Abstract
Upper tract urothelial carcinoma (UTUC) is a rare and challenging-to-treat malignancy. In most patients it is a sporadic tumor entity, less commonly it falls on the spectrum of Lynch syndrome, an autosomal dominant familial tumor syndrome. Localized UTUC with high-risk features as well as the metastatic disease scenario might require systemic therapy. Platinum-based combination chemotherapy is currently the recommended management option. However, the introduction of immune checkpoint inhibitors into the therapeutic armamentarium has led to a paradigm shift in treatment standards. Immunotherapy has been shown to be safe and effective in treating at least metastatic UTUC, although UTUC-specific high-level evidence is still lacking. Recent technological advances and noteworthy research efforts have greatly improved the general understanding of the biological landscape of UTUC. According to the main findings, UTUC represent a particular subtype of urothelial carcinoma frequently associated with activated FGFR3 signaling, a luminal–papillary phenotype and a T-cell-depleted microenvironment. This improved knowledge promises precision oncology approaches that match treatment decision strategies and genomic profile to ultimately result in better clinical outcomes. The aim of this review was to summarize the main currently available evidence on immune checkpoint inhibition and clinical genomics in UTUC.
1. Introduction
Upper tract urothelial carcinoma (UTUC) is a rare and challenging-to-treat malignancy. It defines urothelial carcinomas (UCs) with primary pyelocaliceal and ureteral tumor location. Although UTUC differs in terms of biological and clinical features from urothelial carcinoma of the bladder (UCB), it is often addressed based on data extrapolated from UCB studies, due to the limited high-level UTUC-specific evidence [1].
UTUC exhibits aggressive clinical behavior. At the time of diagnosis, more than half of patients with UTUC harbor muscle-invasive disease, and up to one in ten are already metastatic [2]. UTUC is also associated with poor clinical outcomes, with 5-year specific survival less than 50 and 10% for pT2/T3 and pT4 tumor stages, respectively [1]. Therefore, non-metastatic UTUC with high-risk features is already considered an early systemic disease [3]. Radical nephroureterectomy (RNU) still represents the mainstay of treatment for patients with high-risk localized UTUC. Based on the currently available literature, the addition of platinum-based combination chemotherapy, to definitive surgery has been shown to improve the prognosis compared to RNU alone [4,5,6] and constitutes the current gold standard treatment according to international guidelines.
Metastatic UTUC is a deadly disease. Platinum-based combination chemotherapy remains the recommended management strategy in the first-line setting of the metastatic scenario. However, the introduction of immune checkpoint (IC) inhibition has determined a paradigm shift in treatment standards [7].
Major advances in the understanding of UTUC biology have been provided by recent genomic and gene expression studies [8]. This improved knowledge promises precision oncology approaches that match treatment decision strategies and genomic profile to ultimately result in better clinical outcomes. Additionally, light has been shed on novel pathways for therapeutic targeting [9].
This review summarizes the main currently available evidence on IC inhibition and clinical genomics in UTUC.
2. Immune Checkpoint Inhibition
Immunotherapy is changing the way we think about and treat UC [7,10,11]. Addressing a high decades-old unmet medical need, the PD-1/PD-L1 pathway inhibition has been shown to be safe and effective in the treatment of metastatic UC. Furthermore, the inhibition of IC CTLA-4 in different stages of the disease is being investigated [11,12]. However, immunotherapy for UTUC still lacks specific evidence. The available data are in fact extrapolated from UC studies, regardless of the primary tumor location in the upper or lower urothelium.
The use of immunotherapy, through IC inhibitors (ICIs), for the therapeutic management of UTUC is very intriguing. Indeed, UTUC remains a challenging to treat tumor due to several aspects [6]. First, patients with UTUC are commonly elderly and frail. Second, both high-risk localized and metastatic diseases might require systemic therapy. Third, most patients have decreased renal function at baseline (and even more after surgery due to the loss of a renal unit) and are unfit for nephrotoxic therapies. Fourth, the difficulties linked to the preoperative tumor assessment in localized disease increase the risk of overtreatment in patients with non-muscle invasive disease [6,7]. Taken together, these observations highlight the need for a therapeutic strategy in UTUC patients that should be effective and associated with a low toxicity profile.
Table 1 summarizes the main currently available data on immunotherapy in UTUC.

Table 1.
Main currently available data on immune checkpoint inhibition in UTUC.
2.1. High-Risk Localized UTUC
RNU remains the cornerstone of treatment for patients with localized UTUC and high-risk features. Recent evidence points to the significant survival benefit of adding systemic therapy, in the form of platinum-based chemotherapy, compared to surgery alone. Currently, the evidence for adjuvant chemotherapy appears stronger (with positive level 1 evidence) than that for neoadjuvant chemotherapy (at best level 2 evidence) [21,22]. Accordingly, the 2021 European Association of Urology (EAU) guidelines strongly recommend the use of post-operative systemic platinum-based chemotherapy in patients with muscle-invasive UTUC [1].
The treatment scenario of non-metastatic muscle-invasive bladder carcinoma (MIBC) has been revolutionized by recent studies supporting the use of ICIs. Short courses of single-agent neoadjuvant pembrolizumab prior to radical cystectomy were shown to be safe and effective, with 42% ypT0 and 54% yp < T2 responses for MIBC patients, in the PURE-01 trial [23].
Following this exciting success, the PURE-02 study, a feasibility study of neoadjuvant pembrolizumab in patients with UTUC, was carried out [13]. Ten patients with non-metastatic UTUC presenting high-risk features according to the modified EAU definition were enrolled [1]. Overall, five, three, and two patients harbored UTUC in the ureters, renal pelvis, and both sites for unilateral multifocal involvement, respectively; seven patients (70%) were male. Treatment consisted of three courses of 200 mg intravenous pembrolizumab every 3 weeks, followed by RNU within 14 days of the last dose. One (10%) treatment-related death occurred within a month of the first pembrolizumab course due to the development of pneumonia and septic shock. Nine patients (90%) completed the neoadjuvant course. One (14.3%) patient achieved a clinical and radiological complete response and refused to undergo RNU. However, her follow-up is still too immature to draw appropriate conclusions. The remaining cases were characterized as uncertain responses or overt nonresponses to the neoadjuvant treatment. Indeed, two (20%) had disease progression at clinical restaging and received subsequent cisplatin-based chemotherapy, prior to RNU.
Although the sample size was very small, the authors of the PURE-02 study did not observe promising signals of activity from single-agent pembrolizumab in the neoadjuvant treatment of UTUC. Possible reasons for the conflicting results reported by the PURE-01 and PURE-02 studies on the preoperative efficacy of pembrolizumab in lower and upper urinary tract UC, respectively, may lie in the intrinsic biological diversity of tumors based on primary location along the urothelium. Indeed, UTUC exhibits a unique mutational and gene expression profile, which will be carefully analyzed below.
Finally, the efficacy and tolerability of immunotherapy, specifically durvalumab agent, in combination with chemotherapy in the neoadjuvant setting of high-risk localized UTUC patients is currently being investigated in phase II [24] and phase III [25] clinical trials. However, these mentioned studies are still in recruiting status, and no results have been published yet.
2.2. First-Line Metastatic UTUC
Cisplatin-based chemotherapy has been the first-line treatment for patients with metastatic UC for over three decades, regardless of the primary tumor location in the lower or upper urinary tract. This systemic disease management strategy conferred an overall survival (OS) benefit of 9–15 months, but at the cost of a significant burden of toxicity [26]. However, in real life, up to two-thirds of UC patients result in being unfit for cisplatin, due to impaired performance status or comorbidities, and alternative chemotherapy approaches are associated with a short duration of response, poor survival, and high toxicity [27,28].
The use of the ICIs atezolizumab and pembrolizumab has been approved for the treatment of PD-L1-positive patients with metastatic UC ineligible for cisplatin-based first-line chemotherapy, based on the results of the phase II trials IMvigor 210 and KEYNOTE-052 [14,15].
Atezolizumab was associated with a median OS benefit of 15.9 months in the cisplatin-unfit patient cohort with metastatic UC included in the IMvigor 210 study (median follow-up 17.2 months) [14]. The proportion of patients with UTUC (n = 33, 28%) who achieved a complete or partial response, defined as objective response rate (ORR), was 39%. Furthermore, the treatment toxicity profile has proved to be largely acceptable even considering that more than 70% of the study population showed an impairment of the renal function at baseline.
Pembrolizumab was associated with an ORR of 22% in 69 (19%) cisplatin-unfit patients with metastatic UTUC included in the KEYNOTE-052 study [15]. In the overall cohort, a PD-L1 positivity, defined as a combined positive score (CPS) ≥ 10% was related to a greater treatment response rate, with an ORR of 38%. Again, Pembrolizumab showed an acceptable toxicity profile in this disease setting.
The addition of atezolizumab and pembrolizumab to platinum-based chemotherapy in the management of metastatic UC has been investigated in two phase III randomized controlled trials (RCT), the IMvigor 130 and KEYNOTE-361, including 312 (26%) and 64 (18%) patients with UTUC, respectively [16,17]. The combination of immune checkpoint inhibition with standard-of-care chemotherapy did not show significant improvement in OS compared to chemotherapy alone, as a first-line strategy in the metastatic setting of UC.
2.3. Second-Line Metastatic UTUC
Long-term remissions after platinum-based chemotherapy for patients with metastatic UC are reported in up to 10% of patients [26]. Consequently, disease progression on platinum is a frequent occurrence. The second-line management of platinum-pretreated patients with metastatic UTUC remains challenging. Furthermore, patients have already borne a significant burden of treatment-related toxicity.
The use of the ICIs pembrolizumab, atezolizumab, avelumab, nivolumab and durvalumab has been approved for the treatment of patients with metastatic UC who have progressed during or after previous platinum-based combination chemotherapy [7]. However, contrary to pembrolizumab, recently, the Food and Drug Administration no longer approves the use of atezolizumab in this setting [29]. Moreover, durvalumab and nivolumab were tested in phase I and II studies that did not report any subgroup analyses based on primary tumor location [30,31,32].
According to the results of the phase III RCT KEYNOTE-045 trial, pembrolizumab was the first ICI supported by level 1 evidence for the treatment of UC platinum-refractory patients [18]. Over a median follow-up of 14.1 months, pembrolizumab was associated with a significant OS benefit compared to investigator/institution’s choice chemotherapy in the second-line UC management setting. In those patients with UTUC (n = 75, 13.8%), the pembrolizumab treatment was associated with a reduction in the risk of death of 50%. Additionally, the ORR was 21.1% with pembrolizumab compared with 11.4% in the chemotherapy group (p = 0.001). These findings were further confirmed after two years of follow-up [33].
Atezolizumab was associated with an ORR of 8% in 65 (21%) patients with metastatic UTUC included in the platinum-pretreated cohort of the phase II IMvigor 210 trial [19]. Interestingly, the atezolizumab treatment showed durable activity related to the PD-L1 expression on immune cells in patients with metastatic UC, with a 26% of ORR in the group of those overexpressing PD-L1 vs. 15% in the overall population. This study was even the first pointing out the association of TCGA subtypes with the response to ICIs in UC, highlighting the tumor mutation load as an efficacy biomarker.
Avelumab was associated with an ORR of 11% in 36 (22%) patients with metastatic platinum-refractory UTUC and at least 6 months of follow-up included in the phase I JAVELIN study [20].
3. Clinical Genomics in UTUC
Precision oncology aims to functionalize genomics in the therapeutic management of cancer patients. Significant efforts have been and continue to be made to understand the mechanisms that drive carcinogenesis in order to implement the personalized treatment pathway selection process and lead to better patient outcomes. Furthermore, it has allowed for the ability to identify biomarkers for clinical response [9].
UCs respond differently to standard-of-care treatment strategies depending on the location of the primary tumor [34]. This simple observation underlies potential differences in mutational and expression profiles of UCs with significant clinical implications. In fact, UCB and UTUC share purely histological appearance, differing instead in embryological, biological and practical aspects [35]. More interestingly, renal pelvis and ureteral UCs, conventionally joined as UTUC, also differ in genomics and clinical management [8].
Recent technological advances have led to a better understanding of the mutational and gene expression profiles of UCs. Although several studies have depicted the genomic landscape of UCB, knowledge of UTUC remains more limited. Again, UTUC pay the price for a lower epidemiological frequency compared to their bladder counterpart.
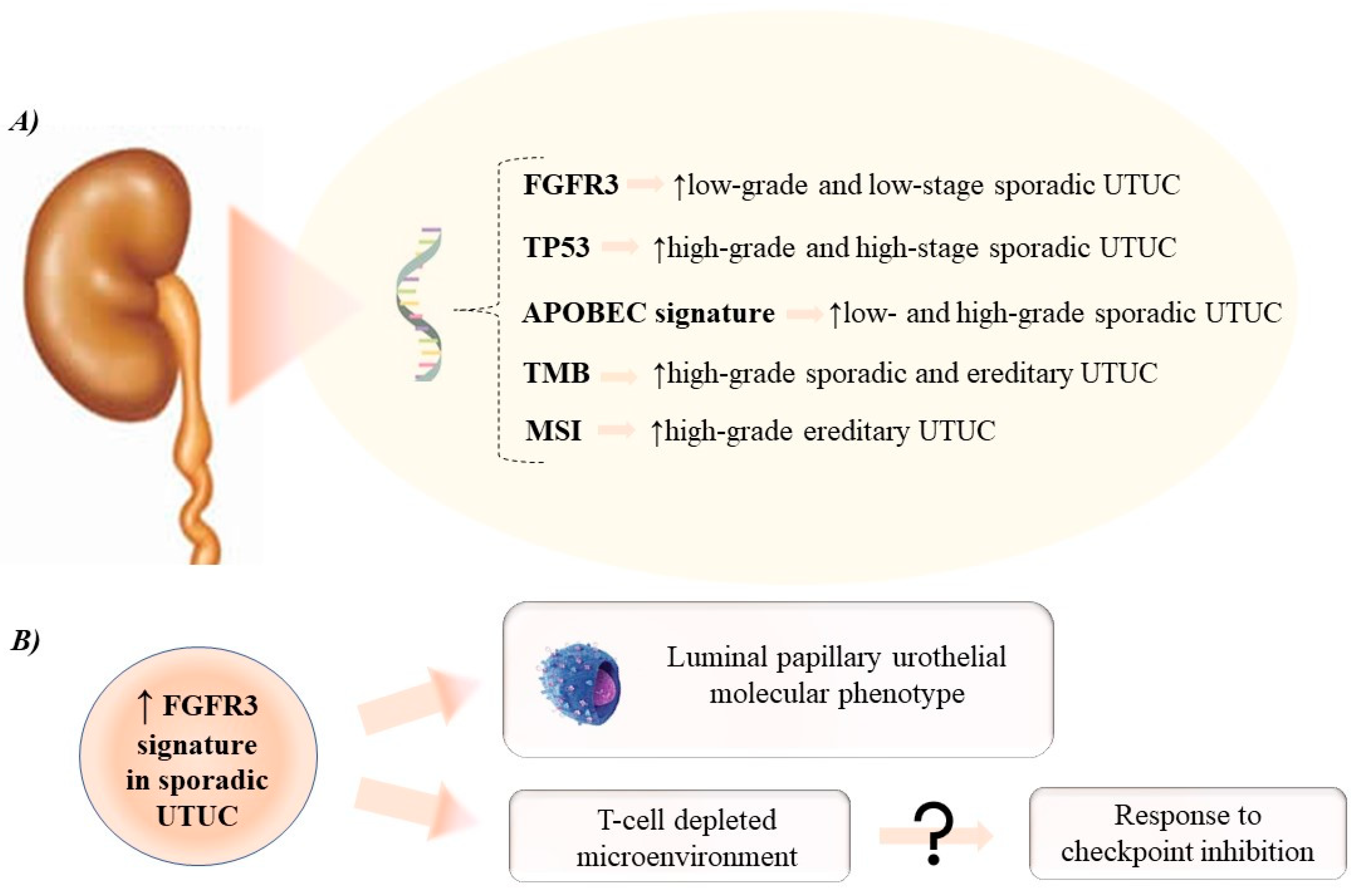
Figure 1 provides an overview of mutational and gene expression profile of UTUC.
Figure 1.
Overview of mutational (A) and gene expression (B) profile in upper tract urothelial carcinoma. APOBEC: apolilpoprotein B mRNA editing enzyme catalytic polypeptide-like; FGFR3: fibroblast growth factor receptor 3; MSI: microsatellite instability; TMB: tumor mutational burden; TP53: tumor protein 53; UTUC: upper tract urothelial carcinoma.
3.1. Mutational Profile of UTUC
Sporadic UTUC shares mutational features in similar genes and epigenetic genes with UCB, but at varying frequencies. Furthermore, genetic patterns differ according to the tumor stage and grade, both for UTUC and UCB. Lastly, different genetic profiles have been reported between UCs arising in renal pelvis vs. ureters.
Using next-generation sequencing, FGFR3 is recognized as the most frequently mutated gene in UTUC, with mutational rates ranging from 40% to 80% in sporadic tumors [36,37,38]. Most FGFR3 mutations are missense. Other common alterations are described for oncogenes or tumor suppressor genes, such as HRAS and genes involved in the p53 signaling (TP53, ATM, ATR) [39]. TP53 mutations are reported in up to 30% of UTUC. Moreover, UCs, regardless of their location in the urothelium, share a molecular signature attributed to the apolilpoprotein B mRNA editing enzyme catalytic polypeptide-like (APOBEC) family of cytosine deaminases, which converts cytosine to uracil [40]. The result is single-stranded DNA editing. Evidence showed that a high APOBEC signature mutation burden was strongly correlated with the tumor mutational burden (TMB) [36].
FGFR3 mutations are more common in low-grade and low-stage UCs. In UTUC, the incidence of FGFR3 mutations is up to 80% in low-grade tumors, while varying between 15 and 30% in their high-grade counterparts [34]. These observations are also common for UCB, where alterations in FGFR3 are more frequently reported for non-muscle-invasive bladder carcinoma (NMIBC) compared to muscle-invasive bladder carcinoma (MIBC) and particularly for low-grade NMIBC [34]. In addition, FGFR3 mutations are correlated with a better clinical prognosis. Conversely, patients with high-grade and high-stage UC appear more likely to harbor TP53 mutations. Indeed, TP53 gene alterations are the most commonly reported in MIBC, and generally correlate with more aggressive UCs and worse clinical outcomes [41].
Necchi et al. used comprehensive genomic profiling to show that FGFR3 and HRAS gene alterations were more common in UTUC compared to UCB [8]. More interestingly, the mutational frequency differences of these two genes have been reported based on the location of the primary tumor in the renal pelvis relative to the ureters. The authors reported alterations in FGFR3 and HRAS in 28 vs. 22% and 9.5 vs. 1.8% in the renal pelvis compared to ureteral tumors, respectively.
UTUC is also represented in the spectrum of Lynch syndrome, an autosomal-dominant familiar cancer syndrome [1]. Lynch-related UTUC harbor germline mutations in the DNA mismatch repair (MMR) genes, with the majority of tumors developing in MSH2 mutation carriers. Loss of function in the MMR system results in microsatellite instability (MSI) throughout the genome. MSI have been found in up to 20% of UTUC, as compared to less than 1% in UCB [42]. In addition, high MSI correlates with a higher TMB and better clinical prognosis.
3.2. Gene Expression Profile of UTUC
Several studies have addressed the comprehensive gene expression profile of UCs, mainly focusing on UCB. Five molecular subtypes of MIBC were identified in The Cancer Genome Atlas (TCGA) classification, through a combination of expression and clinical data [43]. Luminal–papillary, basal–squamous, luminal–infiltrated, luminal, and neuronal were the subtypes reported in 35, 35, 19, 6, and 5% of MIBC, according to TCGA, respectively. From a clinical-prognostic point of view, the luminal–papillary and neuronal subtypes have the best and worst survival outcomes, respectively. To overcome the classification schemes proposed later on and provide a consensus definition, Kamoun et al. recently described six biological classes of MIBC: luminal papillary (LumP), luminal nonspecified, luminal unstable (LumU), stroma-rich, basal/squamous (Ba/Sq), and neuroendocrine-like (NE-like) [44]. All luminal subtypes overexpress urothelial differentiation markers, LumP tumors have an FGFR3 signature, while Ba/Sq tumors overexpress basal markers.
Again, data on UTUC remains scarce, mainly due to its rarity. UCB and UTUC appear to share similar gene expression profiles, but at varying frequencies [34]. In this context, UCB tends to express genes that mark urothelial basal cells and belongs to the basal-like subtype, while most UTUC expresses genes consistent with a luminal urothelial molecular subtype. Even more interesting is the observation that an UCB developing after UTUC is likely to be luminal, while an UTUC arising after UCB is often basal.
The luminal expression profile of UTUC was confirmed and refined by Robinson et al. [38]. Through RNA sequencing of 32 UTUC tumors, the authors found that 84.3% (n = 24) of their samples were luminal tumors and 62.5% (n = 20) showed a luminal–papillary phenotype, using the TCGA subtypes. In addition, examining the expression of key immune genes, 87.5% (n = 28) of UTUC tumors were found to be T-cell depleted with downregulation of the T-cell-related signaling. The authors concluded that UTUC represents a particular subtype of UC associated with a luminal–papillary phenotype and T-cell-depleted microenvironment [38].
3.3. Implications for Systemic Therapy
The efficacy of systemic cancer therapy ultimately relies on the tumor genomic landscape. Advances in the knowledge of the biological profile of UTUC promise precision therapeutic management. Above all, efforts to investigate the mutational and gene expression aspects of UTUC have been noteworthy, even considering that this is often managed on the basis of UCB evidence, due to its rarity.
Platinum-based chemotherapy is currently the systemic approach of choice in both high-risk localized and metastatic UTUC [1]. It works by inducing DNA damage and promoting cellular apoptosis. A high TMB, supported by a mutation profile in TP-53 signaling or a high MSI, defines the biological identikit of UTUC that should be associated with a higher response rate to chemotherapy [45].
Immunotherapy, through the PD-1/PD-L1 pathway inhibition, has been shown to be safe and effective in treating at least metastatic UTUC [7]. It works by promoting the defense of the immune system. Again, a high TMB is associated with the expression of surface neoantigens on tumor cells and a high response rate to immunotherapy [46].
Most sporadic UTUC show mutations in the FGFR3 gene. Often, these are associated with a better prognosis. Therapeutic strategies selectively targeting the FGF receptor could be addressed to FGFR3 mutated tumors. Erdafitinib is a pan-FGF tyrosine kinase inhibitor approved as second-line treatment for locally advanced or metastatic UC with FGFR mutations [12]. In a recent phase II study, the use of erdafitinib was associated with a 40% response rate in 99 patients with disease progression following chemotherapy [47]. This study included 23 patients with UTUC and visceral metastases showing a 43% response rate. Additional FGFR-directed agents also continue to be investigated across multiple disease stage in mutated UC including infigratinib and rogaratinib among others [12]. Furthermore, ongoing trials are combining these agents with ICI and chemotherapy regimens.
Overall, UTUC exhibits a landscape of more than 50% possibly actionable genomic alterations [8]. A field of growing interest among investigators is the use of prognostic biomarkers to identify targetable biological profiles. Blood-based evaluation, using ct-DNA, of genomic signatures may present a further opportunity to develop response biomarkers for available therapeutic armamentarium options. In UCs, proof-of-concept data documented that ctDNA is detectable in plasma and urine, and could be a prognostic factor [48,49,50,51]. Liquid biopsy could represent a cost-effective and minimally invasive method for biomarker identification and patient stratification.
4. The Immune Microenvironment in UTUC
The immune defense system plays a leading role in the host’s antitumor response. This occurs mainly through the recognition of neoantigens exposed on the tumor cell surface, as a consequence of the genomic alterations that promote carcinogenesis. In particular, CD8 T cells support the immuno-elimination of tumor cells [52].
Tumors differ in immunogenicity levels, and therefore in the tumor immune microenvironment. Consequently, different tumors exhibit different immunological potential to counteract the development and progression of the disease. Overall, UCs have long been recognized as being strongly immunogenic tumors [10].
Immuno-editing is defined as the path by which the tumor bypasses immune-surveillance. Activation of T-cell function inhibitory pathways, such as the PD-1/PD-L1 IC axis, is a well-known tumor immuno-evasion strategy. Indeed, this pathway has been shown to play an important role in the development of UC [53].
Taken together, these observations provide the rationale for the clinical investigation of cancer immunotherapy, through IC inhibition, in UC at the beginning of the last decade. At that time, the use of antibodies inhibiting the PD-1/PD-L1 pathway had already demonstrated robust anti-cancer activity in several malignancies [54].
Overall, immunotherapy with ICI has been shown to be effective in treating UC [7].
UTUC display different mutational and gene expression profiles compared to UCBs. It follows that the tumor immune microenvironment may also differ among UC based on the primary tumor location. Actually, sporadic UTUC has a luminal–papillary T-cell-depleted contexture and activated FGFR3 signaling. In addition, upregulation of FGFR3 in UTUC seems to be associated with a lower CD8 T-cell gene signature and, more interestingly, it has been shown to be important in shaping the observed T-cell-depleted phenotype [38]. Consequently, sporadic UTUC should frequently be characterized by an immune desert profile and refractoriness to immunotherapy. In contrast, UTUC developed in a Lynch syndrome context exhibits high MSI and TMB. According to these biological features, it could be considered an immune hot tumor. However, the profiles depicted did not match the clinical outcomes reported in the leading studies investigating the efficacy of immunotherapy in UTUC [7]. Again, this is indirect evidence that a significant knowledge gap has yet to be filled.
5. Conclusions
UTUC is a challenging-to treat malignancy, also due to its rarity and limited high-level evidence to support its clinical management. However, significant advances in knowledge have recently been made to ultimately improve patient prognosis. Immunotherapy is changing the way we think about and treat UC, and PD-1/PD-L1 pathway inhibition has been shown to be safe and effective in the systemic management of metastatic UTUC. Currently, therapeutic decision making remains primarily guided by clinical and radiological evaluation. Improved understanding of the genomic landscape of UTUC should lead to a paradigm shift in treatment strategies. Several therapeutically actionable molecular pathways have recently been described, and novel clinical trials investigating therapeutic options for UTUC by stratifying patients for the biological profile are expected.
Author Contributions
Conceptualization, G.C. and E.X.; methodology, C.C.R. and A.P.; validation, I.O., B.P., V.E., V.M. and J.-F.H., data curation, P.L.-C. and A.P.; writing—original draft preparation, G.C., C.C.R. and A.P.; writing—review and editing, I.O., P.L.-C., B.P., V.E., V.M., J.-F.H., S.F.S. and E.X. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
Our research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
- Rouprêt, M.; Babjuk, M.; Burger, M.; Capoun, O.; Cohen, D.; Compérat, E.M.; Cowan, N.C.; Dominguez-Escrig, J.L.; Gontero, P.; Hugh Mostafid, A.; et al. European Association of Urology Guidelines on Upper Urinary Tract Urothelial Carcinoma: 2020 Update. Eur. Urol. 2020, 79, 62–79. [Google Scholar] [CrossRef]
- Collà Ruvolo, C.; Nocera, L.; Stolzenbach, L.F.; Wenzel, M.; Cucchiara, V.; Tian, Z.; Shariat, S.F.; Saad, F.; Longo, N.; Montorsi, F.; et al. Incidence and Survival Rates of Contemporary Patients with Invasive Upper Tract Urothelial Carcinoma. Eur. Urol. Oncol. 2020, 4, 792–801. [Google Scholar] [CrossRef]
- Collà Ruvolo, C.; Nocera, L.; Stolzenbach, L.F.; Wenzel, M.; Califano, G.; Tian, Z.; Verze, P.; Shariat, S.F.; Saad, F.; Briganti, A.; et al. Tumor Size Predicts Muscle-Invasive and Non-Organ-Confined Disease in Upper Tract Urothelial Carcinoma at Radical Nephroureterectomy. Eur. Urol. Focus 2021. [Google Scholar] [CrossRef]
- Leow, J.J.; Chong, Y.L.; Chang, S.L.; Valderrama, B.P.; Powles, T.; Bellmunt, J. Neoadjuvant and Adjuvant Chemotherapy for Upper Tract Urothelial Carcinoma: A 2020 Systematic Review and Meta-Analysis, and Future Perspectives on Systemic Therapy. Eur. Urol. 2021, 79, 635–654. [Google Scholar] [CrossRef]
- Pradère, B.; Califano, G.; Xylinas, E. Perioperative Chemotherapy for Upper Tract Urothelial Carcinoma: Show Me the Evidence. Curr. Opin. Urol. 2021, 31, 66–67. [Google Scholar] [CrossRef]
- Califano, G.; Xylinas, E. Re: Phase II Trial of Neoadjuvant Systemic Chemotherapy Followed by Extirpative Surgery in Patients with High Grade Upper Tract Urothelial Carcinoma. Eur. Urol. 2020, 78, 113–114. [Google Scholar] [CrossRef]
- Califano, G.; Ouzaid, I.; Verze, P.; Hermieu, J.-F.; Mirone, V.; Xylinas, E. Immune Checkpoint Inhibition in Upper Tract Urothelial Carcinoma. World J. Urol. 2020, 39, 1357–1367. [Google Scholar] [CrossRef]
- Necchi, A.; Madison, R.; Pal, S.K.; Ross, J.S.; Agarwal, N.; Sonpavde, G.; Joshi, M.; Yin, M.; Miller, V.A.; Grivas, P.; et al. Comprehensive Genomic Profiling of Upper-Tract and Bladder Urothelial Carcinoma. Eur. Urol. Focus 2021, 7, 1339–1346. [Google Scholar] [CrossRef]
- Hassler, M.R.; Bray, F.; Catto, J.W.F.; Grollman, A.P.; Hartmann, A.; Margulis, V.; Matin, S.F.; Roupret, M.; Sfakianos, J.P.; Shariat, S.F.; et al. Molecular Characterization of Upper Tract Urothelial Carcinoma in the Era of Next-Generation Sequencing: A Systematic Review of the Current Literature. Eur. Urol. 2020, 78, 209–220. [Google Scholar] [CrossRef]
- Califano, G.; Ouzaid, I.; Verze, P.; Stivalet, N.; Hermieu, J.-F.; Xylinas, E. New Immunotherapy Treatments in Non-Muscle Invasive Bladder Cancer. Arch. Esp. Urol. 2020, 73, 945–953. [Google Scholar]
- Peyrottes, A.; Ouzaid, I.; Califano, G.; Hermieu, J.-F.; Xylinas, E. Neoadjuvant Immunotherapy for Muscle-Invasive Bladder Cancer. Med. Kaunas Lith. 2021, 57, 769. [Google Scholar] [CrossRef]
- Cathomas, R.; Lorch, A.; Bruins, H.M.; Compérat, E.M.; Cowan, N.C.; Efstathiou, J.A.; Fietkau, R.; Gakis, G.; Hernández, V.; Espinós, E.L.; et al. The 2021 Updated European Association of Urology Guidelines on Metastatic Urothelial Carcinoma. Eur. Urol. 2022, 81, 95–103. [Google Scholar] [CrossRef]
- Necchi, A.; Martini, A.; Raggi, D.; Cucchiara, V.; Colecchia, M.; Lucianò, R.; Villa, L.; Mazzone, E.; Basile, G.; Scuderi, S.; et al. A Feasibility Study of Preoperative Pembrolizumab before Radical Nephroureterectomy in Patients with High-Risk, Upper Tract Urothelial Carcinoma: PURE-02. Urol. Oncol. Semin. Orig. Investig. 2022, 40, 10.e1–10.e6. [Google Scholar] [CrossRef]
- Balar, A.V.; Galsky, M.D.; Rosenberg, J.E.; Powles, T.; Petrylak, D.P.; Bellmunt, J.; Loriot, Y.; Necchi, A.; Hoffman-Censits, J.; Perez-Gracia, J.L.; et al. Atezolizumab as First-Line Treatment in Cisplatin-Ineligible Patients with Locally Advanced and Metastatic Urothelial Carcinoma: A Single-Arm, Multicentre, Phase 2 Trial. Lancet 2017, 389, 67–76. [Google Scholar] [CrossRef] [Green Version]
- Balar, A.V.; Castellano, D.; O’Donnell, P.H.; Grivas, P.; Vuky, J.; Powles, T.; Plimack, E.R.; Hahn, N.M.; de Wit, R.; Pang, L.; et al. First-Line Pembrolizumab in Cisplatin-Ineligible Patients with Locally Advanced and Unresectable or Metastatic Urothelial Cancer (KEYNOTE-052): A Multicentre, Single-Arm, Phase 2 Study. Lancet Oncol. 2017, 18, 1483–1492. [Google Scholar] [CrossRef]
- Galsky, M.D.; Arija, J.Á.A.; Bamias, A.; Davis, I.D.; De Santis, M.; Kikuchi, E.; Garcia-del-Muro, X.; De Giorgi, U.; Mencinger, M.; Izumi, K.; et al. Atezolizumab with or without Chemotherapy in Metastatic Urothelial Cancer (IMvigor130): A Multicentre, Randomised, Placebo-Controlled Phase 3 Trial. Lancet 2020, 395, 1547–1557. [Google Scholar] [CrossRef]
- Powles, T.; Csőszi, T.; Özgüroğlu, M.; Matsubara, N.; Géczi, L.; Cheng, S.Y.-S.; Fradet, Y.; Oudard, S.; Vulsteke, C.; Morales Barrera, R.; et al. Pembrolizumab Alone or Combined with Chemotherapy versus Chemotherapy as First-Line Therapy for Advanced Urothelial Carcinoma (KEYNOTE-361): A Randomised, Open-Label, Phase 3 Trial. Lancet Oncol. 2021, 22, 931–945. [Google Scholar] [CrossRef]
- Bellmunt, J.; de Wit, R.; Vaughn, D.J.; Fradet, Y.; Lee, J.-L.; Fong, L.; Vogelzang, N.J.; Climent, M.A.; Petrylak, D.P.; Choueiri, T.K.; et al. Pembrolizumab as Second-Line Therapy for Advanced Urothelial Carcinoma. N. Engl. J. Med. 2017, 376, 1015–1026. [Google Scholar] [CrossRef] [Green Version]
- Rosenberg, J.E.; Hoffman-Censits, J.; Powles, T.; van der Heijden, M.S.; Balar, A.V.; Necchi, A.; Dawson, N.; O’Donnell, P.H.; Balmanoukian, A.; Loriot, Y.; et al. Atezolizumab in Patients with Locally Advanced and Metastatic Urothelial Carcinoma Who Have Progressed Following Treatment with Platinum-Based Chemotherapy: A Single-Arm, Multicentre, Phase 2 Trial. Lancet 2016, 387, 1909–1920. [Google Scholar] [CrossRef] [Green Version]
- Patel, M.R.; Ellerton, J.; Infante, J.R.; Agrawal, M.; Gordon, M.; Aljumaily, R.; Britten, C.D.; Dirix, L.; Lee, K.-W.; Taylor, M.; et al. Avelumab in Metastatic Urothelial Carcinoma after Platinum Failure (JAVELIN Solid Tumor): Pooled Results from Two Expansion Cohorts of an Open-Label, Phase 1 Trial. Lancet Oncol. 2018, 19, 51–64. [Google Scholar] [CrossRef]
- Birtle, A.; Johnson, M.; Chester, J.; Jones, R.; Dolling, D.; Bryan, R.T.; Harris, C.; Winterbottom, A.; Blacker, A.; Catto, J.W.F.; et al. Adjuvant Chemotherapy in Upper Tract Urothelial Carcinoma (the POUT Trial): A Phase 3, Open-Label, Randomised Controlled Trial. Lancet 2020, 395, 1268–1277. [Google Scholar] [CrossRef]
- Foerster, B.; Abufaraj, M.; Petros, F.; Azizi, M.; Gupta, M.; Schweitzer, D.; Margulis, V.; Iwata, T.; Kimura, S.; Shabsigh, A.; et al. Efficacy of Preoperative Chemotherapy for High Risk Upper Tract Urothelial Carcinoma. J. Urol. 2020, 203, 1101–1108. [Google Scholar] [CrossRef]
- Necchi, A.; Anichini, A.; Raggi, D.; Briganti, A.; Massa, S.; Lucianò, R.; Colecchia, M.; Giannatempo, P.; Mortarini, R.; Bianchi, M.; et al. Pembrolizumab as Neoadjuvant Therapy Before Radical Cystectomy in Patients With Muscle-Invasive Urothelial Bladder Carcinoma (PURE-01): An Open-Label, Single-Arm, Phase II Study. J. Clin. Oncol. 2018, 36, 3353–3360. [Google Scholar] [CrossRef] [Green Version]
- Centre Hospitalier Universitaire de Nîmes. Safety & Efficacy of Neoadjuvant Immunotherapy With Durvalumab (MEDI 4736) Combined With Neoadjuvant Chemotherapy (Gemcitabine/Cisplatin or Gemcitabine/Carboplatin) in Patients With Operable, High-Risk, Localized Urothelial Carcinoma of the Upper Urinary Tract; Centre Hospitalier Universitaire de Nîmes: Nîmes, France, 2021. Available online: www.clinicaltrials.gov (accessed on 27 December 2021).
- National Cancer Institute (NCI). A Phase II/III Trial of MEDI4736 (Durvalumab) and Chemotherapy for Patients With High Grade Upper Tract Urothelial Cancer Prior to Nephroureterectomy; National Cancer Institute (NCI): Bethesda, MD, USA, 2021. Available online: www.clinicaltrials.gov (accessed on 27 December 2021).
- Loehrer, P.J.; Einhorn, L.H.; Elson, P.J.; Crawford, E.D.; Kuebler, P.; Tannock, I.; Raghavan, D.; Stuart-Harris, R.; Sarosdy, M.F.; Lowe, B.A. A Randomized Comparison of Cisplatin Alone or in Combination with Methotrexate, Vinblastine, and Doxorubicin in Patients with Metastatic Urothelial Carcinoma: A Cooperative Group Study. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 1992, 10, 1066–1073. [Google Scholar] [CrossRef]
- Galsky, M.D.; Hahn, N.M.; Rosenberg, J.; Sonpavde, G.; Hutson, T.; Oh, W.K.; Dreicer, R.; Vogelzang, N.; Sternberg, C.N.; Bajorin, D.F.; et al. A Consensus Definition of Patients with Metastatic Urothelial Carcinoma Who Are Unfit for Cisplatin-Based Chemotherapy. Lancet Oncol. 2011, 12, 211–214. [Google Scholar] [CrossRef]
- Galsky, M.D.; Hahn, N.M.; Rosenberg, J.; Sonpavde, G.; Hutson, T.; Oh, W.K.; Dreicer, R.; Vogelzang, N.; Sternberg, C.N.; Bajorin, D.F.; et al. Treatment of Patients With Metastatic Urothelial Cancer “Unfit” for Cisplatin-Based Chemotherapy. J. Clin. Oncol. 2011, 29, 2432–2438. [Google Scholar] [CrossRef] [Green Version]
- Atezolizumab for Urothelial Carcinoma. Available online: https://www.fda.gov/drugs/resources-information-approved-drugs/atezolizumab-urothelial-carcinoma (accessed on 27 December 2021).
- Powles, T.; O’Donnell, P.H.; Massard, C.; Arkenau, H.-T.; Friedlander, T.W.; Hoimes, C.J.; Lee, J.L.; Ong, M.; Sridhar, S.S.; Vogelzang, N.J.; et al. Efficacy and Safety of Durvalumab in Locally Advanced or Metastatic Urothelial Carcinoma: Updated Results From a Phase 1/2 Open-Label Study. JAMA Oncol. 2017, 3, e172411. [Google Scholar] [CrossRef]
- Sharma, P.; Callahan, M.K.; Bono, P.; Kim, J.; Spiliopoulou, P.; Calvo, E.; Pillai, R.N.; Ott, P.A.; de Braud, F.; Morse, M.; et al. Nivolumab Monotherapy in Recurrent Metastatic Urothelial Carcinoma (CheckMate 032): A Multicentre, Open-Label, Two-Stage, Multi-Arm, Phase 1/2 Trial. Lancet Oncol. 2016, 17, 1590–1598. [Google Scholar] [CrossRef] [Green Version]
- Sharma, P.; Retz, M.; Siefker-Radtke, A.; Baron, A.; Necchi, A.; Bedke, J.; Plimack, E.R.; Vaena, D.; Grimm, M.-O.; Bracarda, S.; et al. Nivolumab in Metastatic Urothelial Carcinoma after Platinum Therapy (CheckMate 275): A Multicentre, Single-Arm, Phase 2 Trial. Lancet Oncol. 2017, 18, 312–322. [Google Scholar] [CrossRef]
- Fradet, Y.; Bellmunt, J.; Vaughn, D.J.; Lee, J.L.; Fong, L.; Vogelzang, N.J.; Climent, M.A.; Petrylak, D.P.; Choueiri, T.K.; Necchi, A.; et al. Randomized Phase III KEYNOTE-045 Trial of Pembrolizumab versus Paclitaxel, Docetaxel, or Vinflunine in Recurrent Advanced Urothelial Cancer: Results of >2 Years of Follow-Up. Ann. Oncol. 2019, 30, 970–976. [Google Scholar] [CrossRef]
- Sfakianos, J.P.; Gul, Z.; Shariat, S.F.; Matin, S.F.; Daneshmand, S.; Plimack, E.; Lerner, S.; Roupret, M.; Pal, S. Genetic Differences Between Bladder and Upper Urinary Tract Carcinoma: Implications for Therapy. Eur. Urol. Oncol. 2021, 4, 170–179. [Google Scholar] [CrossRef]
- Green, D.A.; Rink, M.; Xylinas, E.; Matin, S.F.; Stenzl, A.; Roupret, M.; Karakiewicz, P.I.; Scherr, D.S.; Shariat, S.F. Urothelial Carcinoma of the Bladder and the Upper Tract: Disparate Twins. J. Urol. 2013, 189, 1214–1221. [Google Scholar] [CrossRef]
- Moss, T.J.; Qi, Y.; Xi, L.; Peng, B.; Kim, T.-B.; Ezzedine, N.E.; Mosqueda, M.E.; Guo, C.C.; Czerniak, B.A.; Ittmann, M.; et al. Comprehensive Genomic Characterization of Upper Tract Urothelial Carcinoma. Eur. Urol. 2017, 72, 641–649. [Google Scholar] [CrossRef]
- Sfakianos, J.P.; Cha, E.K.; Iyer, G.; Scott, S.N.; Zabor, E.C.; Shah, R.H.; Ren, Q.; Bagrodia, A.; Kim, P.H.; Hakimi, A.A.; et al. Genomic Characterization of Upper Tract Urothelial Carcinoma. Eur. Urol. 2015, 68, 970–977. [Google Scholar] [CrossRef] [Green Version]
- Robinson, B.D.; Vlachostergios, P.J.; Bhinder, B.; Liu, W.; Li, K.; Moss, T.J.; Bareja, R.; Park, K.; Tavassoli, P.; Cyrta, J.; et al. Upper Tract Urothelial Carcinoma Has a Luminal-Papillary T-Cell Depleted Contexture and Activated FGFR3 Signaling. Nat. Commun. 2019, 10, 2977. [Google Scholar] [CrossRef] [Green Version]
- Thouvenin, J.; Martínez Chanzá, N.; Alhalabi, O.; Lang, H.; Tannir, N.M.; Barthélémy, P.; Malouf, G.G. Efficacy of Immune Checkpoint Inhibitors in Upper Tract Urothelial Carcinomas: Current Knowledge and Future Directions. Cancers 2021, 13, 4341. [Google Scholar] [CrossRef]
- Roberts, S.A.; Lawrence, M.S.; Klimczak, L.J.; Grimm, S.A.; Fargo, D.; Stojanov, P.; Kiezun, A.; Kryukov, G.V.; Carter, S.L.; Saksena, G.; et al. An APOBEC Cytidine Deaminase Mutagenesis Pattern Is Widespread in Human Cancers. Nat. Genet. 2013, 45, 970–976. [Google Scholar] [CrossRef]
- Audenet, F.; Isharwal, S.; Cha, E.K.; Donoghue, M.T.A.; Drill, N.; Ostrovnaya, I.; Pietzak, E.J.; Sfakianos, J.P.; Bagrodia, A.; Murugan, P.; et al. Clonal Relatedness and Mutational Differences between Upper Tract and Bladder Urothelial Carcinoma. Clin. Cancer Res. 2019, 25, 967–976. [Google Scholar] [CrossRef] [Green Version]
- Bonneville, R.; Krook, M.A.; Kautto, E.A.; Miya, J.; Wing, M.R.; Chen, H.-Z.; Reeser, J.W.; Yu, L.; Roychowdhury, S. Landscape of Microsatellite Instability Across 39 Cancer Types. JCO Precis. Oncol. 2017, 1, 73. [Google Scholar] [CrossRef]
- Robertson, A.G.; Kim, J.; Al-Ahmadie, H.; Bellmunt, J.; Guo, G.; Cherniack, A.D.; Hinoue, T.; Laird, P.W.; Hoadley, K.A.; Akbani, R.; et al. Comprehensive Molecular Characterization of Muscle-Invasive Bladder Cancer. Cell 2018, 174, 1033. [Google Scholar] [CrossRef] [Green Version]
- Kamoun, A.; de Reyniès, A.; Allory, Y.; Sjödahl, G.; Robertson, A.G.; Seiler, R.; Hoadley, K.A.; Groeneveld, C.S.; Al-Ahmadie, H.; Choi, W.; et al. A Consensus Molecular Classification of Muscle-Invasive Bladder Cancer. Eur. Urol. 2020, 77, 420–433. [Google Scholar] [CrossRef]
- Teo, M.Y.; Bambury, R.M.; Zabor, E.C.; Jordan, E.; Al-Ahmadie, H.; Boyd, M.E.; Bouvier, N.; Mullane, S.A.; Cha, E.K.; Roper, N.; et al. DNA Damage Response and Repair Gene Alterations Are Associated With Improved Survival In Patients With Platinum-Treated Advanced Urothelial Carcinoma. Clin. Cancer Res. Off. J. Am. Assoc. Cancer Res. 2017, 23, 3610–3618. [Google Scholar] [CrossRef] [Green Version]
- van Dijk, N.; Funt, S.A.; Blank, C.U.; Powles, T.; Rosenberg, J.E.; van der Heijden, M.S. The Cancer Immunogram as a Framework for Personalized Immunotherapy in Urothelial Cancer. Eur. Urol. 2019, 75, 435–444. [Google Scholar] [CrossRef]
- Loriot, Y.; Necchi, A.; Park, S.H.; Garcia-Donas, J.; Huddart, R.; Burgess, E.; Fleming, M.; Rezazadeh, A.; Mellado, B.; Varlamov, S.; et al. Erdafitinib in Locally Advanced or Metastatic Urothelial Carcinoma. N. Engl. J. Med. 2019, 381, 338–348. [Google Scholar] [CrossRef]
- Rebuzzi, S.E.; Banna, G.L.; Murianni, V.; Damassi, A.; Giunta, E.F.; Fraggetta, F.; De Giorgi, U.; Cathomas, R.; Rescigno, P.; Brunelli, M.; et al. Prognostic and Predictive Factors in Advanced Urothelial Carcinoma Treated with Immune Checkpoint Inhibitors: A Review of the Current Evidence. Cancers 2021, 13, 5517. [Google Scholar] [CrossRef]
- Birkenkamp-Demtröder, K.; Christensen, E.; Nordentoft, I.; Knudsen, M.; Taber, A.; Høyer, S.; Lamy, P.; Agerbæk, M.; Jensen, J.B.; Dyrskjøt, L. Monitoring Treatment Response and Metastatic Relapse in Advanced Bladder Cancer by Liquid Biopsy Analysis. Eur. Urol. 2018, 73, 535–540. [Google Scholar] [CrossRef]
- Patel, K.M.; van der Vos, K.E.; Smith, C.G.; Mouliere, F.; Tsui, D.; Morris, J.; Chandrananda, D.; Marass, F.; van den Broek, D.; Neal, D.E.; et al. Association Of Plasma And Urinary Mutant DNA With Clinical Outcomes In Muscle Invasive Bladder Cancer. Sci. Rep. 2017, 7, 5554. [Google Scholar] [CrossRef] [Green Version]
- Vandekerkhove, G.; Lavoie, J.-M.; Annala, M.; Murtha, A.J.; Sundahl, N.; Walz, S.; Sano, T.; Taavitsainen, S.; Ritch, E.; Fazli, L.; et al. Plasma CtDNA Is a Tumor Tissue Surrogate and Enables Clinical-Genomic Stratification of Metastatic Bladder Cancer. Nat. Commun. 2021, 12, 184. [Google Scholar] [CrossRef]
- Chen, D.S.; Mellman, I. Oncology Meets Immunology: The Cancer-Immunity Cycle. Immunity 2013, 39, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Dunn, G.P.; Bruce, A.T.; Ikeda, H.; Old, L.J.; Schreiber, R.D. Cancer Immunoediting: From Immunosurveillance to Tumor Escape. Nat. Immunol. 2002, 3, 991–998. [Google Scholar] [CrossRef]
- Emens, L.A.; Ascierto, P.A.; Darcy, P.K.; Demaria, S.; Eggermont, A.M.M.; Redmond, W.L.; Seliger, B.; Marincola, F.M. Cancer Immunotherapy: Opportunities and Challenges in the Rapidly Evolving Clinical Landscape. Eur. J. Cancer 2017, 81, 116–129. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).