools/mos/36-item-short-form/scoring.html (accessed on 21 May 2022).
- Ware, J.; Kosinski, M.; Keller, S. SF-12: How to Score the SF-12 Physical and Mental Health Summary Scales; The Health Institute, New England Medical Center: Boston, MA, USA, 1998. [Google Scholar]
- Brazier, J.; Roberts, J.; Deverill, M. The estimation of a preference-based measure of health from the SF-36. J. Health Econ. 2002, 21, 271–292. [Google Scholar] [CrossRef] [Green Version]
- Dritsaki, M.; Petrou, S.; Williams, M.; Lamb, S.E. An empirical evaluation of the SF-12, SF-6D, EQ-5D and Michigan hand outcome questionnaire in patients with rheumatoid arthritis of the hand. Health Qual. Life Outcomes 2017, 15, 20. [Google Scholar] [CrossRef] [Green Version]
- Herdman, M.; Gudex, C.; Lloyd, A.; Janssen, M.; Kind, P.; Parkin, D.; Bonsel, G.; Badia, X. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual. Life Res. 2011, 20, 1727–1736. [Google Scholar] [CrossRef] [Green Version]
- van Hout, B.; Janssen, M.F.; Feng, Y.S.; Kohlmann, T.; Busschbach, J.; Golicki, D.; Lloyd, A.; Scalone, L.; Kind, P.; Pickard, A.S. Interim scoring for the EQ-5D-5L: Mapping the EQ-5D-5L to EQ-5D-3L value sets. Value Health 2012, 15, 708–715. [Google Scholar] [CrossRef] [Green Version]
- EQ-5D-5L Crosswalk Index Value Calculator. Available online: https://euroqol.org (accessed on 26 February 2022).
- Horsman, J.; Furlong, W.; Feeny, D.; Torrance, G. The health utilities index (HUI®): Concepts, measurement properties and applications. Health Qual. Life Outcomes 2003, 1, 54. [Google Scholar] [CrossRef] [Green Version]
- Pelttari, H.; Sintonen, H.; Schalin-Jäntti, C.; Välimäki, M.J. Health-related quality of life in long-term follow-up of patients with cured TNM Stage I or II differentiated thyroid carcinoma. Clin. Endocrinol. 2009, 70, 493–497. [Google Scholar] [CrossRef]
- Sintonen, H. The 15D instrument of health-related quality of life: Properties and applications. Ann. Med. 2001, 33, 328–336. [Google Scholar] [CrossRef]
- Herschbach, P.; Berg, P.; Dankert, A.; Duran, G.; Engst-Hastreiter, U.; Waadt, S.; Keller, M.; Ukat, R.; Henrich, G. Fear of progression in chronic diseases: Psychometric properties of the fear of progression questionnaire. J. Psychosom. Res. 2005, 58, 505–511. [Google Scholar] [CrossRef]
- Mahendran, R.; Liu, J.; Kuparasundram, S.; Griva, K. Validation of the english and simplified mandarin versions of the fear of progression questionnaire–short form in chinese cancer survivors. BMC Psychol. 2020, 8, 10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gotay, C.C.; Pagano, I.S. Assessment of survivor concerns (ASC): A newly proposed brief questionnaire. Health Qual. Life Outcomes 2007, 5, 15. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Giesinger, J.M.; Kuijpers, W.; Young, T.; Tomaszewski, K.A.; Friend, E.; Zabernigg, A.; Holzner, B.; Aaronson, N.K. Thresholds for clinical importance for four key domains of the EORTC QLQ-C30: Physical functioning, emotional functioning, fatigue and pain. Health Qual. Life Outcomes 2016, 14, 87. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Singer, S.; Jordan, S.; Locati, L.D.; Pinto, M.; Tomaszewska, I.M.; Araújo, C.; Hammerlid, E.; Vidhubala, E.; Husson, O.; Kiyota, N.; et al. The EORTC module for quality of life in patients with thyroid cancer: Phase III. Endocr. Relat. Cancer 2017, 24, 197–207. [Google Scholar] [CrossRef] [Green Version]
- Husson, O.; Haak, H.R.; Mols, F.; Nieuwenhuijzen, G.A.; Nieuwlaat, W.A.; Reemst, P.H.; Huysmans, D.A.; Toorians, A.W.; van de Poll-Franse, L.V. Development of a disease-specific health-related quality of life questionnaire (THYCA-QoL) for thyroid cancer survivors. Acta Oncol. 2013, 52, 447–454. [Google Scholar] [CrossRef]
- Dow, K.H.; Ferrell, B.R.; Anello, C. Quality-of-life changes in patients with thyroid cancer after withdrawal of thyroid hormone therapy. Thyroid 1997, 7, 613–619. [Google Scholar] [CrossRef]
- Ryu, C.H.; Park, B.; Ryu, J.; Ryu, Y.M.; Jo, S.A.; Lee, Y.J.; Lee, E.-K.; Hwangbo, Y.; Joo, J.; Jung, Y.-S. Development and evaluation of a korean version of a thyroid-specific quality-of-life questionnaire scale in thyroid cancer patients. Cancer Res. Treat. 2018, 50, 405–415. [Google Scholar] [CrossRef] [Green Version]
- Watt, T.; Hegedüs, L.; Groenvold, M.; Bjorner, J.B.; Rasmussen, Å.K.; Bonnema, S.J.; Feldt-Rasmussen, U. Validity and reliability of the novel thyroid-specific quality of life questionnaire, ThyPRO. Eur. J. Endocrinol. 2010, 162, 161–167. [Google Scholar] [CrossRef] [Green Version]
- Billewicz, W.Z.; Chapman, R.S.; Crooks, J.; Day, M.E.; Gossage, J.; Wayne, E.; Young, J.A. Statistical methods applied to the diagnosis of hypothyroidism. Q. J. Med. 1969, 38, 255–266. [Google Scholar]
- Smets, E.; Garssen, B.; Bonke, B. Manual; Multidimensional Fatigue Inventory; Medical Psychology, Academic Medical Centre: Amsterdam, The Netherland, 1995. [Google Scholar]
- Buysse, D.J.; Reynolds, C.F., III; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef]
- Stern, A.F. The hospital anxiety and depression scale. Occup. Med. 2014, 64, 393–394. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Oei, T.P.; Evans, L.; Crook, G.M. Utility and validity of the STAI with anxiety disorder patients. Br. J. Clin. Psychol. 1990, 29, 429–432. [Google Scholar] [CrossRef] [PubMed]
- Jacobson, B.H.; Johnson, A.; Grywalski, C.; Silbergleit, A.; Jacobson, G.; Benninger, M.S.; Newman, C.W. The voice handicap index (VHI). Am. J. Speech-Lang. Pathol. 1997, 6, 66–70. [Google Scholar] [CrossRef]
- Teliti, M.; Monti, E.; Comina, M.; Conte, L.; Vera, L.; Gay, S.; Saccomani, G.; Ferone, D.; Giusti, M. A comparative cross-sectional study on sleep quality in patients with a history of differentiated thyroid carcinoma and its correlation with quality of life. Endocrine 2021, 73, 347–357. [Google Scholar] [CrossRef] [PubMed]
- Bongers, P.J.; Greenberg, C.A.; Hsiao, R.; Vermeer, M.; Vriens, M.R.; Lutke Holzik, M.F.; Goldstein, D.P.; Devon, K.; Rotstein, L.E.; Sawka, A.M.; et al. Differences in long-term quality of life between hemithyroidectomy and total thyroidectomy in patients treated for low-risk differentiated thyroid carcinoma. Surgery 2020, 167, 94–101. [Google Scholar] [CrossRef]
- Crevenna, R.; Zettinig, G.; Keilani, M.; Posch, M.; Schmidinger, M.; Pirich, C.; Nuhr, M.; Wolzt, M.; Quittan, M.; Fialka-Moser, V.; et al. Quality of life in patients with non-metastatic differentiated thyroid cancer under thyroxine supplementation therapy. Support. Care Cancer 2003, 11, 597–603. [Google Scholar] [CrossRef]
- Jeon, M.J.; Lee, Y.M.; Sung, T.Y.; Han, M.; Shin, Y.W.; Kim, W.G.; Kim, T.Y.; Chung, K.W.; Shong, Y.K.; Kim, W.B. Quality of life in patients with papillary thyroid microcarcinoma managed by active surveillance or lobectomy: A cross-sectional study. Thyroid 2019, 29, 956–962. [Google Scholar] [CrossRef]
- Karapanou, O.; Papadopoulos, A.; Vlassopoulou, B.; Vassilopoulos, C.; Pappa, E.; Tsagarakis, S.; Niakas, D. Health status of Greek thyroid cancer patients after radioiodine administration compared to a demographically matched general population sample. Hell. J. Nucl. Med. 2012, 15, 98–102. [Google Scholar] [CrossRef]
- Lan, Y.; Luo, Y.; Zhang, M.; Jin, Z.; Xiao, J.; Yan, L.; Zhu, Y. Quality of life in papillary thyroid microcarcinoma patients undergoing radiofrequency ablation or surgery: A comparative study. Front. Endocrinol. 2020, 11, 249. [Google Scholar] [CrossRef]
- Lan, Y.; Cao, L.; Song, Q.; Jin, Z.; Xiao, J.; Yan, L.; Luo, Y.; Zhang, M. The quality of life in papillary thyroid microcarcinoma patients undergoing lobectomy or total thyroidectomy: A cross-sectional study. Cancer Med. 2021, 10, 1989–2002. [Google Scholar] [CrossRef]
- Li, J.; Zhang, B.; Bai, Y.; Liu, Y.; Zhang, B.; Jin, J. Health-related quality of life analysis in differentiated thyroid carcinoma patients after thyroidectomy. Sci. Rep. 2020, 10, 5765. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mlees, M.A.; Elbarbary, A.H. Hemithyroidectomy vs. total thyroidectomy for minimally invasive follicular thyroid carcinoma: Quality of life and oncological outcomes. Surg. Pract. 2022, 26, 34–41. [Google Scholar] [CrossRef]
- Nakamura, T.; Miyauchi, A.; Ito, Y.; Ito, M.; Kudo, T.; Tanaka, M.; Kohsaka, K.; Kasahara, T.; Nishihara, E.; Fukata, S.; et al. Quality of life in patients with low-risk papillary thyroid microcarcinoma: Active surveillance versus immediate surgery. Endocr. Pract. 2020, 26, 1451–1457. [Google Scholar] [CrossRef]
- Nies, M.; Klein Hesselink, M.S.; Huizinga, G.A.; Sulkers, E.; Brouwers, A.H.; Burgerhof, J.G.M.; van Dam, E.W.C.M.; Havekes, B.; van den Heuvel-Eibrink, M.M.; Corssmit, E.P.M.; et al. Long-term quality of life in adult survivors of pediatric differentiated thyroid carcinoma. J. Clin. Endocrinol. Metab. 2017, 102, 1218–1226. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- van Gerwen, M.; Cooke, P.V.; Alpert, N.; Mols, F.; Genden, E.; Schwartz, R.M. Patient-reported outcomes following total thyroidectomy and lobectomy in thyroid cancer survivors: An analysis of the PROFILES Registry data. Support. Care Cancer 2022, 30, 687–693. [Google Scholar] [CrossRef]
- Yang, S.; Xu, X. Anxiety and quality of life among papillary thyroid cancer patients awaiting final pathology results after surgery. Endocrine 2022, 76, 377–384. [Google Scholar] [CrossRef]
- Zhang, M.; Tufano, R.P.; Russell, J.O.; Zhang, Y.; Zhang, Y.; Qiao, Z.; Luo, Y. Ultrasound-guided radiofrequency ablation Versus surgery for low-risk papillary thyroid microcarcinoma: Results of over 5 years’ follow-up. Thyroid 2020, 30, 408–417. [Google Scholar] [CrossRef]
- Chen, W.; Li, J.; Peng, S.; Hong, S.; Xu, H.; Lin, B.; Liang, X.; Liu, Y.; Liang, J.; Zhang, Z.; et al. Association of total thyroidectomy or thyroid lobectomy with the quality of life in patients with differentiated thyroid cancer with low to intermediate risk of recurrence. JAMA Surg. 2022, 157, 200–209. [Google Scholar] [CrossRef]
- Lubitz, C.C.; De Gregorio, L.; Fingeret, A.L.; Economopoulos, K.P.; Termezawi, D.; Hassan, M.; Parangi, S.; Stephen, A.E.; Halpern, E.F.; Donelan, K.; et al. Measurement and variation in estimation of quality of life effects of patients undergoing treatment for papillary thyroid carcinoma. Thyroid 2017, 27, 197–206. [Google Scholar] [CrossRef] [Green Version]
- Moon, J.H.; Ryu, C.H.; Cho, S.W.; Choi, J.Y.; Chung, E.J.; Hah, J.H.; Hwangbo, Y.; Jeong, W.J.; Jung, Y.S.; Kim, J.H.; et al. Effect of initial treatment choice on 2-year quality of life in patients with low-risk papillary thyroid microcarcinoma. J. Clin. Endocrinol. Metab. 2021, 106, 724–735. [Google Scholar] [CrossRef]
- van Velsen, E.F.S.; Massolt, E.T.; Heersema, H.; Kam, B.L.R.; van Ginhoven, T.M.; Visser, W.E.; Peeters, R.P. Longitudinal analysis of quality of life in patients treated for differentiated thyroid cancer. Eur. J. Endocrinol. 2019, 181, 671–679. [Google Scholar] [CrossRef] [PubMed]
- Hedman, C.; Strang, P.; Djärv, T.; Widberg, I.; Lundgren, C.I. Anxiety and fear of recurrence despite a good prognosis: An interview study with differentiated thyroid cancer patients. Thyroid 2017, 27, 1417–1423. [Google Scholar] [CrossRef] [Green Version]
- Kletzien, H.; Macdonald, C.L.; Orne, J.; Francis, D.O.; Leverson, G.; Wendt, E.; Sippel, R.S.; Connor, N.P. Comparison between patient-perceived voice changes and quantitative voice measures in the first postoperative year after thyroidectomy: A secondary analysis of a randomized clinical trial. JAMA Otolaryngol. Head Neck Surg. 2018, 144, 995–1003. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nickel, B.; Tan, T.; Cvejic, E.; Baade, P.; McLeod, D.S.A.; Pandeya, N.; Youl, P.; McCaffery, K.; Jordan, S. Health-related quality of life after diagnosis and treatment of differentiated thyroid cancer and association with type of surgical treatment. JAMA Otolaryngol. Head Neck Surg. 2019, 145, 231–238. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Diamond-Rossi, S.A.; Jonklaas, J.; Jensen, R.E.; Kuo, C.; Stearns, S.; Esposito, G.; Davidson, B.J.; Luta, G.; Bloom, G.; Graves, K.D. Looking under the hood of “the cadillac of cancers”: Radioactive iodine-related craniofacial side effects among patients with thyroid cancer. J. Cancer Surviv. 2020, 14, 847–857. [Google Scholar] [CrossRef] [PubMed]
- Doubleday, A.R.; Robbins, S.E.; Macdonald, C.L.; Elfenbein, D.M.; Connor, N.P.; Sippel, R.S. What is the experience of our patients with transient hypoparathyroidism after total thyroidectomy? Surgery 2021, 169, 70–76. [Google Scholar] [CrossRef]
- Tonon, G. Relevance of the use of qualitative methods in the study of quality of life. In Qualitative Studies in Quality of Life: Methodology and Practice; Tonon, G., Ed.; Springer International Publishing: Cham, Switzerland, 2015; pp. 3–21. [Google Scholar]
- Haymart, M.R.; Esfandiari, N.H.; Stang, M.T.; Sosa, J.A. Controversies in the management of low-risk differentiated thyroid cancer. Endocr. Rev. 2017, 38, 351–378. [Google Scholar] [CrossRef]
- Hwangbo, Y.; Kim, J.M.; Park, Y.J.; Lee, E.K.; Lee, Y.J.; Park, D.J.; Choi, Y.S.; Lee, K.D.; Sohn, S.Y.; Kim, S.W.; et al. Long-term recurrence of small papillary thyroid cancer and its risk factors in a korean multicenter study. J. Clin. Endocrinol. Metab. 2017, 102, 625–633. [Google Scholar] [CrossRef] [Green Version]
- Rajjoub, S.R.; Yan, H.; Calcatera, N.A.; Kuchta, K.; Wang, C.E.; Lutfi, W.; Moo-Young, T.A.; Winchester, D.J.; Prinz, R.A. Thyroid lobectomy is not sufficient for T2 papillary thyroid cancers. Surgery 2018, 163, 1134–1143. [Google Scholar] [CrossRef]
- Christou, N.; Mathonnet, M. Complications after total thyroidectomy. J. Visc. Surg. 2013, 150, 249–256. [Google Scholar] [CrossRef]
- Sun, H.; Yang, Y.; Zhang, J.; Liu, T.; Wang, H.; Garg, S.; Zhang, B. Fear of cancer recurrence, anxiety and depressive symptoms in adolescent and young adult cancer patients. Neuropsychiatr. Dis. Treat. 2019, 15, 857–865. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Johansson, B.; Brandberg, Y.; Hellbom, M.; Persson, C.; Petersson, L.M.; Berglund, G.; Glimelius, B. Health-related quality of life and distress in cancer patients: Results from a large randomised study. Br. J. Cancer 2008, 99, 1975–1983. [Google Scholar] [CrossRef] [PubMed]
- Tagay, S.; Herpertz, S.; Langkafel, M.; Erim, Y.; Bockisch, A.; Senf, W.; Görges, R. Health-related Quality of Life, depression and anxiety in thyroid cancer patients. Qual. Life Res. 2006, 15, 695–703. [Google Scholar] [CrossRef]
- Dionisi-Vici, M.; Fantoni, M.; Botto, R.; Nervo, A.; Felicetti, F.; Rossetto, R.; Gallo, M.; Arvat, E.; Torta, R.; Leombruni, P. Distress, anxiety, depression and unmet needs in thyroid cancer survivors: A longitudinal study. Endocrine 2021, 74, 603–610. [Google Scholar] [CrossRef] [PubMed]
- Lasry, J.C.; Margolese, R.G. Fear of recurrence, breast-conserving surgery, and the trade-off hypothesis. Cancer 1992, 69, 2111–2115. [Google Scholar] [CrossRef]
- Sprangers, M.A. Quality-of-life assessment in oncology. Achievements and challenges. Acta Oncol. 2002, 41, 229–237. [Google Scholar] [CrossRef]
- Easley, J.; Miedema, B.; Robinson, L. It’s the “good” cancer, so who cares? Perceived lack of support among young thyroid cancer survivors. Oncol. Nurs. Forum 2013, 40, 596–600. [Google Scholar] [CrossRef] [Green Version]
- Randle, R.W.; Bushman, N.M.; Orne, J.; Balentine, C.J.; Wendt, E.; Saucke, M.; Pitt, S.C.; Macdonald, C.L.; Connor, N.P.; Sippel, R.S. Papillary thyroid cancer: The good and bad of the “good cancer”. Thyroid 2017, 27, 902–907. [Google Scholar] [CrossRef]
- Büel-Drabe, N.; Steinert, H.; Moergeli, H.; Weidt, S.; Seiler, A.; Jenewein, J. Thyroid cancer has a small impact on patient–partner relationships and their frequency of sexual activity. Palliat. Support. Care 2018, 16, 335–346. [Google Scholar] [CrossRef]
- Javaloyes, N.; Crespo, A.; Redal, M.C.; Brugarolas, A.; Botella, L.; Escudero-Ortiz, V.; Sureda, M. Psycho-oncological intervention through counseling in patients with differentiated thyroid cancer in treatment with radioiodine (counthy, NCT05054634): A non-randomized controlled study. Front. Psychol. 2022, 13, 269. [Google Scholar] [CrossRef]
- Wu, H.-X.; Zhong, H.; Xu, Y.-D.; Xu, C.-P.; Zhang, Y.; Zhang, W. Psychological and behavioral intervention improves the quality of life and mental health of patients suffering from differentiated thyroid cancer treated with postoperative radioactive iodine-131. Neuropsychiatr. Dis. Treat. 2016, 12, 1055–1060. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Henry, M.; Frenkiel, S.; Chartier, G.; MacDonald, C.; Payne, R.J.; Black, M.J.; Mlynarek, A.M.; Zeitouni, A.; Kost, K.; Loiselle, C.; et al. Thyroid cancer patients receiving an interdisciplinary team-based care approach (ITCA-ThyCa) appear to display better outcomes: Program evaluation results indicating a need for further integrated care and support. Psychooncology 2018, 27, 937–945. [Google Scholar] [CrossRef] [PubMed]
- Cancer Journey Portfolio. Screening for Distress, the 6th Vital Sign: A Guide to Implementing Best Practices in Person-Centred Care. 2012. Available online: www.cancerview.ca (accessed on 26 February 2022).
- Shah, M.D.; Witterick, I.J.; Eski, S.J.; Pinto, R.; Freeman, J.L. Quality of life in patients undergoing thyroid surgery. J. Otolaryngol. 2006, 35, 209. [Google Scholar] [CrossRef] [PubMed]
- Lee, L.; Mitmaker, E.J.; Chabot, J.A.; Lee, J.A.; Kuo, J.H. Cost-effectiveness of diagnostic lobectomy versus observation for thyroid nodules >4 cm. Thyroid 2016, 26, 271–279. [Google Scholar] [CrossRef]
- Vargas-Salas, S.; Martínez, J.R.; Urra, S.; Domínguez, J.M.; Mena, N.; Uslar, T.; Lagos, M.; Henríquez, M.; González, H.E. Genetic testing for indeterminate thyroid cytology: Review and meta-analysis. Endocr. Relat. Cancer 2018, 25, R163–R177. [Google Scholar] [CrossRef] [Green Version]
- Dingle, I.F.; Mishoe, A.E.; Nguyen, S.A.; Overton, L.J.; Gillespie, M.B. Salivary morbidity and quality of life following radioactive iodine for well-differentiated thyroid cancer. Otolaryngol. Head Neck Surg. 2013, 148, 746–752. [Google Scholar] [CrossRef]
| Characteristics | Number of Studies |
|---|---|
| Methodology | |
| Quantitative | 20 |
| Qualitative | 2 |
| Mixed methods | 3 |
| Cross-sectional | 19 |
| Transversal | 6 |
| Surgery extent | |
| TT | 14 |
| HT | 1 |
| Both | 10 |
| Comparisons for physical-related HrQoL | |
| HT vs. TT | 9 |
| Postoperative vs. Preoperative | 3 |
| Postoperative vs. Healthy controls | 8 |
| Postoperative vs. AS | 3 |
| Comparisons for psychological-related HrQoL | |
| HT vs. TT | 10 |
| Postoperative vs. Preoperative | 2 |
| Postoperative vs. Healthy controls | 8 |
| Postoperative vs. AS | 3 |
| Comparisons for social-related HrQoL | |
| HT vs. TT | 7 |
| Postoperative vs. Preoperative | 1 |
| Postoperative vs. Healthy controls | 8 |
| Postoperative vs. AS | 2 |
| QoL instruments and scores (minimum-maximum) | |
| 15D instrument (0–1) | 1 |
| ASC (1–4) | 1 |
| Billewicz Score (−47–67) | 1 |
| EORTC QLC-C30 (0–100) | 3 |
| EORTC QLQ-THY34 (0–100) | 1 |
| EQ5D-5L (−0.11–1.0) | 1 |
| FoP (0–4) | 1 |
| FoP-Q-SF (1–5) | 2 |
| HADS (0–21) | 4 |
| HUI2 (−0.03 to 1.0) | 1 |
| HUI3 (−0.36–1.0) | 1 |
| KT-QoL (0–10) | 1 |
| MFI-20 (20–100) | 3 |
| PSQI. (0–21) | 1 |
| SDQ (0–51 (f.), 0–55 (m.)) | 1 |
| SF-6D (0.3–1.0) | 1 |
| SF-12 (0–100) | 2 |
| SF-36 (0–100) | 9 |
| STAI (20–80) | 1 |
| ThyPRO (0–100) | 2 |
| THYCA-QoL | 6 |
| VHI (0–120) | 1 |
| Visual analog scale (0–10) | 1 |
| Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | |
|---|---|---|---|---|---|---|---|---|
| Bongers et al. (2019) [52] | Y | Y | Y | Y | Y | Y | N | Y |
| Crevanna et al. (2003) [53] | N | N | U | Y | N | N/a | N | Y |
| Hoftijzer et al. (2007) [18] | Y | N | Y | Y | N | N/a | N | Y |
| Jeon et al. (2019) [54] | Y | Y | Y | Y | Y | Y | N | Y |
| Karapanou et al. (2012) [55] | Y | Y | Y | Y | Y | N | N | Y |
| Lan et al. (2020) [56] | Y | Y | Y | Y | Y | Y | N | Y |
| Lan et al. (2021) [57] | Y | Y | Y | Y | Y | Y | N | Y |
| Li et al. (2020) [58] | Y | Y | Y | Y | Y | Y | N | Y |
| Mlees et al. (2022) [59] | Y | Y | Y | Y | Y | Y | N | Y |
| Nakamura et al. (2020) [60] | Y | Y | Y | Y | N | N/a | N | Y |
| Nies et al. (2017) [61] | Y | N | Y | Y | Y | N/a | N | Y |
| Pelttari et al. (2009) [34] | Y | N | Y | Y | Y | Y | N | Y |
| Teliti et al. (2021) [51] | Y | Y | Y | Y | Y | Y | N | Y |
| Van Gerwen et al.(2022) [62] | Y | Y | Y | Y | Y | N | N | Y |
| Yang et al.(2022) [63] | Y | Y | Y | Y | Y | Y | N | Y |
| Zhang et al. (2020) [64] | Y | N | Y | Y | N | N/a | N | Y |
| Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Q10 | Q11 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Chen et al. (2021) [65] | Y | Y | Y | Y | Y | N/a | N | Y | Y | Y | Y |
| Lubitz et al. (2017) [66] | Y | Y | Y | N | N | N/a | Y | Y | N | Y | Y |
| Moon et al. (2021) [67] | Y | Y | Y | N | N | N/a | N | Y | N | Y | Y |
| Van Velsen et al. (2019) [68] | Y | Y | Y | Y | Y | N/a | N | Y | N | Y | Y |
| Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Q10 | |
|---|---|---|---|---|---|---|---|---|---|---|
| Hedman et al. (2017) [69] | U | Y | Y | Y | Y | N | N | U | Y | Y |
| Kletzien et al. (2018) [70] | U | Y | Y | U | U | N | N | U | Y | Y |
| Nickel et al. (2019) [71] | U | Y | Y | Y | Y | N | N | U | Y | Y |
| Diamond Rossi et al. (2020) [72] | U | Y | Y | Y | Y | N | N | U | Y | Y |
| Doubleday et al. (2020) [73] | U | Y | Y | N | N | N | N | U | Y | Y |
| Study and Country | Sample Size | Surgery Extent | Pathology Details | RAI (%) | Morbidity Rates (%) | Postop a Time of QoL Assessment | QoL Instrument | QoL Items | Changes in QoL Scores | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| TT vs. HT | Postop vs. Preop b | Postop vs. Healthy Controls | Postop vs. AS | |||||||||||||||
| Physical health component | ||||||||||||||||||
| Crevanna et al. (2003) [53] Austria | 150 51 (subgroup) | TT | DTC | 100 | RLNi f: 3.3 HypoPTH g: 16.6 | 0–23 y. (mean 5.5 y.) | SF-36 | Bodily pain Physical functioning Vitality | - | - | <1 y. +4.1 −1.7 −10.3 | 0–23 y. +5.4 −1.2 −4.7 | - | |||||
| Hoftijzer et al. (2007) [18] The Netherlands | 153 | TT | DTC | 100 | N/a | 0.3–41.8 y. | SF-36 MFI-20 | Bodily pain Physical functioning General fatigue Physical fatigue | - | - | −2.43 −4.07 +2.43 +2.35 | - | ||||||
| Karapanou et al. (2012) [55] Greece | 60 | TT | PTC c | 100 | N/a | 2–6 m. | SF-36 | Bodily pain Physical functioning Vitality | - | - | −0.09 −6.88 −6.20 | - | ||||||
| Li et al. (2020) [58] China | 174 | TT | DTC | 100 | N/a | 1 y. | SF-36 | Bodily pain Physical functioning Vitality | - | - | −7.4 −0.3 −8.7 | - | ||||||
| Nies et al. (2017) [61] The Netherlands | 67 | TT | DTC | 97 | Permanent hypoPTH: 25.4 RLNi: 14.9 | 5–44.7 y. (mean 17.8 y.) | SF-36 MFI-20 | Bodily pain Physical functioning General fatigue Physical fatigue | - | - | −16 −5 +1 +2 | - | ||||||
| Pelttari et al. (2009) [34] Finland | 341 | TT (98.8%) | 94% PTC 6% FTC d | 84.5 | RLNi: 1.4 Permanent hypoPTH: 1.7 | 5–19.5 y. (mean 12.4 y.) | 15D instrument | Mobility Vision Hearing Breathing Sleeping Eating Speech Elimination Discomfort and symptoms Vitality Sexual activity | - | - | +0.010 +0.005 −0.013 −0.002 −0.036 −0.003 −0.017 +0.005 +0.044 −0.011 −0.019 | - | ||||||
| Teliti et al. (2021) [51] Italy | 119 | TT (95.6%) | DTC | 71 | N/a | Mean 9.9 y. | PSQI ThyPRO Billewicz score VAS | Global PSQI Sleep quality Sleep latency Sleep duration Sleep efficiency Sleep disturbance Use of sleep medication Daytime dysfunction Goiter symptoms Hyperthyroid symptoms Hypothyroid symptoms Eye symptoms Tiredness Cognitive problems Cosmetic complaints Hypothyroid symptoms Complaints due to medical therapies | - | - | +0.985 +0.093 −0.049 +0.1799 +0.394 +0.083 +0.013 +0.283 +2.00 +0.78 +0.517 +1.134 −0.52 +7.04 +1.227 = +0.6 | - | ||||||
| Van Velsen et al. (2019) [68] The Netherlands | 185 | TT | 88% PTC 12% FTC | 100 | RLNi: 9.2 Transient hypoPTH: 20.0 Permanent hypoPTH: 16.8 | 2–4 y. | MFI-20 SF-36 ThyPRO | General fatigue Physical fatigue Physical functioning Vitality Tiredness Cognitive problems | - | 2 y. +0.7 +0.2 −2.4 −2.7 +1.0 +4.9 | 4 y. +0.6 = −0.8 −2.3 +1.4 +5.0 | 2 y.☨ +5.1 +4.8 -8.0 -13.5 +6.6 +0.3 | 4 y.☨ +5.0 +4.6 -6.4 -13.1 +7.0 +0.4 | - | ||||
| Doubleday et al. (2020) [73] USA | 62 | TT | DTC | N/a | Transient hypoPTH: 4.8 | 2 w. 6 w. 6 m. 1 y. | SF-12 | Physical component | - | −8.07 −1.40 +0.65 +1.49 | - | - | ||||||
| Kletzien et al. (2018) [70] USA | 42 | TT | PTC | N/a | RLNi: 19.0 | 2 w. 6 w. 6 m. 1 y. | VHI | Voice impairment (total) | - | +9.70 +8.70 +1.32 −1.42 | - | - | ||||||
| Chen et al. (2021) [65] China | 427 365 | HT TT | DTC | 2.3 18.1 | Transient hypoPTH: 6.6 RLNi: 0.4 Transient hoarseness: 21.1 Transient hypoPTH: 32.2 RLNi: 1.6 Transient hoarseness: 30.8 | 1 m.–1 y. | EORTC QLC-C30 THYCA-QoL | Physical functioning Cognitive functioning Fatigue Nausea/vomiting Pain Dyspnoea Sleep disturbances Appetite loss Constipation Diarrhea Neuromuscular Voice Concentration Sympathetic Throat/mouth Sensory Problems with scar Feeling chilly Tingling hands/feet Weight gain Headache Decreased libido | 1 m −2.1 0.6 3.2 −0.03 2.7 −0.3 0.5 −0.03 −0.25 −0.5 2.7 8.2 0.5 1.9 2.3 −1.7 3.0 2.9 2.4 1.2 −1.6 −3.9 | 3 m −2.7 −0.3 2.97 0.2 0.5 −0.4 −0.3 1.57 −0.1 −0.4 3.6 3.8 0.1 2.4 2.1 −0.5 2.2 0.6 3.1 2.95 −0.5 −0.9 | 6 m −0.1 1.98 −0.7 0.02 0.8 −1.1 −0.5 0.15 −0.4 0.05 1.1 0.1 −1.4 0.9 −0.45 −1.1 1.5 0.4 1.1 0.05 −1.8 −2.3 | 1 y. 0.2 1.8 −1.7 −0.2 0.05 1.0 −3.2 −1.1 −0.6 0.2 0.1 −0.9 −1.6 1.7 −0.2 −0.45 0.9 −0.9 −0.4 −2.5 −0.6 1.0 | - | - | - | |||
| Bongers et al. (2019) [52] Canada | 59 211 | HT TT | 47.5% PTC 52.5% FVPTC e 33.6% PTC 65.4% FVPTC 0.9% FTC | 0 43.6 | Permanent hypoPTH: 0.0 Persistent RLNi: 0.0 Permanent hypoPTH: 6.2 Persistent RLNi: 0.0 | 0.9–12.7 y. | EORTC QLC-C30 EORTC QLQ-THY34 | Physical functioning Cognitive functioning Fatigue Nausea/vomiting Pain Dyspnoea Sleep disturbances Appetite loss Constipation Diarrhea Fatigue Neck discomfort Voice concerns Hair problems Swallowing Dry mouth Temperature intolerance Restlessness Shoulder function Joint pain Tingling/numbness Cramps | +0.1 +6.5 −4.2 +1.2 +2.0 +0.3 −8.4 −0.5 −0.6 +0.3 −5.0 −2.8 +0.4 +2.5 +1.5 +0.6 −6.2 −1.1 −1.7 +4.2 +0.2 +3.8 | - | - | - | ||||||
| Lan et al. (2021) [57] China | 34 35 | HT TT | PTMC | 0 | RLNi: 0.0 RLNi: 8.6 | 0-45 m. | SF-36 THYCA-QoL FoP-Q-SF | Bodily pain Physical functioning Vitality Neuromuscular Voice Concentration Sympathetic Throat/mouth Sensory Problems with scar Feeling chilly Tingling hands/feet Weight gain Headache Decreased libido Physical health | −9 = −5 +11 = = +16 = −8 +33 = = +16 −17 −33 = | - | - | - | ||||||
| Lan et al. (2020) [56] China | 18 16 | HT TT | PTMC | N/a | RLNi: 5.9 | Mean 20.29 m. | SF-36 THYCA-QoL FoP-Q-SF | Bodily pain Physical functioning Vitality Neuromuscular Voice Concentration Sympathetic Throat/mouth Sensory Problems with scar Feeling chilly Tingling hands/feet Weight gain Headache Decreased libido Physical health | −3.34 −2.39 −11.8 +4.09 −7.18 +5.79 +7.87 −2.78 +4.16 +9.49 −0.93 +4.63 +6.25 +3.47 −4.4 +0.28 | - | - | - | ||||||
| Mlees et al. (2022) [59] Egypt | 42 40 | HT TT | Minimally invasive FTC | N/a | Transient hypoPTH: 2.4 Transient hypoPTH: 12.5 Permanent hypoPTH: 2.5 Temporary RLNi: 7.5 Persistent RLNi: 2.5 Seroma: 7.5 Infection: 5.0 | 12 m. | SF-36 | Bodily pain Physical functioning Vitality | −2.8 −1.8 −5.3 | - | - | - | ||||||
| Van Gerwen et al. (2021) [62] USA | 34 24 | HT TT | 84.4% PTC 15.5% FTC | 0 | N/a | 2–20 y. | EORTC QLC-C30 | Physical functioning Cognitive functioning Fatigue Nausea/vomiting Pain Dyspnoea Insomnia Appetite loss Constipation Diarrhea | −6.8 3.6 3.6 1.1 7.6 9.1 9.6 −0.8 5.5 −2.9 | - | - | - | ||||||
| Zhang et al. (2020) [64] China | 19 8 | HT TT | PTMC | N/a | Persistent RLNi: 2.5 Permanent hypoPTH: 0.0 Persistent RLNi: 7.1 Permanent hypoPTH: 7.1 | Median: 63.6 m. | THYCA-QoL | Neuromuscular Voice Concentration Sympathetic Throat/mouth Sensory Problems with scar Feeling chilly Tingling hands/feet Weight gain Headache Decreased libido | = +0.72 = −0.13 −0.14 +0.05 −0.32 −0.21 −0.11 −0.16 +0.14 = | - | - | - | ||||||
| Moon et al. (2020) [67] South Korea | 238 79 500 | HT TT AS | PTMC | N/a | N/a | 6 m. 1 y 1.5 y. ≥2. Y. | KT-QoL | Physical subscale | −0.6 −0.4 −0.5 0.004 | HT −0.7 −0.5 −1.1 −0.5 | TT −1.3 −0.9 −1.5 −0.5 | |||||||
| Nakamura et al. (2020) [60] Japan | 17 32 298 | HT TT AS | PTMC | N/a | Temporary RLNi: 6 Persistent RLNi: 0 Transient hypoPTH: 33 Permanent hypoPTH: 4 - | 64–130 m. (mean: 84 m.) | THYCA-QoL | Neuromuscular Voice Concentration Sympathetic Throat/mouth Sensory Problems with scar Feeling chilly Tingling hands/feet Weight gain Headache Decreased libido | −11 −17 −33 +17 = = = = = +33 +33 = | - | - | HT +11 +17 +33 = = = = = = = = = | TT = = = +17 = = = = = +33 +33 = | |||||
| Jeon et al. (2019) [54] South Korea | 148 43 | HT AS | PTMC | 0 | Transient hypoPTH: 1.4 - | 14.2–53.0 m. | SF-12 THYCA-QoL | Bodily pain Physical functioning Vitality Neuromuscular Voice Concentration Sympathetic Throat/mouth Sensory Problems with scar Feeling chilly Tingling hands/feet Weight gain Headache Decreased libido | - | - | - | −12.04 −2.05 −0.94 +5.72 +2.95 +5.03 +4.99 +5.98 +1.18 +9.12 +4.87 +4.17 +5.08 +2.90 −9.27 | ||||||
| Psychological health component | ||||||||||||||||||
| Crevanna et al. (2003) [53] Austria | 150 51 (sub-group) | TT | DTC | 100 | RLNi: 3.3 HypoPTH: 16.6 | 0–23 y. (mean: 5.5 y.) | SF-36 | Mental health | - | - | <1 y. −8.14 | 0–23 y. −2.46 | - | |||||
| Hoftijzer et al. (2007) [18] Netherlands | 153 | TT | DTC | 100 | N/a | 0.3–41.8 y. | MFI-20 HADS SDQ | Reduced motivation Mental fatigue Anxiety Depression Anxiety + depression Somatization | - | - | +1.38 +1.61 +1.48 +0.75 +2.23 +4.27 | |||||||
| Karapanou et al. (2012) [55] Greece | 60 | TT | PTC | 100 | N/a | 2–6 m. | SF-36 | Mental health | - | - | +2.46 | - | ||||||
| Li et al. (2020) [58] China | 174 | TT | DTC | 100 | N/a | 1 y. | SF-36 | Mental Health | - | - | −10.2 | - | ||||||
| Nies et al. (2017) [61] Netherlands | 67 | TT | DTC | 97 | Permanent hypoPTH: 25.4 RLNi: 14.9 | 5–44.7 y. (mean 17.8 y.) | SF-36 MFI-20 HADS | Mental Health Reduced motivation Mental fatigue Anxiety Depression | - | - | = = +2 +1 = | - | ||||||
| Pelttari et al. (2009) [34] Finland | 341 | TT (98.8%) | 94.5% PTC 5.5% FTC | 84.5 | RLNi: 1.4 Permanent hypoPTH: 1.7 | 5–19.5 y. (mean 12.4 y.) | 15D instrument | Mental function Depression Distress | - | - | +0.003 −0.014 −0.023 | - | ||||||
| Teliti et al. (2021) [51] Italy | 119 | TT (95.6%) | DTC | 71 | N/a | Mean 9.9 y. | ThyPRO g | Anxiety Depressivity Emotional susceptibility | - | - | +0.407 +0.554 +0.38 | - | ||||||
| Van Velsen et al. (2019) [68] Netherlands | 185 | TT | 88% PTC 12% FTC | 100 | RLNi: 9.2 Transient hypoPTH: 20.0 Permanent hypoPTH: 16.8 | 2-4 y. | MFI-20 SF-36 ThyPRO | Mental fatigue Mental health Anxiety Depressivity | - | 2 y. +0.7 +1.5 −13.1 −5.8 | 4 y. +0.4 +2.6 −13.8 −5.9 | 2 y.☨ +4.7 −8.6 +0.6 −2.9 | 4 y.☨ +4.4 −7.5 −0.1 −3.0 | - | ||||
| Doubleday et al. (2020) [73] USA | 62 | TT | DTC | N/a | Transient hypoPTH: 4.8 | 2 w. 6 w. 6 m. 1 y. | SF-12 | Mental health component | - | +5.04 +3.58 +3.61 +4.84 | - | - | ||||||
| Chen et al. (2021) [65] China | 427 365 | HT TT | DTC | 2.3 18.1 | Transient hypoPTH: 6.6 RLNi: 0.4 Transient hoarseness: 21.1 Transient hypoPTH: 32.2 RLNi: 1.6 Transient hoarseness: 30.8 | 1 m.–1 y. | EORTC QLC-C30 THYCA-QoL HADS | Emotional function Psychological symptoms Anxiety Depression | 1 m. −3.2 2.3 0.6 0.4 | 3 m. −0.9 0.5 0.4 0.3 | 6 m. 1.0 −1.1 −0.05 −0.1 | 1 y. −0.6 −0.45 0.1 −0.15 | - | - | - | |||
| Bongers et al. (2019) [52] Canada | 59 211 | HT TT | 47.5% PTC 52.5% FVPTC e 33.6% PTC 65.4% FVPTC 0.9% FTC | 0 43.6 | Permanent hypoPTH: 0.0 Persistent RLNi: 0.0 Permanent hypoPTH: 6.2 Persistent RLNi: 0.0 | 0.9–12.7 y. | EORTC QLC-C30 EORTC QLQ-THY34 ASC | Emotional functioning Body image altered Fear Worry Cancer worry Future test worry New cancer worry Recurrence worry General health worry Death worry Health worry Overall worry | +3.8 −5.5 −5.2 −7.9 −0.7 −0.2 −0.2 −0.3 −0.4 = −0.3 −1.1 | - | - | - | ||||||
| Lan et al. (2021) [57] China | 34 35 | HT TT | PTMC | 0 | RLNi: 0.0 RLNi: 8.6 | 0–45 m. | SF-36 THYCA-QoL | Mental health Psychological | −10 +8 | - | - | - | ||||||
| Lan et al. (2020) [56] China | 18 16 | HT TT | PTMC | N/a | RLNi: 5.9 | Mean 20.29 m. | SF-36 THYCA-QoL | Mental health Psychological | −2.58 +12.8 | - | - | - | ||||||
| Mlees et al. (2022) [59] Egypt | 42 40 | HT TT | Minimally invasive FTC | N/a | Transient hypoPTH: 2.4 Transient hypoPTH: 12.5 Permanent hypoPTH: 2.5 Temporary RLNi: 7.5 Persistent RLNi: 2.5 Seroma: 7.5 Infection: 5.0 | 12 m. | SF-36 | Mental health | −4.1 | - | - | - | ||||||
| Van Gerwen et al. (2021) [62] USA | 34 24 | HT TT | 84.4% PTC 15.5% FTC | 0 | N/a | 2–20 y. | EORTC QLC-C30 | Emotional functioning | −5.4 | - | - | - | ||||||
| Yanf et al. (2022) [63] China | 86 263 | HT TT | PTC | N/a | N/a | <1 w.–1 mo. | STAI | State anxiety | 1.39 | - | - | - | ||||||
| Zhang et al. (2020) [64] China | 19 8 | HT TT | PTMC | N/a | Persistent RLNi: 2.5 Permanent hypoPTH: 0.0 Persistent RLNi: 7.1 Permanent hypoPTH: 7.1 | Median: 63.6 m. | THYCA-QoL | Psychological problems | −0.22 | - | - | - | ||||||
| Moon et al. (2020) [67] South Korea | 238 79 500 | HT TT AS | PTMC | N/a | N/a | 6 m. 1 y 1.5 y. ≥2 y. | KT-QoL | Mental health subscale | −0.4 −0.4 −0.7 0.11 | HT −0.4 −0.3 −0.5 −0.2 | TT −0.8 −0.7 −1.2 −0.1 | |||||||
| Nakamura et al. (2020) [60] Japan | 17 32 298 | HT TT AS | PTMC | N/a | Temporary RLNi: 6 Persistent RLNi: 0 Transient hypoPTH: 33 Permanent hypoPTH: 4 - | 64–130 m. (mean: 84 m.) | THYCA-QoL HADS | Psychological Anxiety Depression Total | = −1 = −1 | - | - | HT +9 +2 +2 +3 | TT +9 +1 +2 +2 | |||||
| Jeon et al. (2019) [54] South Korea | 148 43 | HT AS | PTMC | 0 | Transient hypoPTH: 1.4 - | 14.2 m.–53.0 m. | SF-12 THYCA-QoL FoP | Mental health Psychological Affective reactions Coping with anxiety | - | - | - | −1.01 +2.57 −0.05 −0.11 | ||||||
| Social functioning component | ||||||||||||||||||
| Crevanna et al. (2003) [53] Austria | 150 51 (sub-group) | TT | DTC | 100 | RLNi: 3.3 HypoPTH: 16.6 | 0–23 y. (mean 5.5 y.) | SF-36 | Role limitations due to emotional health Role limitations due to physical health Social functioning and interactions | - | - | <1 y. −30.2 −18.3 −9.19 | 0–23 y. −16.39 −10.92 −3.19 | - | |||||
| Hoftijzer et al. (2007) [18] Netherlands | 153 | TT | DTC | 100 | N/a | 0.3–41.8 y. | SF-36 MFI-20 | Role limitations due to emotional health Role limitations due to physical health Social functioning and interactions Reduced activity | - | - | −2.71 −8.03 −6.97 +1.61 | - | ||||||
| Karapanou et al. (2012) [55] Greece | 60 | TT | PTC | 100 | N/a | 2–6 m. | SF-36 | Role limitations due to emotional health Role limitations due to physical health Social functioning and interactions | - | - | −7.22 −11.25 −9.17 | - | ||||||
| Li et al. (2020) [58] China | 174 | TT | DTC | 100 | N/a | 1 y. | SF-36 | Role limitations due to emotional health Role limitations due to physical health Social functioning and interactions | - | - | −10.0 −7.1 −7.6 | - | ||||||
| Nies et al. (2017) [61] Netherlands | 67 | TT | DTC | 97 | Permanent hypoPTH: 25.4 RLNi: 14.9 | 5–44.7 y (mean 17.8 y.) | SF-36 MFI-20 | Role limitations due to emotional health Role limitations due to physical health Social functioning and interactions Reduced activity | - | - | = = −12 = | - | ||||||
| Pelttari et al. (2009) [34] Finland | 341 | TT (98.8%) | 94.5% PTC 5.5% FTC | 84.5 | RLNi: 1.4 Permanent hypoPTH: 1.7 | 5–19.5 y. (mean 12.4 y.) | 15D instrument | Usual activities | - | - | +0.004 | - | ||||||
| Teliti et al. (2021) [51] Italy | 119 | TT (95.6%) | DTC | 71 | N/a | Mean 9.9 y. | ThyPRO g | Social life impairment Daily life impairment Sex life impairment | - | - | +0.074 +1.199 +0.825 | - | ||||||
| Van Velsen et al. (2019) [68] Netherlands | 185 | TT | 88% PTC 12% FTC | 100 | RLNi: 9.2 Transient hypoPTH: 20.0 Permanent hypoPTH: 16.8 | 2–4 y. | SF-36 ThyPRO | Social functioning Social life impairment Daily life impairment | - | 2 y. +3.2 −0.9 −2.3 | 4 y. +3.6 −1.5 −3.0 | 2 y.☨ −16.8 N/a N/a | 4 y.☨ −16.4 N/a N/a | - | ||||
| Chen et al. (2021) [65] China | 427 365 | HT TT | DTC | 2.3 18.1 | Transient hypoPTH: 6.6 RLNi: 0.4 Transient hoarseness: 21.1 Transient hypoPTH: 32.2 RLNi: 1.6 Transient hoarseness:30.8 | 1 m.–1 y. | EORTC QLC-C30 | Role function Social function Financial difficulties | 1 m. −2.8 −3.7 2.3 | 3 m. −2.96 −2.9 3.8 | 6 m. 1.1 −0.9 2.5 | 1 y. 1.1 1.4 0.5 | - | - | - | |||
| Bongers et al. (2019) [52] Canada | 59 211 | HT TT | 47.5% PTC 52.5% FVPTC e 33.6% PTC 65.4% FVPTC 0.9% FTC | 0 43.6 | Permanent hypoPTH: 0.0 Persistent RLNi: 0.0 Permanent hypoPTH: 6.2 Persistent RLNi: 0.0 | 0.9–12.7 y. | EORTC QLC-C30 EORTC QLQ-THY34 | Role functioning Social functioning Financial difficulties Impact on job Social support | +2.6 +5.8 −4.8 −10.7 +6.7 | - | - | - | ||||||
| Lan et al. (2021) [57] China | 34 35 | HT TT | PTMC | 0 | RLNi: 0.0 RLNi: 8.6 | 0–45 m. | SF-36 FoP-Q-SFi | Role limitations due to emotional health Role limitations due to physical health Social functioning and interactions Social family | −33 −50 −11 = | - | - | - | ||||||
| Lan et al. (2020) [56] China | 18 16 | HT TT | PTMC | N/a | RLNi: 5.9 | Mean 20.3 m. | SF-36 FoP-Q-SF | Role limitations due to emotional health Role limitations due to physical health Social functioning and interactions Social family | −22.4 −31.8 −10.3 +0.26 | - | - | - | ||||||
| Mlees et al. (2022) [59] Egypt | 42 40 | HT TT | Minimally invasive FTC | N/a | Transient hypoPTH: 2.4 Transient hypoPTH: 12.5 Permanent hypoPTH: 2.5 Temporary RLNi: 7.5 Persistent RLNi: 2.5 Seroma: 7.5 Infection: 5.0 | 12 m. | SF-36 | Role limitations due to emotional health Role limitations due to physical health Social functioning and interactions | −5.6 −3.2 +1.9 | - | - | - | ||||||
| Van Gerwen et al. (2021) [62] USA | 34 24 | HT TT | 84.4% PTC 15.5% FTC | 0 | N/a | 2–20 y. | EORTC QLC-C30 | Role functioning Social functioning Financial difficulties | −8.4 −13.1 11.6 | - | - | - | ||||||
| Moon et al. (2020) [67] South Korea | 238 79 500 | HT TT AS | PTMC | N/a | N/a | 6 m. 1 y 1.5 y. ≥2 y. | KT-QoL | Social subscale | −0.5 −0.7 −0.3 0.3 | HT −0.7 −0.4 −1.0 −0.7 | TT −1.2 −1.0 −1.3 −0.4 | |||||||
| Jeon et al. (2019) [54] South Korea | 148 43 | HT AS | PTMC | 0 | Transient hypoPTH: 1.4 - | 14.2–53.0 m. | SF-12 FoP | Role limitations due to emotional health Role limitations due to physical health Social functioning Partnership/family Work Loss of autonomy | - | - | - | −3.09 −2.42 −2.17 +0.03 +0.08 −0.14 | ||||||
| Global HrQoL | ||||||||||||||||||
| Crevanna et al. (2003) [53] Austria | 150 51 (sub-group) | TT | DTC | 100 | RLNi: 3.3 HypoPTH: 16.6 | 0–23 y. (mean 5.5 y.) | SF-36 | General health | - | - | <1 y. +0.5 | 0–23 y. +4.4 | - | |||||
| Hoftijzer et al. (2007) [18] Netherlands | 153 | TT | DTC | 100 | N/a | 0.3–41.8 y. | SF-36 | General health Change in health | - | - | −5.75 −2.62 | - | ||||||
| Karapanou et al. (2012) [55] Greece | 60 | TT | PTC | 100 | N/a | 2–6 m. | SF-36 | General health | - | - | −4.14 | - | ||||||
| Li et al. (2020) [58] China | 174 | TT | DTC | 100 | N/a | 1 y. | SF-36 | General health | - | - | −11.7 | - | ||||||
| Pelttari et al. (2009) [34] Finland | 341 | TT (98.8%) | 95% PTC 5% FTC | 84.5 | RLNi: 1.4 Permanent hypoPTH: 1.7 | 5–19.5 y. (mean 12.4 y.) | 15D instrument | Global score | - | - | −0.002 | - | ||||||
| Van Velsen et al. (2019) [68] Netherlands | 185 | TT | 88% PTC 12% FTC | 100 | RLNi: 9.2 Transient hypoPTH: 20.0 Permanent hypoPTH: 16.8 | 2–4 y. | SF-36 ThyPRO | General health perception Composite score | - | 2 y. −0.5 −1.7 | 4 y. −1.0 −2.5 | 2 y.☨ −15.3 N/a | 4 y.☨ −15.8 N/a | - | ||||
| Doubleday et al. (2020) [73] USA | 62 | TT | DTC | N/a | Transient hypoPTH: 4.8 | 2 w. 6 w. 6 m. 1 y. | EORTC QLC-C30 | Global scale | - | −3.63 +0.65 +8.38 +11.6 | - | - | ||||||
| Lubitz et al. (2017) [66] USA | 95 | TT (96%) | 74% PTC 16% FVPTC | 49 | HypoPTH: 5.0 Hematoma: 1.0 RLNi: 3.3 | 2–4 w. 6–12 m. | EQ5D-5L SF-6D HUI2 HUI3 | Global scores | - | 2–4 w. 0.02 0.04 0.01 0.02 | 6–12 m −0.00 −0.01 0.01 0.02 | - | - | |||||
| Chen et al. (2021) [65] China | 427 365 | HT TT | DTC | 2.3 18.1 | Transient hypoPTH: 6.6 RLNi: 0.4 Transient hoarseness: 21.1 Transient hypoPTH: 32.2 RLNi: 1.6 Transient hoarseness: 30.8 | 1 m.–1 y | EORTC QLC-C30 | Global scale | 1 m. −2.1 | 3 m. −2.9 | 6 m. −1.0 | 1 y. −0.04 | - | - | - | |||
| Bongers et al. (2019) [52] Canada | 59 211 | HT TT | 47.5% PTC 52.5% FVPTC e 33.6% PTC 65.4% FVPTC 0.9% FTC | 0 43.6 | Permanent hypoPTH: 0.0 Persistent RLNi: 0.0 Permanent hypoPTH: 6.2 Persistent RLNi: 0.0 | 0.9–12.7 y. | EORTC QLC-C30 | Global scale | +0.80 | - | - | - | ||||||
| Lan et al. (2021) [57] China | 34 35 | HT TT | PTMC | 0 | RLNi: 0.0 RLNi: 8.6 | 0–45 m. | SF-36 | General health | −4.00 | - | - | - | ||||||
| Lan et al. (2020) [56] China | 18 16 | HT TT | PTMC | N/a | RLNi: 5.9 | Mean 20.29 m. | SF-36 | General health | −4.72 | - | - | - | ||||||
| Mlees et al. (2022) [59] Egypt | 42 40 | HT TT | Minimally invasive FTC | N/a | Transient hypoPTH: 2.4 Transient hypoPTH: 12.5 Permanent hypoPTH: 2.5 Temporary RLNi: 7.5 Persistent RLNi: 2.5 Seroma: 7.5 Infection: 5.0 | 12 m. | SF-36 | General health | −3.1 | - | - | - | ||||||
| Van Gerwen et al. (2021) [62] USA | 34 24 | HT TT | 84.4% PTC 15.5% FTC | 0 | N/a | 2–20 y. | EORTC QLC-C30 | Global health | −1.9 | - | - | - | ||||||
| Moon et al. (2020) [67] South Korea | 238 79 500 | HT TT AS | PTMC | N/a | N/a | 6 m. 1 y 1.5 y. ≥2. y. | KT-QoL | Global subscale | −0.5 −0.4 −0.5 −0.02 | HT −0.6 −0.4 −0.7 −0.4 | TT −1.0 −0.8 −1.1 −0.5 | |||||||
| Jeon et al. (2019) [54] South Korea | 148 43 | HT AS | PTMC | 0 | Transient hypoPTH: 1.4 - | 14.2–53.0 m. | SF-12 | General health | - | - | - | −1.65 | ||||||
| Study and Country | Sample Size | Surgery Extent | Pathology Details | RAI (%) | Time of QoL Assessment | Methodology | Identified Themes | Frequency of Responses (%) | Conclusion | |
|---|---|---|---|---|---|---|---|---|---|---|
| Diamond-Rossi et al. (2020) [72] USA | 47 | TT | 87% PTC a 13% FTC b | 100 | 0.17 to 10 y. post-RAI (mean 3.9 y. post-RAI) | Thematic analysis Focus groups | Xerostomia (dry mouth) Salivary gland dysfunction Xeropthalmia (dry eyes) Epiphora (Eye tearing) Dysgeusia (altered taste) Epistaxis Lack of knowledge and preparation for treatment Regret of treatment Distress that thyroid cancer is labeled as a “good cancer” | 18.3 14.8 18.9 16.8 19.8 4.2 N/a N/a N/a | Thyroid cancer survivors reported a wide range of RAI treatment-related effects and psychosocial concerns that appear to reduce quality of life. The psychosocial concerns reported by participants underscore the significant unmet information and support needs prior to and following RAI treatment among DTC patients. | |
| Doubleday et al. (2020) [73] USA | 62 | TT | DTC | N/a | Preop c Postop d 2 w. Postop 6 w. Postop 6 m. Postop 1 y. | Grounded theory analysis Semistructured interviews | Numbness and tingling Minor symptoms Interference of symptoms with life (major symptoms); Sleep disturbance: nighttime symptoms and difficult medication schedule; Unclear attribution of symptoms: muscle cramps; Symptom persistence and frustration; Concerns/problems with high calcium carbonate intake: nausea and frustration; Fear of calcium overdose; Felt self-conscious; Knew what to expect; Felt supported; Adaptation | Postop: 2 w.: 51 6 w.:27 1 y.: 40 | Early postoperative transient hypoparathyroidism is common, but when appropriately managed did not have a substantial negative impact on the overall quality of life. | |
| Hedman et al. (2017) [69] Sweden | 21 | TT | 71% PTC 29% FTC | 100 | 3 m.–18 y. since diagnosis (mean 4 y.) | Content analysis Semistructured interviews | Anxiety Contraindications: hidden anxiety Distrust as a source of anxiety Protective strategies | N/a N/a N/a N/a | Anxiety is a common—although partially hidden—problem in DTC survivors, as they tended to deny it early in the dialogues. As anxiety is clearly related to follow-up routines, these should therefore be reevaluated. | |
| Kletzien et al. (2018) [70] USA | 42 | TT | PTC | N/a | Preop Postop 2 w Postop 6 w Postop 6 m Postop 1 y | Grounded theory analysis Semistructured interviews | Any concerns or symptoms of impaired communication | Preop: 5 Postop: 2 w.: 57 6 w.: 44 6 m.: 31 1 y.: 50 | Voice changes are common after surgery for papillary thyroid cancer and affect quality of life for many patients even after 1 year of follow-up. | |
| Nickel et al. (2019) [71] Australia | 791 214 | TT HT | 89% PTC 11% FTC | 33 | 2–91 w. post-diagnosis (Median 23.1 w.) | Content analysis Structured telephone interview | Overall physical symptoms Fatigue Medication issues Voice issues Throat/neck discomfort Weight concerns Autonomic symptoms Other physical symptoms Overall psychological symptoms Emotional distress Mood issues Anxiety/depression Re-evaluation of life Overall lifestyle Impact on work Increased consciousness about health/lifestyle No adverse effects or issues overall No adverse effects Minor impact relative to other issues | HT 54.2 28.5 15.9 9.3 8.4 7.0 5.1 10.7 19.2 14.5 3.3 2.3 1.4 4.2 1.9 2.3 34.6 34.1 0.5 | TT 69.2 35.3 24.4 12.6 10.9 6.8 4.9 14.2 18.4 12.6 4.0 3.2 1.5 9.2 5.6 3.9 21.7 19.8 1.9 | According to the results of this study, patients diagnosed with DTC report wide-ranging HrQoL issues; these seem more prevalent among patients who undergo total thyroidectomies (with or without neck dissection) rather than hemithyroidectomies. For patients with small, localized DTCs, hemithyroidectomy may offer fewer adverse effects of treatment and better HrQoL outcomes than total thyroidectomy. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Landry, V.; Siciliani, E.; Henry, M.; Payne, R.J. Health-Related Quality of Life following Total Thyroidectomy and Lobectomy for Differentiated Thyroid Carcinoma: A Systematic Review. Curr. Oncol. 2022, 29, 4386-4422. https://doi.org/10.3390/curroncol29070350
Landry V, Siciliani E, Henry M, Payne RJ. Health-Related Quality of Life following Total Thyroidectomy and Lobectomy for Differentiated Thyroid Carcinoma: A Systematic Review. Current Oncology. 2022; 29(7):4386-4422. https://doi.org/10.3390/curroncol29070350
Chicago/Turabian StyleLandry, Vivianne, Elizabeth Siciliani, Melissa Henry, and Richard J. Payne. 2022. "Health-Related Quality of Life following Total Thyroidectomy and Lobectomy for Differentiated Thyroid Carcinoma: A Systematic Review" Current Oncology 29, no. 7: 4386-4422. https://doi.org/10.3390/curroncol29070350
APA StyleLandry, V., Siciliani, E., Henry, M., & Payne, R. J. (2022). Health-Related Quality of Life following Total Thyroidectomy and Lobectomy for Differentiated Thyroid Carcinoma: A Systematic Review. Current Oncology, 29(7), 4386-4422. https://doi.org/10.3390/curroncol29070350






