Physical Activity in the Prevention of Type 2 Diabetes
Abstract
Introduction
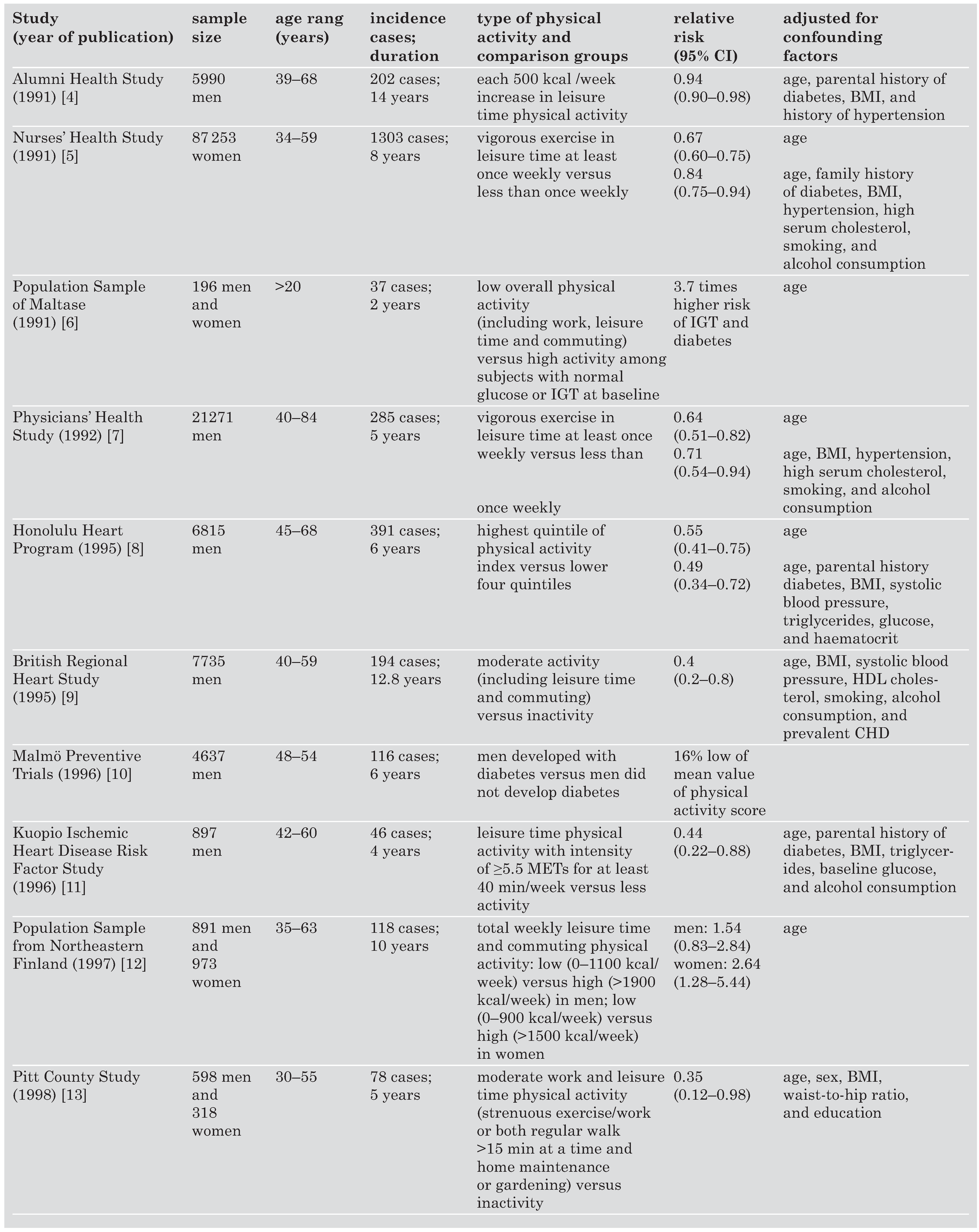
Physical activity and type 2 diabetes in prospective epidemiological studies
Physical fitness and type 2 diabetes in prospective epidemiological studies
Changes in the lifestyle and type 2 diabetes in clinical trials
Prevention of cardiovascular disease by physical activity in diabetic patients
Acknowledgments
References
- Wild, S.; Roglic, G.; Green, A.; Sicree, R.; King, H. Global preva lence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care 2004, 27, 1047–53. [Google Scholar]
- Neel, J.V. Diabetes mellitus: a “thrifty” genotype rendered detrimental by “progress”? Am J Hum Genet 1962, 14, 353–62. [Google Scholar]
- Wing, R.R.; Goldstein, M.G.; Acton, K.J.; Birch, L.L.; Jakicic, J.M.; Sallis, J.F.; et al. Behavioral science research in diabetes: lifestyle changes related to obesity, eating behavior, and physical activity. Diabetes Care 2001, 24, 117–23. [Google Scholar] [CrossRef]
- Helmrich SP, Ragland DR, Leung RW, Paffenbarger RS Jr. Physical activity and reduced occurrence of non-insulin-de-pendent diabetes mellitus. N Engl J Med 1991, 325, 147–52.
- Manson, J.E.; Rimm, E.B.; Stampfer, M.J.; Colditz, G.A.; Willett, W.C.; Krolewski, A.S.; et al. Physical activity and incidence of non-insulin-dependent diabetes mellitus in women. Lancet 1991, 338, 774–8. [Google Scholar]
- Schranz, A.; Tuomilehto, J.; Marti, B.; Jarrett, R.J.; Grabauskas, V.; Vassallo, A. Low physical activity and worsening of glucose tolerance: results from a 2-year follow-up of a population sample in Malta. Diabetes Res Clin Pract 1991, 11, 127–36. [Google Scholar]
- Manson, J.E.; Nathan, D.M.; Krolewski, A.S.; Stampfer, M.J.; Wil lett, W.C.; Hennekens, C.H. A prospective study of exercise and incidence of diabetes among US male physicians. Jama 1992, 268, 63–7. [Google Scholar]
- Burchfiel, C.M.; Sharp, D.S.; Curb, J.D.; Rodriguez, B.L.; Hwang, L.J.; Marcus, E.B.; et al. Physical activity and incidence of di abetes: the Honolulu Heart Program. Am J Epidemiol 1995, 141, 360–8. [Google Scholar] [CrossRef]
- Perry, I.J.; Wannamethee, S.G.; Walker, M.K.; Thomson, A.G.; Whincup, P.H.; Shaper, A.G. Prospective study of risk factors for development of non-insulin dependent diabetes in mid dle aged British men. BMJ 1995, 310, 560–4. [Google Scholar]
- Eriksson, K.F.; Lindgarde, F. Poor physical fitness, and im paired early insulin response but late hyperinsulinaemia, as predictors of NIDDM in middle-aged Swedish men. Dia betologia 1996, 39, 573–9. [Google Scholar]
- Lynch, J.; Helmrich, S.P.; Lakka, T.A.; Kaplan, G.A.; Cohen, R.D.; Sa lonen, R.; et al. Moderately intense physical activities and high levels of cardiorespiratory fitness reduce the risk of non-insulin-dependent diabetes mellitus in middle-aged men. Arch Intern Med 1996, 156, 1307–14. [Google Scholar]
- Haapanen, N.; Miilunpalo, S.; Vuori, I.; Oja, P.; Pasanen, M. As sociation of leisure time physical activity with the risk of coronary heart disease, hypertension and diabetes in mid dle-aged men and women. Int J Epidemiol 1997, 26, 739–47. [Google Scholar]
- James, S.A.; Jamjoum, L.; Raghunathan, T.E.; Strogatz, D.S.; Furth, E.D.; Khazanie, P.G. Physical activity and NIDDM in African-Americans. The Pitt County Study. Diabetes Care 1998, 21, 555–62. [Google Scholar]
- Hu, F.B.; Sigal, R.J.; Rich-Edwards, J.W.; Colditz, G.A.; Solomon, C.G.; Willett, W.C.; et al. Walking compared with vigorous physical activity and risk of type 2 diabetes in women: a prospective study. Jama 1999, 282, 1433–9. [Google Scholar] [CrossRef]
- Wei, M.; Gibbons, L.W.; Mitchell, T.L.; Kampert, J.B.; Lee, C.D.; Blair, S.N. The association between cardiorespiratory fitness and impaired fasting glucose and type 2 diabetes mellitus in men. Ann Intern Med 1999, 130, 89–96. [Google Scholar]
- Folsom, A.R.; Kushi, L.H.; Hong, C.P. Physical activity and inci dent diabetes mellitus in postmenopausal women. Am J Public Health 2000, 90, 134–8. [Google Scholar]
- Okada, K.; Hayashi, T.; Tsumura, K.; Suematsu, C.; Endo, G.; Fu-jii, S. Leisure-time physical activity at weekends and the risk of type 2 diabetes mellitus in Japanese men: the Osaka Health Survey. Diabet Med 2000, 17, 53–8. [Google Scholar] [CrossRef]
- Wannamethee, S.G.; Shaper, A.G.; Alberti, K.G. Physical activ ity, metabolic factors, and the incidence of coronary heart disease and type 2 diabetes. Arch Intern Med 2000, 160, 2108–16. [Google Scholar]
- Hu, F.B.; Leitzmann, M.F.; Stampfer, M.J.; Colditz, G.A.; Willett, W.C.; Rimm, E.B. Physical activity and television watching in relation to risk for type 2 diabetes mellitus in men. Arch Intern Med 2001, 161, 1542–8. [Google Scholar] [CrossRef]
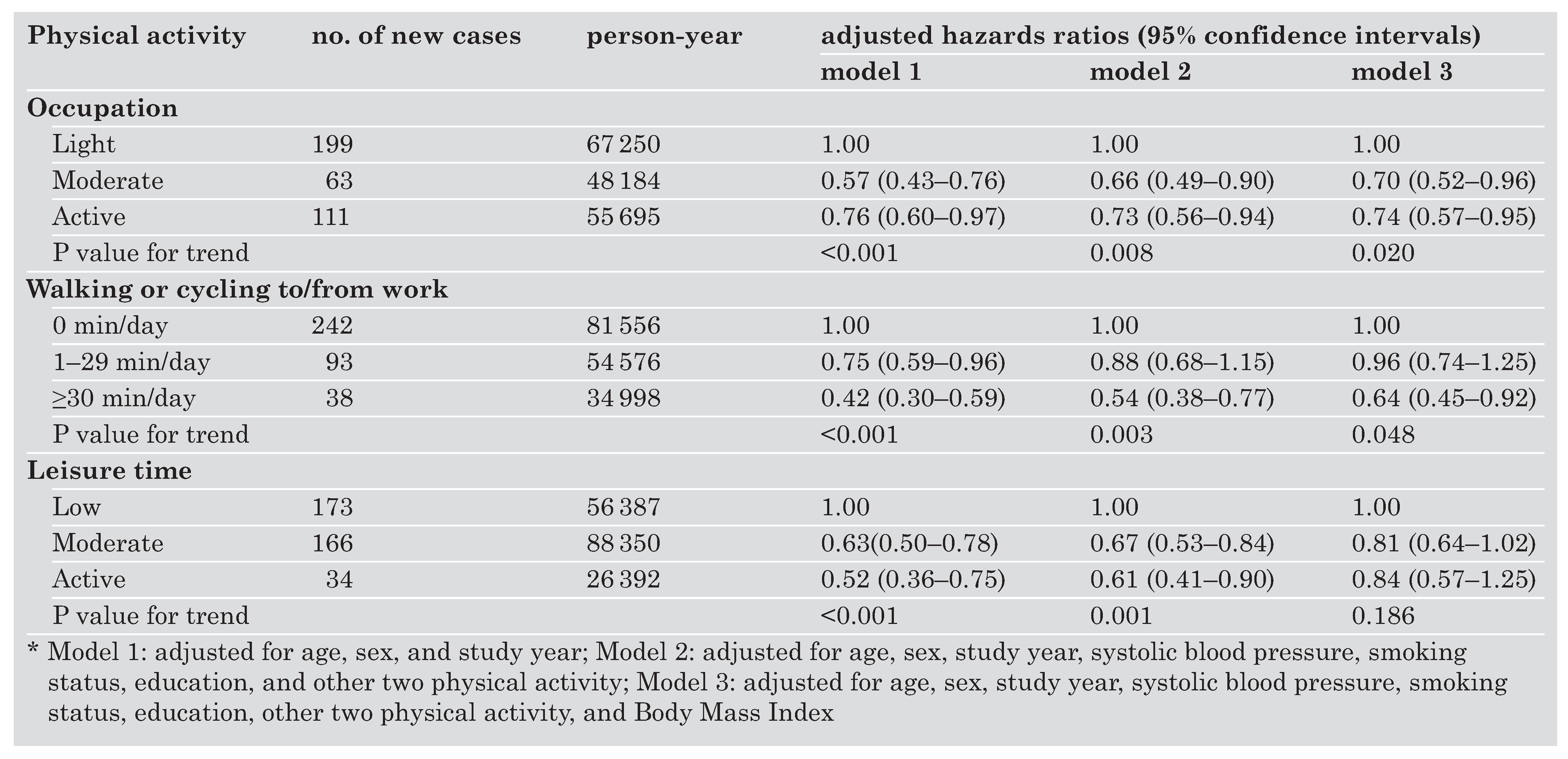
- Hu, G.; Qiao, Q.; Silventoinen, K.; Eriksson, J.G.; Jousilahti, P.; Lindstrom, J.; et al. Occupational, commuting, and leisure-time physical activity in relation to risk for type 2 diabetes in middle-aged Finnish men and women. Diabetologia 2003, 46, 322–9. [Google Scholar]
- Kriska, A.M.; Saremi, A.; Hanson, R.L.; Bennett, P.H.; Kobes, S.; Williams, D.E.; et al. Physical activity, obesity, and the inci dence of type 2 diabetes in a high-risk population. Am J Epi demiol 2003, 158, 669–75. [Google Scholar]
- Sawada, S.S.; Lee, I.M.; Muto, T.; Matuszaki, K.; Blair, S.N. Car diorespiratory fitness and the incidence of type 2 diabetes: prospective study of Japanese men. Diabetes Care 2003, 26, 2918–22. [Google Scholar]
- Dotevall, A.; Johansson, S.; Wilhelmsen, L.; Rosengren, A. In creased levels of triglycerides, BMI and blood pressure and low physical activity increase the risk of diabetes in Swedish women. A prospective 18-year follow-up of the BEDA*study. Diabet Med 2004, 21, 615–22. [Google Scholar]
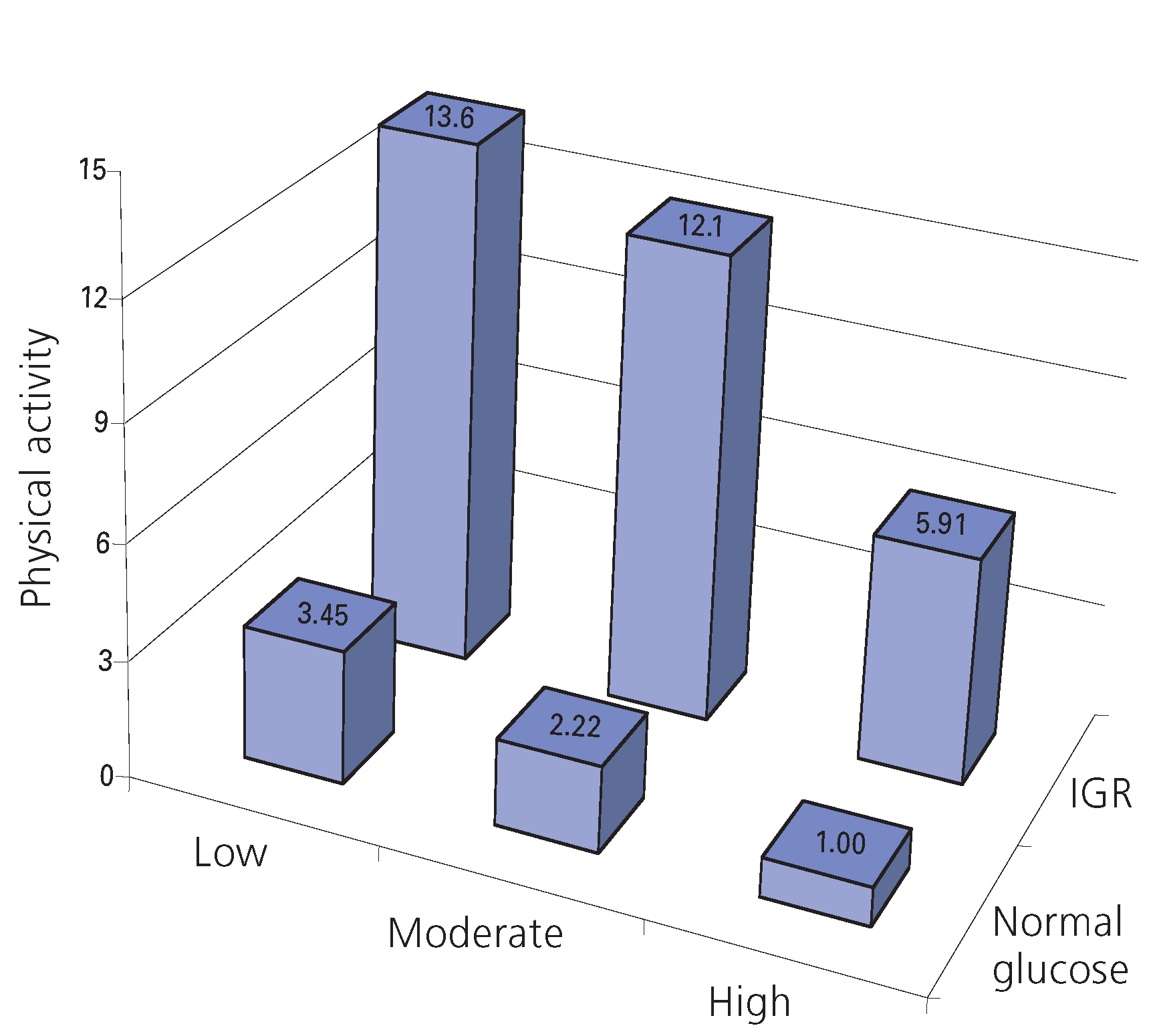
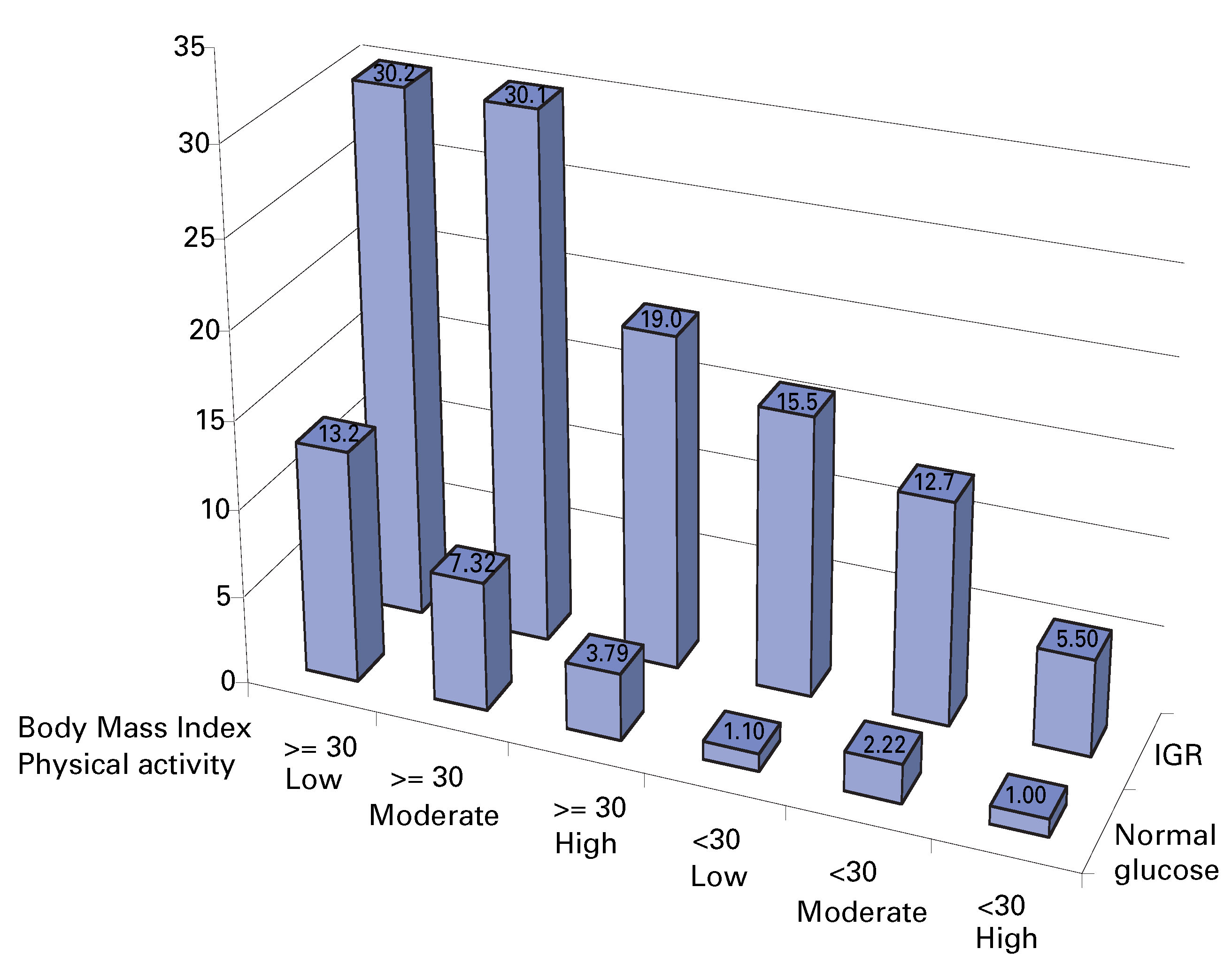
- Hu, G.; Lindstrom, J.; Valle, T.T.; Eriksson, J.G.; Jousilahti, P.; Sil ventoinen, K.; et al. Physical activity, body mass index, and risk of type 2 diabetes in patients with normal or impaired glucose regulation. Arch Intern Med 2004, 164, 892–6. [Google Scholar]
- Eriksson, K.F.; Lindgarde, F. Prevention of type 2 (non-insulin-dependent) diabetes mellitus by diet and physical exercise. The 6-year Malmo feasibility study. Diabetologia 1991, 34, 891–8. [Google Scholar]
- Pan, X.; Li, G.; Hu, Y.; Wang, J.; Yang, W.; An, Z.; et al. Effects of diet and exercise in preventing NIDDM in people with im paired glucose tolerance. The Da Qing IGT and Diabetes Study. Diabetes Care 1997, 20, 537–44. [Google Scholar]
- Tuomilehto, J.; Lindstrom, J.; Eriksson, J.G.; Valle, T.T.; Hamalainen, H.; Ilanne-Parikka, P.; et al. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med 2001, 344, 1343–50. [Google Scholar] [PubMed]
- Knowler, W.C.; Barrett-Connor, E.; Fowler, S.E.; Hamman, R.F.; Lachin, J.M.; Walker, E.A.; et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 2002, 346, 393–403. [Google Scholar] [PubMed]
- Eriksson, J.; Lindstrom, J.; Valle, T.; Aunola, S.; Hamalainen, H.; Ilanne-Parikka, P.; et al. Prevention of type II diabetes in sub jects with impaired glucose tolerance: the Diabetes Preven tion Study (DPS) in Finland. Study design and 1-year in terim report on the feasibility of the lifestyle intervention programme. Diabetologia 1999, 42, 793–801. [Google Scholar]
- Laaksonen, D.E.; Lindström, J.; Lakka, T.A.; Eriksson, J.G.; Niska nen, L.; Wikström, K.; et al. Physical activity in the prevention of type 2 diabetes: The Finnish Diabetes Prevention Study. 2004. [Google Scholar]
- The Diabetes Prevention Program Research Group. The Diabetes Prevention Program (DPP): description of lifestyle intervention. Diabetes Care 2002, 25, 2165–71.
- Wei, M.; Gibbons, L.W.; Kampert, J.B.; Nichaman, M.Z.; Blair, S.N. Low cardiorespiratory fitness and physical inactivity as pre dictors of mortality in men with type 2 diabetes. Ann Intern Med 2000, 132, 605–11. [Google Scholar] [CrossRef]
- Hu, F.B.; Stampfer, M.J.; Solomon, C.; Liu, S.; Colditz, G.A.; Speizer, F.E.; et al. Physical activity and risk for cardiovascular events in diabetic women. Ann Intern Med 2001, 134, 96–105. [Google Scholar] [CrossRef] [PubMed]
- Batty, G.D.; Shipley, M.J.; Marmot, M.; Smith, G.D. Physical activity and cause-specific mortality in men with type 2 diabetes/impaired glucose tolerance: evidence from the Whitehall study. Diabet Med 2002, 19, 580–8. [Google Scholar] [PubMed]
- Gregg, E.W.; Gerzoff, R.B.; Caspersen, C.J.; Williamson, D.F.; Narayan, K.M. Relationship of walking to mortality among US adults with diabetes. Arch Intern Med 2003, 163, 1440–7. [Google Scholar] [PubMed]
- Tanasescu, M.; Leitzmann, M.F.; Rimm, E.B.; Hu, F.B. Physical activity in relation to cardiovascular disease and total mor tality among men with type 2 diabetes. Circulation 2003, 107, 2435–9. [Google Scholar] [CrossRef]
- Hu, G.; Eriksson, J.; Barengo, N.C.; Lakka, T.A.; Valle, T.T.; Nis-sinen, A.; et al. Occupational, commuting, and leisure-time physical activity in relation to total and cardiovascular mor tality among Finnish subjects with type 2 diabetes. Circula tion 2004, 110, 666–73. [Google Scholar]
- Mayer-Davis, E.J.; D’Agostino, R.; Jr Karter, A.J.; Haffner, S.M.; Rewers, M.J.; Saad, M.; et al. Intensity and amount of physical activity in relation to insulin sensitivity: the Insulin Resis tance Atherosclerosis Study. Jama 1998, 279, 669–74. [Google Scholar]
- Laaksonen, D.E.; Lakka, H.M.; Salonen, J.T.; Niskanen, L.K.; Rau ramaa, R.; Lakka, T.A. Low levels of leisure-time physical activity and cardiorespiratory fitness predict development of the metabolic syndrome. Diabetes Care 2002, 25, 1612–8. [Google Scholar] [CrossRef]
- Lakka, T.A.; Laaksonen, D.E.; Lakka, H.M.; Mannikko, N.; Niska nen, L.K.; Rauramaa, R.; et al. Sedentary lifestyle, poor cardio respiratory fitness, and the metabolic syndrome. Med Sci Sports Exerc 2003, 35, 1279–86. [Google Scholar]
- Pate, R.R.; Pratt, M.; Blair, S.N.; Haskell, W.L.; Macera, C.A.; Bouchard, C.; et al. Physical activity and public health. A rec ommendation from the Centers for Disease Control and Pre vention and the American College of Sports Medicine. Jama 1995, 273, 402–7. [Google Scholar] [CrossRef]
- Willett, W.C.; Dietz, W.H.; Colditz, G.A. Guidelines for healthy weight. N Engl J Med 1999, 341, 427–34. [Google Scholar] [CrossRef]
- Blair, S.N.; Cheng, Y.; Holder, J.S. Is physical activity or physi cal fitness more important in defining health benefits? Med Sci Sports Exerc 2001, 33, S379–99. [Google Scholar] [CrossRef]
- Wannamethee, S.G.; Shaper, A.G. Physical activity in the prevention of cardiovascular disease: an epidemiological perspective. Sports Med 2001, 31, 101–14. [Google Scholar] [CrossRef] [PubMed]
- Dubbert, P.M.; Carithers, T.; Sumner, A.E.; Barbour, K.A.; Clark, B.L.; Hall, J.E.; et al. Obesity, physical inactivity, and risk for cardiovascular disease. Am J Med Sci 2002, 324, 116–26. [Google Scholar] [CrossRef] [PubMed]
- Erlichman, J.; Kerbey, A.L.; James, W.P. Physical activity and its impact on health outcomes. Paper 1, The impact of phys ical activity on cardiovascular disease and all-cause mortal ity: an historical perspective. Obes Rev 2002, 3, 257–71. [Google Scholar]
- Katzmarzyk, P.T.; Janssen, I.; Ardern, C.I. Physical inactivity, excess adiposity and premature mortality. Obes Rev 2003, 4, 257–90. [Google Scholar] [CrossRef]
  |
 |
 |
 |
© 2025 by the authors. Attribution - Non-Commercial - NoDerivatives 4.0.
Share and Cite
Hu, G.; Lakka, T.A.; Barengo, N.C.; Tuomilehto, J. Physical Activity in the Prevention of Type 2 Diabetes. Cardiovasc. Med. 2004, 7, 394. https://doi.org/10.4414/cvm.2004.01056
Hu G, Lakka TA, Barengo NC, Tuomilehto J. Physical Activity in the Prevention of Type 2 Diabetes. Cardiovascular Medicine. 2004; 7(11):394. https://doi.org/10.4414/cvm.2004.01056
Chicago/Turabian StyleHu, Gang, Timo A. Lakka, Noël C. Barengo, and Jaakko Tuomilehto. 2004. "Physical Activity in the Prevention of Type 2 Diabetes" Cardiovascular Medicine 7, no. 11: 394. https://doi.org/10.4414/cvm.2004.01056
APA StyleHu, G., Lakka, T. A., Barengo, N. C., & Tuomilehto, J. (2004). Physical Activity in the Prevention of Type 2 Diabetes. Cardiovascular Medicine, 7(11), 394. https://doi.org/10.4414/cvm.2004.01056




