Curing Heart Failure with Cathether Ablation?
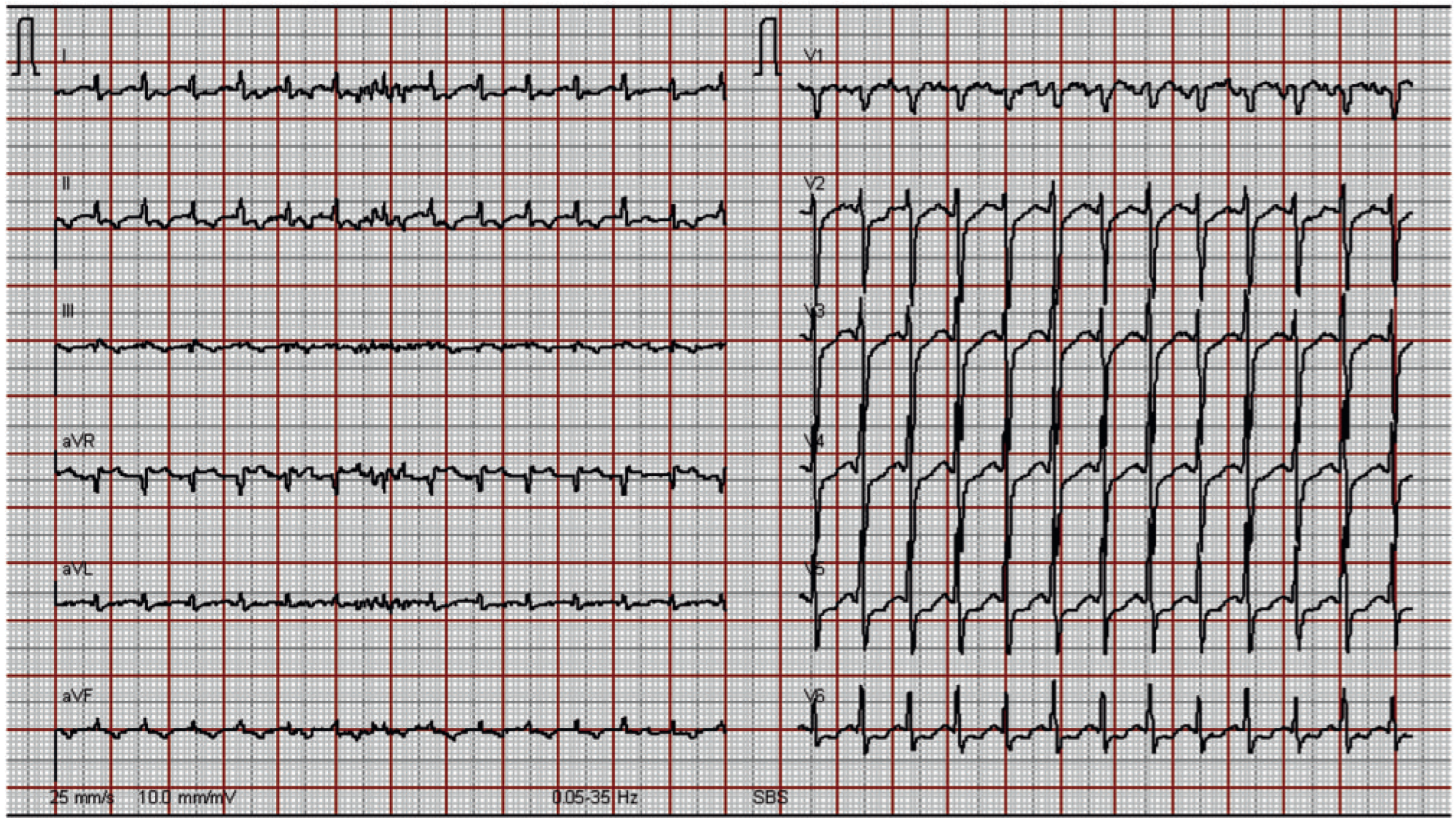
1. Case Presentation
2. Questions
3. Commentary
Conflicts of Interest
References
- Khasnis, A.; Jongnarangsin, K.; Abela, G.; Veerareddy, S.; Reddy, V.; Thakur, R. Tachycardia-induced cardiomyopathy: A review of literature. Pacing Clin Electrophysiol. 2005, 28, 710–721. [Google Scholar] [CrossRef] [PubMed]
- Gopinathannair, R.; Sullivan, R.; Olshansky, B. Tachycardia-mediated cardiomyopathy: Recognition and management. Curr Heart Fail Rep. 2009, 6, 257–264. [Google Scholar] [CrossRef] [PubMed]

© 2010 by the author. Attribution - Non-Commercial - NoDerivatives 4.0.
Share and Cite
Mutschelknauss, M.; Rickenbacher, P.; Kühne, M. Curing Heart Failure with Cathether Ablation? Cardiovasc. Med. 2010, 13, 288. https://doi.org/10.4414/cvm.2010.01528
Mutschelknauss M, Rickenbacher P, Kühne M. Curing Heart Failure with Cathether Ablation? Cardiovascular Medicine. 2010; 13(9):288. https://doi.org/10.4414/cvm.2010.01528
Chicago/Turabian StyleMutschelknauss, Marcus, Peter Rickenbacher, and Michael Kühne. 2010. "Curing Heart Failure with Cathether Ablation?" Cardiovascular Medicine 13, no. 9: 288. https://doi.org/10.4414/cvm.2010.01528
APA StyleMutschelknauss, M., Rickenbacher, P., & Kühne, M. (2010). Curing Heart Failure with Cathether Ablation? Cardiovascular Medicine, 13(9), 288. https://doi.org/10.4414/cvm.2010.01528



