Percutaneous Closure of Ventricular Septal Defect Following Aortic Valve Replacement
Abstract
Introduction
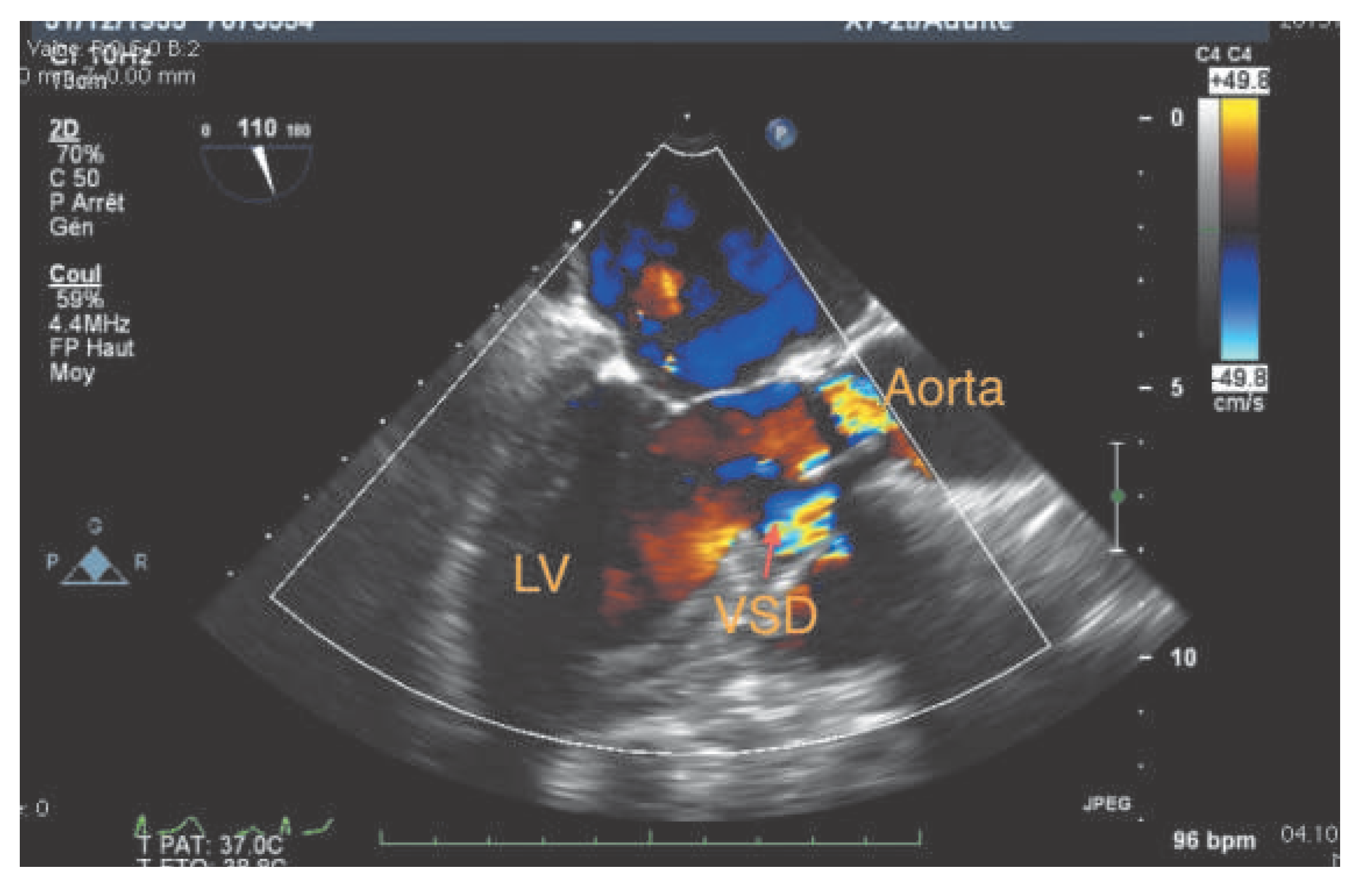
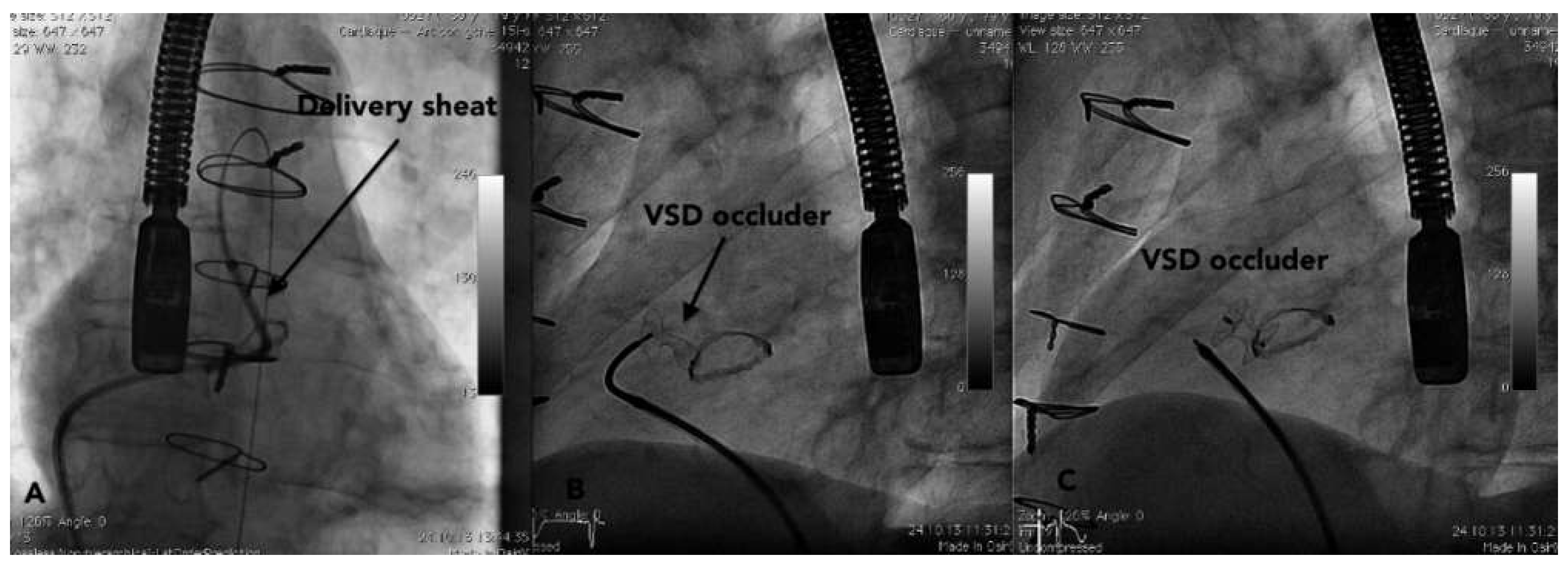
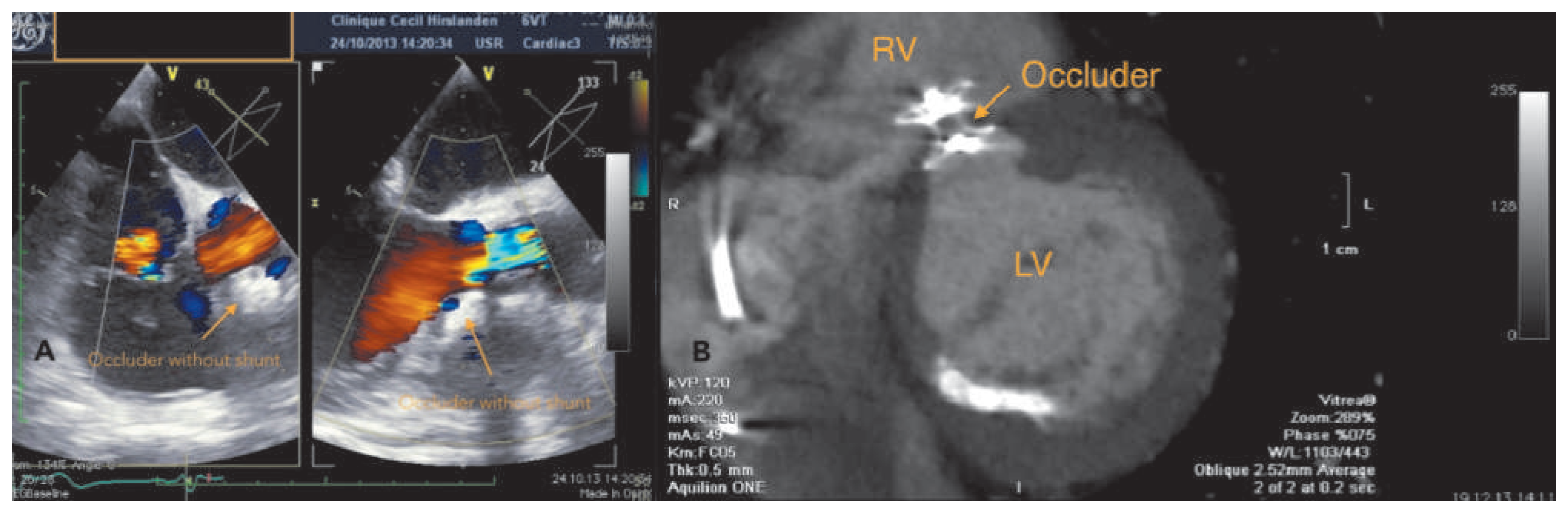
Case report
Discussion
Funding/potential competing interests:
References
- Holzer, R.; Latson, L.; Hijazi, Z.M. Device closure of iatrogenic membranous ventricular septal defects after prosthetic aortic valve replacement using the Amplatzer membranous ventricular septal defect occluder. Catheter Cardiovasc Interv. 2004, 62, 276–280. [Google Scholar] [CrossRef] [PubMed]
- Koneti, N.R.; Sreeram, N.; Penumatsa, R.R.; Arramraj, S.K.; Karunakar, V.; Trieschmann, U. Transcatheter retrograde closure of perimembranous ventricular septal defects in children with the Amplatzer duct occluder II device. J Am Coll Cardiol. 2012, 60, 2421–2422. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Noble, S.; Ibrahim, R. Transcatheter membranous ventricular septal defect closure through a mechanical aortic prosthesis using the Amplatzer membranous ventricular septal defect occluder. Catheter Cardiovasc Interv. 2009, 73, 167–172. [Google Scholar] [CrossRef] [PubMed]
- Klein, A.J.; Garcia, J.A.; Carroll, J.D. Percutaneous closure of an iatrogenic ventricular septal defect following mechanical aortic valve replacement using the transseptal technique. Catheter Cardiovasc Interv. 2007, 70, 1018–1024. [Google Scholar] [CrossRef] [PubMed]
- Butera, G.; Carminati, M.; Chessa, M.; et al. Transcatheter closure of perimembranous VSD: Early and long-term results. J Am Coll Cardiol. 2007, 50, 1189–1195. [Google Scholar] [CrossRef] [PubMed]

© 2014 by the author. Attribution - Non-Commercial - NoDerivatives 4.0.
Share and Cite
Goy, J.-J.; Ruchat, P.; Stoltc, V.; Schlueter, L.; Berger, A. Percutaneous Closure of Ventricular Septal Defect Following Aortic Valve Replacement. Cardiovasc. Med. 2014, 17, 266. https://doi.org/10.4414/cvm.2014.00270
Goy J-J, Ruchat P, Stoltc V, Schlueter L, Berger A. Percutaneous Closure of Ventricular Septal Defect Following Aortic Valve Replacement. Cardiovascular Medicine. 2014; 17(9):266. https://doi.org/10.4414/cvm.2014.00270
Chicago/Turabian StyleGoy, Jean-Jacques, Patrick Ruchat, Valérie Stoltc, Léopold Schlueter, and Alexandre Berger. 2014. "Percutaneous Closure of Ventricular Septal Defect Following Aortic Valve Replacement" Cardiovascular Medicine 17, no. 9: 266. https://doi.org/10.4414/cvm.2014.00270
APA StyleGoy, J.-J., Ruchat, P., Stoltc, V., Schlueter, L., & Berger, A. (2014). Percutaneous Closure of Ventricular Septal Defect Following Aortic Valve Replacement. Cardiovascular Medicine, 17(9), 266. https://doi.org/10.4414/cvm.2014.00270



