Risk of Anxiety and Depression after Diagnosis of Young-Onset Colorectal Cancer: A Population-Based Cohort Study
Abstract
:1. Introduction
2. Materials and Methods
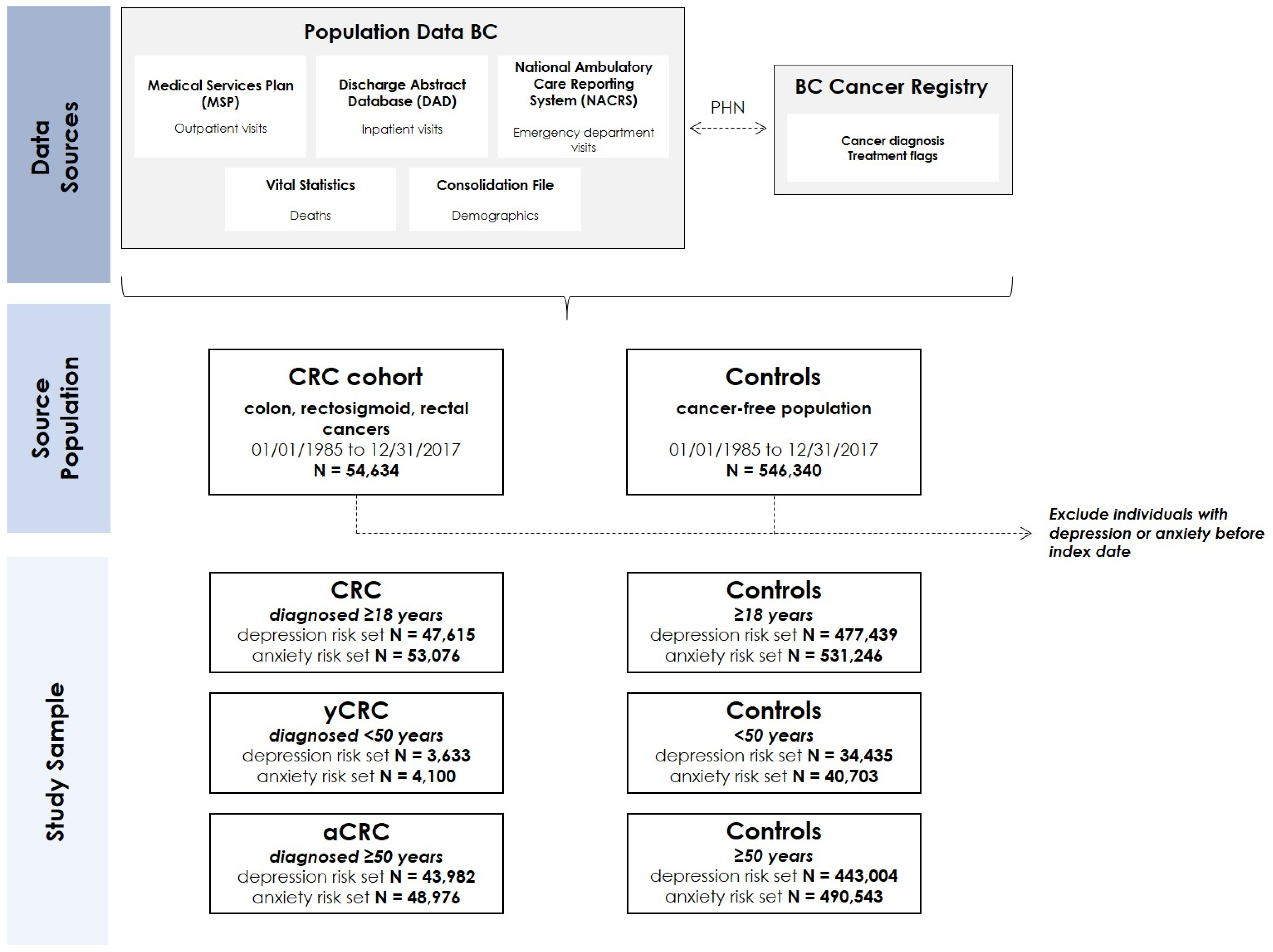
2.1. Data Source and Study Population
2.2. Outcome Ascertainment
2.3. Covariate Ascertainment
2.4. Statistical Analysis
2.5. Study Conduct
3. Results
3.1. Risk of Depression and Anxiety for yCRC in Comparison to aCRC
3.2. Risk of Depression and Anxiety for CRC, yCRC and aCRC in Comparison to Controls
3.3. Depression and Anxiety According to Phases of CRC Care
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Canadian Cancer Society. Canadian Cancer Statistics. 2019. Available online: https://www.cancer.ca/~/media/cancer.ca/CW/cancer%20information/cancer%20101/Canadian%20cancer%20statistics/Canadian-Cancer-Statistics-2019-EN.pdf?la=en (accessed on 15 October 2021).
- Canadian Cancer Society. Cancer Statistics at a Glance. 2021. Available online: https://cancer.ca/en/research/cancer-statistics/cancer-statistics-at-a-glance (accessed on 15 October 2021).
- Brenner, D.R.; Heer, E.; Sutherland, R.L.; Ruan, Y.; Tinmouth, J.; Heitman, S.J.; Hilsden, R.J. National Trends in Colorectal Cancer Incidence among Older and Younger Adults in Canada. JAMA Netw. Open. 2019, 2, e198090. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mosher, C.E.; Winger, J.G.; Given, B.A.; Helft, P.R.; O’Neil, B.H. Mental health outcomes during colorectal cancer survivorship: A review of the literature. Psycho-Oncol. 2016, 25, 1261–1270. [Google Scholar] [CrossRef] [PubMed]
- Sun, L.M.; Liang, J.A.; Lin, C.L.; Sun, S.; Kao, C.H. Risk of mood disorders in patients with colorectal cancer. J. Affect. Disord. 2017, 218, 59–65. [Google Scholar] [CrossRef] [PubMed]
- Lloyd, S.; Baraghoshi, D.; Tao, R.; Garrido-Laguna, I.; Gilcrease, G.W., 3rd; Whisenant, J.; Weis, J.R.; Scaife, C.; Pickron, T.B.; Huang, L.C.; et al. Mental Health Disorders are More Common in Colorectal Cancer Survivors and Associated with Decreased Overall Survival. Am. J. Clin. Oncol. 2019, 42, 355–362. [Google Scholar] [CrossRef] [PubMed]
- Weissman, S.; Ghoneim, S.; Sanayei, A.; Said, H.; Rosenblatt, S.; Mohammed, A.; Jafri, S.; Atoot, A.; Feuerstein, J.D. New-onset depression after colorectal cancer diagnosis: A population-based longitudinal study. Intl. J. Colorectal Dis. 2021, 36, 2599–2602. [Google Scholar] [CrossRef]
- Kim, S.E.; Paik, H.Y.; Yoon, H.; Lee, J.E.; Kim, N.; Sung, M.K. Sex- and gender-specific disparities in colorectal cancer risk. World J. Gastroenterol. 2015, 21, 5167–5175. [Google Scholar] [CrossRef]
- Afifi, M. Gender differences in mental health. Singap. Med. J. 2007, 48, 385–391. [Google Scholar]
- Holdcroft, A. Gender bias in research: How does it affect evidence based medicine? J. R. Soc. Med. 2007, 100, 2–3. [Google Scholar] [CrossRef]
- Heidari, S.; Babor, T.F.; De Castro, P.; Tort, S.; Curno, M. Sex and Gender Equity in Research: Rationale for the SAGER guidelines and recommended use. Res. Integr. Peer Rev. 2016, 1, 2. [Google Scholar] [CrossRef] [Green Version]
- Government of British Columbia. Population Estimates 2020. Available online: https://www2.gov.bc.ca/gov/content/data/statistics/people-population-community/population/population-estimates (accessed on 15 October 2021).
- BC Ministry of Health (2019): National Ambulatory Care Reporting System (NACRS). Population Data BC. Data Extract. MOH. 2019. Available online: http://www.popdata.bc.ca/data (accessed on 15 October 2021).
- BC Cancer Registry Data (2019). BC Cancer. Data Extract. BC Cancer. 2019.
- BC Ministry of Health (2019): PharmaNet. BC Ministry of Health. Data Extract. Data Stewardship Committee. 2019. Available online: http://www.popdata.bc.ca/data (accessed on 15 October 2021).
- BC Ministry of Health (2019): Consolidation File (MSP Registration and Premium Billing). V2. Population Data BC. Data Extract. MOH. 2019. Available online: http://popdata.bc.ca/data (accessed on 15 October 2021).
- BC Vital Statistics Agency (2019): Vital Statistics Deaths. Population Data BC. Data Extract BC Vital Statistics Agency. 2019. Available online: http://www.popdata.bc.ca/data (accessed on 15 October 2021).
- British Columbia Ministry of Health (2018): Medical Services Plan (MSP) Payment Information File. Population Data BC. Data Extract. MOH. 2019. Available online: http://www.popdata.bc.ca/data (accessed on 15 October 2021).
- Canadian Institute for Health Information (2019): Discharge Abstract Database (Hospital Separations). Population Data BC. Data Extract. MOH. 2019. Available online: http://www.popdata.bc.ca/data (accessed on 15 October 2021).
- Doktorchik, C.; Patten, S.; Eastwood, C.; Peng, M.; Chen, G.; Beck, C.A.; Jetté, N.; Williamson, T.; Quan, H. Validation of a case definition for depression in administrative data against primary chart data as a reference standard. BMC Psychiatry 2019, 19, 9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marrie, R.A.; Fisk, J.D.; Yu, B.N.; Leung, S.; Elliott, L.; Caetano, P.; Warren, S.; Evans, C.; Wolfson, C.; Svenson, L.W.; et al. Mental comorbidity and multiple sclerosis: Validating administrative data to support population-based surveillance. BMC Neurol. 2013, 13, 16. [Google Scholar] [CrossRef] [Green Version]
- Marrie, R.A.; Walker, J.R.; Graff, L.A.; Lix, L.M.; Bolton, J.M.; Nugent, Z.; Targownik, L.E.; Bernstein, C.N. Performance of administrative case definitions for depression and anxiety in inflammatory bowel disease. J. Psychosom. Res. 2016, 89, 107–113. [Google Scholar] [CrossRef]
- Romano, P.S.; Roos, L.L.; Jollis, J.G. Adapting a clinical comorbidity index for use with ICD-9-CM administrative data: Differing perspectives. J. Clin. Epidemiol. 1993, 46, 1075–1079, discussion 1081–1090. [Google Scholar] [CrossRef]
- American Joint Committee on Cancer. AJCC Cancer Staging Manual, 8th ed.; Springer International Publishing: Berlin/Heidelberg, Germany, 2017. [Google Scholar]
- BC Cancer. Cancer Management Guidelines: Gastrointestinal (Colon). 2012. Available online: http://www.bccancer.bc.ca/health-professionals/clinical-resources/cancer-management-guidelines/gastrointestinal/colon (accessed on 29 October 2021).
- Mariotto, A.B.; Warren, J.L.; Zeruto, C.; Coughlan, D.; Barrett, M.J.; Zhao, L.; Yabroff, K.R. Cancer-Attributable Medical Costs for Colorectal Cancer Patients by Phases of Care: What Is the Effect of a Prior Cancer History? J. Natl. Cancer Inst. Monogr. 2020, 2020, 22–30. [Google Scholar] [CrossRef] [PubMed]
- Sharma, S.K. Importance of case definition in epidemiological studies. Neuroepidemiology 2011, 37, 141–142. [Google Scholar] [CrossRef] [PubMed]
- Akhtar-Danesh, N.; Landeen, J. Relation between depression and sociodemographic factors. Int. J. Ment. Health Sys. 2007, 1, 4. [Google Scholar] [CrossRef] [Green Version]
- Gask, L.; Coventry, P. Person-centred mental health care: The challenge of implementation. Epidemiol. Psychiatr. Sci. 2012, 21, 139–144. [Google Scholar] [CrossRef] [Green Version]
- Patten, S.B.; Williams, J.V.; Lavorato, D.H.; Wang, J.L.; McDonald, K.; Bulloch, A.G. Descriptive epidemiology of major depressive disorder in Canada in 2012. Can. J. Psychiatry 2015, 60, 23–30. [Google Scholar] [CrossRef] [Green Version]
- Wang, J.; Williams, J.; Lavorato, D.; Schmitz, N.; Dewa, C.; Patten, S.B. The incidence of major depression in Canada: The National Population Health Survey. J. Affect. Disord. 2010, 123, 158–163. [Google Scholar] [CrossRef]
- Cavanagh, A.; Wilson, C.J.; Kavanagh, D.J.; Caputi, P. Differences in the Expression of Symptoms in Men Versus Women with Depression: A Systematic Review and Meta-analysis. Harv. Rev. Psychiatry 2017, 25, 29–38. [Google Scholar] [CrossRef] [PubMed]
- Oliffe, J.L.; Rossnagel, E.; Seidler, Z.E.; Kealy, D.; Ogrodniczuk, J.S.; Rice, S.M. Men’s Depression and Suicide. Curr. Psychiatry Rep. 2019, 21, 103. [Google Scholar] [CrossRef] [PubMed]
- Seidler, Z.E.; Dawes, A.J.; Rice, S.M.; Oliffe, J.L.; Dhillon, H.M. The role of masculinity in men’s help-seeking for depression: A systematic review. Clin. Psychol. Rev. 2016, 49, 106–118. [Google Scholar] [CrossRef] [PubMed]
- Hung, M.S.; Chen, I.C.; Lee, C.P.; Huang, R.J.; Chen, P.C.; Tsai, Y.H.; Yang, Y. Incidence and risk factors of depression after diagnosis of lung cancer: A nationwide population-based study. Med. Baltim. 2017, 96, e6864. [Google Scholar] [CrossRef] [PubMed]
| Characteristic | CRC (n = 54,634) | Controls (n = 546,340) | yCRC (n = 4223) | Controls (n = 42,230) | aCRC (n = 50,411) | Controls (n = 504,110) |
|---|---|---|---|---|---|---|
| Age, mean (SD) | 67.9 (11.9) | 67.9 (11.9) | 43.2 (6.0) | 43.1 (6.0) | 70.0 (9.8) | 70.0 (9.8) |
| Female, n (%) | 25,402 (46.5) | 254,020 (46.5) | 2091 (49.5) | 20,910 (49.5) | 23,311 (46.2) | 233,110 (46.2) |
| Charlson–Romano comorbidity index, mean (SD) | 0.91 (2.12) | 0.14 (0.60) | 0.81 (2.06) | 0.04 (0.35) | 0.92 (2.13) | 0.14 (0.62) |
| Neighbourhood income quintile, n (%) | ||||||
| Quintile 1 | 11,301 (20.7) | 116,633 (21.4) | 774 (18.3) | 8723 (20.7) | 10,527 (20.9) | 107,910 (21.4) |
| Quintile 2 | 10,325 (18.9) | 108,446 (19.9) | 794 (18.8) | 8521 (20.2) | 9531 (18.9) | 99,925 (19.8) |
| Quintile 3 | 13,166 (24.1) | 118,427 (21.7) | 1024 (24.3) | 8645 (20.5) | 12,142 (24.1) | 109,782 (21.8) |
| Quintile 4 | 9850 (18.0) | 100,190 (18.3) | 828 (19.6) | 8410 (19.9) | 9022 (17.9) | 91,780 (18.2) |
| Quintile 5 | 9992 (18.3) | 102,644 (18.8) | 803 (19.0) | 7931 (18.8) | 9189 (18.2) | 94,713 (18.8) |
| Residence, n (%) | ||||||
| Urban | 46,510 (85.1) | 468,596 (85.8) | 3691 (87.4) | 37,276 (88.3) | 42,819 (84.9) | 431,320 (85.6) |
| Rural | 8124 (14.9) | 77,744 (14.2) | 532 (12.6) | 4954 (11.7) | 7592 (15.1) | 72,790 (14.4) |
| Health care use, mean (SD) | ||||||
| Number of outpatient visits | 14.1 (12.6) | 10.0 (11.4) | 10.2 (9.8) | 9.3 (12.5) | 14.4 (12.7) | 10.1 (11.3) |
| Number of inpatient visits | 0.8 (1.1) | 0.3 (0.8) | 0.7 (1.0) | 0.2 (0.7) | 0.9 (1.1) | 0.3 (0.8) |
| Depression HR (95% CI) | Anxiety HR (95% CI) | |
|---|---|---|
| 1: Unadjusted model | ||
| yCRC (vs. aCRC) | 1.15 (1.05, 1.25) | 1.30 (1.12, 1.50) |
| 2: Multivariable model a,b | ||
| yCRC (vs. aCRC) | 1.41 (1.25, 1.60) | 1.05 (0.86, 1.28) |
| 3: Unadjusted models stratified by sex c | ||
| Males, yCRC (vs. aCRC) | 1.26 (1.11, 1.43) | 1.34 (1.06, 1.70) |
| Females, yCRC (vs. aCRC) | 1.03 (0.91, 1.17) | 1.23 (1.02, 1.49) |
| 4: Multivariable models stratified by sex c | ||
| Males, yCRC (vs. aCRC) | 1.76 (1.48, 2.10) | 1.00 (0.72, 1.38) |
| Females, yCRC (vs. aCRC) | 1.17 (0.99, 1.38) | 1.07 (0.83, 1.38) |
| Depression HR (95% CI) | Anxiety HR (95% CI) | |
|---|---|---|
| 1: Unadjusted model | ||
| yCRC (vs. aCRC) | 1.15 (1.05, 1.25) | 1.30 (1.12, 1.50) |
| 2: Multivariable model a,b | ||
| yCRC (vs. aCRC) | 1.56 (1.13, 2.14) | 1.17 (0.79, 1.75) |
| 3: Unadjusted models stratified by sex c | ||
| Males, yCRC (vs. aCRC) | 1.26 (1.11, 1.43) | 1.34 (1.06, 1.70) |
| Females, yCRC (vs. aCRC) | 1.03 (0.91, 1.17) | 1.23 (1.01, 1.49) |
| 4: Multivariable models stratified by sex c | ||
| Males, yCRC (vs. aCRC) | 1.60 (1.02, 2.52) | 0.93 (0.47, 1.83) |
| Females, yCRC (vs. aCRC) | 1.49 (0.93, 2.37) | 1.34 (0.81, 2.22) |
| CRC HR (95% CI) | yCRC HR (95% CI) | aCRC HR (95% CI) | ||||
|---|---|---|---|---|---|---|
| 1: Depression | Unadjusted | Adjusted | Unadjusted | Adjusted | Unadjusted | Adjusted |
| All a,b | 1.12 (1.09, 1.15) | 1.03 (1.00, 1.06) | 1.02 (0.94, 1.12) | 1.00 (0.92, 1.10) | 1.13 (1.10, 1.17) | 1.03 (1.00, 1.07) |
| Females c | 1.04 (1.00, 1.08) | 0.97 (0.93, 1.01) | 0.88 (0.78, 1.00) | 0.88 (0.78, 1.00) | 1.06 (1.01, 1.10) | 0.98 (0.94, 1.03) |
| Males c | 1.22 (1.17, 1.27) | 1.11 (1.06, 1.16) | 1.22 (1.07, 1.38) | 1.17 (1.03, 1.33) | 1.22 (1.17, 1.27) | 1.10 (1.05, 1.15) |
| 2: Anxiety | ||||||
| All a,b | 1.19 (1.13, 1.25) | 1.11 (1.06, 1.17) | 1.08 (0.94, 1.25) | 1.10 (0.95, 1.27) | 1.20 (1.14, 1.27) | 1.11 (1.05, 1.18) |
| Females c | 1.15 (1.08, 1.23) | 1.09 (1.02, 1.16) | 1.08 (0.90, 1.29) | 1.10 (0.91, 1.33) | 1.17 (1.09, 1.25) | 1.09 (1.02, 1.17) |
| Males c | 1.23 (1.14, 1.33) | 1.15 (1.06, 1.25) | 1.10 (0.88, 1.38) | 1.10 (0.88, 1.39) | 1.25 (1.15, 1.36) | 1.16 (1.06, 1.26) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Howren, A.; Sayre, E.C.; Cheng, V.; Oveisi, N.; McTaggart-Cowan, H.; Peacock, S.; De Vera, M.A. Risk of Anxiety and Depression after Diagnosis of Young-Onset Colorectal Cancer: A Population-Based Cohort Study. Curr. Oncol. 2022, 29, 3072-3081. https://doi.org/10.3390/curroncol29050249
Howren A, Sayre EC, Cheng V, Oveisi N, McTaggart-Cowan H, Peacock S, De Vera MA. Risk of Anxiety and Depression after Diagnosis of Young-Onset Colorectal Cancer: A Population-Based Cohort Study. Current Oncology. 2022; 29(5):3072-3081. https://doi.org/10.3390/curroncol29050249
Chicago/Turabian StyleHowren, Alyssa, Eric C. Sayre, Vicki Cheng, Niki Oveisi, Helen McTaggart-Cowan, Stuart Peacock, and Mary A. De Vera. 2022. "Risk of Anxiety and Depression after Diagnosis of Young-Onset Colorectal Cancer: A Population-Based Cohort Study" Current Oncology 29, no. 5: 3072-3081. https://doi.org/10.3390/curroncol29050249
APA StyleHowren, A., Sayre, E. C., Cheng, V., Oveisi, N., McTaggart-Cowan, H., Peacock, S., & De Vera, M. A. (2022). Risk of Anxiety and Depression after Diagnosis of Young-Onset Colorectal Cancer: A Population-Based Cohort Study. Current Oncology, 29(5), 3072-3081. https://doi.org/10.3390/curroncol29050249






