Data collection
Between 1 January 2005 and 31 December 2017, a total of 877 composite graft replacements were performed at our institution (average of 65 cases per year). All patients who underwent this procedure because of acute type A aortic dissection, acute aortic valve endocarditis with destruction of the aortic root and/or aorto-ventricular disconnection and those in whom composite graft replacement was a redo procedure were eliminated from the present analysis (n = 255). We excluded also those patients who underwent a Ross procedure, a homograft or xenograft as mini-aortic root replacement, in a similar technique to that of composite graft replacement. Therefore, we report here the results obtained in 622 patients treated in an elective operative setting by 16 different surgeons in a tertiary teaching institution.
The most important demographic factors are presented in
Table 1 and the indications for composite graft replacement in
Table 2. We usually used 5 cm as cut-off diameter of the aortic root and/or the ascending aorta in the large majority of patients. In particular subsets of patients with a potentially higher risk of aortic complication, a cut-off between 4.5 cm and 5 cm was also considered as operative indication:
- –
younger patients (<60 years with an estimated life expectancy of more than 15 to 20 years),
- –
those with a particular cardiovascular risk and/or family history of aortic disease and
- –
those with a small body surface area and therefore an unfavourable indexed aortic diameter,
- –
those with connective tissue diseases.
The classical cut-off diameter in patients with true bicuspid and pseudo-bicuspid aortic valve was usually 4.5 cm to 5 cm during the whole observational period, especially in those patients younger than 65 years and in those with a noticeably very thin aortic wall, and pertinently when the aortic valve was the primary indication for surgery.
The decision to proceed with an open distal anastomosis to completely eradicate the pathology of the ascending aorta and to avoid a suture in a still moderately dilated aorta (usually >4 cm) was discussed in the team, but the final intraoperative decision was left at the discretion of the surgeon. In all patients with an aortic arch diameter less than 4.5 cm, a conservative approach, with the anastomosis performed proximally to the innominate artery, was chosen. In all other cases, partial or total arch replacement was performed (see operative details in
Table 3).
Surgical techniques
Composite graft replacement was performed through a median sternotomy with central cannulation for all procedures in the absence of a contraindication to approaching the ascending aorta or the proximal aortic arch because of severe calcifications. In this case, arterial cannulation was performed at the level of the right subclavian artery and only exceptionally at the level of the right extern iliac / common femoral artery. Cardiopulmonary bypass was conducted in mild hypothermia (32°C) for all standard cases and in moderate hypothermia (26–28°C) if the distal anastomosis was performed with an open technique at the level of the proximal arch and in all cases in which the arch had to be replaced with re-implantation of one, two or all three supra-aortic vessels. This depended on the extent of the arch disease. In the latter case, selective antegrade cerebral perfusion through self-blocking catheters (LeMaitre Vascular, Burlington, MA) was administered in both common carotid arteries (temperature of the perfusate 20°C, flow 500–800 ml/min, pressure 50–60 mm Hg). Myocardial protection was performed with single-shot low-volume cardioplegia (Cardioplexol©, Bichsel, Interlaken*) to obtain cardiac arrest and blood cardioplegia was repeated at 20- to 30-minute intervals thereafter.
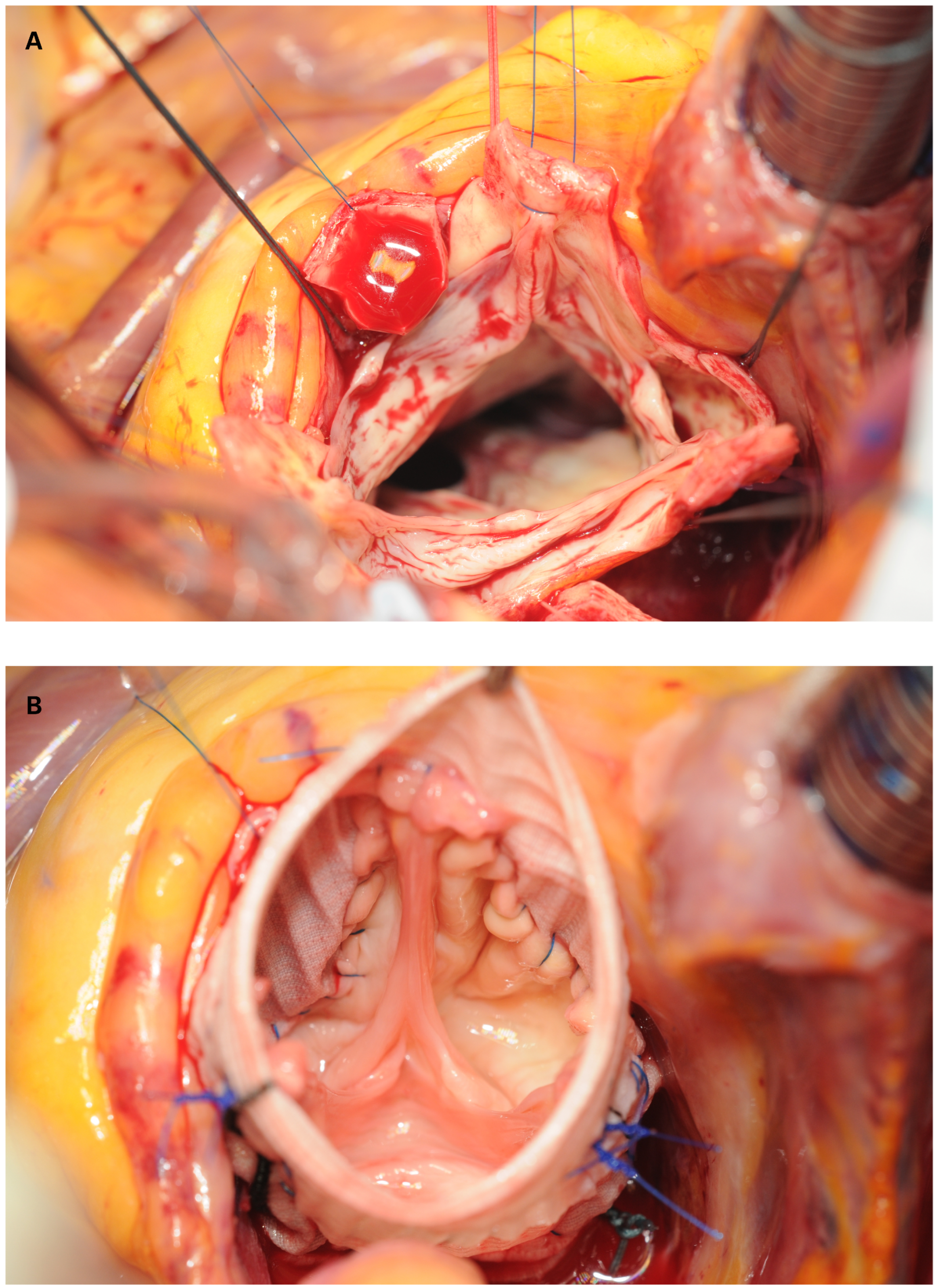
The large majority of the patients underwent the modified Bentall procedure with the open technique, including complete resection of the pathological aorta and excision of the coronary artery orifices. The proximal anastomosis at the level of the aortic annulus was performed using interrupted Ethibound 2.0 sutures, followed by direct re-implantation of the coronary buttons using a 6.0 polypropylene running suture (
Figure 3). A bovine pericardial strip was used at the discretion of the surgeons to reinforce the suture lines in the case of friable coronary buttons or aortic wall. Fibrin glue (Evicel
®, Ethicon, New Brunswick, NJ, USA) was applied to prevent oozing from the anastomoses.
When the pathology was limited to the ascending aorta, the distal anastomosis was performed with the aortic clamp in place and constructed with a 4.0 Prolene running suture. If the distal anastomosis had to be performed at the level of the proximal or more distal arch, we routinely used a Vascutek Terumo Anteflow (Terumo®, Renfrewshire, Scotland, UK) prosthesis with a side arm for the arterial return cannula that was used for rewarming and reperfusion. Finally, an end-to-end anastomosis was made between the “root” and the “arch” prostheses; this sequence allowed the time during which the patient was cooled down to be shortened and usually accelerated the rewarming period. As soon as the target temperature of 35.5°C was reached, cardiopulmonary bypass was discontinued, the patient decannulated and the chest closed in typical way.
Transoesophageal echocardiography was used throughout the procedure to check for any additional pathology (for instance patent foramen ovale) and to optimally monitor the weaning process (filling condition, ventricular contractility, function of the prosthesis).
Data acquisition
Preoperative and perioperative data were prospectively collected in a computerised chart (Dendrite) and retrospectively analysed. All patients had previously signed informed consent to the procedure and the local ethics committee has given approval for the study (2019-01033).
All continuous variables are expressed as mean ± standard deviation or median with interquartile range (when not normally distributed). The Shapiro-Wilk test was used to assess the normality of data distribution. Categorical variables are expressed as percentages. For the full analysis of the data, we used Student’s t-test, the Mann-Whitney Utest and the chi-square test.
Primary outcome was defined as 30-day mortality. Secondary outcomes were: re-thoracotomy for bleeding, myocardial infarction, acute kidney injury and permanent neurological deficits.
Univariate and multivariate analysis of the potential predictors for operative mortality were performed using a Cox regression model that allowed testing of the association between independent risk factors and mortality or adverse perioperative outcome (including 30-day mortality, re-thoracotomy for bleeding, myocardial infarction, acute kidney injury according to KDIGO definition), and permanent neurological deficits (defined according to the Guidelines For Reporting Morbidity and Mortality after Cardiac Valve Operations VARC). Risk factors were determined by selecting variables with a p-value <0.1 from univariate analysis. A p-value <0.05 was considered as statistically significant.
Results
The mean age of the patient was 59.5 ± 12.5 years (range 16–85), 423 patients (68%) were male, mean body mass index was 27.8 ± 4.3 kg/m
2 (18.4–37.3). Annulo-aortic dilatation with or without aortic valve dysfunction was the most frequent indication (n = 448), bicuspid valve with aortic root and/or ascending aortic dilatation was found in 107 patients. All available demographic characteristics and cardiovascular risk factors are summarised in
Table 1. Approximatively half of the patients (n = 288, 46%) were in New York heart association (NYHA) functional class I, 226 (36.3%) were in class II, 93 (15%) were in class III and only 15 patients (2.7%) were in class IV. A majority of patients presented with various degrees of aortic regurgitation and pure aortic stenosis was present in 164 patients (26.5%). Forty-nine patients (7.8%) had neither significant stenosis nor regurgitation but only a dilated aortic root ± dilated ascending aorta. A congenital pathology (bicuspid aortic valve) was present in 107 patients (17.3%), a degenerative aetiology was seen in 60 patients (9.6%). Connective tissue disease (Marfan or Loeys-Dietz syndrome) was confirmed by clinical and/or genetic analysis in 33 patients. The mean diameter of the aortic root was 5.4 cm (4.8–8.4) and of the ascending aorta 5.6 cm (5.0–9); there was no significant difference in diameters between patients with a tricuspid or a bicuspid valve (
Table 2).
The most important perioperative factors are summarised in
Table 3. An isolated composite graft was performed in 336 patients (44%), with some extension into the aortic arch required in 195 patients (31.4%): this includes a majority of patients in whom the distal anastomosis was performed in an open fashion to radically exclude a dilated cranial ascending aorta (n = 139) and those with some degree of dilatation at the level of the aortic arch itself (n = 56). The mean cross-clamp and cardiopulmonary bypass times were 86.5 ± 49 minutes (range 51–143) and 110 ± 81 minutes (range 90–253), respectively. Hypothermic circulatory arrest was used in 31.3% (195/622) with a mean duration of 16.2 minutes (range 8–46).
Mechanical and tissue prostheses were used in 187 (31%) and 435 (69%) patients, respectively. The decision to use a mechanical or tissue valve was made according to the European Society of Cardiology (ESC) / European Association for Cardio-Thoracic Surgery (EACTS) guidelines and included the patient’s age and preference, comorbidities, and the personal experience of the surgical team [
7]. In general, tissue valves were used in patients older than 65 years (since 2010 the age threshold was set closer to 60 years owing to the increasing possibility to treat prosthetic degeneration with transcatheter aortic valve implantation) and also used in those with an predicted shorter life expectancy due to significant comorbidities, as well as in those who did not accept life-long oral anticoagulation or had contraindications for anticoagulation.
The mean age of patients was 52 years (range 16–74) and 67 years (25–85) in the mechanical and tissue valve groups, respectively.
When a mechanical valve was indicated, we used either a prefabricated St. Jude Medical composite graft (Abbott Inc. St-Paul, MN) or the Medtronic valved conduit (Medtronic, Dublin, Ireland). Among patients who received a biological conduit, a Carpentier-Edwards Magna or Magna Ease tissue valve (Edwards Lifesciences, Irvine, CA) was hand-sewn into a Vascutek graft. Between 2001 and 2006 a series of prefabricated bio-composite grafts (Shelhigh, Union, NJ) was used in 115 patients [
8]; only 17 of those who received such an implant in 2005 and 2006 were included in this analysis, since a substantial number had been implanted in the presence of acute dissection, destructive endocarditis and/or graft infection.
Additional procedures were performed in 91 patients; a large majority received either coronary artery bypass grafting (n = 46) or mitral valve repair or replacement (n = 39). Smaller procedures such as ablation because of atrial fibrillation, closure of a patent foramen ovale or occlusion of the left atrial appendage were performed in 98 patients (
Table 3). All patients with a mechanical valve received intravenous heparin 10,000–20,000 U/d from postoperative day 1 and oral warfarin usually from postoperative day 3 or 4. Long-term anticoagulation was maintained with a target international normalised ratio (INR) of 2.5 and salicylic acid was administered for 3 months. Patients who received a biological conduit received aspirin 100 mg as long as tolerated, unless there was an indication for oral anticoagulation, such as atrial fibrillation or poor left ventricular function (LVEF <35%).
Early mortality (30-day) occurred in nine patients (1.4%). Causes of death were: low output syndrome in three patients and cerebrovascular damage in four, severe respiratory failure due to postoperative pneumonia in one and multiorgan failure due to postoperative septicaemia in the last patient. Perioperative complications are summarised in
Table 4. These included re-exploration because of bleeding in 3.5%, stroke in 2.5% and acute renal failure (rise in creatinine over 150 µmol/l or requiring dialysis) in 3.9% of the patients. The most frequently observed arrhythmia was atrial fibrillation in 152 patients (24.5%).
Out of a univariate analysis including 17 demographic, pre- and intra-operative factors, those with a p-value below 0.05 were entered in a multivariate logistic regression analysis (
Table 5). The latter revealed that a severely reduced left ventricular function (LVEF <0.30) (odds ratio [OR] 4.9, 95% confidence interval [CI] 1.7–12.2), aortic regurgitation grade IV (OR 6.35, 95% CI 1.8–17.8), NYHA functional class III or IV (OR 2.94, 95% CI 1.5–7.4) and need for additional coronary artery bypass grafting (OR 4.25, 95% CI 1.6–11.3) were the independent risk factors for mortality (
Table 6).
To allow a comparison of outcomes between aortic valve replacement and composite grafts, we collected and summarised the same characteristics for a large cohort of 1244 patients out of 4685 patients who underwent isolated aortic valve replacement during the same period [
9]. Every isolated aortic valve replacement that was performed immediately before and after each composite graft procedure has been considered for the purpose of comparing 30-day mortality and morbidity only. There was no significant difference in terms of early mortality (1.1%) and incidence of perioperative complications between patients who underwent elective composite graft replacement and those who received isolated aortic valve replacement (
Table 7).
Discussion
Composite graft replacement of the aortic root (called the Bentall procedure in the past) is the most radical treatment to eradicate pathologies of the aortic root with or without involvement of the aortic valve. This procedure has helped to save a tremendous number of lives and has received important technical refinements that have resulted in a significant reduction of perioperative morbidity and mortality in the last 20 years [
10,
11,
12,
13,
14,
15,
16,
17,
18,
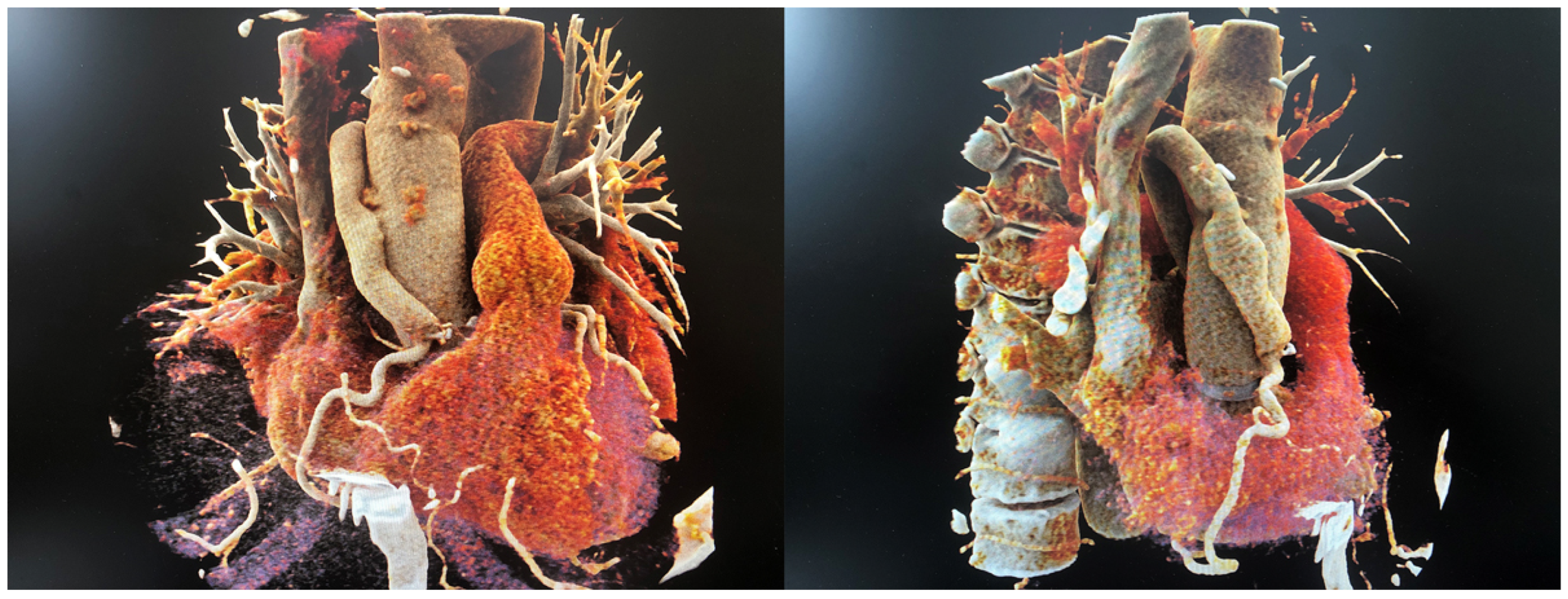
19]. Beside modifications of the original technique (such as the open technique that allows for instance a better visual control during coronary reimplantation), optimisation of cardiopulmonary bypass technology and improved myocardial protection together with better perioperative management have contributed to make the electively performed composite graft procedure a standard of practice with very low mortality and morbidity in high volume centres. Parallel to this, technical advances have also increasingly allowed the native aortic valve to be preserved in a substantial number of patients (remodelling or re-implantation procedures as shown in
Figure 4), thus avoiding the implantation of a prosthetic valve and life-long anticoagulation, which is particularly beneficial in younger patients [
20,
21,
22,
23].
As a result, the referral pattern for the treatment of an enlarged aortic root has changed, and includes nowadays not only patients with a clear-cut indication (e.g., aortic root or ascending diameter >5.5–6 cm), but also healthier patients who are referred at an earlier stage of the aortic disease (diameter 4.5–5 cm) because they are anxious about the spontaneous outcome of the unoperated condition [
24,
25]. The latter fact has been emphasised by some analyses of the International Registry of Acute Aortic Dissection (IRAD), which have shown that acute aortic dissection may occasionally occur in a pretty “normal-sized” ascending aorta or aortic root [
26]. At the other extreme of complexity, more patients with multiple previous surgeries have recently been more addressed, to repair late problems of prior aortic surgery such as pseudoaneurysms, prosthetic endocarditis and vascular graft infection, as well as ongoing disease in the downstream aorta (distal ascending, arch and/or proximal descending segments).
Presently, the guidelines still recommend prophylactic surgical replacement of the ascending aorta at a diameter of >5–5.5 cm, mainly to avoid an emergency situation, but encouraged by the very satisfactory outcomes of composite graft surgery, there is increasing opinion that a more aggressive approach may be justified [
27,
28].
The primary goal of this study was to analyse the early results of elective composite graft replacement in a teaching institution. Our hypothesis was that, thanks to the growing number of patients who undergo this procedure, the results have greatly improved and may nowadays be pretty comparable to those obtained in patients who undergo isolated aortic valve replacement.
The question “why compare composite graft with isolated aortic valve replacement?” may be considered as either futile or pertinent: futile since one may argue the pathologies requiring either aortic root or only aortic valve replacement are not comparable, pertinent because the dilated aortic root is a continuous variable with some grey zones for a surgical indication. These concern mainly:
- –
Younger patients with either aortic stenosis or regurgitation (the latter not amenable to a valve sparing procedure) and a dilatation around 4.5 cm. Due to the increasing life expectancy of the current generations, isolated valve surgery may not be the definitive option since a further growth requiring redo surgery may be a realistic situation if the aortic root is not addressed at initial surgical repair.
- –
Patients with a bicuspid valve and moderate dilatation of the aortic root. The best surgical management is still matter of discussion.
During the same time period, we experienced a substantial number of patients who, for their long-term outcome, would have been better treated with a composite graft (especially those under 60 years of age with a moderately enlarged aortic root of around 4.5 cm), but still underwent isolated aortic valve replacement because a composite graft was considered by the operating surgeon to significantly increase the perioperative risk.
Thanks to several master theses in our institution and participation in TAVI-SAVR prospective trials, we have acquired a robust database on patients who underwent isolated aortic valve replacement (Dendrite clinical database from the European Association of Cardio-thoracic Surgery). Our initial idea was to perform either a casematched study or a propensity score analysis, but the ethics committee did not support such an analysis for methodological reasons, since it argued that the indications for either surgical aortic valve replacement (SAVR) or a composite graft would not be the same. We had to accept this point of view, although we did not completely agree since the argumentation did not take into account the “continuum” characteristic of the aortic root diameter and the fluent indications. Nevertheless, we decided to limit our comparison to two large cohorts of patients operated on throughout the same period.
Despite the excellent results of the present single-centre analysis, we still believe that composite graft surgery remains technically more demanding (longer perfusion and ischaemia times) than other standard procedures performed in daily surgical practice, such as isolated aortic valve replacement. For this reason, before advocating a wider application of a more radical approach to aortic root pathologies (for instance at a diameter of 4.5–5 cm), it is crucial to correctly balance the reduced risk of acute type A aortic dissection obtained by a more liberal indication and therefore earlier surgery with the realistic procedural risks of a prophylactic aortic root replacement in the index insitution.
This is the reason why we compared a series of composite graft replacements with a contemporaneous series of isolated valve replacements in a non-matched population. When early mortality and complications are compared, we are able to conclude that the complexity of the composite graft procedure did not result in a significant increase of adverse outcome compared with aortic valve replacement only. This is one reason why we believe that a somewhat liberal indication to proceed with composite graft replacement may be justified for patients with a borderline aortic root diameter, provided that surgery is performed by a team of surgeons with an appropriate expertise. A recent analysis of the Society of Thoracic Surgeons Adult Cardiac Surgery Database has confirmed a significant decrease of risk-adjusted mortality in centres performing more than 40 aortic root operations per year. Interestingly, 95% of treating centres in the US performs fewer than 16 aortic root procedures per year and, in a pooled analysis of the Society of Thoracic Surgeons (STS) database, the observed mortality for aortic root surgery was over 4% [
14].
Although a number of 40 procedures per year seems to be reasonable, we believe that US numbers cannot be applied 1:1 everywhere around the world, and that 25–30 composite graft procedures per year may be sufficient if teaching and supervision are practiced with utmost attention and dedication. However, we recognise that the discussion about minimum case load remains a controversial topic in cardiac and aortic surgery [
29,
30,
31,
32].
Our reported in-hospital mortality of 1.4% for elective composite graft surgery is comparable to that observed in other contemporary analyses of other high-volume centres. In a series of over 500 patients, Etz has reported an early mortality rate of 1.4% for composite grafts with mechanical valves and 3.7% with biological valves [
12]. In a 17-year experience, Kallenbach et al. observed an average early mortality rate of 4.8%, which has been reduced to 1.6% in the most recent treatment period (last 5 years) [
13]. Furthermore, some centres have reported a perioperative mortality close to zero, even for more complex procedures such the valve-sparing reimplantation technique, but this type of surgery is usually applied in selected and younger patients with aortic root dilatation with or without aortic valve regurgitation [
33,
34].
In 2016, a group of co-authors from Paris and Rotterdam published a systematic review and meta-analysis about the Bentall procedure to create a benchmark for the potential therapeutic benefit of valve-sparing aortic root replacement [
17]. They identified 46 papers (published between 1998 and 2015) with a total of more than 7600 patients who underwent a Bentall operation using a mechanical valve only. The pooled early mortality was 5.6% and the authors were not able to show a trend towards reduced mortality in more recent years. The annual linearised occurrence of late mortality was 2.02% during the first 6 years; it was 2.66% for major valve-related adverse events, 0.64% for thromboembolism, 0.46% for haemorrhage and 0.39% for endocarditis. Use of a mechanical valve was associated with a decreased hazard of reoperation.
From the STS database, early mortality following a composite graft was 8.9% but these data included patients with acute endocarditis and those operated on non-electively [
14,
31]; therefore, a true comparison with our results is not reasonable.
In this series of elective aortic root replacements, adding a short period of circulatory arrest at a core temperature of 28–30°C with bilateral antegrade selective cerebral perfusion did not increase the risk for either mortality or morbidity. This may appear surprising, but the average duration of circulatory arrest was ±15 minutes and all patients underwent a standard cerebral protection protocol including pentothal and bilateral antegrade cerebral perfusion.
It has to be noted, that a substantial proportion of these operations was performed by senior resident surgeons as a teaching procedure. This is a classical function of a teaching tertiary institution. Another interesting observation is that some of the surgeons of our team are left-handed [
35]. The fact that the operation was performed by a younger surgeon or by a left-handed surgeon did not increase the perioperative risk. Adsumilli revealed the perceptions of left-handed surgeons in adapting to a right-handed world [
36]. The concept in our team was that left-handed surgeons do not have to adapt to techniques described by right-handed mentors. Early laterality related mentoring during surgical residency may reduce the inconveniences that left-handed surgeons could encounter during learning [
37]. In addition, some specific steps of the procedure may be facilitated by being left handed, for instance the distal anastomosis with the arch open, and the re-attachment of the left coronary artery to the composite graft.
This analysis includes all limitations of a retrospective single-centre study. The use of univariate and multivariate analysis for determining predicting factors of operative mortality is adequate but a case-match study or a propensity score analysis would have been more appropriate for comparing the outcomes of isolated aortic valve replacement with those of aortic root replacement.
Nevertheless, we would like to repeat our statement from above that the question “why compare composite graft with isolated aortic valve replacement?” is a pertinent one. During the same period, we had a substantial number of redo operations following isolated aortic valve replacement in patients who had valve replacement alone, although their root was already moderately dilated at the time of the index operation. We may speculate that these patients would have benefited initially from a more aggressive approach.
Together with the encouraging results observed in the present series, this is the reason why we believe that a more liberal approach to root replacement might be justified in a substantial number of patients with borderline root dilatation.