Summary
We report the unusual case of a 15-year-old male who experienced transient complete nodal atrioventricular block in combination with left bundle branch block during radiofrequency catheter ablation of a left free wall accessory pathway via a transaortic approach.
Key words: atrioventricular block; bundle branch block; radiofrequency catheter ablation; accessory pathway
Introduction
Radiofrequency (RF) catheter ablation has become a standard treatment in symptomatic patients with Wolff-Parkinson-White syndrome [
1]. In general, this technique is associated with a high success rate and a low complication rate in both adult and pediatric patients [
2,
3,
4]. Although a certain risk of inadvertent atrioventricular block may be associated with RF catheter ablation of right-sided and septal accessory pathways, this complication is rarely observed during RF catheter ablation of left-sided free wall accessory pathways using a transaortic approach [
2,
3,
4]. We report the unusual case of a 15-year-old male experiencing transient complete nodal atrioventricular (AV) block and left bundle branch block (LBBB) during successful RF catheter ablation of a left free wall accessory pathway via a transaortic approach.
Case report descripton
A 15-year-old male with a 3-month history of recurrent tachycardias was referred to our hospital for further evaluation. Although most of the tachycardias were regular, certain episodes were described as irregular. The electrocardiogram (ECG) showed a preexcitation pattern compatible with the presence of Wolff-Parkinson-White syndrome with a left free wall accessory pathway (fig. 1A). During an electrophysiologic study atrial fibrillation with a fast ventricular rate (minimum cycle length 186 ms) was induced. Subsequently, ventricular rate was reduced by intravenous administration of propafenone (70 mg) and sinus rhythm was restored by cardioversion (200 Joule) under sedation with midazolam (4 mg i.v.). During transaortic insertion of a 7 F, 4 mm tip ablation catheter (Marinr™, Medtronic Inc., Minneapolis, MN, USA) orthodromic circus movement tachycardia with a LBBB pattern was induced (fig. 2). Shortly after spontaneous termination of this arrhythmia a change of the QRS morphology suggesting full preexcitation due to blockade of antegrade conduction via the AV node was noted (fig. 3). Because of the imminent risk of recurrent episodes of atrial fibrillation with fast ventricular rates we decided to proceed to RF catheter ablation of the accessory pathway after prophylactic insertion of a right ventricular pacing catheter. Within seconds after the onset of RF energy delivery, complete AV-block with alternating junctional escape rhythm with LBBB aberration and idioventricular rhythm of RBBB pattern was noted (fig. 4). RF energy was discontinued immediately which was followed by restoration of accessory pathway conduction resulting in sinus rhythm with full preexcitation suggesting compromised nodal AV conduction. The second RF burn was, again, followed by complete AV-block with junctional escape rhythm of LBBB pattern. However, after 20 seconds AV conduction via the AV node recovered with residual first degree AV-block and LBBB. Because of recovery of accessory pathway conduction a third RF burn was delivered, leading to sustained interruption of accessory pathway conduction associated with normal AV node conduction and LBBB. After catheter removal, the patient was observed in the cardiac care unit for 12 hours. During this time the LBBB resolved with restoration of normal infranodal conduction and without recurrence of accessory pathway conduction. At a 3-month follow-up visit the patient had remained asymptomatic and the ECG was normal (fig. 1B).
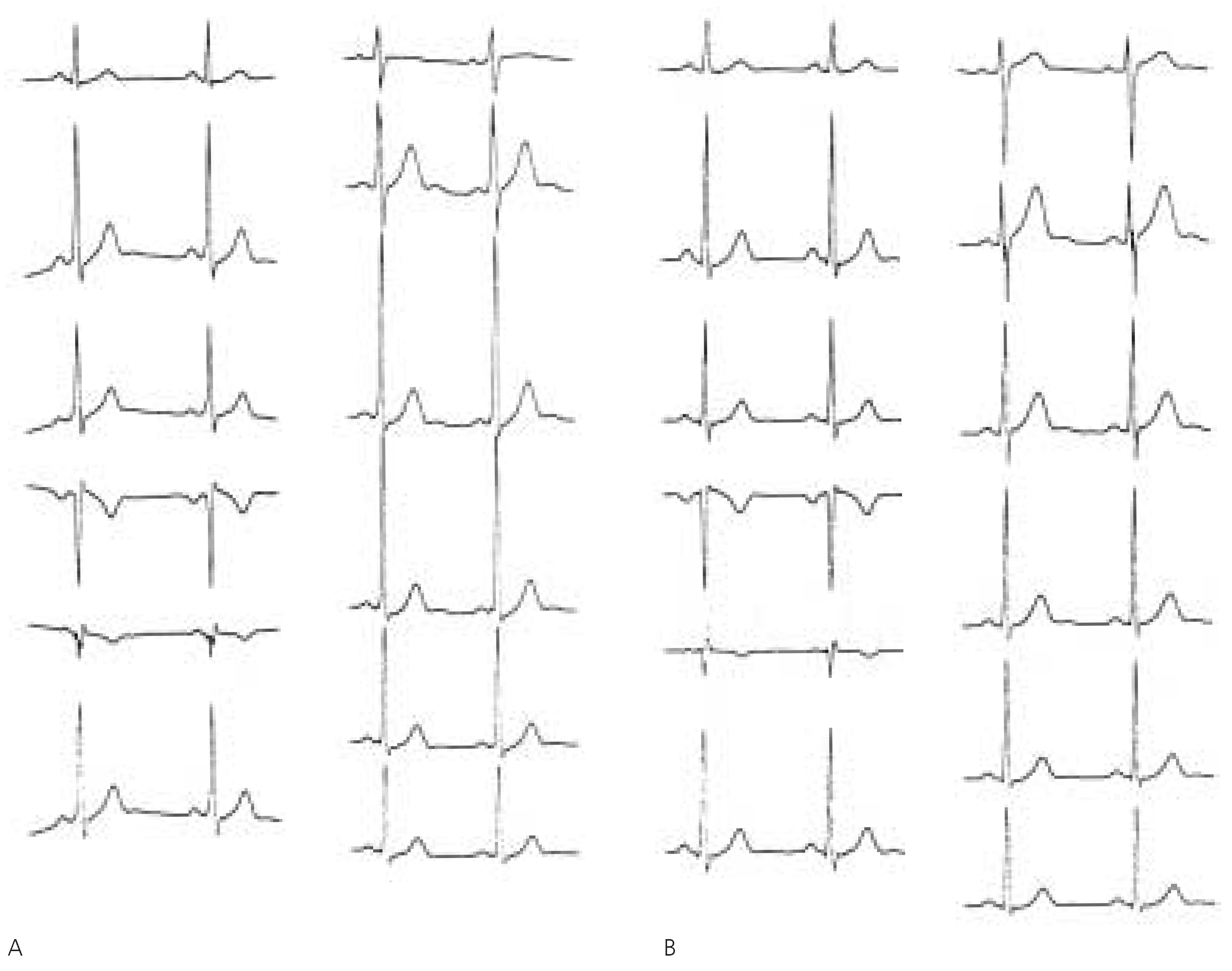
Figure 1.
A 12-lead electrocardiogramm at baseline showing preexcitation compatible with the presence of Wolff-Parkinson-White syndrome with a left free wall accessory pathway. B 12-lead electrocardiogram at 3-month follow-up without evidence of residual intracardiac conduction abnormalities or relapse of accessory pathway conduction.
Figure 1.
A 12-lead electrocardiogramm at baseline showing preexcitation compatible with the presence of Wolff-Parkinson-White syndrome with a left free wall accessory pathway. B 12-lead electrocardiogram at 3-month follow-up without evidence of residual intracardiac conduction abnormalities or relapse of accessory pathway conduction.
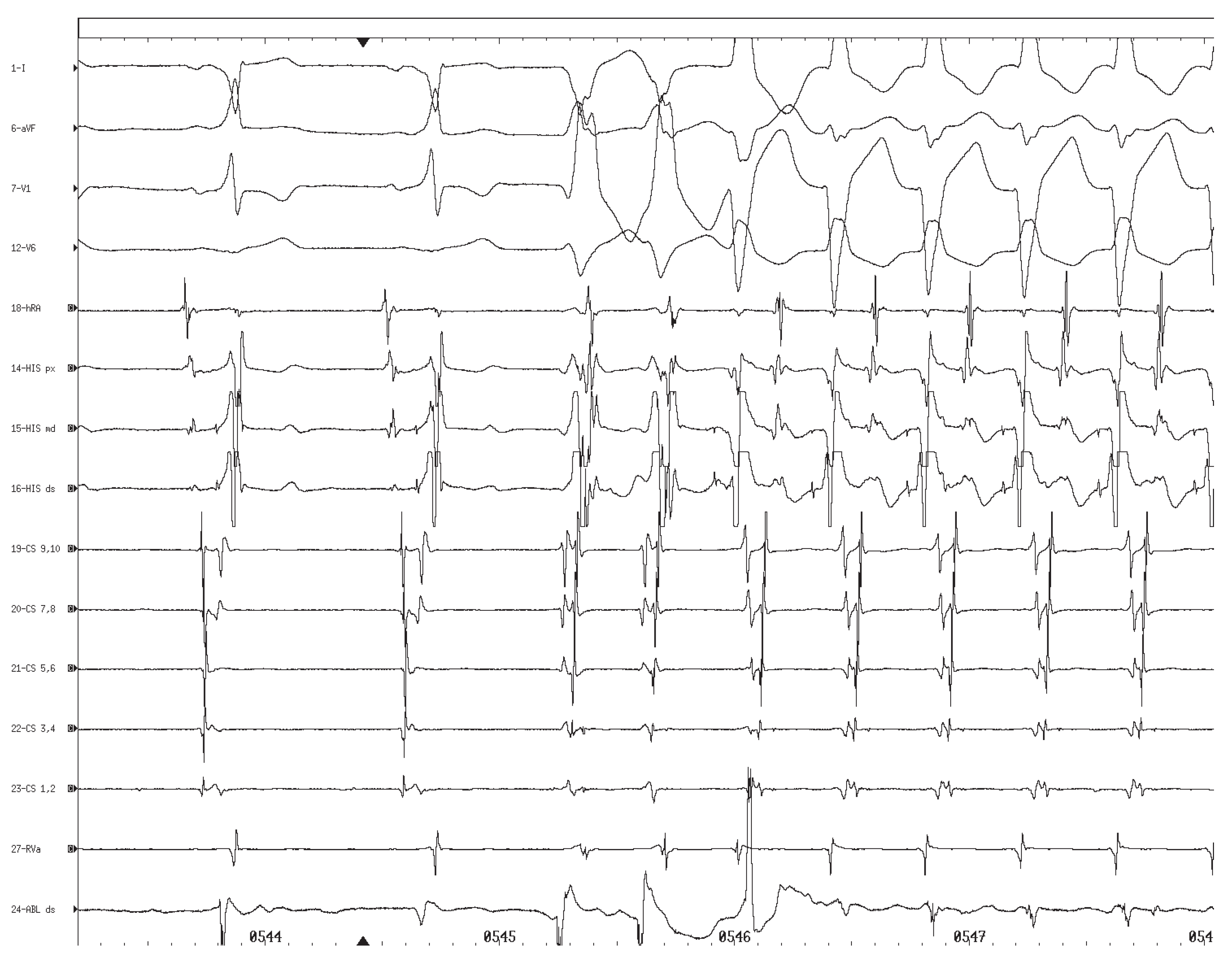
Figure 2.
Induction of orthodromic circus movement tachycardia with left bundle branch block morphology (cycle length 432 ms) by two left ventricular extrasystoles with right bundle branch block morphology.
Figure 2.
Induction of orthodromic circus movement tachycardia with left bundle branch block morphology (cycle length 432 ms) by two left ventricular extrasystoles with right bundle branch block morphology.
Figure 3.
Sinus rhythm with full preexcitation (right bundle branch block morphology and absence of a His potential) suggesting an impairment or blockade of antegrade conduction over the atrioventricular node.
Figure 3.
Sinus rhythm with full preexcitation (right bundle branch block morphology and absence of a His potential) suggesting an impairment or blockade of antegrade conduction over the atrioventricular node.
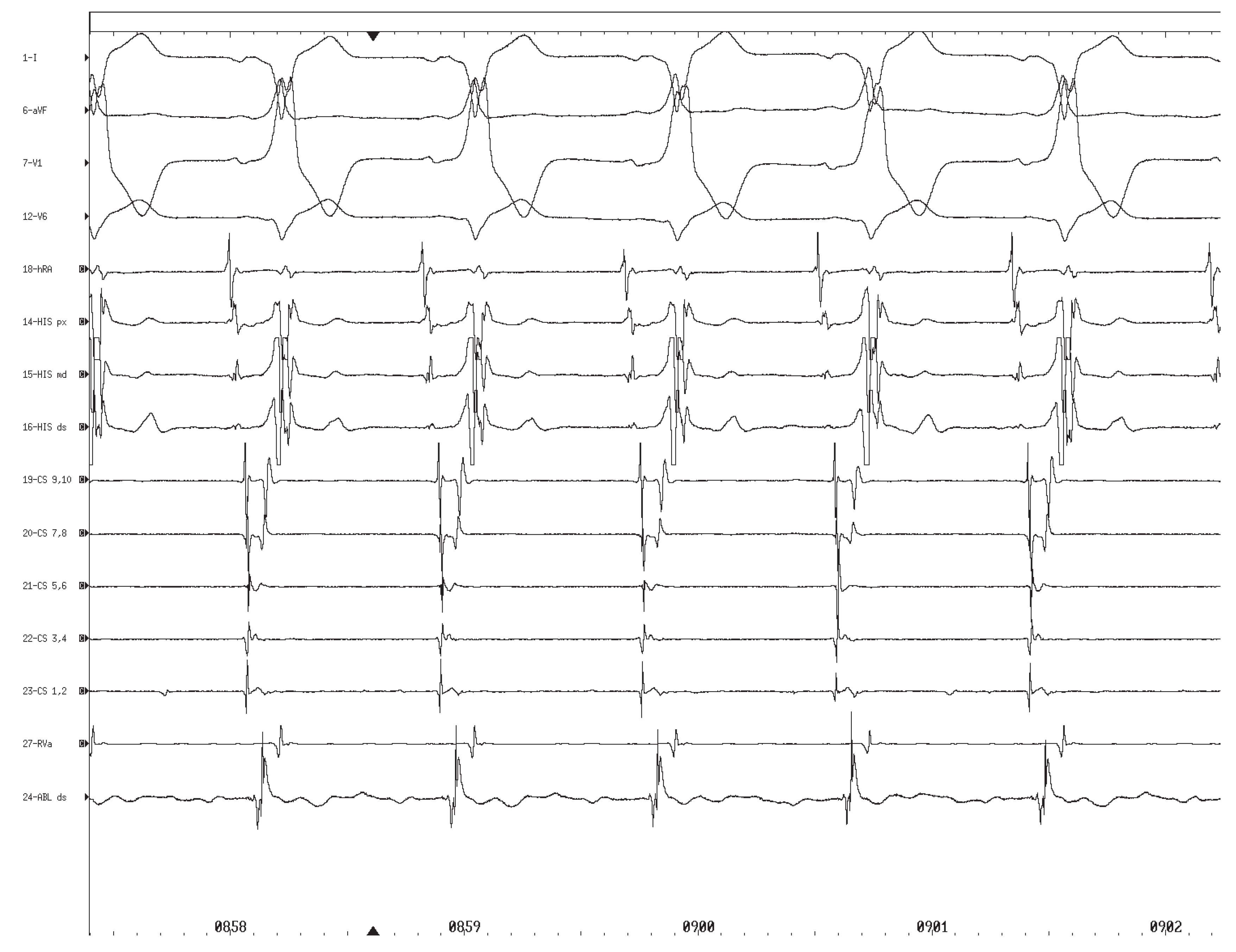
Figure 4.
Complete atrioventricular block with alternating junctional escape rhythm with left bundle branch block aberration and idioventricular rhythm of right bundle branch block pattern. Note the presence of a His potential in the first two complexes indicating the presence of atrioventricular block at the nodal level in combination with left bundle branch block. Ventricular cycle length 1500 ms.
Figure 4.
Complete atrioventricular block with alternating junctional escape rhythm with left bundle branch block aberration and idioventricular rhythm of right bundle branch block pattern. Note the presence of a His potential in the first two complexes indicating the presence of atrioventricular block at the nodal level in combination with left bundle branch block. Ventricular cycle length 1500 ms.
Discussion
Complete AV-block is an unusual complication of RF catheter ablation of left-sided accessory pathways [
2,
3,
4]. To our knowledge, only four cases of transient complete nodal or infranodal AV-block during RF catheter ablation of leftsided accessory pathways using a transaortic approach have been reported in patients with and without preexisting RBBB [
5,
6,
7]. Remarkably, our patient experienced a combined conduction abnormality at both the nodal and infranodal level during successful transaortic RF ablation of a left free wall accessory pathway resulting in transient complete nodal AV-block and LBBB.
The mechanism causing these transient conduction abnormalities may be speculated upon. Given that the site of RF ablation is remote from the physiologic conduction system and the fact that the observed conduction abnormalities occurred prior to the first delivery of RF energy RF-induced damage to the AV node and the left bundle branch may be ruled out as a cause of the transient conduction disorder. In contrast, mechanic trauma to the AV node and the left bundle branch during insertion of the ablation catheter across the aortic valve and/or direct pressure to these structures by the bent shaft of the ablation catheter placed at the mitral anulus is a likely mechanism responsible for the described conduction abnormalities. In line with this presumption is the observation that LBBB aberration occurred for the first time during orthodromic circus movement tachycardia, which was induced while inserting the ablation catheter into the left ventricle. Moreover, the fact that the change in the QRS morphology from partial to complete preexcitation indicating new onset of AV conduction impairment occurred shortly after insertion of the ablation catheter suggests a connection between the placement of the ablation catheter and the development of AV-block. Further support for an important role of mechanical trauma in the pathogenesis of cardiac conduction abnormalities during ablation of left-sided accessory pathways stems from a case report by Singh et al. describing recurrence of transient complete AV block during transaortic reinsertion of an ablation catheter into the left ventricle in a patient who had experienced a similar conduction abnormality during successful RF catheter ablation of a left free wall accessory pathway earlier [
6]. Finally, benzodiazepine-induced enhancement of vagal tone and pharmacologic sodium channel blockade by propafenone as well as electric cardioversion may have contributed to the pathogenesis of the transient conduction abnormalities observed in our patient.
Because of the presence of an adequate junctional/ventricular escape rhythm temporary pacing was not necessary during the period of complete AV block in our patient. However, since the initiation of an escape rhythm is unpredictable, the prophylactic insertion of a right sided pacing catheter prior to planned ablation of left-sided accessory pathways by a transaortic approach seems an appropriate measure.
Similar to other case reports [
5,
6,
7], the observed conduction abnormalities were only transient and normal conduction was restored within a few hours after termination of the intervention. In contrast, however, Calkins et al. reported one case of complete AV block requiring placement of a permanent pacemaker among 270 patients who underwent RF catheter ablation of a left free wall accessory pathway, indicating that this complication not always follows a benign course [
2].
In conclusion, development of complete AV block represents an uncommon but potentially serious complication of RF catheter ablation of left free wall accessory pathways. Although evaluation of conduction abnormalities may be impaired in the presence of preexcitation, subtle signs suggesting the onset of AV conduction abnormalities during or after insertion of the ablation catheter across the aortic valve, such as a sudden change in the preexcitation pattern suggestive of new onset of AV-block, should not be ignored. Given the potentially serious outcome of inadvertent complete AV block we recommend the insertion of a prophylactic right ventricular pacing catheter in all patients undergoing RF catheter ablation of left-sided accessory pathways via a transaortic approach.