Inflammatory Indexes as Predictive Biomarkers of Postoperative Complications in Oncological Thoracic Surgery
Abstract
:1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef] [PubMed]
- Didkowska, J.; Wojciechowska, U.; Mańczuk, M.; Łobaszewski, J. Lung cancer epidemiology: Contemporary and future challenges worldwide. Ann. Transl. Med. 2016, 4, 150. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Coussens, L.M.; Werb, Z. Inflammation and cancer. Nature 2002, 420, 860–867. [Google Scholar] [CrossRef] [PubMed]
- Grivennikov, S.I.; Greten, F.R.; Karin, M. Immunity, inflammation, and cancer. Cell 2010, 140, 883–899. [Google Scholar] [CrossRef] [Green Version]
- Greten, F.R.; Grivennikov, S.I. Inflammation and Cancer: Triggers, Mechanisms, and Consequences. Immunity 2019, 51, 27–41. [Google Scholar] [CrossRef]
- Ying, H.Q.; Deng, Q.W.; He, B.S.; Pan, Y.Q.; Wang, F.; Sun, H.L.; Chen, J.; Liu, X.; Wang, S.K. The prognostic value of preoperative NLR, d-NLR, PLR and LMR for predicting clinical outcome in surgical colorectal cancer patients. Med. Oncol. 2014, 31, 305. [Google Scholar] [CrossRef]
- Łochowski, M.; Łochowska, B.; Zawadzka, I.; Cieślik-Wolski, B.; Kozik, D.; Kozak, J. Prognostic value of neutrophil-to-lymphocyte, platelet-to-lymphocyte and lymphocyte-to-monocyte ratio ratios in patients operated on due to non-small cell lung cancer. J. Thorac. Dis. 2019, 11, 3377–3384. [Google Scholar] [CrossRef]
- Yamagishi, T.; Fujimoto, N.; Nishi, H.; Miyamoto, Y.; Hara, N.; Asano, M.; Fuchimoto, Y.; Wada, S.; Kitamura, K.; Ozaki, S.; et al. Prognostic significance of the lymphocyte-to-monocyte ratio in patients with malignant pleural mesothelioma. Lung Cancer 2015, 90, 111–117. [Google Scholar] [CrossRef]
- Drpa, G.; Sutic, M.; Baranasic, J.; Jakopovic, M.; Samarzija, M.; Kukulj, S.; Knezevic, J. Neutrophil-to-lymphocyte ratio can predict outcome in extensive-stage small cell lung cancer. Radiol. Oncol. 2020, 54, 437–446. [Google Scholar] [CrossRef]
- Guo, M.; Li, W.; Li, B.; Zou, B.; Wang, S.; Meng, X.; Sun, X.; Yu, J.; Wang, L. Prognostic value of delta inflammatory biomarker-based nomograms in patients with inoperable locally advanced NSCLC. Int. Immunopharmacol. 2019, 72, 395–401. [Google Scholar] [CrossRef]
- Wang, Y.; Hu, X.; Xu, W.; Wang, H.; Huang, Y.; Che, G. Prognostic value of a novel scoring system using inflammatory response biomarkers in non-small cell lung cancer: A retrospective study. Thorac. Cancer 2019, 10, 1402–1411. [Google Scholar] [CrossRef] [PubMed]
- Qi, Q.; Zhuang, L.; Shen, Y.; Geng, Y.; Yu, S.; Chen, H.; Liu, L.; Meng, Z.; Wang, P.; Chen, Z. A novel systemic inflammation response index (SIRI) for predicting the survival of patients with pancreatic cancer after chemotherapy. Cancer 2016, 122, 2158–2167. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, S.; Yang, Z.; Du, H.; Zhang, W.; Che, G.; Liu, L. Novel systemic inflammation response index to predict prognosis after thoracoscopic lung cancer surgery: A propensity score-matching study. ANZ J. Surg. 2019, 89, E507–E513. [Google Scholar] [CrossRef] [PubMed]
- Shen, Y.J.; Qian, L.Q.; Ding, Z.P.; Luo, Q.Q.; Zhao, H.; Xia, W.Y.; Fu, Y.Y.; Feng, W.; Zhang, Q.; Yu, W.; et al. Prognostic Value of Inflammatory Biomarkers in Patients With Stage I Lung Adenocarcinoma Treated With Surgical Dissection. Front. Oncol. 2021, 11, 711206. [Google Scholar] [CrossRef]
- Qi, W.X.; Xiang, Y.; Zhao, S.; Chen, J. Assessment of systematic inflammatory and nutritional indexes in extensive-stage small-cell lung cancer treated with first-line chemotherapy and atezolizumab. Cancer Immunol. Immunother. 2021, 70, 3199–3206. [Google Scholar] [CrossRef]
- Zinellu, A.; Collu, C.; Nasser, M.; Paliogiannis, P.; Mellino, S.; Zinellu, E.; Traclet, J.; Ahmad, K.; Mangoni, A.A.; Carru, C.; et al. The Aggregate Index of Systemic Inflammation (AISI): A Novel Prognostic Biomarker in Idiopathic Pulmonary Fibrosis. J. Clin. Med. 2021, 10, 4134. [Google Scholar] [CrossRef]
- Ziarnik, E.; Grogan, E.L. Postlobectomy Early Complications. Thorac. Surg. Clin. 2015, 25, 355–364. [Google Scholar] [CrossRef] [Green Version]
- LaPar, D.J.; Bhamidipati, C.M.; Lau, C.L.; Jones, D.R.; Kozower, B.D. The Society of Thoracic Surgeons General Thoracic Surgery Database: Establishing generalizability to national lung cancer resection outcomes. Ann. Thorac. Surg. 2012, 94, 216–221. [Google Scholar] [CrossRef]
- Shapiro, M.; Swanson, S.J.; Wright, C.D.; Chin, C.; Sheng, S.; Wisnivesky, J.; Weiser, T.S. Predictors of major morbidity and mortality after pneumonectomy utilizing the Society for Thoracic Surgeons General Thoracic Surgery Database. Ann. Thorac. Surg. 2010, 90, 927–935. [Google Scholar] [CrossRef]
- Paliogiannis, P.; Ginesu, G.C.; Tanda, C.; Feo, C.F.; Fancellu, A.; Fois, A.G.; Mangoni, A.A.; Sotgia, S.; Carru, C.; Porcu, A.; et al. Inflammatory cell indexes as preoperative predictors of hospital stay in open elective thoracic surgery. ANZ J. Surg. 2018, 88, 616–620. [Google Scholar] [CrossRef]
- Mohri, Y.; Tanaka, K.; Toiyama, Y.; Ohi, M.; Yasuda, H.; Inoue, Y.; Kusunoki, M. Impact of Preoperative Neutrophil to Lymphocyte Ratio and Postoperative Infectious Complications on Survival After Curative Gastrectomy for Gastric Cancer: A Single Institutional Cohort Study. Medicine 2016, 95, e3125. [Google Scholar] [CrossRef] [PubMed]
- Ortiz-López, D.; Acosta-Mérida, M.A.; Casimiro-Pérez, J.A.; Silvestre-Rodríguez, J.; Marchena-Gómez, J. First day postoperative values of the neutrophil-to-lymphocyte ratio, platelet-to-lymphocyte ratio, and C-reactive protein as complication predictors following gastric oncologic surgery. Valor del Ratio Neutrófilo-Linfocito, Ratio Plaqueta-Linfocito y Proteína C Reactiva del primer día como predictores de complicaciones postoperatorias tras cirugía oncológica gástrica. Rev. Gastroenterol. Mex. 2021. [Google Scholar] [CrossRef]
- Paliogiannis, P.; Deidda, S.; Maslyankov, S.; Paycheva, T.; Farag, A.; Mashhour, A.; Misiakos, E.; Papakonstantinou, D.; Mik, M.; Losinska, J.; et al. Blood cell count indexes as predictors of anastomotic leakage in elective colorectal surgery: A multicenter study on 1432 patients. World J. Surg. Oncol. 2020, 18, 89. [Google Scholar] [CrossRef] [PubMed]
- Miyakita, H.; Sadahiro, S.; Saito, G.; Okada, K.; Tanaka, A.; Suzuki, T. Risk scores as useful predictors of perioperative complications in patients with rectal cancer who received radical surgery. Int. J. Clin. Oncol. 2017, 22, 324–331. [Google Scholar] [CrossRef] [Green Version]
- Vaughan-Shaw, P.G.; Rees, J.R.; King, A.T. Neutrophil lymphocyte ratio in outcome prediction after emergency abdominal surgery in the elderly. Int. J. Surg. 2012, 10, 157–162. [Google Scholar] [CrossRef] [Green Version]
- Giakoumidakis, K.; Fotos, N.V.; Patelarou, A.; Theologou, S.; Argiriou, M.; Chatziefstratiou, A.A.; Katzilieri, C.; Brokalaki, H. Perioperative neutrophil to lymphocyte ratio as a predictor of poor cardiac surgery patient outcomes. Pragmat. Obs. Res. 2017, 8, 9–14. [Google Scholar] [CrossRef] [Green Version]
- Lan, H.; Zhou, L.; Chi, D.; Zhou, Q.; Tang, X.; Zhu, D.; Yue, J.; Liu, B. Preoperative platelet to lymphocyte and neutrophil to lymphocyte ratios are independent prognostic factors for patients undergoing lung cancer radical surgery: A single institutional cohort study. Oncotarget 2017, 8, 35301–35310. [Google Scholar] [CrossRef] [Green Version]
| Global Cohort (n = 249) | Open Surgery (n = 184) | VATS (n = 65) | p-Value | |
|---|---|---|---|---|
| Age, years | 66 (58–72) | 66 (59–72) | 64 (50–72) | 0.21 |
| Gender, females (%) | 67 (26.9) | 45 (24.5) | 22 (33.8) | 0.14 |
| BMI | 25.4 ± 4.1 | 25.4 ± 4.1 | NA | NA |
| Non-smokers, (%) | 48 (19.3) | 27 (14.7) | 21 (32.3) | 0.002 |
| Pack Years | 37 (16–60) | 38 (17–60) | 31 (10–60) | 0.5 |
| ASA score | I 89; II 83; | I 73; II 61; | I 16; II 22; | 0.085 |
| III 60; NA 17 | III 38; NA 12 | III 22; NA 5 | <0.000001 | |
| Surgery duration, hours | 3.0 (2.1–4.0) | 3.5 (2.5–4.5) | 2.0 (1.0–2.4) | <0.000001 |
| Hospital Stay, days | 8.0 (5.0–10.0) | 9.0 (7.0–11.0) | 5.0 (3.0–6.5) | 0.036 |
| Complications, (%) | 58 (23.3) | 49 (26.6) | 9 (13.8) | 0.21 |
| Surgery Type | <0.0001 | |||
| Lobectomy, n (%) | 139 (55.8) | 129 (70.1) | 10 (15.4) | |
| Wedge resection, n (%) | 67 (26.9) | 31 (16.8) | 36 (55.4) | |
| Pneumonectomy, n (%) | 9 (3.6) | 9 (4.9) | 0 (0) | |
| Explorative procedure, n (%) | 17 (6.8) | 6 (3.2) | 11 (16.9) | |
| Other, n (%) | 17 (6.8) | 9 (4.9) | 8 (12.3) | |
| Blood Cell Count—Indexes | ||||
| Lymphocytes, (×109/L) | 1.9 (1.5–2.4) | 1.9 (1.5–2.4) | 2.0 (1.5–2.5) | 0.77 |
| Monocytes, (×109/L) | 0.5 (0.4–0.6) | 0.5 (0.4–0.7) | 0.4 (0.3–0.6) | 0.05 |
| Neutrophils, (×109/L) | 4.6 (3.5–5.7) | 4.5 (3.5–5.7) | 4.7 (3.0–5.4) | 0.28 |
| Platelets, (×109/L) | 255 (209–333) | 256 (210–333) | 248 (208–331) | 0.80 |
| RDW, (fL) | 13.7 (12.9–14.8) | 13.8 (13.0–14.8) | 13.4 (12.7–14.8) | 0.16 |
| MPV, (fL) | 8.3 (7.6–8.9) | 8.3 (7.7–9.0) | 8.1 (7.4–8.6) | 0.42 |
| NLR | 2.3 (1.7–3.3) | 2.4 (1.7–3.3) | 2.0 (1.5–3.3) | 0.17 |
| PLR | 137 (98–189) | 137 (101–188) | 139 (94–190) | 0.79 |
| LMR | 4.4 (2.8–5.3) | 3.8 (2.8–5.0) | 4.5 (2.8–6.7) | 0.03 |
| SIRI | 1.1 (0.7–1.8) | 1.2 (0.8–1.8) | 1.0 (0.5–1.7) | 0.05 |
| AISI | 281 (163–565) | 316 (181–573) | 246 (121–448) | 0.05 |
| Complications (All) | Complications (Open) | Complications (Vats) | ||
|---|---|---|---|---|
| NLR | Preoperative | rho = 0.00, p = 0.96 | rho = 0.03, p = 0.65 | rho = −0.18, p = 0.17 |
| 1st postop day | rho = −0.07, p = 0.29 | rho = −0.10, p = 0.19 | rho = 0.03, p = 0.84 | |
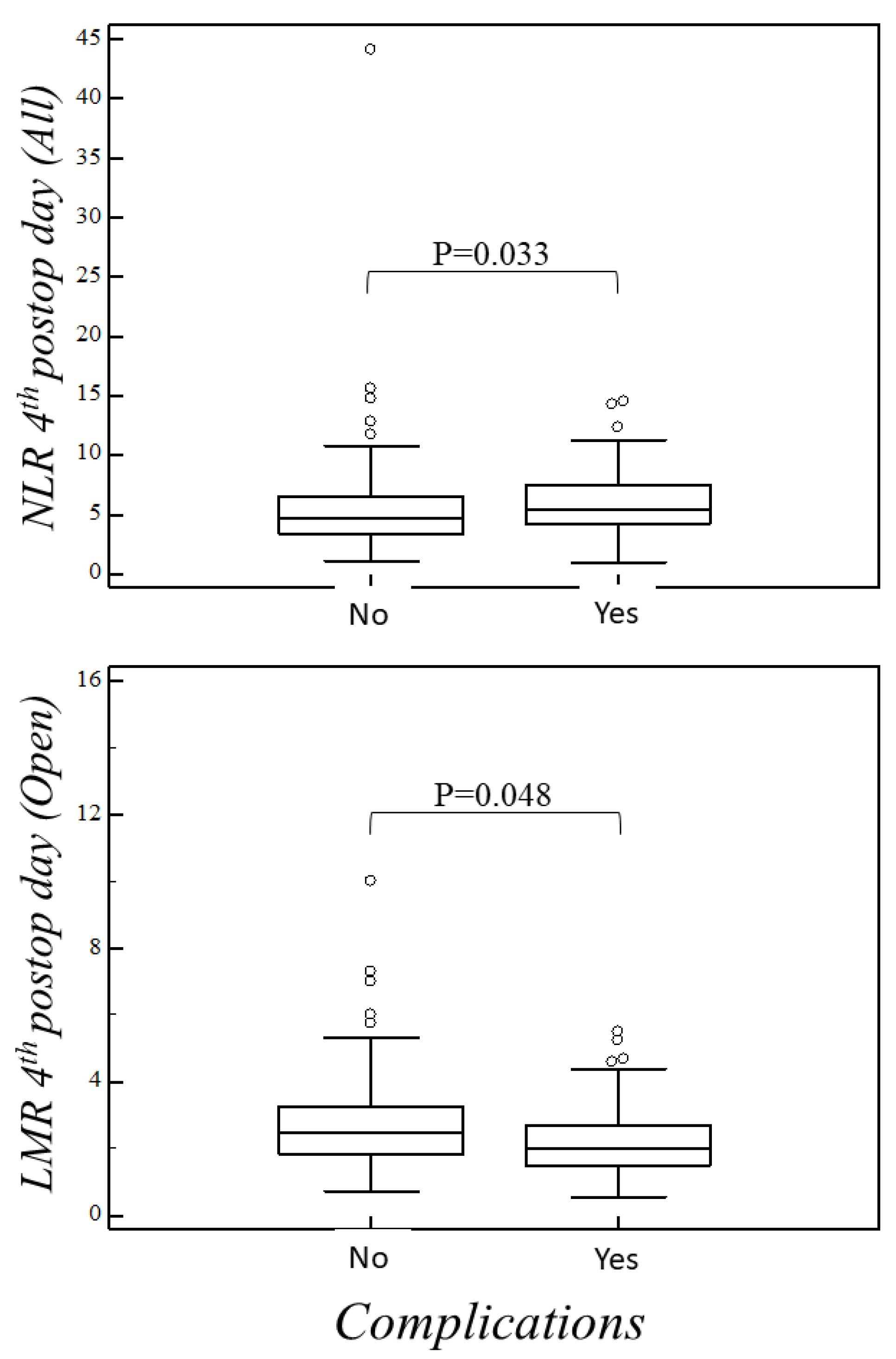
| 4th postop day | rho = 0.15, p = 0.03 | rho = 0.14, p = 0.07 | rho = 0.14, p = 0.37 | |
| PLR | Preoperative | rho = 0.01, p = 0.87 | rho = 0.01, p = 0.88 | rho = 0.00, p = 0.92 |
| 1st postop day | rho = −0.03, p = 0.65 | rho = −0.04, p = 0.63 | rho = 0.02, p = 0.90 | |
| 4th postop day | rho = 0.10, p = 0.17 | rho = 0.09, p = 0.24 | rho = 0.12, p = 0.44 | |
| LMR | Preoperative | rho = −0.03, p = 0.60 | rho = −0.06, p = 0.39 | rho = 0.13, p = 0.32 |
| 1st postop day | rho = 0.02, p = 0.74 | rho = 0.00, p = 0.96 | rho = 0.15, p = 0.26 | |
| 4th postop day | rho = −0.11, p = 0.10 | rho = −0.15, p = 0.048 | rho = 0.07, p = 0.63 | |
| SIRI | Preoperative | rho = 0.27, p = 0.68 | rho = 0.07, p = 0.38 | rho = −0.18, p = 0.17 |
| 1st postop day | rho = −0.05, p = 0.43 | rho = −0.04, p = 0.61 | rho = −0.17, p = 0.22 | |
| 4th postop day | rho = 0.11, p = 0.12 | rho = 0.14, p = 0.07 | rho = −0.07, p = 0.63 | |
| AISI | Preoperative | rho = 0.03, p = 0.68 | rho = 0.06, p = 0.40 | rho = −0.18, p = 0.17 |
| 1st postop day | rho = −0.02, p = 0.77 | rho = 0.00, p = 0.97 | rho = −0.10, p = 0.44 | |
| 4th postop day | rho = 0.09, p = 0.10 | rho = 0.13, p = 0.10 | rho = −0.04, p = 0.77 |
| Hospital Stay (All) | Hospital Stay (Open) | Hospital Stay (VATS) | ||
|---|---|---|---|---|
| NLR | Preoperative | rho = 0.12, p = 0.06 | rho = 0.13, p = 0.08 | rho = 0.06, p = 0.67 |
| 1st postop day | rho = 0.24, p = 0.004 | rho = 0.16, p = 0.043 | rho = 0.12, p = 0.38 | |
| 4th postop day | rho = 0.23, p = 0.001 | rho = 0.19, p = 0.013 | rho= 0.10, p = 0.51 | |
| PLR | Preoperative | rho = 0.04, p = 0.55 | rho = 0.04, p = 0.61 | rho = 0.16, p = 0.22 |
| 1st postop day | rho = 0.11, p = 0.10 | rho = 0.13, p = 0.09 | rho = 0.16, p = 0.23 | |
| 4th postop day | rho = 0.19, p = 0.007 | rho = 0.17, p = 0.03 | rho = 0.27, p = 0.07 | |
| LMR | Preoperative | rho = −0.13, p = 0.046 | rho = −0.11, p = 0.13 | rho = 0.05, p = 0.71 |
| 1st postop day | rho = −0.16, p = 0.016 | rho = −0.15, p = 0.055 | rho = 0.02, p = 0.88 | |
| 4th postop day | rho = −0.11, p = 0.10 | rho = −0.11, p = 0.14 | rho = 0.11, p = 0.46 | |
| SIRI | Preoperative | rho = 0.17, p = 0.008 | rho = 0.20, p = 0.009 | rho = 0.00, p = 0.97 |
| 1st postop day | rho = 0.21, p = 0.002 | rho = 0.21, p = 0.007 | rho = −0.02, p = 0.87 | |
| 4th postop day | rho = 0.17, p = 0.014 | rho = 0.17, p = 0.03 | rho = −0.14 p = 0.36 | |
| AISI | Preoperative | rho = 0.18, p = 0.005 | rho = 0.21, p = 0.006 | rho = 0.06, p = 0.64 |
| 1st postop day | rho = 0.22, p = 0.001 | rho = 0.24, p = 0.002 | rho = 0.08, p = 0.55 | |
| 4th postop day | rho = 0.17, p = 0.01 | rho = 0.18, p = 0.02 | rho = −0.02, p = 0.88 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ginesu, G.C.; Paliogiannis, P.; Feo, C.F.; Cossu, M.L.; Scanu, A.M.; Fancellu, A.; Fois, A.G.; Zinellu, A.; Perra, T.; Veneroni, S.; et al. Inflammatory Indexes as Predictive Biomarkers of Postoperative Complications in Oncological Thoracic Surgery. Curr. Oncol. 2022, 29, 3425-3432. https://doi.org/10.3390/curroncol29050276
Ginesu GC, Paliogiannis P, Feo CF, Cossu ML, Scanu AM, Fancellu A, Fois AG, Zinellu A, Perra T, Veneroni S, et al. Inflammatory Indexes as Predictive Biomarkers of Postoperative Complications in Oncological Thoracic Surgery. Current Oncology. 2022; 29(5):3425-3432. https://doi.org/10.3390/curroncol29050276
Chicago/Turabian StyleGinesu, Giorgio Carlo, Panagiotis Paliogiannis, Claudio F. Feo, Maria Laura Cossu, Antonio Mario Scanu, Alessandro Fancellu, Alessandro Giuseppe Fois, Angelo Zinellu, Teresa Perra, Simone Veneroni, and et al. 2022. "Inflammatory Indexes as Predictive Biomarkers of Postoperative Complications in Oncological Thoracic Surgery" Current Oncology 29, no. 5: 3425-3432. https://doi.org/10.3390/curroncol29050276
APA StyleGinesu, G. C., Paliogiannis, P., Feo, C. F., Cossu, M. L., Scanu, A. M., Fancellu, A., Fois, A. G., Zinellu, A., Perra, T., Veneroni, S., & Porcu, A. (2022). Inflammatory Indexes as Predictive Biomarkers of Postoperative Complications in Oncological Thoracic Surgery. Current Oncology, 29(5), 3425-3432. https://doi.org/10.3390/curroncol29050276












