Patient-Reported Outcomes Measurement in Radiation Oncology: Interpretation of Individual Scores and Change over Time in Clinical Practice
Abstract
:1. Introduction
1.1. Purpose and Context
1.2. Approach
2. Results
2.1. Types of Differential Item Functioning (DIF)
- (1)
- Lack of scalar invariance: individuals interpret the items and/or response scales differently from other people.
- (2)
- Lack of metric invariance: individuals assigning different meanings to items used for measuring a construct (e.g., health).
- (3)
- Lack of configural invariance: individuals not defining the construct (e.g., health) the same as other people.
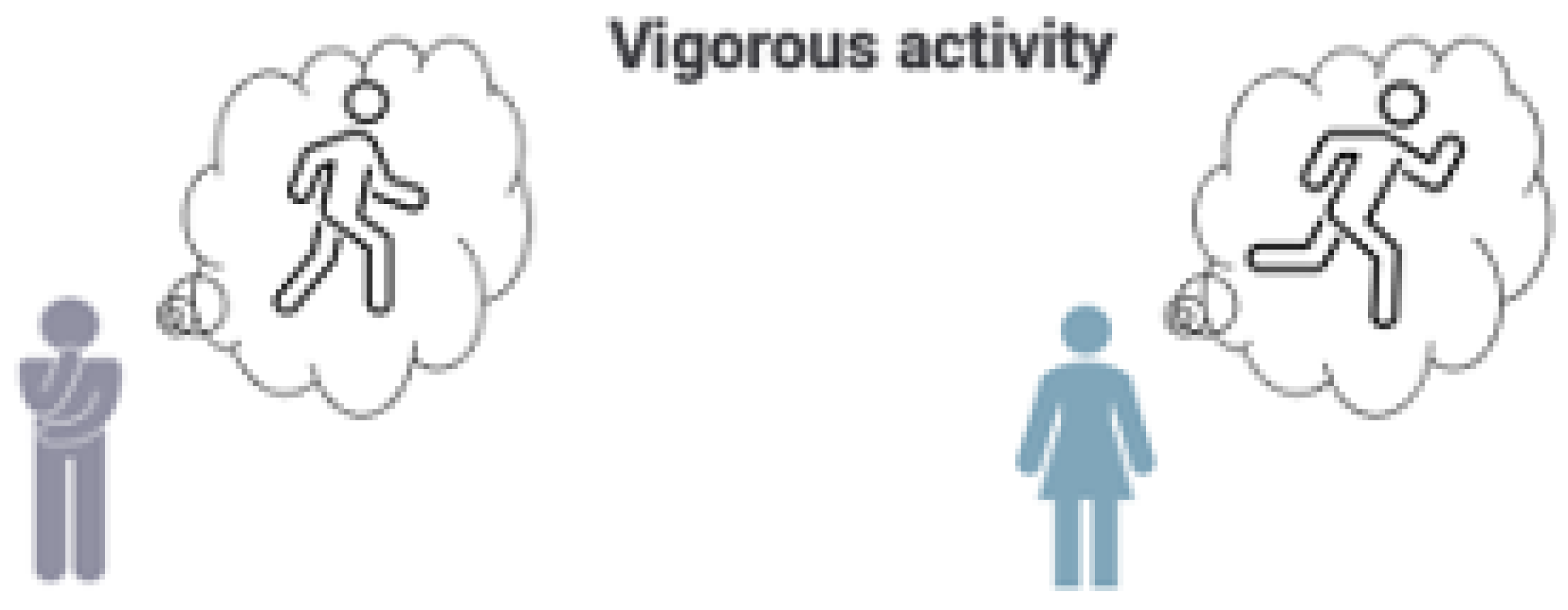
- Clinician:
- Bill, you rated vigorous activity as moderately difficult. Many of my other patients who are very active think of running when they are imagining a vigorous activity. Is that what you were thinking of when rating vigorous activity as moderately difficult?
- Bill:
- Ah, I see what you mean. For me, vigorous activity does not mean running, but rather, being able to walk around my neighborhood without losing my breath.
- Clinician:
- Bill, you rated the “worrying about dying” item as “very much”, and this raises an important question. In answering this question, are you concerned about the quality of your life or the length of your life, or both? Let me put this in the context of cancer treatment: some patients choose a treatment with a goal to prolong their life, while others are more concerned with potential side effects and complications that could affect their quality of life.
- Bill:
- I would rather live a shorter life where I could do more with better quality of life than take a chance on treatment that may extend my life, but result in significant complications.
- Clinician:
- That’s important to know. Let’s talk more about different treatment options and their potential side effects that could affect your quality of life.
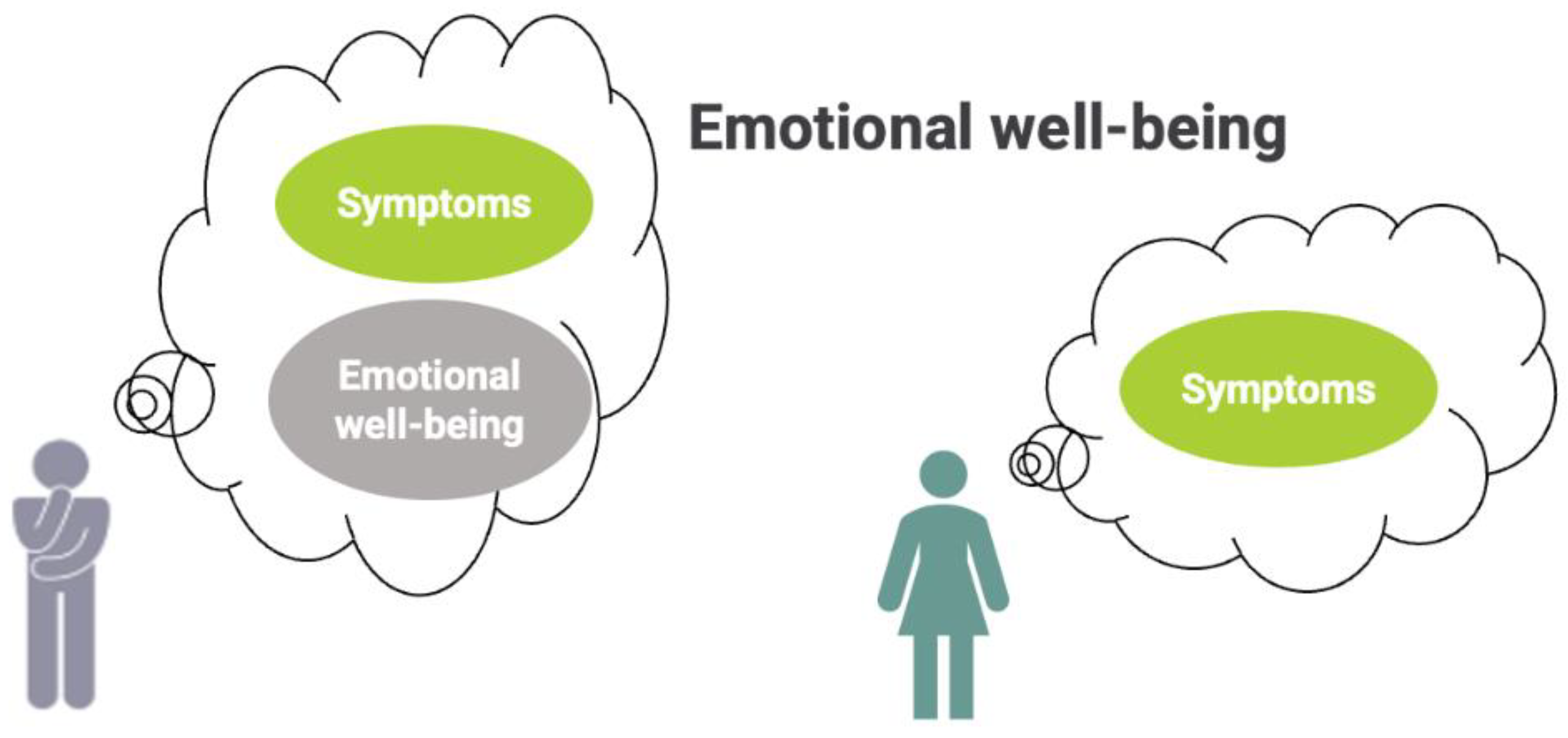
- Clinician:
- You rated your overall health rating as being quite low, even though you report no symptoms. Can you tell me more about why you’re not happy with your health despite not having any symptoms?
- Bill:
- Well, I don’t have a lot of physical symptoms, but I’m anxious about my cancer diagnosis and sometimes feel down.
- Clinician:
- So, in your case, feeling healthy includes your emotional well-being, and being worried about your diagnosis makes you feel discouraged. That’s understandable. Let me give you some information on resources to help address your concerns about your cancer treatment and improve your overall health.
2.2. Types of Response Shift (RS)
- (1)
- Recalibration: change in internal standards of measurement by which people interpret items and response scales.
- (2)
- Reprioritization: change in the relative importance (i.e., assigned meaning) of domains or items.
- (3)
- Reconceptualization: change in the definition of the target construct.
- Clinician:
- Looking at your PROM scores, I see that you rated your overall pain as an 8 before your radiation therapy, and a 5 afterwards. It’s good that you feel your pain has improved, but you’ve mentioned to me a few times that you’re still experiencing some issues. Can you explain why your pain score improved by 3 points, even though you have discomfort?
- Bill:
- Actually, looking at my “before” and “after” scores side by side and thinking back to how I felt before, I realize that 8/10 was too high. I really feel that 5/10 is a good number for how I feel now, but comparing that to how I felt before, I now think I should have rated my overall pain back then as 6/10.
- Clinician:
- Thanks for explaining. While it seems like your new score suggests that things are getting better, your new perspective on your pain now relative to your pain before treatment improves my understanding of your recovery process. Would you like a referral to a pain specialist to better manage your pain? Is there anything else we could address to improve your overall pain right now?
- Bill:
- You know, that would be great. I really am grateful that I can still walk, but the pain doesn’t seem to be lessening over time.
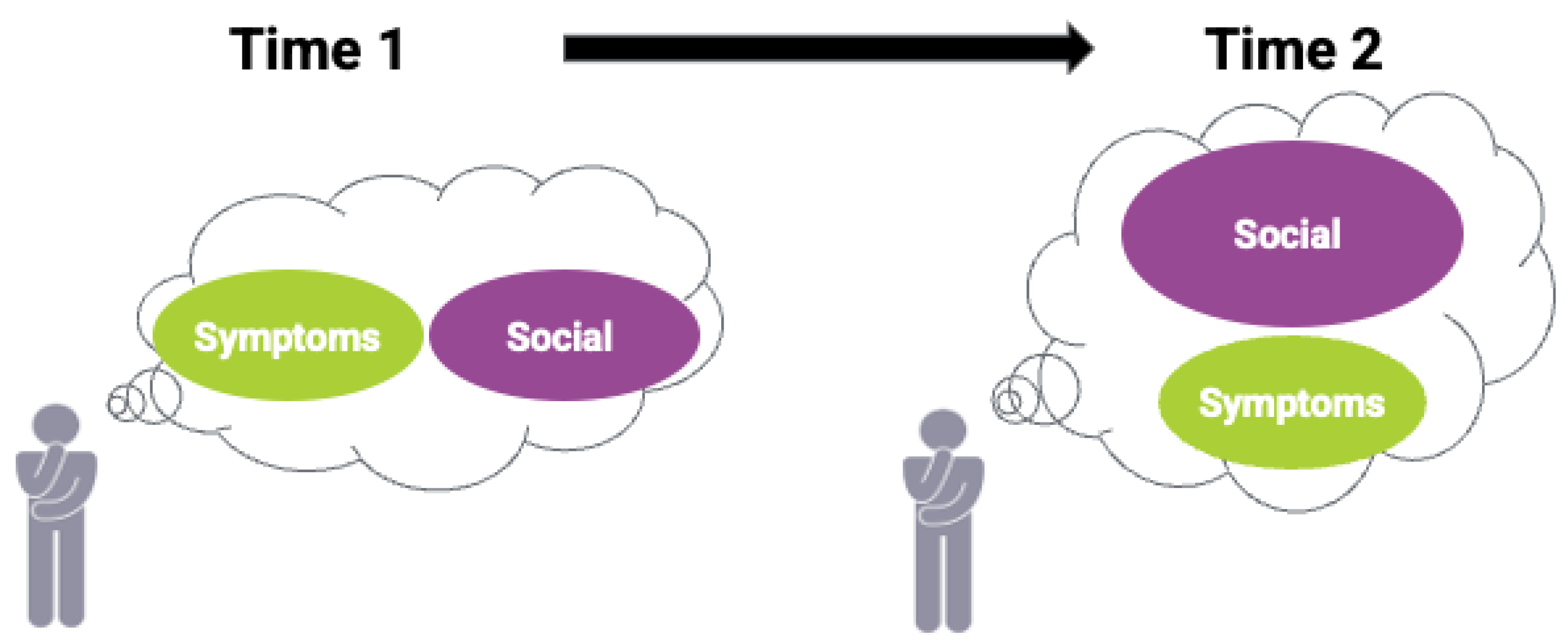
- Clinician:
- I noticed that your latest PROM scores regarding social well-being are different from before. Can you explain your shift in thinking?
- Bill:
- While I valued the time with family and friends before this intense radiation treatment, I thought being cancer-free was equally important to me. But after treatment, I’ve come to realize that while I still want to be cancer-free, spending quality time with family and friends is much more important and wanted to convey that in my latest PROM.
- Clinician:
- That’s good to know. Based on your changed priority, does the current treatment seem to negatively impact your social functioning?
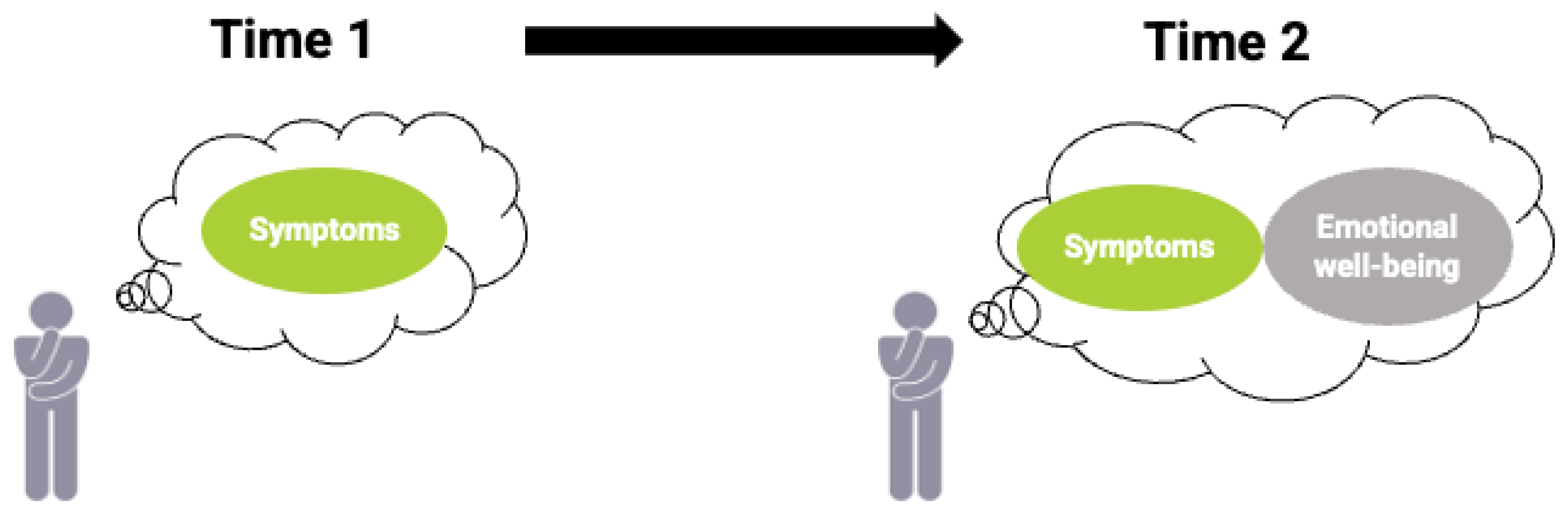
- Clinician:
- Looking at your health questionnaire from before and after radiation therapy, it looks like your overall health scores have improved, even though you are still reporting some pain and depression. Can you explain what has changed for you after treatment?
- Bill:
- There are still symptoms, but I’ve started to meditate, which has helped to reduce my anxiety and improve my sleep. The improvement in my symptom scores reflect that. Thanks for giving me the chance to explain my scores on the questionnaire.
- Clinician:
- You’re welcome. I asked because otherwise it would seem like you were having side effects of treatment and I might have even suggested a different path forward.
3. Discussion
3.1. Implications for Practice
3.2. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- LeBlanc, T.W.; Abernethy, A.P. Patient-Reported Outcomes in Cancer Care—Hearing the Patient Voice at Greater Volume. Nat. Rev. Clin. Oncol. 2017, 14, 763–772. [Google Scholar] [CrossRef] [PubMed]
- van Egdom, L.S.E.; Oemrawsingh, A.; Verweij, L.M.; Lingsma, H.F.; Koppert, L.B.; Verhoef, C.; Klazinga, N.S.; Hazelzet, J.A. Implementing Patient-Reported Outcome Measures in Clinical Breast Cancer Care: A Systematic Review. Value Health 2019, 22, 1197–1226. [Google Scholar] [CrossRef] [PubMed]
- Sawatzky, R.; Kwon, J.-Y.; Barclay, R.; Chauhan, C.; Frank, L.; van den Hout, W.B.; Nielsen, L.K.; Nolte, S.; Sprangers, M.A.G.; Response Shift—In Sync Working Group. Implications of Response Shift for Micro-, Meso-, and Macro-Level Healthcare Decision-Making Using Results of Patient-Reported Outcome Measures. Qual. Life Res. 2021, 30, 3343–3357. [Google Scholar] [CrossRef] [PubMed]
- Laugsand, E.A.; Sprangers, M.A.G.; Bjordal, K.; Skorpen, F.; Kaasa, S.; Klepstad, P. Health Care Providers Underestimate Symptom Intensities of Cancer Patients: A Multicenter European Study. Health Qual. Life Outcomes 2010, 8, 104. [Google Scholar] [CrossRef] [Green Version]
- Datta, S.S.; Ghosal, N.; Daruvala, R.; Chakraborty, S.; Shrimali, R.K.; van Zanten, C.; Parry, J.; Agrawal, S.; Atreya, S.; Sinha, S.; et al. How Do Clinicians Rate Patient’s Performance Status Using the ECOG Performance Scale? A Mixed-Methods Exploration of Variability in Decision-Making in Oncology. Ecancermedicalscience 2019, 13, 913. [Google Scholar] [CrossRef] [Green Version]
- Stiegelis, H.E.; Ranchor, A.V.; Sanderman, R. Psychological Functioning in Cancer Patients Treated with Radiotherapy. Patient Educ. Couns. 2004, 52, 131–141. [Google Scholar] [CrossRef]
- Zugazagoitia, J.; Guedes, C.; Ponce, S.; Ferrer, I.; Molina-Pinelo, S.; Paz-Ares, L. Current Challenges in Cancer Treatment. Clin. Ther. 2016, 38, 1551–1566. [Google Scholar] [CrossRef] [Green Version]
- Magnuson, A.; Elias, R.; Koll, T. Expanding Therapeutic Options for Older Adults: Case-Based Updates in Breast and Lung Cancer. J. Am. Geriatr. Soc. 2019, 67, 1012–1019. [Google Scholar] [CrossRef]
- Jacobs, L.A.; Shulman, L.N. Follow-up Care of Cancer Survivors: Challenges and Solutions. Lancet Oncol. 2017, 18, e19–e29. [Google Scholar] [CrossRef]
- Grewal, A.S.; Berman, A.T. Patient-Centered Outcomes in Radiation Oncology. Hematol. Oncol. Clin. N. Am. 2019, 33, 1105–1116. [Google Scholar] [CrossRef]
- Remick, J.S.; Kowalski, E.; Samanta, S.; Choi, S.; Palmer, J.D.; Mishra, M.V. Health-Related Quality of Life and Patient-Reported Outcomes in Radiation Oncology Clinical Trials. Curr. Treat. Options Oncol. 2020, 21, 87. [Google Scholar] [CrossRef] [PubMed]
- Yang, L.Y.; Manhas, D.S.; Howard, A.F.; Olson, R.A. Patient-Reported Outcome Use in Oncology: A Systematic Review of the Impact on Patient-Clinician Communication. Support. Care Cancer 2018, 26, 41–60. [Google Scholar] [CrossRef] [PubMed]
- Teresi, J.A.; Fleishman, J.A. Differential Item Functioning and Health Assessment. Qual. Life Res. 2007, 16 (Suppl. 1), 33–42. [Google Scholar] [CrossRef] [PubMed]
- Schipper, H.; Clinch, J.J.; Olweny, C.L.M. Definitions and Conceptual Issues. In Quality of Life and Pharmacoeconomics in Clinical Trials; Lippincott-Raven Publishers: Philadelphia, PA, USA, 1996; pp. 11–23. [Google Scholar]
- Vanier, A.; Oort, F.J.; McClimans, L.; Ow, N.; Gulek, B.G.; Böhnke, J.R.; Sprangers, M.; Sébille, V.; Mayo, N.; The Response Shift—In Sync Working Group. Response Shift in Patient-Reported Outcomes: Definition, Theory, and a Revised Model. Qual. Life Res. 2021, 30, 3309–3322. [Google Scholar] [CrossRef]
- Chow, E.; Chiu, H.; Doyle, M.; Hruby, G.; Holden, L.; Barnes, E.A.; Tsao, M.; Mallia, G.; Harris, K.; Danjoux, C. Patient Expectation of the Partial Response and Response Shift in Pain Score. Support. Cancer Ther. 2007, 4, 110–118. [Google Scholar] [CrossRef]
- Pagano, I.S.; Gotay, C.C. Ethnic Differential Item Functioning in the Assessment of Quality of Life in Cancer Patients. Health Qual. Life Outcomes 2005, 3, 60. [Google Scholar] [CrossRef] [Green Version]
- Sommer, K.; Cottone, F.; Aaronson, N.K.; Fayers, P.; Fazi, P.; Rosti, G.; Angelucci, E.; Gaidano, G.; Venditti, A.; Voso, M.T.; et al. Consistency Matters: Measurement Invariance of the EORTC QLQ-C30 Questionnaire in Patients with Hematologic Malignancies. Qual. Life Res. 2020, 29, 815–823. [Google Scholar] [CrossRef]
- Sulmasy, D.P.; Astrow, A.B.; He, M.K.; Seils, D.M.; Meropol, N.J.; Micco, E.; Weinfurt, K.P. The Culture of Faith and Hope: Patients’ Justifications for Their High Estimations of Expected Therapeutic Benefit When Enrolling in Early Phase Oncology Trials. Cancer 2010, 116, 3702–3711. [Google Scholar] [CrossRef] [Green Version]
- Reuben, D.B.; Jennings, L.A. Putting Goal-Oriented Patient Care Into Practice. J. Am. Geriatr. Soc. 2019, 67, 1342–1344. [Google Scholar] [CrossRef] [Green Version]
- Miner, A.S.; Schueller, S.M.; Lattie, E.G.; Mohr, D.C. Creation and Validation of the Cognitive and Behavioral Response to Stress Scale in a Depression Trial. Psychiatry Res. 2015, 230, 819–825. [Google Scholar] [CrossRef] [Green Version]
- Pickering, T.G.; James, G.D.; Boddie, C.; Harshfield, G.A.; Blank, S.; Laragh, J.H. How Common Is White Coat Hypertension? JAMA 1988, 259, 225–228. [Google Scholar] [CrossRef] [PubMed]


| DIF/RS | Oncology Example | Types | Examples of Implications for Clinical Practice |
|---|---|---|---|
| DIF: Two patients who have the same level of health may report different PROM scores (e.g., due to cultural, environmental, personal, or experiential differences) | For items of physical and emotional functioning, scalar DIF relative to sex were observed, where males were more likely to endorse items with intensive physical activities and irritability than females [18] | Lack of scalar invariance (interpret items and response scales differently from others) | If this type of DIF is ignored, the decision to address side effects of treatment (e.g., worsening physical function, increased irritability) may be overlooked for males |
| Relative to Caucasian and Japanese groups, items related to physical, cognitive and social functioning, nausea and vomiting, and financial difficulties exhibited DIF for Filipinos. On these items, Filipinos exhibited either higher or lower quality of life (QoL) scores, even though their overall QoL was the same [17] | Lack of metric invariance (assign different meanings to items used for measuring health) | If this type of DIF is ignored, Filipino patients’ concerns about impaired quality of life may not be addressed because scores do not reflect those aspects that are most problematic when given cancer treatment | |
| Lack of configural invariance (define health differently from others) | If this type of DIF is ignored, it will be more difficult for clinicians to prioritize interventions based on how patients define aspects of their health | ||
| RS: A patient has changes in their health level, but report the same PROM scores over time | Majority of patients with bone metastases with palliative radiation therapy (73%) had reduction in pain scores, but response shift resulted in no changes in overall pain score [16] | Recalibration (change in measurement standards) | If this type of RS is ignored, the impact of treatments based on PROMs may either be over or under-estimated |
| Reprioritization (change in relative importance of items) | If this type of RS is ignored, patients may be prescribed treatment that could have adverse effects on their social function, which may be more important than being cancer-free | ||
| Reconceptualization (change in definition of construct) | If this type of RS is ignored, clinicians may attribute higher pain scores to the treatment itself, and may, therefore, no longer continue the treatment |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kwon, J.-Y.; Russell, L.; Coles, T.; Klaassen, R.J.; Schick-Makaroff, K.; Sibley, K.M.; Mitchell, S.A.; Sawatzky, R. Patient-Reported Outcomes Measurement in Radiation Oncology: Interpretation of Individual Scores and Change over Time in Clinical Practice. Curr. Oncol. 2022, 29, 3093-3103. https://doi.org/10.3390/curroncol29050251
Kwon J-Y, Russell L, Coles T, Klaassen RJ, Schick-Makaroff K, Sibley KM, Mitchell SA, Sawatzky R. Patient-Reported Outcomes Measurement in Radiation Oncology: Interpretation of Individual Scores and Change over Time in Clinical Practice. Current Oncology. 2022; 29(5):3093-3103. https://doi.org/10.3390/curroncol29050251
Chicago/Turabian StyleKwon, Jae-Yung, Lara Russell, Theresa Coles, Robert J. Klaassen, Kara Schick-Makaroff, Kathryn M. Sibley, Sandra A. Mitchell, and Richard Sawatzky. 2022. "Patient-Reported Outcomes Measurement in Radiation Oncology: Interpretation of Individual Scores and Change over Time in Clinical Practice" Current Oncology 29, no. 5: 3093-3103. https://doi.org/10.3390/curroncol29050251
APA StyleKwon, J.-Y., Russell, L., Coles, T., Klaassen, R. J., Schick-Makaroff, K., Sibley, K. M., Mitchell, S. A., & Sawatzky, R. (2022). Patient-Reported Outcomes Measurement in Radiation Oncology: Interpretation of Individual Scores and Change over Time in Clinical Practice. Current Oncology, 29(5), 3093-3103. https://doi.org/10.3390/curroncol29050251





