Evolution of the Surgical Management of Lung Cancer Invading the Spine: A Single Center Experience
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
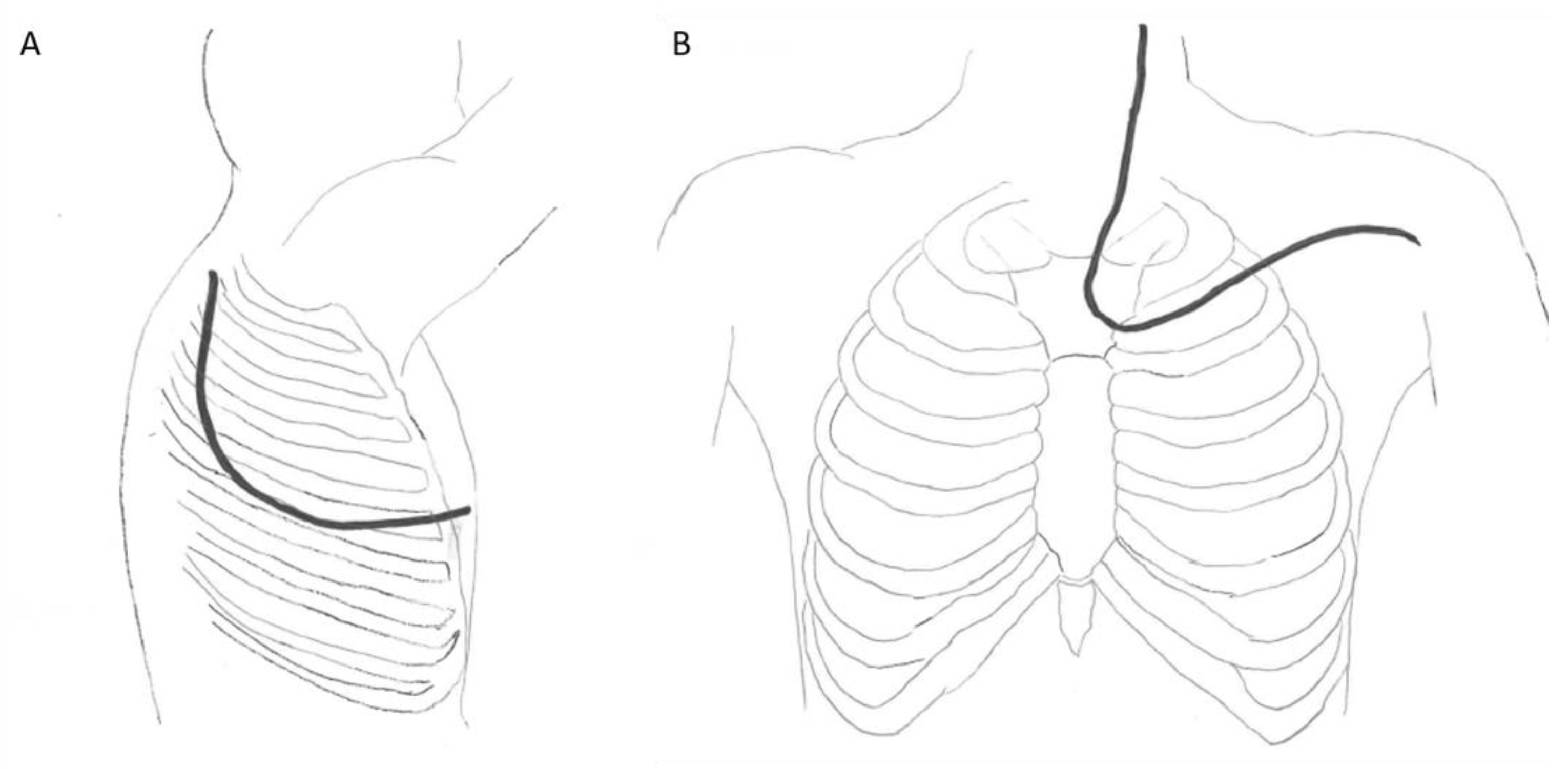
2.2. Operative Technique
2.3. Statistical Analysis
3. Results
3.1. Patient Population
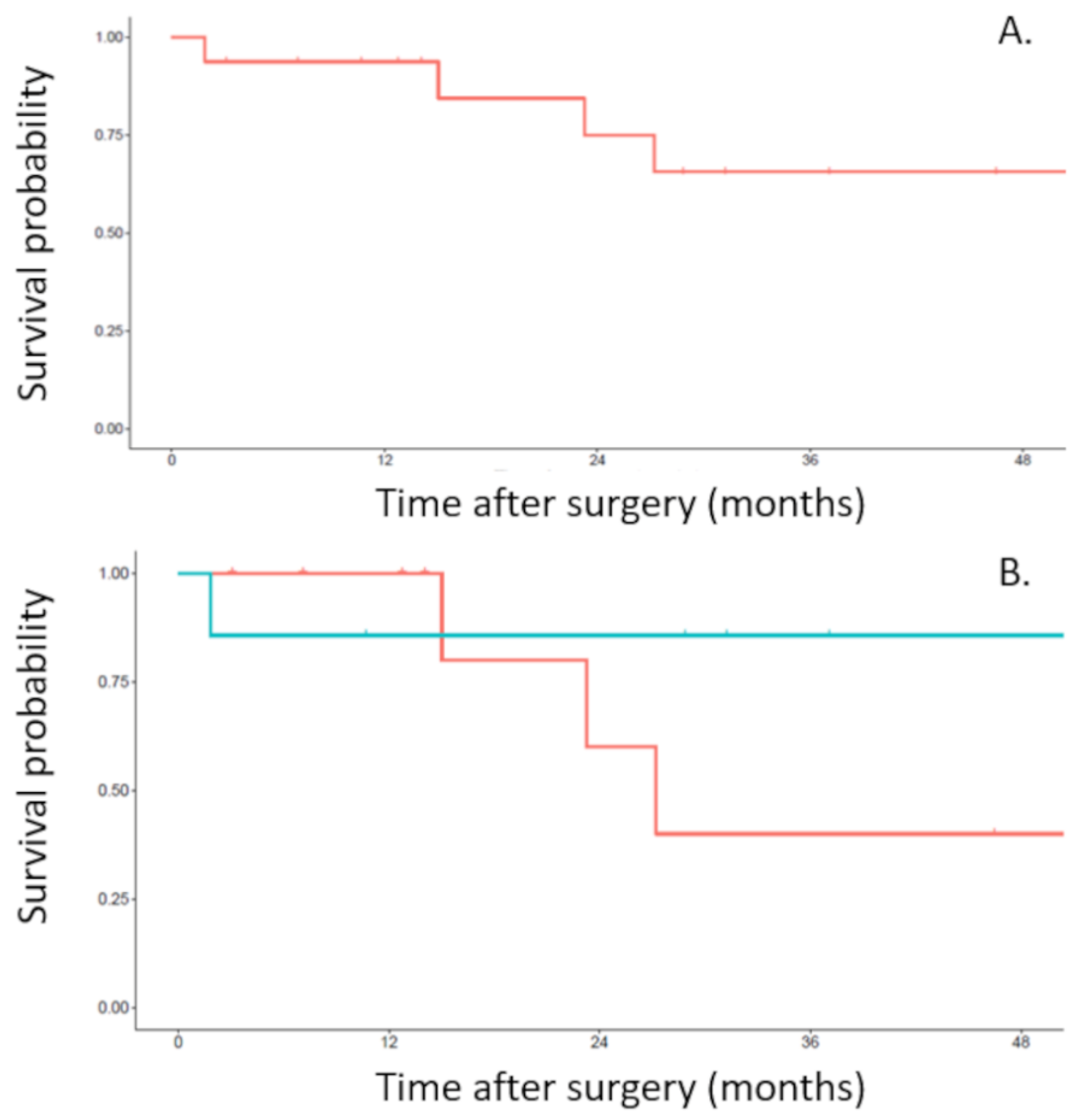
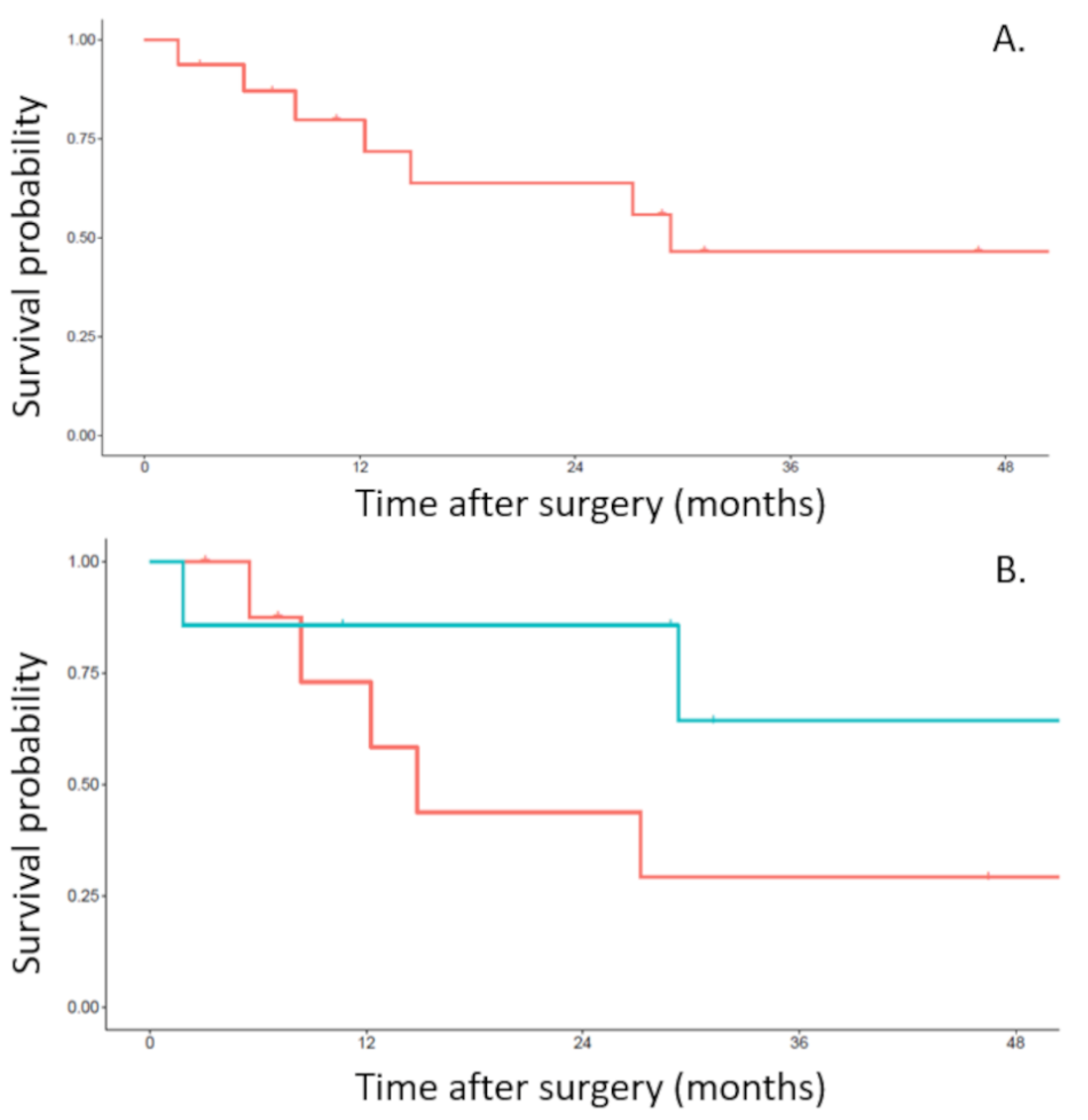
3.2. Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tandberg, D.J.; Tong, B.C.; Ackerson, B.G.; Kelsey, C.R. Surgery versus stereotactic body radiation therapy for stage I non-small cell lung cancer: A comprehensive review. Cancer 2018, 124, 667–678. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Varela, G.; Thomas, P.A. Surgical management of advanced non-small cell lung cancer. J. Thorac. Dis. 2014, 6 (Suppl. S2), S217–S223. [Google Scholar] [PubMed]
- Anraku, M.; Waddell, T.K.; de Perrot, M.; Lewis, S.J.; Pierre, A.F.; Darling, G.E.; Johnston, M.R.; Zener, R.E.; Rampersaud, Y.R.; Shepherd, F.A.; et al. Induction chemoradiotherapy facilitates radical resection of T4 non-small cell lung cancer invading the spine. J. Thorac. Cardiovasc. Surg. 2009, 137, 441–447.e1. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grunenwald, D.H.; Mazel, C.; Girard, P.; Veronesi, G.; Spaggiari, L.; Gossot, D.; Debrosse, D.; Caliandro, R.; Le Guillou, J.L.; Le Chevalier, T. Radical en bloc resection for lung cancer invading the spine. J. Thorac. Cardiovasc. Surg. 2002, 123, 271–279. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dindo, D.; Demartines, N.; Clavien, P.A. Classification of surgical complications: A new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann. Surg. 2004, 240, 205–213. [Google Scholar] [CrossRef] [PubMed]
- Chardack, W.M.; MacCallum, J.D. Pancoast tumor; five-year survival without recurrence or metastases following radical resection and postoperative irradiation. J. Thorac. Surg. 1956, 31, 535–542. [Google Scholar] [CrossRef]
- Shaw, R.R.; Paulson, D.L.; Kee, J.L. Treatment of Superior Sulcus Tumor by Irradiation Followed by Resection. Ann. Surg. 1961, 154, 29–40. [Google Scholar] [CrossRef] [PubMed]
- Rusch, V.W.; Giroux, D.J.; Kraut, M.J.; Crowley, J.; Hazuka, M.; Winton, T.; Johnson, D.H.; Shulman, L.; Shepherd, F.; Deschamps, C.; et al. Induction chemoradiation and surgical resection for superior sulcus non-small-cell lung carcinomas: Long-term results of Southwest Oncology Group Trial 9416 (Intergroup Trial 0160). J. Clin. Oncol. 2007, 25, 313–318. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Collaud, S.; Fadel, E.; Schirren, J.; Yokomise, H.; Bolukbas, S.; Dartevelle, P.; Keshavjee, S.; Waddell, T.K.; de Perrot, M. En Bloc Resection of Pulmonary Sulcus Non-small Cell Lung Cancer Invading the Spine: A Systematic Literature Review and Pooled Data Analysis. Ann. Surg. 2015, 262, 184–188. [Google Scholar] [CrossRef] [PubMed]
- Sundaresan, N.; Hilaris, B.S.; Martini, N. The combined neurosurgical-thoracic management of superior sulcus tumors. J. Clin. Oncol. 1987, 5, 1739–1745. [Google Scholar] [CrossRef] [PubMed]
- Cormier, J.M. Voie D’abord: Abord de L’artère Sous-Clavière; Patel, J., Léger, L., Eds.; Nouveau Traité de Technique Chirurgicale (Tome V), Masson et Cie: Paris, France, 1970; pp. 107–140. [Google Scholar]
- Dartevelle, P.G.; Chapelier, A.R.; Macchiarini, P.; Lenot, B.; Cerrina, J.; Ladurie, F.L.; Parquin, F.J.; Lafont, D. Anterior transcervical-thoracic approach for radical resection of lung tumors invading the thoracic inlet. J. Thorac. Cardiovasc. Surg. 1993, 105, 1025–1034. [Google Scholar] [CrossRef]
- Grunenwald, D.; Mazel, C.; Girard, P.; Berthiot, G.; Dromer, C.; Baldeyrou, P. Total vertebrectomy for en bloc resection of lung cancer invading the spine. Ann. Thorac. Surg. 1996, 61, 723–725, discussion 725–726. [Google Scholar] [CrossRef]
- Chadeyras, J.B.; Mazel, C.; Grunenwald, D. Vertebral en bloc resection for lung cancer: Twelve years’ experience. Ann. Chir. 2006, 131, 616–622. (In French) [Google Scholar] [CrossRef] [PubMed]
- Kwee, M.M.; Ho, Y.H.; Rozen, W.M. The prone position during surgery and its complications: A systematic review and evidence-based guidelines. Int. Surg. 2015, 100, 292–303. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zairi, F.; Sunna, T.; Liberman, M.; Boubez, G.; Wang, Z.; Shedid, D. Single Posterior Approach for En-Bloc Resection and Stabilization for Locally Advanced Pancoast Tumors Involving the Spine: Single Centre Experience. Asian Spine J. 2016, 10, 1047–1057. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fadel, E.; Missenard, G.; Chapelier, A.; Mussot, S.; Leroy-Ladurie, F.; Cerrina, J.; Dartevelle, P. En bloc resection of non-small cell lung cancer invading the thoracic inlet and intervertebral foramina. J. Thorac. Cardiovasc. Surg. 2002, 123, 676–685. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gandhi, S.; Walsh, G.L.; Komaki, R.; Gokaslan, Z.L.; Nesbitt, J.C.; Putnam, J.B., Jr.; Roth, J.A.; Merriman, K.W.; McCutcheon, I.E.; Munden, R.F.; et al. A multidisciplinary surgical approach to superior sulcus tumors with vertebral invasion. Ann. Thorac. Surg. 1999, 68, 1778–1784, discussion 1784–1785. [Google Scholar] [CrossRef]
- Koizumi, K.; Haraguchi, S.; Hirata, T.; Hirai, K.; Mikami, I.; Yamagishi, S.; Okada, D.; Kinoshita, H.; Enomoto, Y.; Nakajima, Y.; et al. Surgical treatment of lung cancer with vertebral invasion. Ann. Thorac. Cardiovasc. Surg. 2004, 10, 229–234. [Google Scholar] [PubMed]
- Schirren, J.; Dönges, T.; Melzer, M.; Schönmayr, R.; Eberlein, M.; Bölükbas, S. En bloc resection of non-small-cell lung cancer invading the spine. Eur. J. Cardiothorac. Surg. 2011, 40, 647–654. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Albain, K.S.; Crowley, J.J.; Turrisi, A.T., 3rd; Gandara, D.R.; Farrar, W.B.; Clark, J.I.; Beasley, K.R.; Livingston, R.B. Concurrent cisplatin, etoposide, and chest radiotherapy in pathologic stage IIIB non-small-cell lung cancer: A Southwest Oncology Group phase II study, SWOG 9019. J. Clin. Oncol. 2002, 20, 3454–3460. [Google Scholar] [CrossRef] [PubMed]
| n = 16 (%) | ||
|---|---|---|
| Gender | ||
| male | 13 (81%) | |
| female | 3 (19%) | |
| Medical history | ||
| smoking | 16 (100%) | |
| stopped smoking | 11 (58%) | |
| Anatomopathology | ||
| Adenocarcinoma | 8 (50%) | |
| Squamous cell carcinoma | 6 (37%) | |
| Poorly differentiated carcinoma | 2 (13%) | |
| Neo adjuvant radiotherapy | ||
| Chemotherapy | ||
| up to 3 cycles | 5 (31%) | |
| 3 to 6 cycles | 11 (69%) | |
| Radiotherapy | ||
| 45 grays | 12 (75%) | |
| 66 grays | 3 (19%) | |
| Resection | ||
| One-step | 9 (56%) | |
| Two-step | 7 (44%) | |
| pN status | ||
| N0 | 14 (87%) | |
| N1 | 0 | |
| N2 | 2 (13%) | |
| Completeness of resection | ||
| R0 | 16 (100%) | |
| R1 | 0 | |
| R2 | 0 | |
| One-Step n = 9 (%) | Two-Step n = 7 (%) | |
|---|---|---|
| Number of rib(s) resected | ||
| 2 | 2 (22.2%) | 1 (14.3%) |
| 3 | 1 (11.1%) | 4 (57.1%) |
| 4 | 4 (44.5%) | 2 (28.6%) |
| 5 | 2 (22.2%) | 0 |
| Number of vertebra(e) resected | ||
| 1 | 1 (11.1%) | 0 |
| 2 | 1 (11.1%) | 3 (42.9%) |
| 3 | 7 (77.8%) | 4 (57.1%) |
| Per operative complications | ||
| Hemorrhage | 3 (33.3%) | 0 |
| Cardiac arrest | 1 (11.1%) | 0 |
| Post-operative complications | ||
| Prolonged drainage | 7 (77.8%) | 4 (57.1%) |
| Pneumonia | 9 (100%) | 5 (71.4%) |
| Atrial fibrillation | 2 (22.2%) | 3 (42.9%) |
| Renal insufficiency | 0 | 2 (28.6%) |
| Upper limb paresis | 4 (44.5%) | 3 (42.9%) |
| Cerebrospinal fluid leak | 2 (22.2%) | 0 |
| Neuropathic pain | 3 (33.3%) | 4 (57.1%) |
| In hospital death | 0 | 1 (14.3%) |
| One-Step n = 9 | Two-Step n = 7 | |
|---|---|---|
| Major post-operative complications | ||
| Atelectasis requiring flexible bronchoscopy | 1 (11.1%) | 3 (42.9%) |
| Respiratory insufficiency requiring tracheotomy | 1 (11.1%) | 0 |
| Surgical revision due to post-operative empyema | 1 (11.1%) | 1 (14.3%) |
| Surgical revision due to wound infection | 2 (22.2%) | 1 (14.3%) |
| Osteosynthesis material infection | 0 | 1 (14.3%) |
| Cerebrospinal fluid leak | 1 (11.1%) | 0 |
| Clavien classification | ||
| Grade I | 1 (11.1%) | 1 (14.3%) |
| Grade II | 4 (44.5%) | 1 (14.3%) |
| Grade IIIa | 1 (11.1%) | 2 (28.6%) |
| Grade IIIb | 2 (22.2%) | 2 (28.6%) |
| Grade IVa | 1 (11.1%) | 0 |
| Grade IVb | 0 | 0 |
| Grade V | 0 | 1 (14.3%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Drevet, G.; Broussolle, T.; Belaroussi, Y.; Duponchelle, L.; Maury, J.M.; Grima, R.; Vaz, G.; Silvestre, C.; Tronc, F. Evolution of the Surgical Management of Lung Cancer Invading the Spine: A Single Center Experience. Curr. Oncol. 2022, 29, 3061-3071. https://doi.org/10.3390/curroncol29050248
Drevet G, Broussolle T, Belaroussi Y, Duponchelle L, Maury JM, Grima R, Vaz G, Silvestre C, Tronc F. Evolution of the Surgical Management of Lung Cancer Invading the Spine: A Single Center Experience. Current Oncology. 2022; 29(5):3061-3071. https://doi.org/10.3390/curroncol29050248
Chicago/Turabian StyleDrevet, Gabrielle, Théo Broussolle, Yanis Belaroussi, Lucie Duponchelle, Jean Michel Maury, Renaud Grima, Gualter Vaz, Clément Silvestre, and François Tronc. 2022. "Evolution of the Surgical Management of Lung Cancer Invading the Spine: A Single Center Experience" Current Oncology 29, no. 5: 3061-3071. https://doi.org/10.3390/curroncol29050248
APA StyleDrevet, G., Broussolle, T., Belaroussi, Y., Duponchelle, L., Maury, J. M., Grima, R., Vaz, G., Silvestre, C., & Tronc, F. (2022). Evolution of the Surgical Management of Lung Cancer Invading the Spine: A Single Center Experience. Current Oncology, 29(5), 3061-3071. https://doi.org/10.3390/curroncol29050248





