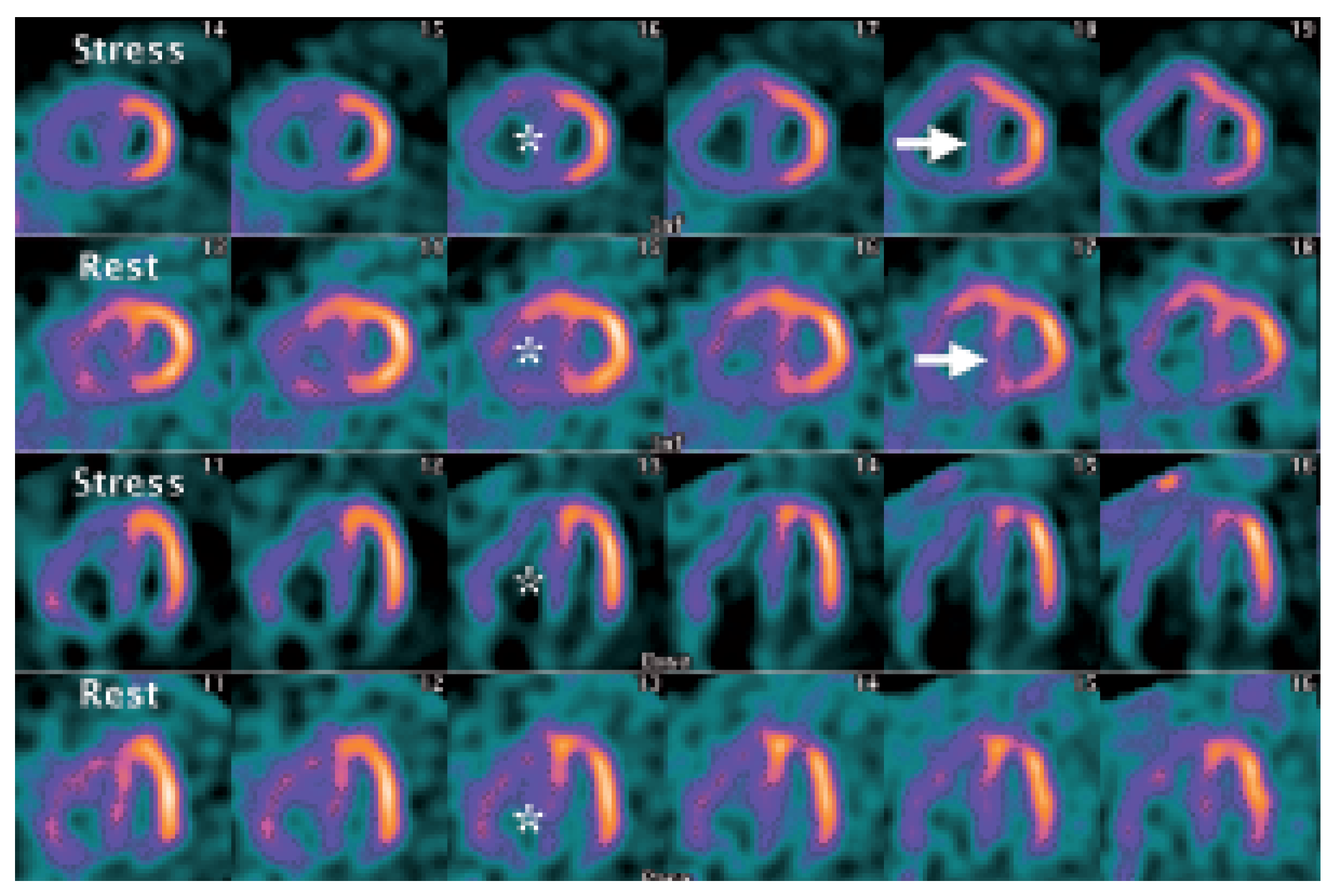
Myocardial Perfusion SPECT Features of Severe Pulmonary Artery Hypertension
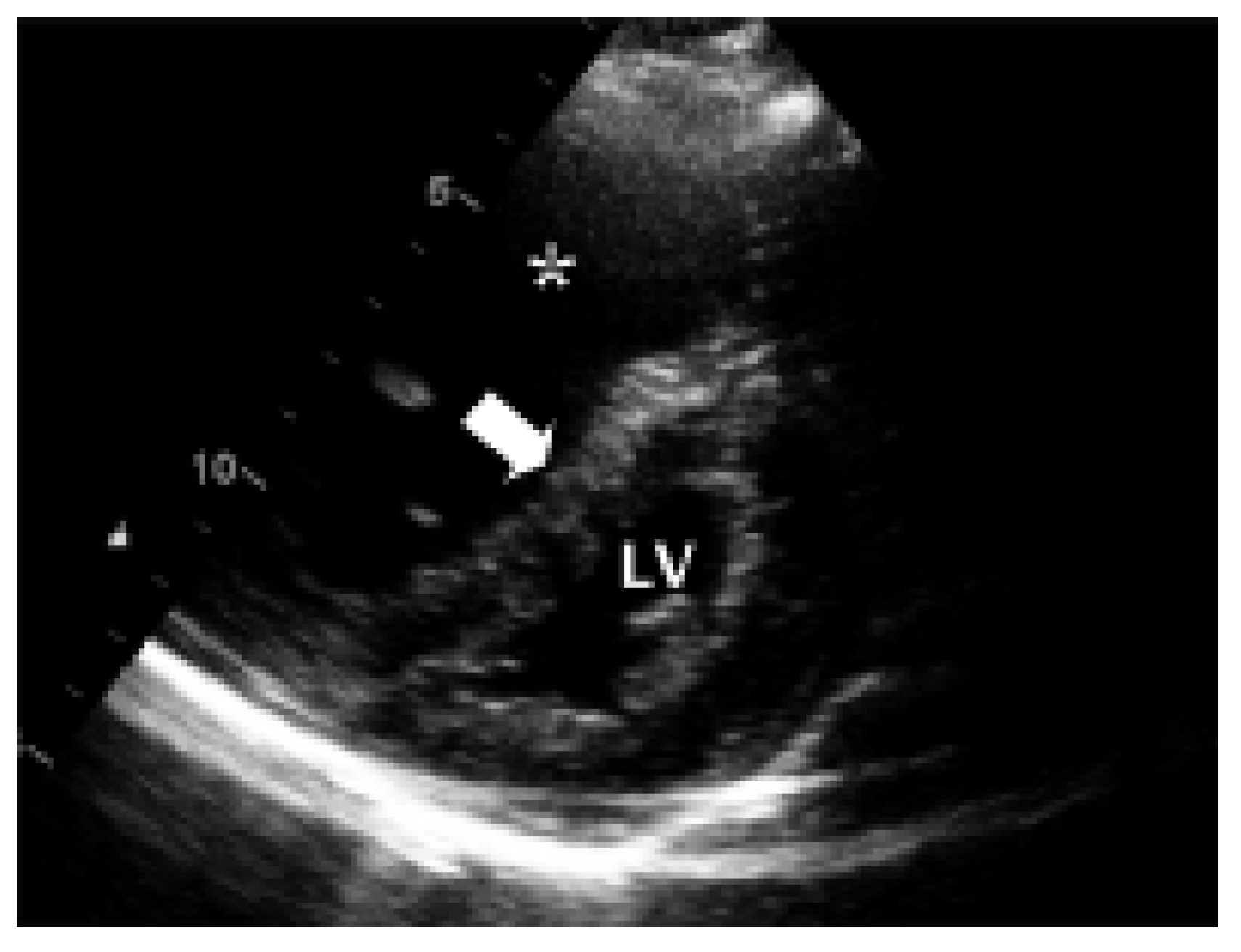
Case Report
Discussion
Conflicts of Interest
References
- Khaja, F.; Alam, M.; Goldstein, S.; Anbe, D.T.; Marks, D.S. Diagnostic value of visualization of the right ventricle using thallium-201 myocardial imaging. Circulation 1979, 59, 182–188. [Google Scholar] [CrossRef]
- Movahed, M.R.; Hepner, A.; Lizotte, P.; Milne, N. Flattening of the interventricular septum (D-shaped left ventricle) in addition to high right ventricular tracer uptake and increased right ventricular volume found on gated SPECT studies strongly correlates with right ventricular overload. J. Nucl. Cardiol. 2005, 12, 428–434. [Google Scholar] [CrossRef] [PubMed]
- Gibbons Kroeker, C.A.; Adeeb, S.; Shrive, N.G.; Tyberg, J.V. Compression induced by RV pressure overload decreases regional coronary blood flow in anaesthetised dogs. Am. J. Physiol. Heart Circ. Physiol. 2006, 290, H2432–H2438. [Google Scholar] [CrossRef] [PubMed]

© 2007 by the author. Attribution - Non-Commercial - NoDerivatives 4.0.
Share and Cite
Maeder, M.T.; Stöckli, M.; Zellweger, M.J. Myocardial Perfusion SPECT Features of Severe Pulmonary Artery Hypertension. Cardiovasc. Med. 2007, 10, 113. https://doi.org/10.4414/cvm.2007.01234
Maeder MT, Stöckli M, Zellweger MJ. Myocardial Perfusion SPECT Features of Severe Pulmonary Artery Hypertension. Cardiovascular Medicine. 2007; 10(3):113. https://doi.org/10.4414/cvm.2007.01234
Chicago/Turabian StyleMaeder, Micha T., Martin Stöckli, and Michael J. Zellweger. 2007. "Myocardial Perfusion SPECT Features of Severe Pulmonary Artery Hypertension" Cardiovascular Medicine 10, no. 3: 113. https://doi.org/10.4414/cvm.2007.01234
APA StyleMaeder, M. T., Stöckli, M., & Zellweger, M. J. (2007). Myocardial Perfusion SPECT Features of Severe Pulmonary Artery Hypertension. Cardiovascular Medicine, 10(3), 113. https://doi.org/10.4414/cvm.2007.01234



