Reproductive Health Experiences of Females Diagnosed with Young-Onset Colorectal Cancer: A Multi-Method Cross-Sectional Survey
Abstract
1. Introduction
2. Methods
2.1. Participant Recruitment
2.2. Study Design and Data Collection
2.3. Statistical Analysis
2.4. Qualitative Analysis
2.5. Ethical Approval and Consent
3. Results
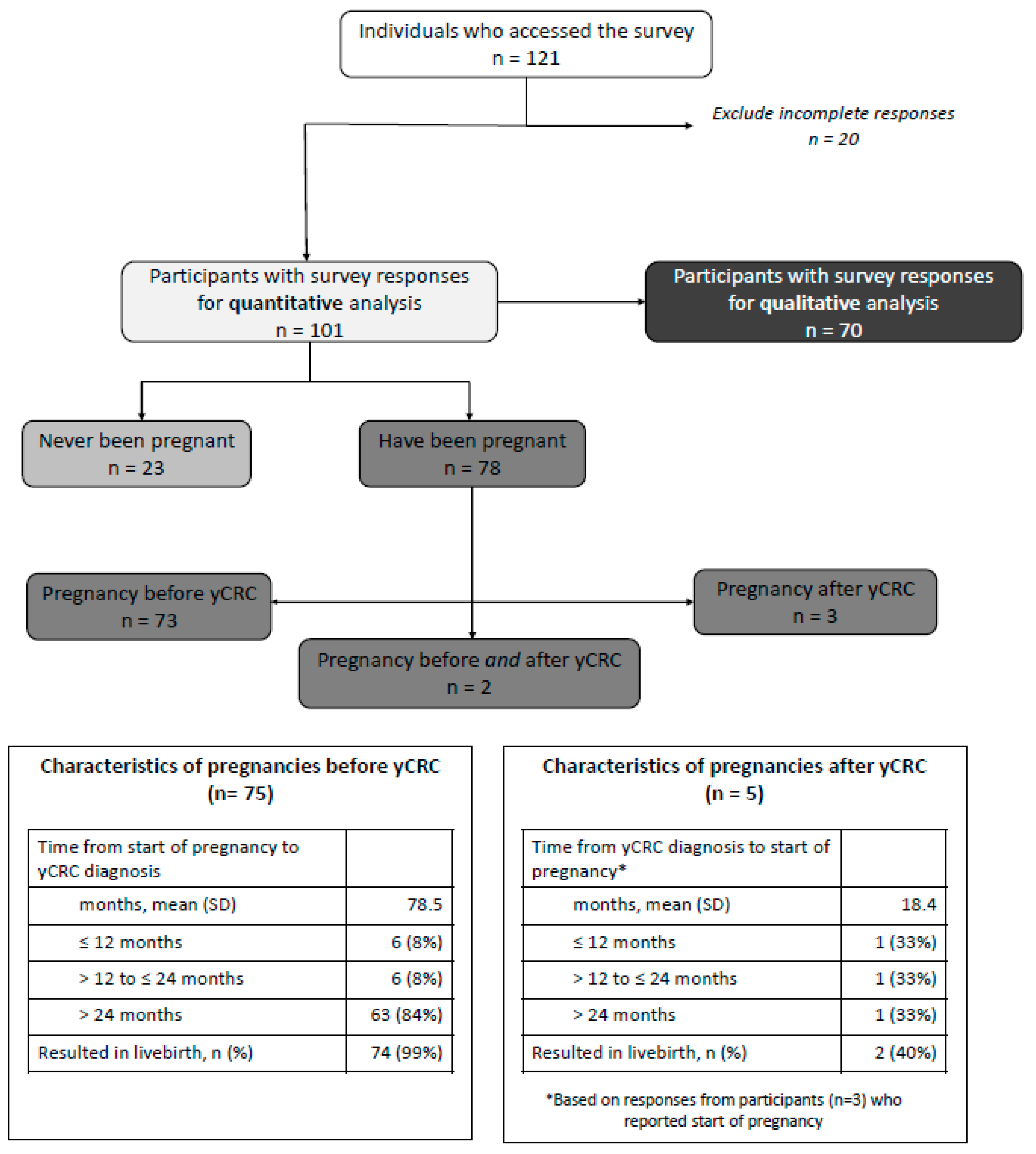
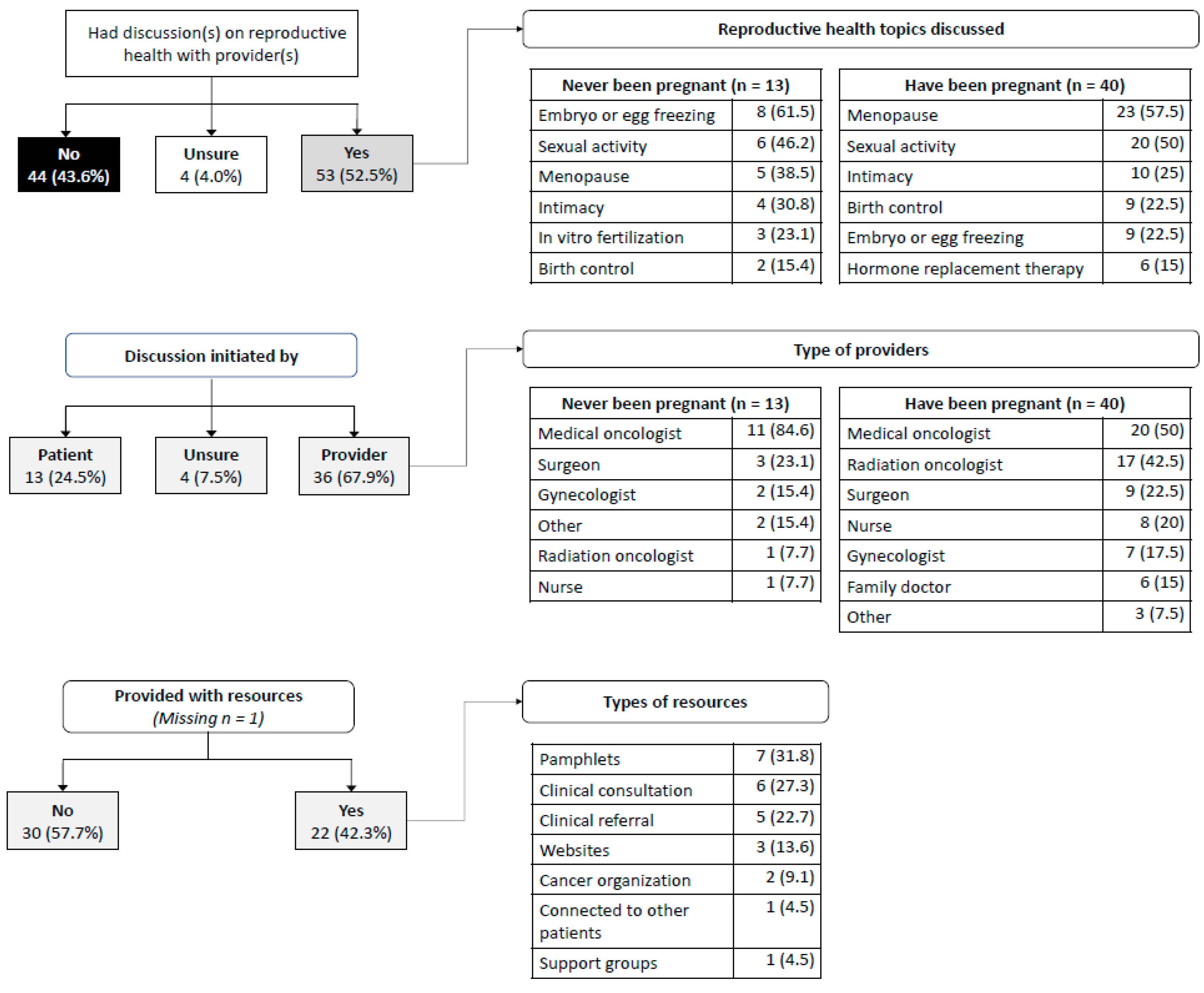
3.1. Experiences with Reproductive Health after yCRC Diagnosis—Quantitative Responses
3.2. Experiences with Reproductive Health after yCRC Diagnosis—Qualitative Responses
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Infertility Definitions and Terminology; World Health Organization: Geneva, Switzerland, 2020; Available online: https://www.who.int/health-topics/infertility#tab=tab_3 (accessed on 1 December 2021).
- Milan, A. Fertility: Fewer Children, Older Moms; Statistics Canada: Ottawa, ON, Canada, 2014; Available online: https://www150.statcan.gc.ca/n1/pub/11-630-x/11-630-x2014002-eng.htm (accessed on 1 December 2021).
- Provencher, C.; Milan, A.; Hallman, S.; D’Aoust, C. Fertility: Overview, 2012 to 2016; Statistics Canada: Ottawa, ON, Canada, 2018; Available online: https://www150.statcan.gc.ca/n1/pub/91-209-x/2018001/article/54956-eng.pdf (accessed on 1 December 2021).
- Khodaverdi, S.; Valeshabad, A.K.; Khodaverdi, M. A case of colorectal cancer during pregnancy: A brief review of the literature. Case Rep. Obstet. Gynecol. 2013, 2013, 626393. [Google Scholar] [CrossRef]
- Parker, S.L.; Tong, T.; Bolden, S.; Wingo, P.A. Cancer Statistics, 1997. CA Cancer J. Clin. 1997, 47, 5–27. [Google Scholar] [CrossRef] [PubMed]
- Abdelsattar, Z.M.; Wong, S.; Regenbogen, S.E.; Jomaa, D.M.; Hardiman, K.M.; Hendren, S. Colorectal cancer outcomes and treatment patterns in patients too young for average-risk screening. Cancer 2016, 122, 929–934. [Google Scholar] [CrossRef]
- Bailey, C.E.; Hu, C.-Y.; You, Y.N.; Bednarski, B.K.; Rodriguez-Bigas, M.A.; Skibber, J.M.; Cantor, S.B.; Chang, G.J. Increasing disparities in the age-related incidences of colon and rectal cancers in the United States, 1975–2010. JAMA Surg. 2015, 150, 17–22. [Google Scholar] [CrossRef] [PubMed]
- You, Y.N.; Yan, X.; Feig, B.W.; Chang, G.J.; Cormier, J.N. Young-onset colorectal cancer: Is it time to pay attention? Arch. Intern. Med. 2012, 172, 287–289. [Google Scholar] [CrossRef] [PubMed]
- Siegel, R.L.; Fedewa, S.A.; Anderson, W.F.; Miller, K.D.; Ma, J.; Rosenberg, P.S.; Jemal, A. Colorectal Cancer Incidence Patterns in the United States, 1974–2013. J. Natl. Cancer Inst. 2017, 109, djw322. [Google Scholar] [CrossRef] [PubMed]
- Siegel, R.L.; Jemal, A.; Ward, E.M. Increase in incidence of colorectal cancer among young men and women in the United States. Cancer Epidemiol. Biomark. Prev. 2009, 18, 1695–1698. [Google Scholar] [CrossRef] [PubMed]
- Din, K.S.E.; Loree, J.M.; Sayre, E.C.; Gill, S.; Brown, C.J.; Dau, H.; De Vera, M.A. Trends in the epidemiology of young-onset colorectal cancer: A worldwide systematic review. BMC Cancer 2020, 20, 288. [Google Scholar]
- Pellino, G.; Simillis, C.; Kontovounisios, C.; Baird, D.L.; Nikolaou, S.; Warren, O.; Tekkis, P.P.; Rasheed, S. Colorectal cancer diagnosed during pregnancy: Systematic review and treatment pathways. Eur. J. Gastroenterol. Hepatol. 2017, 29, 743–753. [Google Scholar] [CrossRef]
- Amarjothi, J.M.V.; Ramasamy, V.; Senthil Kumaran, G.R.; Naganath Babu, O.L. Challenges associated with colorectal cancer in pregnancy. Case Rep. Gastroenterol. 2019, 13, 253–257. [Google Scholar] [CrossRef]
- Jones, A.; Povlow, M.R. Colorectal cancer presenting with constipation during pregnancy. Cureus 2017, 9, e1190. [Google Scholar] [CrossRef]
- Benedict, C.; Thom, B.; Friedman, D.N.; Diotallevi, D.; Pottenger, E.M.; Raghunathan, N.J.; Kelvin, J.F. Young adult female cancer survivors’ unmet information needs and reproductive concerns contribute to decisional conflict regarding posttreatment fertility preservation. Cancer 2016, 122, 2101–2109. [Google Scholar] [CrossRef]
- Canzona, M.R.; Garcia, D.; Fisher, C.L.; Raleigh, M.; Kalish, V.; Ledford, C.J. Communication about sexual health with breast cancer survivors: Variation among patient and provider perspectives. Patient Educ. Couns. 2016, 99, 1814–1820. [Google Scholar] [CrossRef]
- Reese, J.B.; Sorice, K.; Lepore, S.J.; Daly, M.B.; Tulsky, J.A.; Beach, M.C. Patient-clinician communication about sexual health in breast cancer: A mixed-methods analysis of clinic dialogue. Patient Educ. Couns. 2019, 102, 436–442. [Google Scholar] [CrossRef]
- Dau, H.; Saad El Din, K.; McTaggart-Cowan, H.; Loree, J.; Gill, S.; De Vera, M. Health information seeking behaviours amon individuals with young-onset and average-onset colorectal cancer: An international cross-sectional survey. Support. Care Cancer 2020, 28, 6011–6021. [Google Scholar] [CrossRef] [PubMed]
- Araujo, L.; Breau, G.; George, M.; Dau, H.; Gastonguay, L.; Brown, E.H.; De Vera, M.A. Shared experiences of diagnosis and treatment of young-onset colorectal cancer: A patient-oriented qualitative study. J. Psychosoc. Oncol. 2020, 2, e17. [Google Scholar] [CrossRef]
- Dau, H.; Safari, A.; Saad El Din, K.; McTaggart-Cowan, H.; Loree, J.M.; Gill, S.; De Vera, M.A. Assessing how health information needs of individuals with colorectal cancer are met across the care continuum: An international cross-sectional survey. BMC Cancer 2020, 20, 1031. [Google Scholar] [CrossRef] [PubMed]
- Wee, M.; Dau, H.; Gastonguay, L.; De Vera, M.A. How do individuals with colorectal cancer perceive the term “cancer survivor”: A cross-sectional survey. J. Cancer Surviv. 2021, 1–12. [Google Scholar] [CrossRef]
- Elo, S.; Kyngas, H. The qualitative content analysis process. J. Adv. Nurs. 2008, 62, 107–115. [Google Scholar] [CrossRef]
- Brockway-Lunardi, L.; Nelson, S.; Pandiri, A.; Tricoli, J.; Umar, A.; Wali, A.; Daschner, P. Early-onset colorectal cancer research: Gaps and opportunities. Colorectal Cancer 2020, 9, CRC34. [Google Scholar] [CrossRef]
- Lowery, J.; Weber, T.; Ahnen, D.; Schroy, P., III; Levell, C.; Smith, R. An action plan to address the rising burden of colorectal cancer in younger adults. Colorectal Cancer 2020, 9, CRC24. [Google Scholar] [CrossRef]
- Biller, L.; Ng, K. Pioneering a new care model for young-onset colorectal cancer: Innovations in clinical care and scientific discovery. Colorectal Cancer 2020, 9, CRC18. [Google Scholar] [CrossRef]
- Siegel, R. Early-onset colorectal cancer: When hoof beats are zebras. Colorectal Cancer 2020, 9, CRC19. [Google Scholar] [CrossRef]
- O’Neill, M.T.; Ni Dhonnchu, T.; Brannigan, A.E. Topic update: Effects of colorectal cancer treatments on female fertility and potential methods for fertility preservation. Dis. Colon Rectum 2011, 54, 363–369. [Google Scholar] [CrossRef] [PubMed]
- Meirow, D.; Nugent, D. The effects of radiotherapy and chemotherapy on female reproduction. Hum. Reprod. Update 2001, 7, 535–543. [Google Scholar] [CrossRef]
- Rasmussen, S.; Larsen, P.; Sondergaard, J.; Elnegaard, S.; RP, S.; Jarbol, D. Specific and non-specific symptoms of colorectal cancer and contact to general practice. Fam. Pract. 2015, 32, 387–394. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Schover, L. Reproductive complications and sexual dysfunction in cancer survivors. In Cancer Survivorship: Today and Tomorrow; Ganze, P.A., Ed.; Springer: New York, NY, USA, 2007; pp. 251–271. [Google Scholar]
| Characteristic n (%) | Never Been Pregnant (n = 23) | Have Been Pregnant (n = 78) | p-Value a |
|---|---|---|---|
| Current age (years) | |||
| 20–29 | 1 (4.3) | 2 (2.6) | 0.51 |
| 30–39 | 9 (39.1) | 16 (20.5) | |
| 40–49 | 8 (34.8) | 39 (50.0) | |
| 50–59 | 4 (17.4) | 18 (23.1) | |
| 60–69 | 1 (4.3) | 2 (2.6) | |
| 70–79 | 0 | 1 (1.3) | |
| Country | |||
| Canada | 8 (34.8) | 37 (48.7) | 0.15 |
| USA | 10 (43.5) | 32 (42.1) | |
| UK | 1 (4.3) | 4 (5.3) | |
| Other b | 4 (5.1) | 3 (3.9) | |
| Ethnicity | |||
| White | 20 (90.9) | 62 (80.5) | 0.66 |
| Hispanic | 0 | 2 (2.6) | |
| Black | 0 | 2 (2.6) | |
| Asian | 0 | 6 (7.8) | |
| Native/Aboriginal | 0 | 1 (1.3) | |
| Middle Eastern | 0 | 1 (1.3) | |
| Other c | 2 (9.1) | 3 (3.9) | |
| Residence | |||
| Urban | 14 (60.9) | 21 (26.9) | 0.03 |
| Suburban | 6 (26.1) | 41 (52.6) | |
| Rural | 3 (13.0) | 15 (19.2) | |
| Do not know | 0 | 1 (1.3) | |
| Education level | |||
| High school or less | 0 | 5 (6.4) | 0.21 |
| Postsecondary or more | 23 (100) | 73 (93.6) | |
| Marital status | |||
| Married/common-law | 17 (73.9) | 67 (85.9) | <0.0001 |
| Single, never married | 6 (26.1) | 1 (1.3) | |
| Separated/divorced/widowed | 0 | 10 (12.8) | |
| CRC Characteristic n (%) | Never Been Pregnant (n = 23) | Have Been Pregnant (n = 78) | p-Value a |
|---|---|---|---|
| Age at Diagnosis | |||
| 20–29 | 3 (13.0) | 6 (7.8) | 0.50 |
| 30–39 | 11 (47.8) | 28 (36.4) | |
| 40–49 | 9 (39.1) | 43 (55.8) | |
| CRC Type | |||
| Colon | 11 (47.8) | 47 (60.3) | 0.52 |
| Rectal | 11 (47.8) | 27 (34.6) | |
| Both Sites | 1 (4.3) | 4 (5.1) | |
| CRC Stage | |||
| Stage 0 | 0 | 3 (3.8) | 0.67 |
| Stage I | 1 (4.3) | 3 (3.8) | |
| Stage II | 6 (26.1) | 10 (12.8) | |
| Stage III | 11 (47.8) | 41 (52.6) | |
| Stage IV | 4 (17.4) | 18 (23.1) | |
| Do not know | 1 (4.3) | 3 (3.8) | |
| Treatment Status | |||
| In treatment | 7 (30%) | 17 (22%) | 0.41 |
| Completed treatment | 16 (70%) | 61 (78%) | |
| Number of Treatment Modalities | |||
| More than one | 18 (78.3) | 72 (92.3) | 0.16 |
| One | 4 (17.4) | 5 (6.4) | |
| None | 1 (4.3) | 1 (1.3) | |
| Treatment Type b,c | |||
| Chemotherapy | 21 (91.3) | 70 (89.7) | 0.83 |
| Surgery | 19 (82.6) | 72 (92.3) | 0.17 |
| Radiation | 7 (30.4) | 35 (44.9) | 0.22 |
| Immunotherapy | 0 | 7 (9.0) | 0.14 |
| None | 1 (4.3) | 1 (1.3) | 0.35 |
| Symptoms experienced b,c | |||
| Blood in the stool | 15 (65.2) | 53 (67.9) | 0.81 |
| Gas, cramps, feeling bloated | 10 (43.5) | 39 (50.0) | 0.58 |
| Narrow stool | 9 (39.1) | 33 (42.3) | 0.79 |
| Weakness or fatigue | 9 (39.1) | 30 (38.5) | 0.95 |
| Constipation | 8 (34.8) | 19 (24.4) | 0.32 |
| Bowel obstruction | 8 (34.8) | 9 (11.5) | 0.009 |
| Diarrhea | 7 (30.4) | 24 (30.8) | 0.98 |
| Weight loss | 7 (30.4) | 20 (25.6) | 0.65 |
| Pain in the abdomen, back, buttocks, or legs | 7 (30.4) | 16 (20.5) | 0.32 |
| Anemia | 6 (26.1) | 31 (39.7) | 0.23 |
| Nausea or vomiting | 6 (26.1) | 11 (14.1) | 0.18 |
| Loss of appetite | 5 (21.7) | 11 (14.1) | 0.38 |
| Bleeding from the rectum | 4 (17.4) | 21 (26.9) | 0.35 |
| Rectal pain or discomfort | 4 (17.4) | 15 (19.2) | 0.84 |
| Other | 1 (4.3) | 9 (11.5) | 0.31 |
| Lump in the abdomen or rectum | 1 (4.3) | 6 (8.0) | 0.58 |
| Fluid buildup in the abdomen | 1 (4.3) | 4 (5.1) | 0.88 |
| Swollen lymph nodes | 1 (4.3) | 2 (2.6) | 0.66 |
| Trouble breathing | 0 | 4 (5.1) | 0.27 |
| Enlarged liver | 0 | 3 (3.8) | 0.34 |
| None | 0 | 1 (1.3) | 0.59 |
| Odds Ratio * (95% Confidence Interval) | |
|---|---|
| Age at yCRC diagnosis ** | |
| 40–49 year (ref) | |
| 30–39 year | 21.94 (5.59, 86.18) |
| 20–29 year | 22.73 (3.53, 146.39) |
| Cancer site | |
| Colon (ref) | |
| Rectum | 0.63 (0.20, 1.98) |
| Both sites | 5.06 (0.34, 74.61) |
| Treatment status ** | |
| Completed treatment (ref) | |
| In treatment | 4.93 (1.29, 18.78) |
| Had discussion with provider(s) | |
| No (ref) | |
| Yes | 1.27 (0.43, 3.74) |
| Unsure | 0.33 (0.012, 8.85) |
| Education | |
| College or more (ref) | |
| Less than college | 2.03 (0.19, 21.85) |
| Themes | Categories | Participant-Mentions N (%) | Representative Quote(s) |
|---|---|---|---|
| Emotional impacts of yCRC | (a) Processing diagnosis | 4 (5.7) | “My greatest concern, when diagnosed, was will I live through this?” (40–49, never been pregnant) “[The diagnosis] made us realize how precious life is.” (40–49, have been pregnant) “You go into immediate fight mode.” (40–49, have been pregnant) |
| (b) Worries and fears | 7 (10.0) | “The thought of having a cancer recurrence with a family scares me.” (20–29, never been pregnant) “I am in fear of my future.” (30–39, have been pregnant) “I no longer feel attractive.” (40–49, have been pregnant) | |
| (c) Coping strategies | 3 (4.3) | “I took my first surgeon’s advice and looked at my treatment one step at a time.” (40–49, have been pregnant) “When looked at by each step, [treatment] is so very much easier to deal with.” (40–49, have been pregnant) “I feel my positive attitude helped me a lot.” (40–49, have been pregnant) | |
| Experiences with reproductive healthcare after yCRC diagnosis | (a) Did not have a discussion with healthcare providers | 10 (14.3) | “No discussion was ever had … [I] was not given any information, so anything would’ve been good.” (20–29, have been pregnant) “There was really no discussions about reproductive health at the beginning.” (40–49, have been pregnant) “Doctors need to be more proactive with discussing fertility-preservation.” (20–29, never been pregnant) |
| (b) Received referral for reproductive healthcare | 2 (2.9) | “Referred me to a fertility specialist.” (40–49, never been pregnant) “Refer to gynec re: menopause after treatment ends.” (40–49, have been pregnant) | |
| (c) Had a discussion with healthcare providers | 9 (12.9) | “They only mention that there may be some pain and discharge.” (40–49, have been pregnant) “I was well informed.” (30–39, have been pregnant) “I went through menopause and needed info about this, which my Dr. provided.” (30–39, have been pregnant) | |
| (a) Online resources | 2 (2.9) | “I found online forums to be a huge help in this area.” (40–49, have been pregnant) “[I] have had to turn to online resources.” (40–49, have been pregnant) | |
| Reproductive and family planning considerations with yCRC diagnosis | (a) Pregnancy history | 33 (47.2) | “I have two healthy children who were conceived prior to the cancer diagnosis and treatment.” (30–39, have been pregnant) “I had 1 teenage child and one adult child at the time of diagnosis.” (40–49, have been pregnant) |
| (a) Impact of yCRC on decisions to have children | 19 (27.1) | “After so much surgery and invasion of my body the thought of giving birth or being pregnant makes me feel dread rather than any sense of excitement.” (30–39, never been pregnant) “I was done with ever being pregnant again but the possibility of adopting was on the table. Now, I’m not sure that is a good idea.” (30–39, have been pregnant) “I’ve been unsure if I wanted kids but I think my health has pushed me towards not having children.” (30–39, never been pregnant) | |
| (b) Role of genetic testing | 8 (11.4) | “I was later diagnosed with Lynch syndrome a and had a full hysterectomy.” (40–49, have been pregnant) “I was able to reflect and confirmed my belief that I would not want children in the future, especially now, given the diagnosis and genetic mutation I am carrying.” (20–29, never been pregnant) | |
| (c) Fertility | 5 (7.1) | “I wish I had been given options to preserve some eggs in case I wanted children in the future.” (20–29, have been pregnant) “In general, there is no solid information about the effects of chemo on fertility. Dr’s said it was an unknown.” (30–39, have been pregnant) “I wish a longer discussion and basic overview of my reproductive health was done.” (30–39, have been pregnant) | |
| Sexual health impacts of yCRC | (a) Vaginal side effects | 8 (11.4) | “Vaginal damage was downplayed.” (40–49, have been pregnant) “I also experienced issues with vaginal stenosis. My doctors never informed me about this long term side effect from the treatments.” (20–29, never been pregnant) “Vaginal changes after radiation being severe.” (30–39, have been pregnant) |
| (b) Intimacy and intercourse | 5 (7.1) | “During and after treatment my interest intimacy was affected and my partner did not understand this, so it would have been good to have some type of counselling as a couple on this topic.” (30–39, have been pregnant) “How difficult sex would be afterwards.” (40–49, have been pregnant) “I did not really digest how this would impact my intimate relationship with my husband.” (40–49, have been pregnant) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Araujo, L.; Rebic, N.; Dau, H.; Brotto, L.; George, M.; De Vera, M.A. Reproductive Health Experiences of Females Diagnosed with Young-Onset Colorectal Cancer: A Multi-Method Cross-Sectional Survey. Curr. Oncol. 2022, 29, 465-478. https://doi.org/10.3390/curroncol29020042
Araujo L, Rebic N, Dau H, Brotto L, George M, De Vera MA. Reproductive Health Experiences of Females Diagnosed with Young-Onset Colorectal Cancer: A Multi-Method Cross-Sectional Survey. Current Oncology. 2022; 29(2):465-478. https://doi.org/10.3390/curroncol29020042
Chicago/Turabian StyleAraujo, Louise, Nevena Rebic, Hallie Dau, Lori Brotto, Manju George, and Mary A. De Vera. 2022. "Reproductive Health Experiences of Females Diagnosed with Young-Onset Colorectal Cancer: A Multi-Method Cross-Sectional Survey" Current Oncology 29, no. 2: 465-478. https://doi.org/10.3390/curroncol29020042
APA StyleAraujo, L., Rebic, N., Dau, H., Brotto, L., George, M., & De Vera, M. A. (2022). Reproductive Health Experiences of Females Diagnosed with Young-Onset Colorectal Cancer: A Multi-Method Cross-Sectional Survey. Current Oncology, 29(2), 465-478. https://doi.org/10.3390/curroncol29020042




