Abstract
Leiomyomas are a common type of benign soft tissue tumor arising from smooth muscle, most often occurring within females’ genitourinary and gastrointestinal tract. However, primary leiomyomas of the chest wall residing in the extra-pleural space are an extremely rare subset of leiomyomatous lesion presentation. We present a case of a fifty-two-year-old male who initially presented complaining of dyspnea worsening with exertion. Computed tomography imaging was performed showing an extra-pleural mass residing under the left sixth rib. Subsequent core needle biopsy and immunohistochemical staining were performed, and the definitive diagnosis of primary leiomyoma of the posterior mediastinal chest wall. Although extremely rare, this neoplastic condition should be included in your differential diagnosis when diagnostic imaging reveals a benign mass residing in the extra-pleural space, and subsequent biopsy specimens consist of smooth muscle fibers.
1. Background
Primary neoplasms arising in the pleural and extra-pleural space are an abnormal finding since 75% of tumors found in this area can be attributed to metastases from around the body, with the remaining 25% being attributed to malignant pleural mesothelioma and solitary fibrous tumors [1,2]. Therefore, extra-pleural leiomyoma are seldom reported in medical literature. The condition is characterized by the growth of neoplastic smooth muscle tissue within the extra-pleural space [1,3]. Here, we present a case of primary leiomyoma of the chest wall arising in a 52-year-old male to expand the medical literature about this rare condition. In addition, a literature review of previously published cases about this disease state is performed.
To our knowledge, this is the most comprehensive and up-to-date review of primary pleural leiomyoma cases.
2. Case Report
In June 2015, a fifty-two-year-old male presented to the clinic with a chief complaint of several episodes of dyspnea on exertion. His past medical history was notable for mental retardation, schizophrenia, hepatitis C and chronic obstructive pulmonary disease (COPD). He also has a history of tobacco abuse and currently resides in a nursing home facility. A chest radiograph was performed showing scattered granulomas with kyphosis and compression deformities of the thoracic spine. A year later, and with no resolution of symptoms, a non-contrast CT scan of the chest was scheduled. The patient exhibited a unilateral extra-pleural mass residing over the posterior portion of the left 6th rib, measuring 4.9 × 3.9 × 2.5 cm along its maximum anteroposterior, transverse, and craniocaudal dimensions, respectively. In addition, subtle erosive changes were noted in the adjacent costovertebral junction (Figure 1). A CT-guided needle core biopsy of the left, extra-pleural mass was obtained. Histological analysis showed intersecting fascicles of bland spindle cells with abundant eosinophilic cytoplasm. No high-grade morphologic features such as brisk mitosis, overt atypia, or necrosis were noted. Immunohistochemical staining showed the lesion was strongly positive for smooth muscle markers (SMA) and desmin and was negative for keratin, CD34, and human melanoma black 45 (HMB45) (Figure 2). The final diagnosis of primary leiomyoma of the lung was made. The mass was removed by a minimally-invasive procedure. After the removal of the mass, the patient’s symptoms improved clinically. The patient’s case was discussed at the multidisciplinary thoracic tumor board. Close clinical and radiologic follow-up was recommended. Upon returning for a 6-month follow-up, his symptoms had resolved completely, and he has continued to remain in good health.
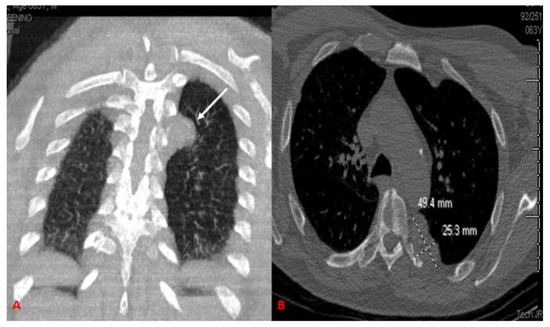
Figure 1.
Non-contrast CT scan of the chest. Coronal (A) images show a well-circumscribed lobulated, homogeneous extrapleural mass (arrow) adjacent to the left 6th rib posteriorly. Bone window (B) shows subtle erosive changes at the left costovertebral junction adjacent to the mass. The homogeneous mass completely surround costovertebral junction.
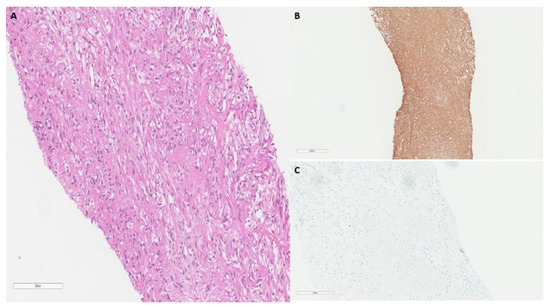
Figure 2.
(A) H&E Pathological findings from CT guided needle biopsy show fascicular smooth muscle bundles separated by vascularized connective tissue, small round nuclei with abundant eosinophilic cytoplasm (20×). (B) SMA stain: strong cytoplasmic staining. (C) Keratin stain: negative keratin staining.
3. Literature Analysis
Primary extra-pleural leiomyoma of the lung is an extraordinarily rare event, with only 14 cases being reported in medical literature to date. Therefore, a comprehensive literature analysis was conducted on PubMed with the keywords “pleural primary leiomyoma” as search criteria. Twelve manuscripts, reporting on fourteen patients, were discovered and determined eligible for analysis. The patient reported on in this manuscript was included as well (Table 1).

Table 1.
Clinical features of reported extra-pleural leiomyoma cases.
4. Discussion
Leiomyomas are benign smooth muscle tumors that were first discovered and characterized in 1854 [3]. Most cases occur in women of childbearing age, with leiomyomas representing the most common neoplasms of the uterus, affecting 20–30% of women between the ages of 30 and 50 years [14,15,16]. However, although uncommon, these smooth muscle neoplasms have been found to occur in other organs such as the small intestines, esophagus, and lung parenchyma [3,4]. Moreover, leiomyomas arising within the pleura and extra-pleural space of the lungs are an extremely rare event, with only 14 reported cases noted in medical literature to date (Table 1). Our literature analysis found the average age of diagnosis was around 41 years old, which is fairly similar to the mean age of 35 for diagnosis of uterine leiomyoma. Of the 15 reported cases, 33% were reported to occur in males while the remaining 66% were reported in female patients.
The majority of individuals with leiomyoma are asymptomatic for many years and only diagnosed incidentally upon physical exam or during imaging for other non-related problems [17,18]. Of the 15 cases used in our review, data about the initial presenting symptoms were found in 14 patients. Of those, 7 of 14 were found to be asymptomatic at diagnosis. The remaining 7 cases all had respiratory complaints, with chest pain and cough being the most common.
Pleural leiomyoma is a benign smooth muscle tumor with low malignant potential. It has the potential for local invasion into surrounding structures. The increased size of the tumor with the involvement of mediastinum makes it difficult to complete resection. It has been reported that pleural leiomyoma can disseminate through the needle tract of FNA biopsy. Thus, an FNA biopsy should be avoided if the tumor can be completely resected [5].
The diagnosis is mainly based on diagnostic imagining and histologic analysis. Typical radiographic findings on CT scans include a well-encapsulated, solitary lesion ranging from a few millimeters to several centimeters, with minimal invasion of adjacent structures [5]. Of the patients included in the review, 12 presented with a solitary lesion diagnosed via CT, while 2 cases had multiple masses at initial diagnosis. However, a definitive diagnosis of primary extra-pleural leiomyoma is difficult and can only be confirmed in conjugation with histological and immunohistochemical analysis [19]. Typical histologic features show negative signs of malignancy including, the absence of elevated mitotic count, low cellularity, lack of cytologic atypia with pleomorphism, and prominent fibrosis, with these features being confirmed through the use of H&E staining [5]. In addition, the neoplastic cells must be of smooth muscle origin and thus should stain positive for smooth muscle actin and desmin [4,5]. The absence of malignant histologic features noted upon H&E staining, combined with positive staining for SMA and desmin provides unambiguous evidence for the diagnosis of leiomyoma.
The role of PET/CT in precision medicine is an essential part of determining the staging of disease, recurrence, residual disease, and evaluating the response of patients to therapy. Combining PET with CT provides high sensitivity with PET camera for tracer distribution while CT provides anatomic localization with precision, thus making PET/CT a sensitive and a more accurate modality for evaluating malignancies [20].
No definitive treatment guidelines have been established for this condition; however, the general practice of complete surgical resection is preferred due to the well-defined and minimally invasive nature of the tumor. Thirteen of the fifteen patients elected this route of treatment (Table 1). Although in general, leiomyomas have low malignant potential, surgery is justified in these specific cases due to the chance of future tumor growth, leading to compression and invasion to adjacent structures and ultimately to serious symptoms. Overall, the prognosis for extra-pleural leiomyoma is excellent as evidenced by the 0% recurrence rate seen in Table 1 with as much as 5 years post-surgical intervention.
5. Conclusions
Primary extra-pleural leiomyoma is an extremely rare neoplastic proliferation of smooth muscle origin arising in the extrapleural cavity of the lungs. Diagnostic imaging and pathological analysis are essential for distinguishing from other pleural cancers such as mesothelioma and solitary fibrous tumors, as well as other leiomyomatous lesions of the lung. Overall, the condition has an excellent prognosis with the vast majority of patients electing for complete surgical resection with little evidence to suggest future recurrence. In conclusion, primary extra-pleural leiomyoma should be included in your differential diagnosis when an extra-pleural mass is found on diagnostic imaging, and subsequent histological analysis reveals a specimen absent of malignant features and exhibiting smooth muscle fibers.
Author Contributions
Conceptualization, A.U., G.T.P., N.A.K. and N.G.P.; methodology, A.U.; software, I.G.; validation, N.G.P. and I.A.E.; formal analysis, G.T.P.; investigation, A.U.; resources, I.G.; data curation, A.U.; writing—original draft preparation, A.U. and G.T.P.; writing—review and editing, N.A.K., I.A.E., N.G.P.; visualization, I.A.E.; supervision, N.A.K. and N.G.P.; project administration, A.U.; funding acquisition, No funding. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Informed consent was obtained from the patient involved in the study.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing does not apply to this article.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Rodríguez, P.M.; Freixinet, J.L.; Plaza, M.L.; Camacho, R. Unusual primary pleural leiomyoma. Interact. Cardiovasc. Thorac. Surg. 2010, 10, 441–442. [Google Scholar] [CrossRef] [PubMed]
- Karpathiou, G.; Stefanou, D.; Froudarakis, M.E. Pleural neoplastic pathology. Respir. Med. 2015, 109, 931–943. [Google Scholar] [CrossRef] [PubMed]
- Haratake, N.; Shoji, F.; Kozuma, Y.; Okamoto, T.; Maehara, Y. Giant Leiomyoma Arising from the Mediastinal Pleura: A Case Report. Ann. Thorac. Cardiovasc. Surg. 2017, 23, 153–156. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Nakada, T.; Akiba, T.; Inagaki, T.; Morikawa, T.; Ohki, T. A Rare Case of Primary Intercostal Leiomyoma: Complete Resection Followed by Reconstruction Using a Gore-Tex® Dual Mesh. Ann. Thorac. Cardiovasc. Surg. 2014, 20, 617–621. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Qiu, X.; Zhu, D.; Wei, S.; Chen, G.; Chen, J.; Zhou, Q. Primary Leiomyoma of the pleura. World J. Surg. Oncol. 2011, 9, 76. [Google Scholar] [CrossRef] [PubMed]
- Arikura, J.; Adachi, H.; Kondo, K. A case of primary pleural leiomyoma. J. Jpn. Assoc. Chest Surg. 2011, 25, 789–793. [Google Scholar] [CrossRef][Green Version]
- Tanaka, H.; Matsuda, T.; Miyagantani, Y.; Yukioka, T.; Matsuda, H.; Shimazaki, S. Reduction of resuscitation fluid volumes in severely burned patients using ascorbic acid administration: A randomized, prospective study. Arch. Surg. 2000, 135, 326–331. [Google Scholar] [CrossRef] [PubMed]
- Moran, C.; Suster, S.; Koss, M.N. Smooth muscle tumours presenting as pleural neoplasms. Histopathology 1995, 27, 227–234. [Google Scholar] [CrossRef] [PubMed]
- Proca, D.M.; Ross, P.; Pratt, J.; Frankel, W.L. Smooth muscle tumor of the pleura. A case report and review of the literature. Arch. Pathol. Lab. Med. 2000, 124, 1688–1692. [Google Scholar] [CrossRef] [PubMed]
- Turhan, K.; Çakan, A.; Cagirici, U. Leiomyoma: An unusual pleural tumor: Report of a case. Turk. Resp. J. 2008, 9, 53–55. [Google Scholar]
- Ziyade, S.; Ugurlucan, M.; Soysal, O.; Akdemir, O.C. Leiomyoma of the extrapleural chest wall: An atypical location. Arch. Med. Sci. AMS 2011, 2, 356. [Google Scholar] [CrossRef] [PubMed]
- Nose, N.; Inoue, M.; Kodate, M.; Kawaguchi, M.; Yasumoto, K. Leiomyoma originating from the extrapleural tissue of the chest wall. Gen. Thorac. Cardiovasc. Surg. 2006, 54, 242–245. [Google Scholar] [CrossRef] [PubMed]
- Kuman, N.K.; Pabuscu, E.; Meteoglu, I. Leiomyomas requiring chest wall resection and reconstruction. Gen. Thorac. Cardiovasc. Surg. 2012, 62, 186–190. [Google Scholar] [CrossRef] [PubMed]
- Laughlin, S.K.; Baird, D.D.; Savitz, D.A.; Herring, A.H.; Hartmann, K.E. Prevalence of uterine leiomyomas in the first trimester of pregnancy: An ultrasound screening study. Obs. Gynecol. 2009, 113, 630. [Google Scholar] [CrossRef] [PubMed]
- Borgfeldt, C.; Andolf, E. Transvaginal ultrasonographic findings in the uterus and the endometrium: Low prevalence of leiomyoma in a random sample of women age 25–40 years. Acta Obs. Gynecol. Scand. 2000, 79, 202–207. [Google Scholar] [CrossRef]
- Karasick, S.; Lev-Toaff, A.S.; Toaff, M.E. Imaging of uterine leiomyomas. Am. J. Roentgenol. 1992, 158, 799–805. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Ma, H.; Cao, J. Benign pulmonary metastasizing leiomyoma of the uterus: A case report. Oncol. Lett. 2015, 9, 1347–1350. [Google Scholar] [CrossRef] [PubMed]
- Jautzke, G.; Müller-Ruchholtz, E.; Thalmann, U. Immunohistological detection of estrogen and progesterone receptors in multiple and well differentiated leiomyomatous lung tumors in women with uterine leiomyomas (so-called benign metastasizing leiomyomas): A report on 5 cases. Pathol. Res. Pract. 1996, 192, 215–223. [Google Scholar] [CrossRef]
- Fu, Y.; Li, H.; Tian, B.; Hu, B. Pulmonary benign metastasizing leiomyoma: A case report and review of the literature. World J. Surg. Oncol. 2012, 10, 268. [Google Scholar] [CrossRef] [PubMed]
- Greenspan, B.S. Role of PET/CT for precision medicine in lung cancer: Perspective of the Society of Nuclear Medicine and Molecular Imaging. Transl. Lung Cancer Res. 2017, 6, 617–620. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).