Zusammenfassung
Hintergrund: Seit 1987 werden die perkutanen kardiologischen Eingriffe zur Erkennung aktueller Trends und für den internationalen Vergleich schweizweit erfasst.
Methoden: Basierend auf einem standardisierten Fragebogen wurden alle Zentren, die bei Erwachsenen perkutane kardiologische Eingriffe durchführen, über Umfang und Details ihrer interventionellen Aktivitäten im Jahr 2005 befragt. Die Rücklaufquote der Fragebögen betrug 100%. Die Daten wurden mit denjenigen früherer Jahre verglichen.
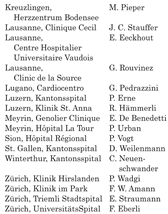
Ergebnisse: Im Jahr 2005 wurden in 5 Universitätsspitälern, 9 öffentlichen, nicht-universitären Zentren und 13 Privatkliniken 36 436 Koronarangiografien (CA) (2004: 35 201; +3,5%) und 16 624 perkutane koronare Interventionen (PCI) (2004: 15 680; + 6%) durchgeführt, dies durch 205 Operateure, von denen 80 ausschliesslich diagnostische Eingriffe durchführten. 93% der PCI wurden ad hoc durchgeführt, und 78% waren EingefässEingriffe. Stents wurden bei 91% aller PCI implantiert (2004: 91%). Medikamenten-beschichtete Stents (drug-eluting stents [DES]) wurden bei 78% der PCI mit Stenting verwendet (2004: 66%). Notfallmässige Eingriffe (primäre PCI oder Rescue-PCI nach Throm-bolyse-Versagen) machten 19% der Untersuchungen aus. Glycoprotein-IIb/IIIa-Antagonisten wurden bei 23% der PCI eingesetzt (2004: 23%). Myokardinfarkte nach PCI wurden auf 1,1% der Eingriffe beziffert, eine notfallmässige aortokoronare Bypass-Operation war in 0,1% der Fälle notwendig, und die Spitalmortalität nach PCI betrug 0,5%.
Zusätzlich wurden 52 Mitralkappen-, 11 Aortenklappenund 16 Pulmonalklappen-Valvuloplastien durchgeführt sowie 510 Eingriffe zum Verschluss eines offenen Foramen ovale und 94 Interventionen zum Verschluss eines Vorhofseptumdefekts.
Schlussfolgerungen: Die Zahl der CA und PCI und vor allem die Verwendung von DES nehmen in der Schweiz stetig zu. Die Zahl der Eingriffe für den Verschluss von offenem Foramen ovale und Vorhofseptumdefekt wächst weiterhin, wahrscheinlich aufgrund einer aggressiveren Abklärung und Behandlung von Patienten mit Hirnschlag.
Schlüsselwörter: Koronarangiographie; Angioplastie; Stents; Ballon-Valvuloplastie; offenes Foramen ovale; Qualitätskontrolle
Introduction
Since 1987, an annual nationwide survey of interventional procedures in all cardiology centres in Switzerland is performed, which allows to recognise contemporary trends and the impact of study results and guidelines on daily practice [
1,
2,
3,
4,
5,
6,
7,
8,
9,
10,
11,
12,
13,
14,
15]. The analysis also serves as an instrument of quality control, which is important in light of the expense and potential of complications of invasive cardiac procedures. The recorded data will also be integrated in the annual survey of the European Society of Cardiology.
The aim of the present study was to provide cardiologist but also other interested physicians with the most recent data on interventional cardiology activities in Switzerland. Importantly, due to the rapid introduction and wide embracement of drug-eluting stents (DES), Switzerland has now a privileged position in this field. Several Swiss cardiology centres have set-up prospective clinical trials investigating important practical issues of DES application [16, 17]. The present data are an important piece of information in the light of these studies and especially the newly detected problem of late and very late stent thrombosis associated with DES [18, 19].
Methods
Based on a standardised questionnaire all cardiology centres performing interventional procedures in adult patients were asked to report on procedures performed during the year 2005. The questionnaire was not sent to the two centres, whose activities are restricted to pediatric patients (Kinderspital Zürich, Kinderspital Bern). The required items included data about infrastructure, operators, availability of cardiac surgery, number of coronary angiographies (CA) and percutaneous coronary interventions (PCI), detailed information about circumstances of PCI (ad hoc interventions, single-vessel PCI, multi-vessel PCI), types of stents (baremetal stents [BMS] or DES) other revascularisation techniques (eg rotablator), adjunctive techniques (eg use of distal protection devices), use of mechanical circulatory support, use of glycoprotein IIb/IIIa inhibitors, number of peripheral and renal artery interventions, number of balloon valvuloplasties, number of interventions for closure of shunts, and complications. As in previous years, the questionnaires were returned by all centres. For some centres, information is not available for all items.
The following definitions were applied:
Coronary angiography (CA)
Diagnostic cardiac catheterisation for visualisation of the coronary arteries, independently whether or not an intervention is performed in the same session. The number of cases is recorded.
Percutaneous coronary intervention (PCI)
Coronary angioplasty with or without stent placement. If PCI is performed directly following the diagnostic procedure during the same session, it is referred to as “ad hoc PCI”. The number of cases, but not the number of vessels dilated is recorded.
Emergency PCI
Primary PCI or rescue PCI after failed thrombolysis for acute ST-segment elevation myocardial infarction (STEMI).
Balloon valvuloplasty
Percutaneous dilatation of stenotic cardiac valves.
Structure of Swiss centres
In 2005, there were 27 active centres (5 university hospitals, 9 public, non-university hospitals, 13 private hospitals), all performing both diagnostic procedures and percutaneous cardiac interventions. The University Hospital Zürich (UniversitätsSpital Zürich [USZ]) and the Kantonsspital Winterthur (KSW) were considered as one centre as there is a close collaboration and exchange of operators between the two hospitals [
15]. Among the 27 centres, 14 work with one catheterisation laboratory, 12 centres have two catheterisation facilities, and there is one centre (USZ/ KSW) with three labs. Eighty (2004: 75) operators perform exclusively diagnostic studies, whereas 125 (2004: 119) cardiologists practice both CA and PCI. In 18 centres, cardiac surgery is available in the same hospital, and 26 centres have an electronic database.
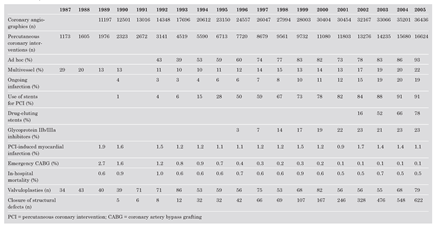
Percutaneous coronary interventions
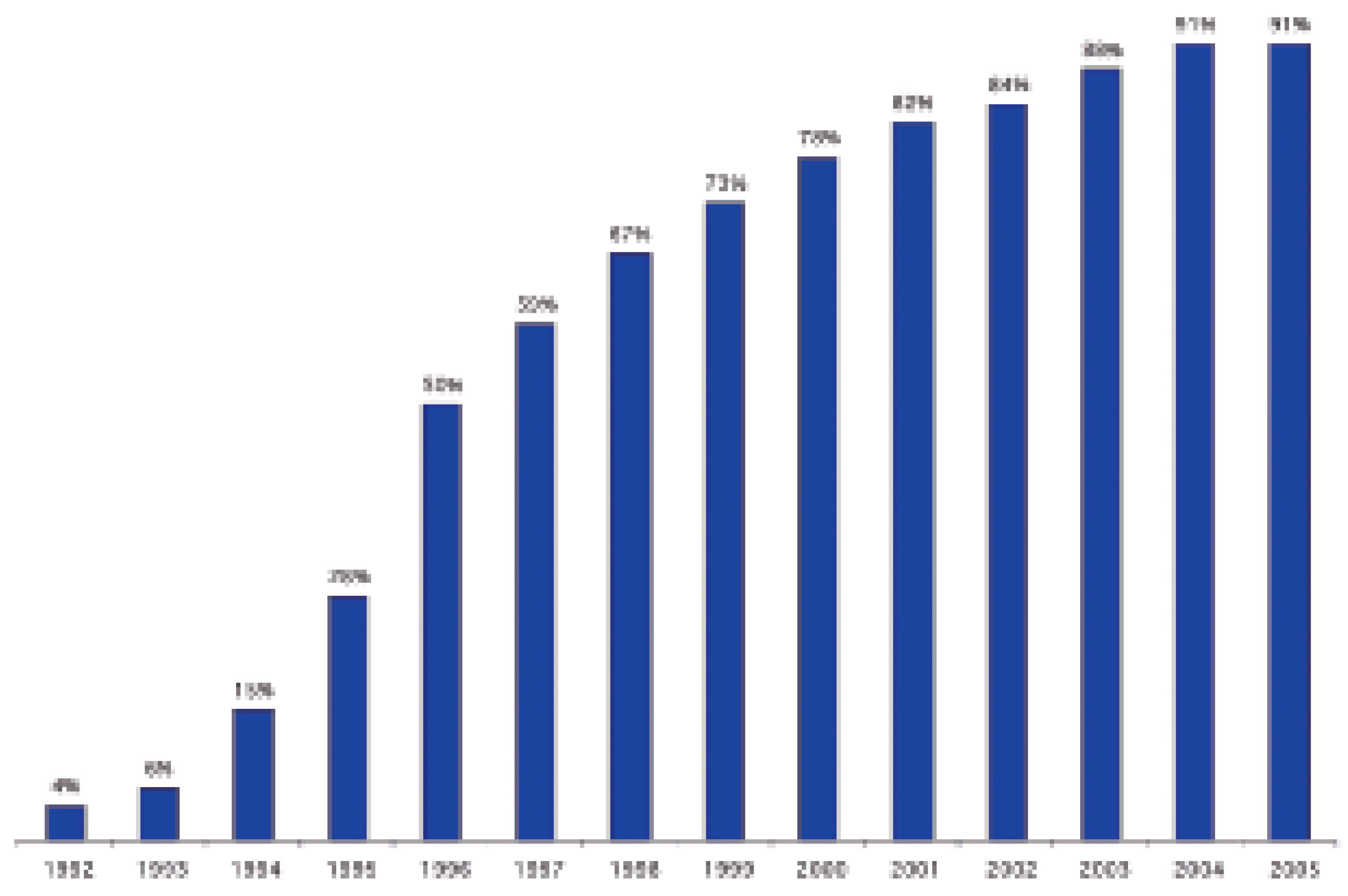
In 2005, 36 436 CA (2004: 35 201; + 3.5%) and 16 624 PCI (2004: 15 680; + 6%) were performed. The evolution of the annual numbers of CA and PCI since 1987 is shown in
Figure 1 and
Table 1. In
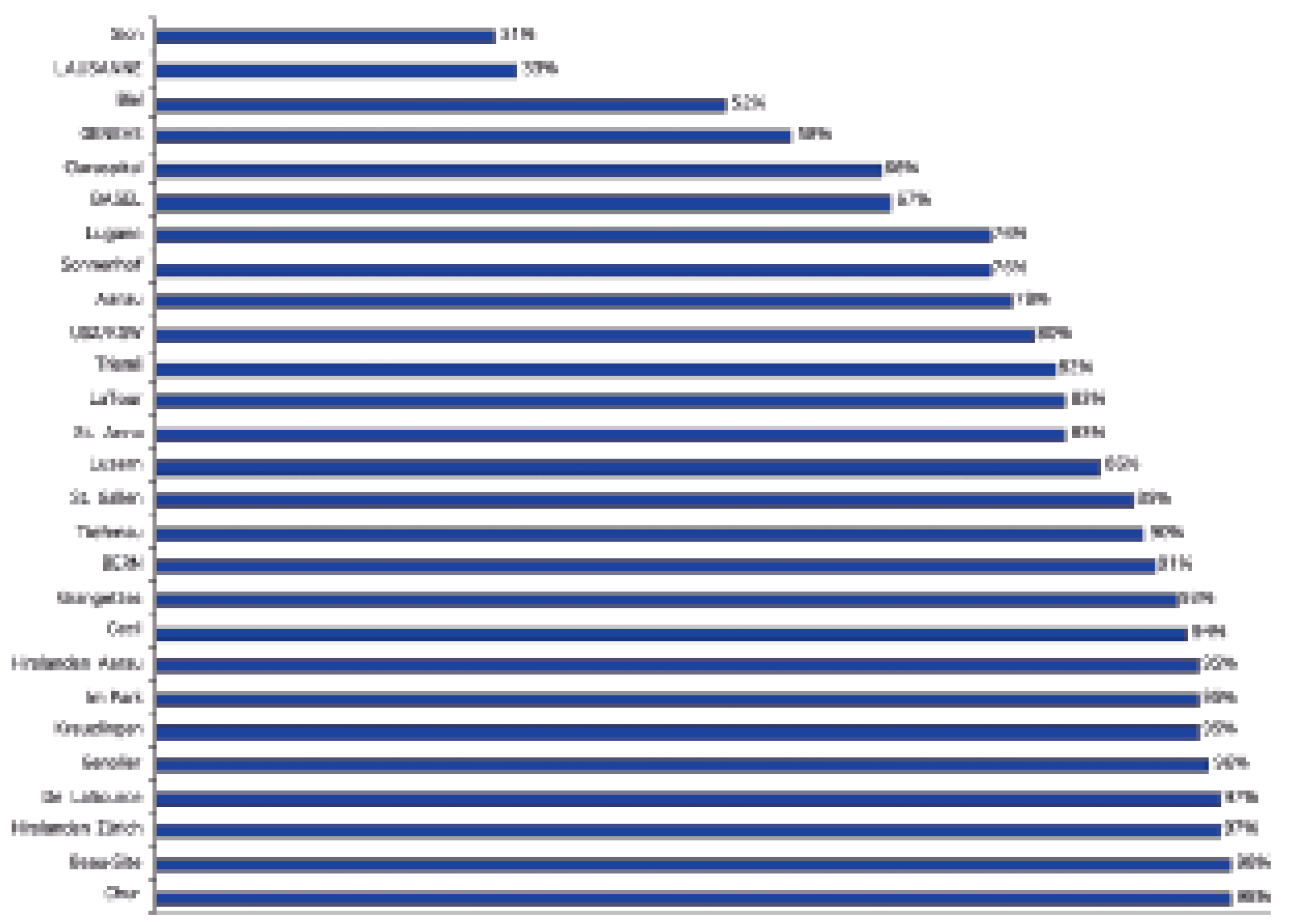
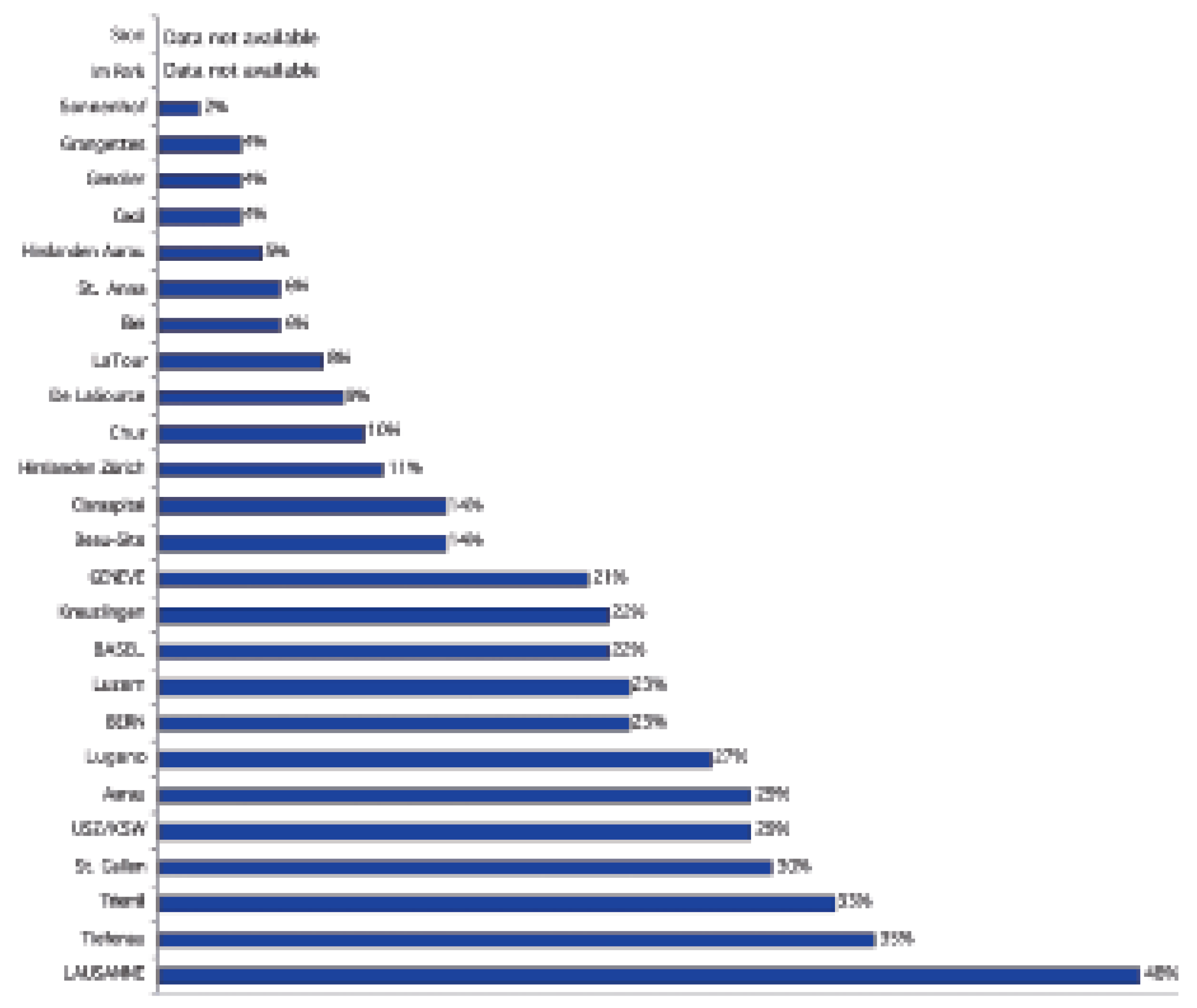
Figure 2, the distribution of all interventions among the different centres is shown. The theoretical numbers of CA and PCI per operator were 178 (2004: 181) and 133 (2004: 132), respectively. There were major differences between the average numbers of examinations per operator among different centres as shown in
Figure 3.
In 15 054/16 126 cases (93%; data not available from one centre), PCI was performed
ad hoc (2004: 86%). The majority of PCI were single-vessel interventions (11 241/14 481; 78%; data not available from three centres; 2004: 80%). The percentage of stents implanted during PCI remained unchanged at 91% (2004: 91%). The evolution of the utilisation of stents from 1992 to 2004 is shown in
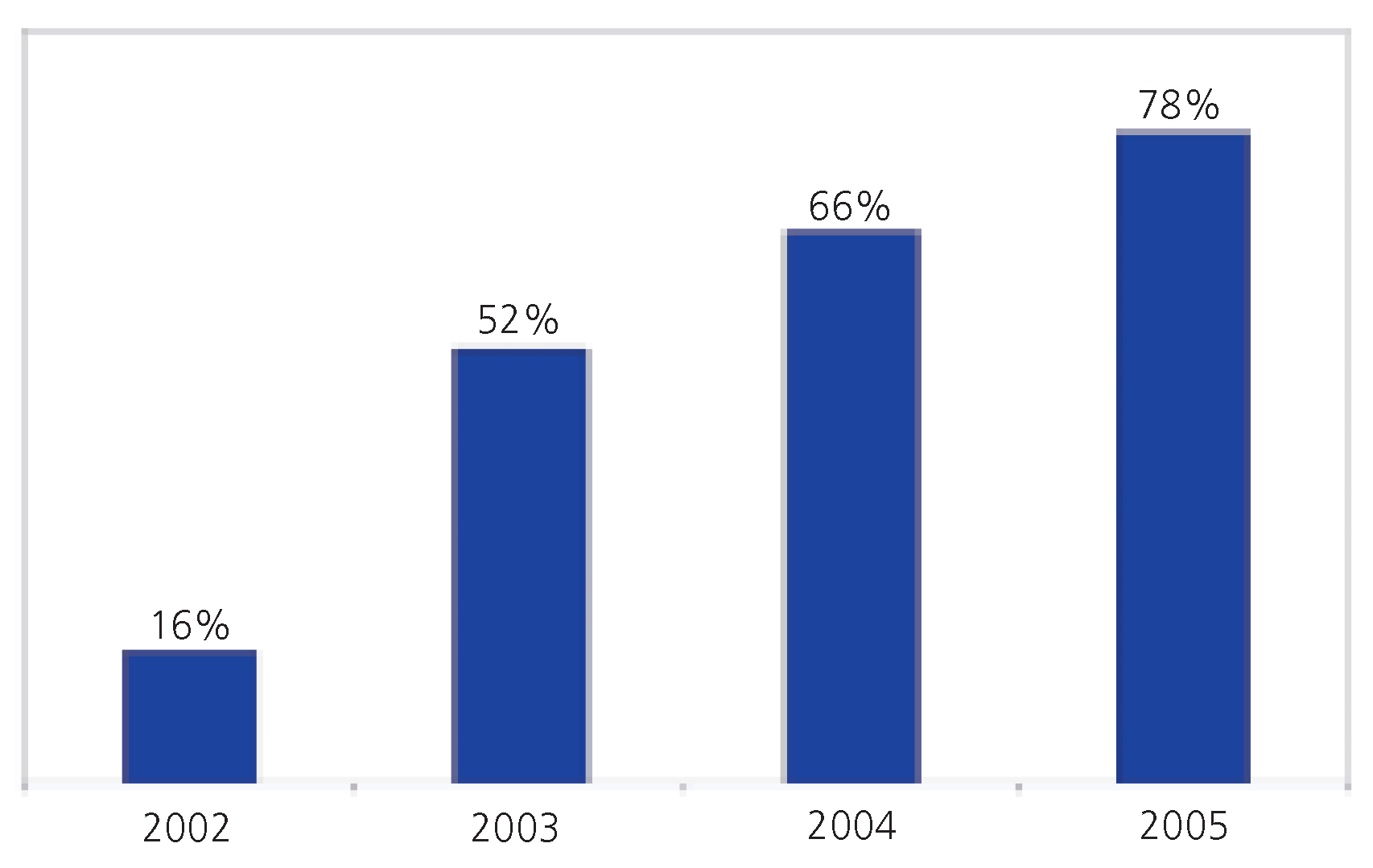
Figure 4. In 7183/12 260 (59%) of stent procedures one single stent was placed, whereas in 5077/12 260 (41%) interventions two or more stents were implanted (data not available from four centres). In 11 871/15 207 (78%) stent procedures, DES were implanted resulting in a further increase of the utilisation of DES compared with previous years (2004: 66%;
Figure 5). The proportion of DES employed for PCI varies considerably among different centres ranging from 31 to 98% as shown in
Figure 6.
Emergency interventions in patients presenting with STEMI (primary PCI or rescue PCI after failed thrombolysis) were reported to account for 3003/15 581 examinations (19%; data not available from two centres). The number of PCI for STEMI among the different centres is shown in
Figure 7.
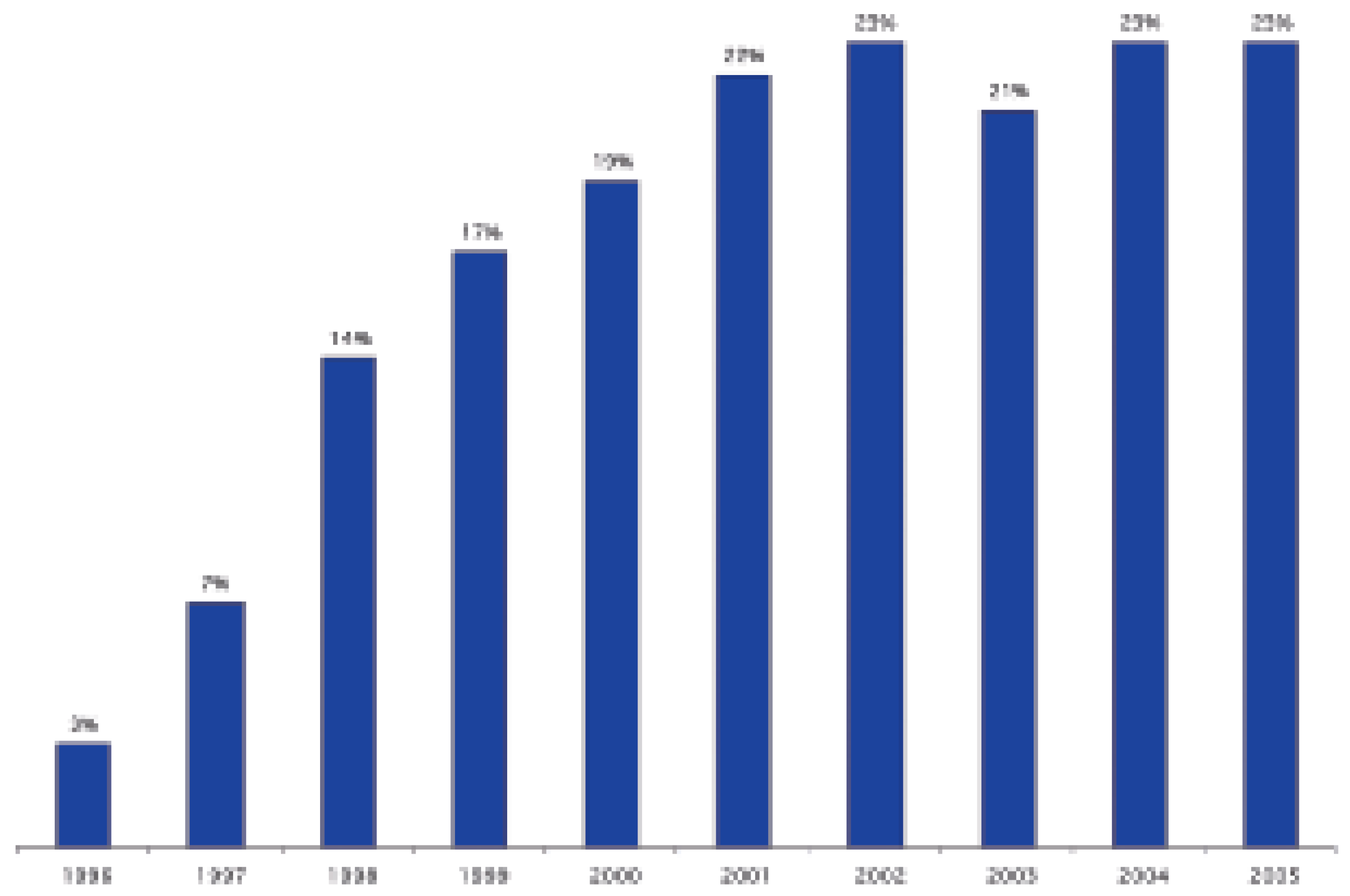
Patients with cardiogenic shock underwent PCI in 226 cases. Glycoprotein IIb/IIIa inhibitors were used in 3623/15 581 (23%; data not available for two centres; 2004: 23%) PCI. Over the last four years, the utilisation rate of glycoprotein IIb/IIIa inhibitors was stable at 21–23% (
Figure 8). However, there are still considerable differences among the different centres with respect to the use of glycoprotein IIb/IIIa inhibitors (
Figure 9).
Distal protection devices were used in 404 (2.4% of PCI; 2004: 480) cases, an intracoronary pressure wire was employed in 436 (2.6%; 2004: 370) cases, and 67 (0.4%; 2004: 59) intracoronary Doppler and 562 (3.4%; 2004: 468) intravascular ultrasound examinations were performed.
Revascularisation techniques other than balloon angioplasty including rotablator (59 cases; 2004: 40), sonotherapy (14 cases, 2004: 0 patients), or laser wire recanalisation (1 case, 2004: 0 patients) have rarely been applied. Atherectomy has not been done in any patient (2004: 0). The number of cases with application of intracoronary brachytherapy has further decreased from 35 in 2004 to 17 cases in 2005. There was an increase in the use of mechanical circulatory support systems consisting of 436 (2004: 332) intraaortic balloon pumps and 37 (2004: 10) percutaneous left ventricular assist devices.
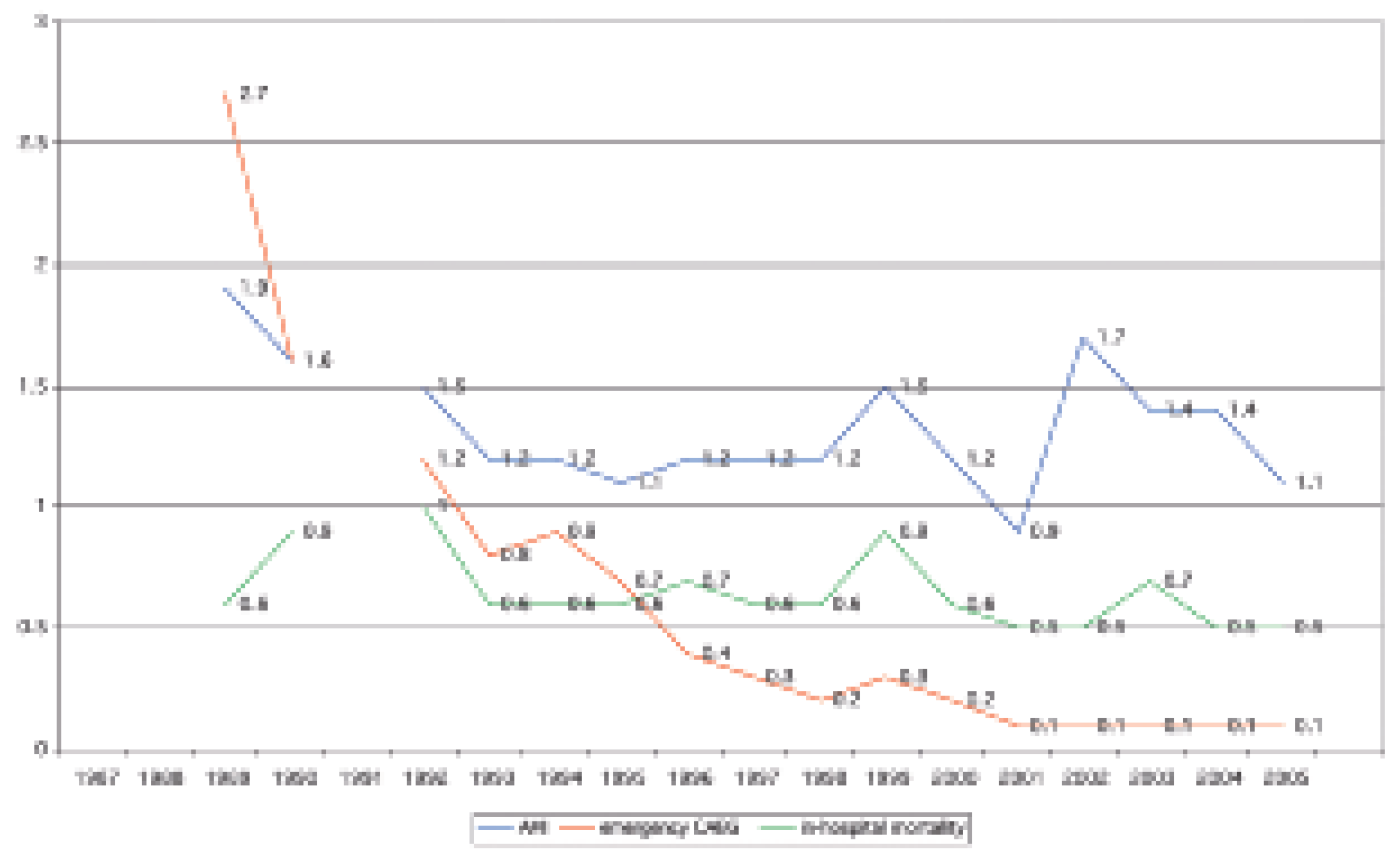
Complications after PCI
Myocardial infarction after PCI was reported in 179/16 624 (1.1%; 2004: 1.4%) cases, emergency coronary artery bypass grafting was needed in 21/16 624 (0.1%; 2004: 0.1%) patients, and 87 (2004: 86) patients were reported to have died during the in-hospital period following PCI. Thus, the mortality rate after PCI is approximately 0.5% (2004: 0.5%). The reported rate of complications after PCI since 1987 is shown in
Figure 10.
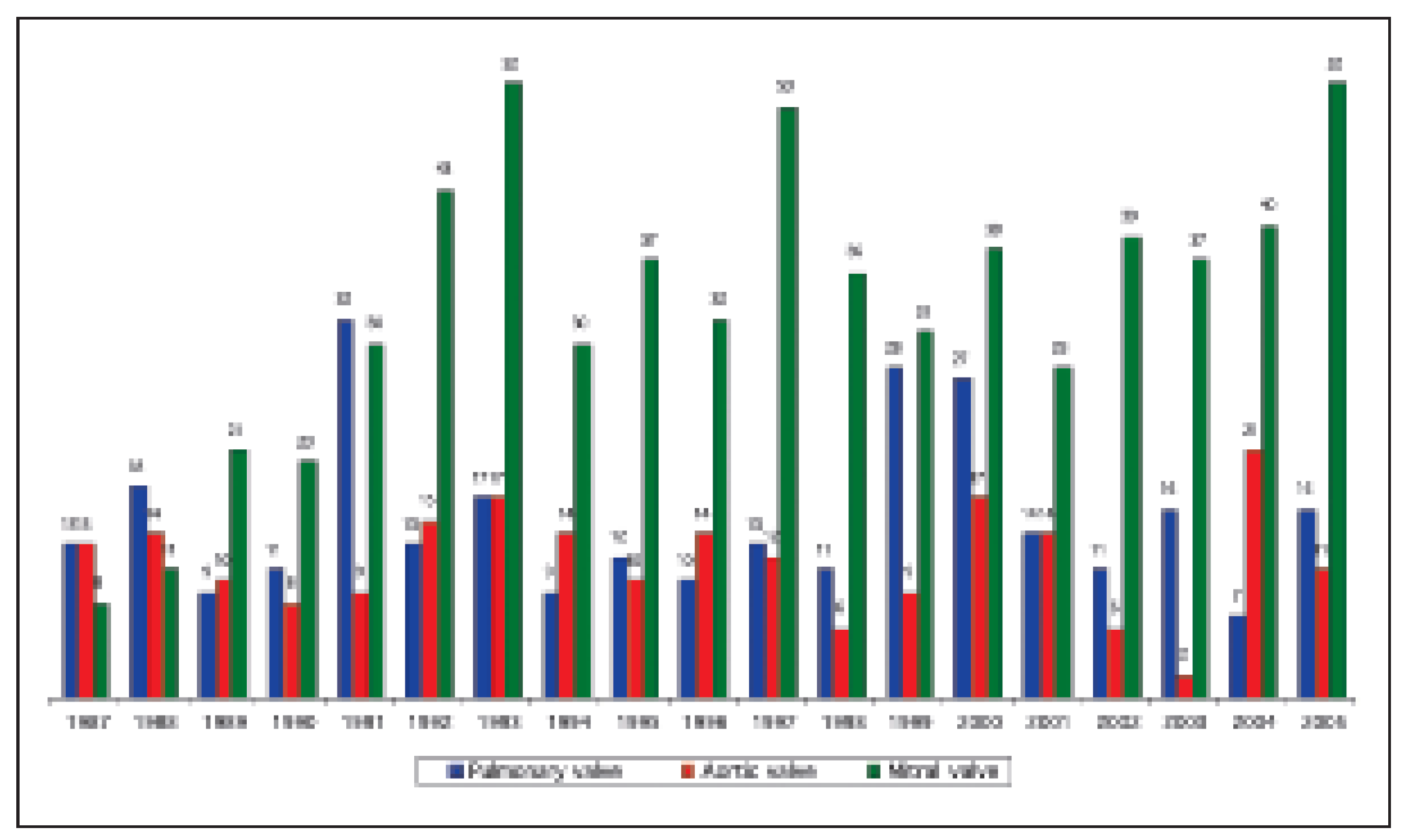
Non-coronary interventions
The number of balloon valvuloplasties did not significantly differ from previous years (
Figure 11). In contrast, the number of procedures for closure of structural defects, especially for patent foramen ovale (PFO), is steadily increasing over the last years (
Figure 12).
Peripheral angioplasties are carried out by radiologists and angiologists in most hospitals. However, cardiologist reported 197 iliac or lower extremity interventions (57% with stent placement), 93 carotid artery angioplasties (81% with stent implantation), and 152 renal artery interventions (82% with stent placement). In addition, alcohol ablation of septal hypertrophy was done in 17 patients.
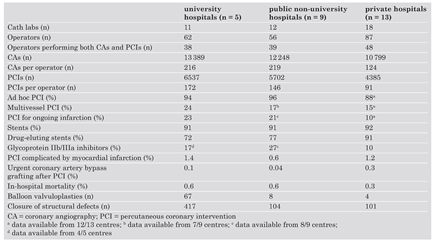
Comparison between university, non-university public, and private hospitals
In
Table 2, there is a comparison of university hospitals, non-university hospitals, and private hospitals with respect to infrastructure, procedures, and complications. When referring to the data from 2004 [
15], it becomes obvious that especially in public non-university hospitals and private hospitals the number of CA and PCI is continuously growing. Interestingly, glycoprotein IIb/IIIa inhibitors were more frequently applied in public non-university hospitals as compared to university hospitals despite similar rates of PCI for STEMI. The DES utilisation rate is higher in private hospitals as compared to university and nonuniversity public hospitals.
Discussion
Despite the retrospective nature of this study with its inherent limitations, the present survey closely mirrors daily practice in interventional cardiology in Switzerland. In 2005, similar trends as in the previous year could be observed: the number of CA and PCI is still slightly growing, and the use of DES and the number of interventions for PFO closure are steadily increasing.
In our last report, we have extensively discussed the current Swiss practice of interventional cardiology in the light of the guidelines of the European Society of Cardiology [
20]. In this context, there are no entirely novel aspects. Accordingly, we herein focus on two particularly pertinent topics,
ie DES utilisation and management of PFO.
DES utilisation in Switzerland
There was no further increase in the percentage of interventions with stent placement within the last three years, which is likely related to technical limitations (small vessels, tortuous vessels, proximal stent with the impossibility to deploy a stent distally) rather than lack of indication. In contrast, the DES utilisation rate increased from 52% in 2003 to currently 78% in 2005. This is not surprising when one considers the dramatic benefit in terms of both angiographic (late lumen loss) and clinical (target vessel revascularisation) endpoints observed in large trials with medium-term follow-up [21, 22]. In fact, the problem of instent-restenosis has almost disappeared in daily practice, and alternative procedures to resolve this problem (ie brachytherapy) have hardly ever been performed during the year 2005. However, in most other European countries the introduction of DES was much slower (
eg 28% DES utilisation in Germany in 2005 [
23]), most probably due to financial constraints. Thus, Switzerland has an exceptional position with a comparatively large experience with DES use. There is still some variation in the DES utilisation in different Swiss centres as shown in
Figure 6. However, at least three quarters of all centres have a DES rate ≥75%.
Results from prospective studies on DES in Switzerland
The non-restricted application of DES provided the unique opportunity for Swiss cardiology centres to be among the first to set-up prospective, randomised studies evaluating the benefit of DES in real world patients. The SIRTAX study found that a sirolimus-eluting stent is superior to a paclitaxel-eluting stent with respect to clinical and angiographic measures of restenosis [16]. The BASKET trial revealed that in an “all-comers” setting, the higher costs for DES as compared to BMS were not compensated by lower follow-up costs at six months, and that DES are only cost effective for elderly patients in specific high-risk groups [17]. The long-term follow-up of these studies however, revealed that DES are not only associated with high cost, but also late stent thrombosis, an unpredictable and sometimes fatal event. Therefore, it seems prudent to revisit the indication of DES in daily practice and to carefully weigh the risks and benefits of DES [18, 19].
DES: implications for future practice
After DES implantation dual antiplatelet therapy is required for several months. It is currently unclear how long both aspirin and clopidogrel must be given to safely prevent late DES stent thrombosis, or whether it can not be prevented at all. Dual antiplatelet therapy however, is associated with an increased risk of bleeding and is difficult to manage in patients also requiring oral anticoagulation (eg for atrial fibrillation or recurrent thrombosis / pulmonary embolism). There is an ongoing debate on a more strict definition of indications and especially contraindications for DES placement.
Non-coronary interventions
The number of balloon valvuloplasties did not significantly change as compared to previous years, probably due to the fact that the diagnosis of congenital or rheumatic valve disease in adults has become rare. In contrast, PFO is a frequent anatomical variant, and due to the more aggressive diagnostic approach in patients with stroke, the condition is more frequently detected. Indications for PFO closure are still under debate, and there is no consensus of optimal management of patients with PFO and stroke. Some authors recommend that high risk features including a temporal association between Valsalva-inducing manoeuvres and stroke, a co-existing hypercoagulable state, recurrent strokes, PFO with large opening, large right-to-left shunt, or right-toleft shunt at rest, or atrial septal aneurysma, should prompt PFO closure [
24]. In contrast, others restrict PFO closure to patients with recurrence of stroke despite therapeutic anticoagulation [
25]. In practice, PFO closure is often much more liberal, as it is difficult not to perform the intervention after PFO has been detected since not only referring physicians but also patients want the “hole in the heart” to be closed. Until further studies clarify indications for PFO closure, a further increase in the number of interventions can be expected.
Limitations of the study
Due to the retrospective nature of the study, some inaccuracies must be assumed. Although he study reflects the practice of interventional cardiology in Switzerland, especially the reported rate of periprocedural complications must be interpreted with caution. A catheterisation laboratory-based retrospective analysis is unlikely to be complete, and we can assume that only complications occurring immediately at the time of catheterisation will have been included. Regarding the high mortality of patients undergoing PCI for cardiogenic shock, these patients have probably not been included into the statistics. In addition, non-obvious complications such as contrast nephropathy will haven been missed. Therefore, a more comprehensive data collection with respect to complications is planned based on a work sheet discussed at the business meeting of the Working Group in 2005 in Lausanne. This sheet has been sent to all centres to be included in the local databases on an optional base.
In addition, despite a more stringent definition of the term “emergency procedures” in the questionnaire (“PCI for STEMI”), a similar number of such interventions was reported when compared to the year 2004, indicating that not only PCI for STEMI but also other urgent interventions might have been reported.
During the writing process we were aware that the activities of the new cath lab in the Lindenhofspital in Berne have not been included in the analysis. Of course, this cath lab should also be included in future surveys.
Conclusions
The number of CA and PCI and the use of DES increased steadily during the last years. Due to full reimbursement of DES, Switzerland has an exceptionally high DES utilisation rate. Given the new problem of late stent thrombosis, DES utilisation might change in coming years. There is also a significant increase in number of interventions for PFO closure, which is probably due to a more aggressive diagnostic approach in patients with stroke.