Clinical Management of Financial Toxicity–Identifying Opportunities through Experiential Insights of Cancer Survivors, Caregivers, and Social Workers
Abstract
:1. Introduction
2. Materials and Methods
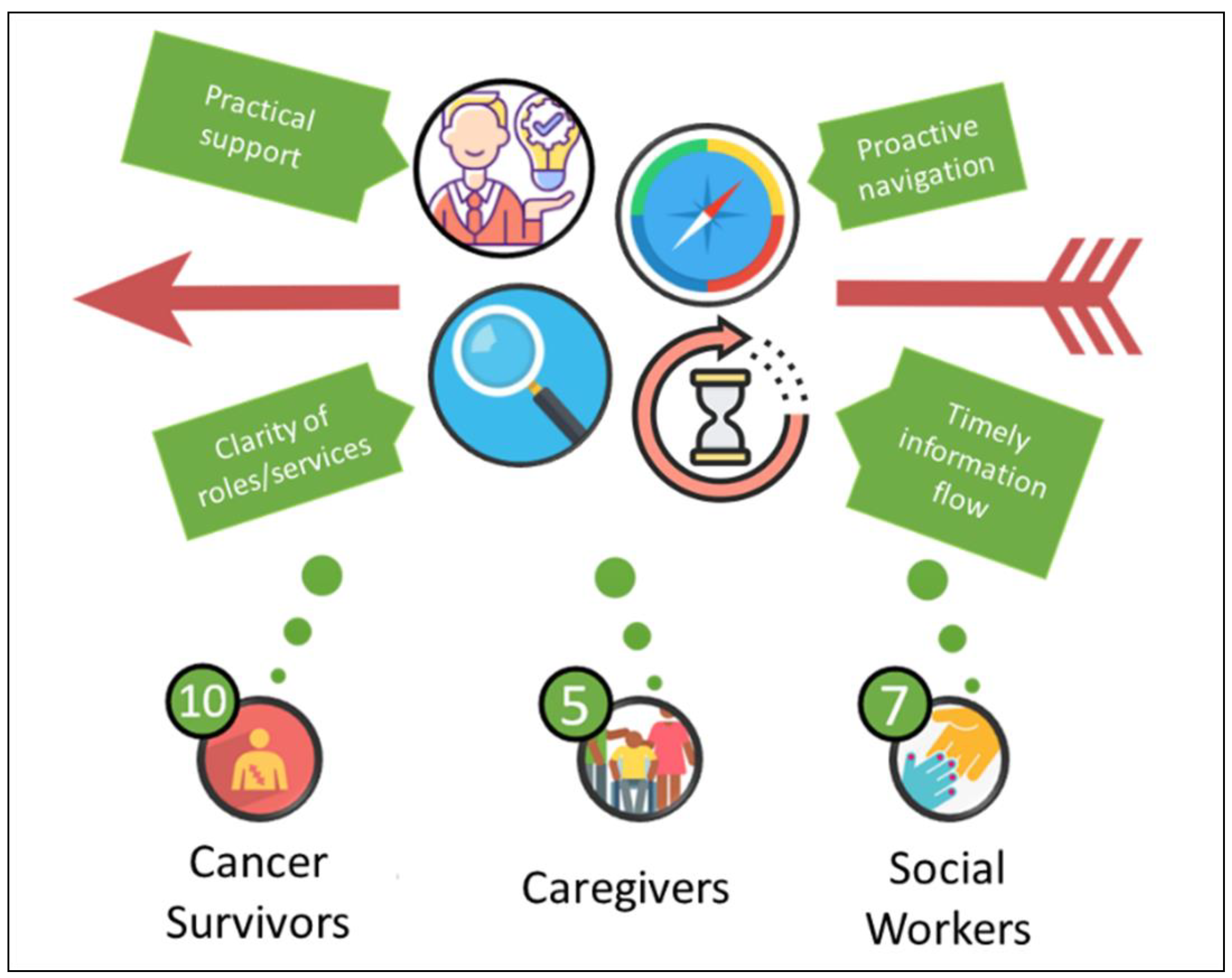
2.1. Participants
2.2. Setting
2.3. Procedure
2.4. Procedure
2.5. Data Analysis
3. Results
3.1. Genuine Concern through Practical Support
3.2. Need for Clarity of Roles and Services
3.3. Importance of Timely Information Flow
3.4. Proactive Navigation as a Priority
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. Interview Guide (Patient Version)
- Tell me about any financial issues you have experienced since the diagnosis of your cancer/since your cancer have come back/since the diagnosis of your most recent cancer?
- Potential subsequent prompts (if applicable):
- Describe your experience and your feelings associated with these issues/events
- How did this affect you, your partner, carer or your family?
- Did you have any finance-related concerns with regards to your cancer treatment? If so, what were they?
- Could you comment on your access to insurance and financial services (i.e., dealings with insurance and insurers, access to financial services, financial advice, loans etc.)
- What guidance or assistance did you receive (and from who)? Were they useful? If not, why not?
- What assistance, care or guidance would have been useful for the circumstance(s) you described above?
- At what point of time would be useful for you/your carers to receive them?
- Do you have any preference with regards to who you would like to receive the assistance or guidance from?
- 2.
- Have you had any employment issues/loss of income since the diagnosis of your cancer/since your cancer have come back/since the most recent diagnosis of your recent cancer?
- Potential subsequent prompts (if applicable):
- How have these issues affected you, your partner, carer or your family/loved ones, your employers and your colleagues? In what way?
- Did you have a return-to-work plan? Tell me more about the plan.
- Have you experienced any challenges in returning to work? What were these challenges? And how have you gone about to overcome these challenges?
- Were there any symptoms or health concerns that restrict your ability to perform your duties at work? If so, what were they?
- What assistance, care or guidance would have been useful for the circumstance(s) you described above?
- At what point of time would be useful for you/your carers to receive them?
- Do you have any preference with regards to timing and who you would like to receive the assistance or guidance from?
- With all the issues/costs discussed above, were there any issues that are not specific to your cancer diagnosis or treatment? (i.e., you believe you would be experiencing that anyway with or without your cancer diagnosis)
- 3.
- Have you had any out-of-pocket costs for your cancer diagnosis and treatment?
- Potential subsequent prompts:
- Throughout the course of your illness, what were the expected and unexpected costs related to your cancer and cancer treatment?
- Consider medications, GP, hospitalisations, medical tests, parking, transport, accommodation, home/selfcare assistance, medical equipment (name specific depending on care type) and supplies, home modification, health foods, complementary or alternative medicine, childcare
- Did you require any travel and/or accommodation arrangements? How did you navigate through that process? Was any assistance provided to you? Was it useful? If not, why not?
- With all the issues/costs discussed above, were there any issues that are not specific to your cancer diagnosis or treatment? (i.e., you believe you would be experiencing that anyway with or without your cancer diagnosis)
- 4.
- Is there anything you would like to add to what we have discussed so far.
Appendix B. Interview Guide (Carer Version)
- * Insert the patient’s name where applicable.
- Tell me about any financial issues you have experienced since the patient’s diagnosis of your cancer/since the patient’s cancer have come back/since the diagnosis of the patient’s most recent cancer?
- Potential subsequent prompts (if applicable):
- How did this affect the patient, yourself, or your family?
- Did you have any finance-related concerns with regards to the patient’s cancer treatment? If so, what were they?
- Could you comment on your experience with regards to accessing insurance and financial services for the patient or your family? (i.e., dealings with insurance and insurers, access to financial services, financial advice, loans etc.)
- Have you/did you receive any guidance or assistance did you or the patient receive (and from who)? Were they useful? If not, why not?
- What assistance, care or guidance would have been useful for the circumstance(s) you described above?
- At what point of time would be useful for the patient or you to receive them?
- Do you have any preference with regards to who you would like to receive the assistance or guidance from?
- 2.
- Have you had any employment issues/loss of income since the patient’s diagnosis of your cancer/since the patient’s cancer have come back/since the diagnosis of the patient’s most recent cancer?
- Potential subsequent prompts (if applicable):
- How have these issues affected the patient, or your family/loved ones, your employers and your colleagues? In what way?
- Have you experienced any challenges in your own work? What were these challenges? And how have you gone about to overcome these challenges?
- How did caring for the patient limit your ability work? Tell me more about that.
- What assistance, care or guidance would have been useful for the circumstance(s) you described above?At what point of time would be useful for you/your carers to receive them?
- Do you have any preference with regards to timing and who you would like to receive the assistance or guidance from?
- With all the issues/costs discussed above, were there any issues that are not specific to the patient’s cancer diagnosis or treatment? (i.e., you believe you would be experiencing that anyway with or without the patient’s cancer diagnosis)
- 3.
- Have you had any out-of-pocket costs for the patient’s cancer diagnosis and treatment?
- Potential subsequent prompts:
- Throughout the course of the patient’s illness, what were the expected and unexpected costs related to the patient’s cancer and cancer treatment?
- ◦
- Consider medications, GP, hospitalisations, medical tests, parking, transport, accommodation, home/selfcare assistance, medical equipment (name specific depending on care type) and supplies, home modification, health foods, complementary or alternative medicine, childcare
- What were the travel and/or accommodation arrangements? How did you navigate through that process? Was any assistance provided to the patient or yourself? Was it useful? If not, why not?
- With all the issues/costs discussed above, were there any issues that are not specific to the patient’s cancer diagnosis or treatment? (i.e., you believe you would be experiencing that anyway with or without the patient’s cancer diagnosis)
- 4.
- In light of what have been discussed, is there any care you believe would very helpful for carers? What are they?
- 5.
- Is there anything you would like to add to what we have discussed so far. What are they?
References
- Yabroff, K.R.; Lawrence, W.F.; Clauser, S.; Davis, W.W.; Brown, M.L. Burden of illness in cancer survivors: Findings from a population-based national sample. J. Natl. Cancer Inst. 2004, 96, 1322–1330. [Google Scholar] [CrossRef] [PubMed]
- Altice, C.K.; Banegas, M.P.; Tucker-Seeley, R.D.; Yabroff, K.R. Financial Hardships Experienced by Cancer Survivors: A Systematic Review. JNCI J. Natl. Cancer Inst. 2016, 109, djw205. [Google Scholar] [CrossRef] [PubMed]
- Gordon, L.G.; Merollini, K.M.D.; Lowe, A.; Chan, R.J. A Systematic Review of Financial Toxicity Among Cancer Survivors: We Can’t Pay the Co-Pay. Patient 2017, 10, 295–309. [Google Scholar] [CrossRef] [Green Version]
- Longo, C.J.; Fitch, M.I.; Banfield, L.; Hanly, P.; Yabroff, K.R.; Sharp, L. Financial toxicity associated with a cancer diagnosis in publicly funded healthcare countries: A systematic review. Support. Care Cancer 2020, 28, 4645–4665. [Google Scholar] [CrossRef] [PubMed]
- Delgado-Guay, M.; Ferrer, J.; Rieber, A.G.; Rhondali, W.; Tayjasanant, S.; Ochoa, J.; Cantu, H.; Chisholm, G.; Williams, J.; Frisbee-Hume, S.; et al. Financial Distress and Its Associations With Physical and Emotional Symptoms and Quality of Life Among Advanced Cancer Patients. Oncologist 2015, 20, 1092–1098. [Google Scholar] [CrossRef] [Green Version]
- Fenn, K.M.; Evans, S.; McCorkle, R.; DiGiovanna, M.P.; Pusztai, L.; Sanft, T.; Hofstatter, E.W.; Killelea, B.K.; Knobf, M.T.; Lannin, D.R.; et al. Impact of financial burden of cancer on survivors’ quality of life. J. Oncol. Pract. 2014, 10, 332–338. [Google Scholar] [CrossRef]
- Chan, R.; Cooper, B.; Paul, S.; Conley, Y.; Kober, K.; Koczwara, B.; Chan, A.; Tan, C.J.; Gordon, L.; Thomy, L.; et al. Distinct financial distress profiles in patients with breast cancer prior to and for 12 months following surgery. BMJ Support. Palliat. Care 2020, in press. [Google Scholar] [CrossRef] [PubMed]
- Chan, R.J.; Cooper, B.; Koczwara, B.; Chan, A.; Tan, C.J.; Paul, S.M.; Dunn, L.B.; Conley, Y.P.; Kober, K.M.; Levine, J.D.; et al. A longitudinal analysis of phenotypic and symptom characteristics associated with inter-individual variability in employment interference in patients with breast cancer. Support. Care Cancer 2019. Epub ahead of printing. [Google Scholar] [CrossRef] [Green Version]
- Chan, R.J.; Button, E.; Thomas, A.; Gates, P.; Yates, P. Nurses attitudes and practices towards provision of survivorship care for people with a haematological cancer on completion of treatment. Support. Care Cancer 2018, 26, 1401–1409. [Google Scholar] [CrossRef]
- Chan, R.J.; Gordon, L.G.; Tan, C.J.; Chan, A.; Bradford, N.K.; Yates, P.; Agbejule, O.A.; Miaskowski, C. Relationships Between Financial Toxicity and Symptom Burden in Cancer Survivors: A Systematic Review. J. Pain Symptom Manag. 2019, 57, 646–660. [Google Scholar] [CrossRef]
- Aranda, S.; Currow, D. Financial toxicity in clinical care today: A “menu without prices”. Med. J. Aust. 2016, 205, 529–530. [Google Scholar] [CrossRef] [PubMed]
- Gordon, L.G.; Chan, R.J. Financial Toxicity Among Patients With Cancer-Where to From Here? Cancer Nurs. 2017, 40, 257–258. [Google Scholar] [CrossRef] [PubMed]
- Carrera, P.M.; Kantarjian HMBlinder, V.S. The financial burden and distress of patients with cancer: Understanding and stepping-up action on the financial toxicity of cancer treatment. CA Cancer J. Clin. 2018, 68, 153–165. [Google Scholar] [CrossRef]
- Koczwara, B. Unemployment after cancer—A hidden driver of financial toxicity. Cancer Forum. 2017, 41, 36–41. [Google Scholar]
- Chan, R.J.; Gordon, L.; Zafar, S.Y.; Miaskowski, C. Financial toxicity and symptom burden: What is the big deal? Support. Care Cancer 2018, in press. [Google Scholar] [CrossRef] [Green Version]
- Zhu, Z.; Xing, W.; Zhang, X.; Hu, Y.; So, W.K.W. Cancer survivors’ experiences with financial toxicity: A systematic review and meta-synthesis of qualitative studies. Psycho-Oncology 2020, 29, 945–959. [Google Scholar] [CrossRef]
- Tsianakas, V.; Robert, G.; Maben, J.; Richardson, A.; Dale, C.; Wiseman, T. Implementing patient-centred cancer care: Using experience-based co-design to improve patient experience in breast and lung cancer services. Support. Care Cancer 2012, 20, 2639–2647. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Green, T.; Bonner, A.; Teleni, L.; Bradford, N.; Purtell, L.; Douglas, C.; Yates, P.; MacAndrew, M.; Dao, H.Y.; Chan, R.J. Use and reporting of experience-based codesign studies in the healthcare setting: A systematic review. BMJ Qual. Saf. 2020, 29, 64–76. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Australian Association of Social Workers. Case Management & Care Coordination; Royal Melbourne Hospital: Melbourne, VIC, Australia, 2015. [Google Scholar]
- Australian Association of Social Workers. Hospital Social Work; Royal Melbourne Hospital: Melbourne, VIC, Australia, 2016. [Google Scholar]
- Vardy, J.L.; Chan, R.; Koczwara, B.; Lisy, K.; Cohn, R.J.; Joske, D.; Dhillon, H.M.; Jefford, M. Clinical Oncology Society of Australia position statement on cancer survivorship care. Aust. J. Gen. Pract. 2019, 48, 833–836. [Google Scholar] [CrossRef] [Green Version]
- Patton, M. Qualitative Research & Evaluation Methods, 3rd ed.; Sage Publications: Saint Paul, MN, USA, 2002. [Google Scholar]
- Sandelowski, M. Whatever happened to qualitative description? Res. Nurs. Health 2000, 23, 334–340. [Google Scholar] [CrossRef]
- Tong, A.; Sainsbury, P.; Craig, J. Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int. J. Qual. Health Care 2007, 19, 349–357. [Google Scholar] [CrossRef]
- Creswell, J.W. Qualitative Inquiry and Research Design: Choosing among Five Traditions; Sage Publications: Thousand Oaks, CA, USA, 1998. [Google Scholar]
- Hennink, M.; Kaiser, B.N. Sample sizes for saturation in qualitative research: A systematic review of empirical tests. Soc. Sci. Med. 2022, 292, 114523. [Google Scholar] [CrossRef]
- Johnson, L.J.; Lamontagne, M.J. Using Content-Analysis to Examine the Verbal or Written Communication of Stakeholders within Early Intervention. J. Early Interv. 1993, 17, 73–79. [Google Scholar] [CrossRef]
- Silverman, D. Interpreting Qualitative Data, 5th ed.; SAGE Publications: London, UK, 2014. [Google Scholar]
- Meropol, N.J.; Schrag, D.; Smith, T.J.; Mulvey, T.M.; Langdon, R.M.; Blum, D.; Ubel, P.A.; Schnipper, L.E. American Society of Clinical Oncology guidance statement: The cost of cancer care. J. Clin. Oncol. 2009, 27, 3868–3874. [Google Scholar] [CrossRef] [Green Version]
- Cancer Council Australia. Standard for Informed Financial Consent; Cancer Council Australia: Sydney, NSW, Australia, 2020. [Google Scholar]
- Basch, E.; Deal, A.M.; Dueck, A.C.; Scher, H.I.; Kris, M.G.; Hudis, C.; Schrag, D. Overall Survival Results of a Trial Assessing Patient-Reported Outcomes for Symptom Monitoring During Routine Cancer Treatment. JAMA 2017, 318, 197–198. [Google Scholar] [CrossRef] [Green Version]
- Chan, R.; Gordon, L. Screening for financial toxicity in clinical care with finance-related outcomes measures. Cancer Nurs. 2021, in press. [Google Scholar] [CrossRef]
- Yezefski, T.; Steelquist, J.; Watabayashi, K.; Sherman, D.; Shankaran, V. Impact of trained oncology financial navigators on patient out-of-pocket spending. Am. J. Manag. Care 2018, 24, S74–S79. [Google Scholar]
- Monak, M.; Bell, K.; Whitt, A. Development of a financial navigation program to ease the burden of financial toxicity. J. Clin. Oncol. 2019, 37, 6565. [Google Scholar] [CrossRef]
- Banegas, M.P.; Dickerson, J.F.; Friedman, N.L.; Mosen, D.; Ender, A.X.; Chang, T.R.; Runge, T.A.; Hornbrook, M.C. Evaluation of a Novel Financial Navigator Pilot to Address Patient Concerns about Medical Care Costs. Perm. J. 2019, 23, 18–84. [Google Scholar] [CrossRef] [Green Version]
- Chan, A.; Ashbury, F.; Fitch, M.I.; Koczwara, B.; Chan, R.J.; On behalf of the MASCC Survivorship Study Group. Cancer survivorship care during COVID-19-perspectives and recommendations from the MASCC survivorship study group. Support. Care Cancer 2020, 28, 3485–3488. [Google Scholar] [CrossRef]
- Emery, J.D.; Jefford, M.; King, M.; Hayne, D.; Martin, A.; Doorey, J.; Hyatt, A.; Habgood, E.; Lim, T.; Hawks, C.; et al. ProCare Trial: A phase II randomized controlled trial of shared care for follow-up of men with prostate cancer. BJU Int. 2017, 119, 381–389. [Google Scholar] [CrossRef]
| Cancer Survivor (n = 10) | Caregiver (n = 5) | |
|---|---|---|
| N (%) | N (%) | |
| Age 40–49 50–59 60–69 70–79 | 3 (30) 4 (40) 1 (10) 2 (20) | 3 (60) 1 (20) 0 1 (20) |
| Sex Female Male | 6 (60) 4 (40) | 4 (80) 1 (20) |
| Diagnosis Central Nervous System Breast Head and Neck Genitourinary Leukaemia | 1 (10) 2 (20) 2 (20) 2 (20) 3 (30) | N/A |
| Partnered versus non-partnered Partnered Non-Partnered | 4 (40) 6 (50) | 4 (80) 1 (20) |
| Highest qualification Lower than high school Completed high school Completed vocational training Completed university degree and above | 3 (30) 2 (20) 4 (40) 1 (10) | 1 (20) 2 (40) 0 2 (40) |
| Currently working for pay Yes No | 4 (33) 8 (66) | 3 (60) 2 (40) |
| Household Income (in AUD) ≤29,999 30,000–49,999 50,000–69,999 70,000–89,999 ≥90,000 Prefer not to say | 1 (10) 2 (20) 2 (20) 2 (20) 2 (20) 1 (10) | N/A |
| Social Worker (n = 7) | |
|---|---|
| N (%) | |
| Age 26–35 36–45 46–55 56–65 | 2 (29) 2 (29) 2 (29) 1 (14) |
| Sex Female | 7 (100) |
| Years of Experience in Social Work <5 years 5–10 years 11–20 years | 2 (29) 0 5 (71) |
| Years of Experience in Cancer Care <5 years 5–10 years 11–20 years | 3 (43) 3 (43) 1 (14) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Longo, C.J.; Gordon, L.G.; Nund, R.L.; Hart, N.H.; Teleni, L.; Thamm, C.; Hollingdrake, O.; Crawford-Williams, F.; Koczwara, B.; Ownsworth, T.; et al. Clinical Management of Financial Toxicity–Identifying Opportunities through Experiential Insights of Cancer Survivors, Caregivers, and Social Workers. Curr. Oncol. 2022, 29, 7705-7717. https://doi.org/10.3390/curroncol29100609
Longo CJ, Gordon LG, Nund RL, Hart NH, Teleni L, Thamm C, Hollingdrake O, Crawford-Williams F, Koczwara B, Ownsworth T, et al. Clinical Management of Financial Toxicity–Identifying Opportunities through Experiential Insights of Cancer Survivors, Caregivers, and Social Workers. Current Oncology. 2022; 29(10):7705-7717. https://doi.org/10.3390/curroncol29100609
Chicago/Turabian StyleLongo, Christopher J., Louisa G. Gordon, Rebecca L. Nund, Nicolas H. Hart, Laisa Teleni, Carla Thamm, Olivia Hollingdrake, Fiona Crawford-Williams, Bogda Koczwara, Tamara Ownsworth, and et al. 2022. "Clinical Management of Financial Toxicity–Identifying Opportunities through Experiential Insights of Cancer Survivors, Caregivers, and Social Workers" Current Oncology 29, no. 10: 7705-7717. https://doi.org/10.3390/curroncol29100609
APA StyleLongo, C. J., Gordon, L. G., Nund, R. L., Hart, N. H., Teleni, L., Thamm, C., Hollingdrake, O., Crawford-Williams, F., Koczwara, B., Ownsworth, T., Born, S., Schoonbeek, S., Stone, L., Barrett, C., & Chan, R. J. (2022). Clinical Management of Financial Toxicity–Identifying Opportunities through Experiential Insights of Cancer Survivors, Caregivers, and Social Workers. Current Oncology, 29(10), 7705-7717. https://doi.org/10.3390/curroncol29100609








