Protective Factors for Falls Among Independent Older Adults: A Cross-Sectional Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
2.2. Population and Sampling
2.3. Instruments and Measurements
2.3.1. Sociodemographic, Health-Related Data, and Behavioral Factors
2.3.2. Fall History
2.3.3. Environmental Assessment
2.4. Data Collection Procedure
2.5. Ethics Approval and Consent to Participate
2.6. Data Analysis
3. Results
3.1. Characteristic Data
3.2. Fall Prevalence and Circumstances
3.3. Factors Associated with Falls
3.4. Multivariate Logistic Regression
4. Discussion
4.1. Contextualizing the Fall Prevalence
4.2. Key Protective Factors and Novel Insights
4.3. Non-Significant Factors and Contrasts with Prior Research
4.4. Contribution to International Research
4.5. Limitations and Strengths
- It addresses a research gap in fall risk among functionally independent, rural older adults, a population often underrepresented in fall studies;
- It identifies non-conventional protective factors such as agricultural work and pet ownership that may be more feasible and culturally relevant in rural communities;
- The use of multivariate analysis strengthens the validity of identified associations and provides evidence for targeted policy and intervention development. This study reveals key protective factors that can inform context-sensitive policy development aimed at preventing falls among non-dependent older adults living in rural areas. Importantly, protective elements such as physical activity through agricultural work, financial stability, and emotional support from pet ownership emerged as modifiable factors. These may serve as strategic targets for culturally grounded, community-based fall prevention interventions.
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Ageing and Health. Available online: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health (accessed on 10 February 2025).
- Xiao, Z.; Wu, W.; Zhao, Q.; Zhang, J.; Hong, Z.; Ding, D. Sensory impairments and cognitive decline in older adults: A review from a population-based perspective. Aging Health Res. 2021, 1, 100002. [Google Scholar] [CrossRef]
- Manini, T.M.; Pahor, M. Physical activity and maintaining physical function in older adults. Br. J. Sports Med. 2009, 43, 28–31. [Google Scholar] [CrossRef]
- Li, Y.; Hou, L.; Zhao, H.; Xie, R.; Yi, Y.; Ding, X. Risk factors for falls among community-dwelling older adults: A systematic review and meta-analysis. Front. Med. 2023, 9, 1019094. [Google Scholar] [CrossRef]
- World Health Organization. Falls: Fact Sheet; World Health Organization: Geneva, Switzerland, 2021; Available online: https://www.who.int/news-room/fact-sheets/detail/falls (accessed on 8 October 2024).
- Tinetti, M.E.; Kumar, C. The patient who falls: “It’s always a trade-off”. JAMA 2010, 303, 258–266. [Google Scholar] [CrossRef]
- Ambrose, A.F.; Paul, G.; Hausdorff, J.M. Risk factors for falls among older adults: A review of the literature. Maturitas 2013, 75, 51–61. [Google Scholar] [CrossRef] [PubMed]
- Talarska, D.; Strugała, M.; Szewczyczak, M.; Tobis, S.; Michalak, M.; Wróblewska, I.; Wieczorowska-Tobis, K. Is independence of older adults safe considering the risk of falls? BMC Geriatr. 2017, 17, 66. [Google Scholar] [CrossRef] [PubMed]
- Sherrington, C.; Fairhall, N.J.; Wallbank, G.K.; Tiedemann, A.; Michaleff, Z.A.; Howard, K.; Clemson, L.; Hopewell, S.; Lamb, S.E. Exercise for preventing falls in older people living in the community. Cochrane Database Syst. Rev. 2019, 1, CD012424. [Google Scholar] [CrossRef] [PubMed]
- Warrington, D.J.; Shortis, E.J.; Whittaker, P.J. Are wearable devices effective for preventing and detecting falls: An umbrella review (a review of systematic reviews). BMC Public Health 2021, 21, 2091. [Google Scholar] [CrossRef]
- Bergen, G.; Stevens, M.R.; Burns, E.R. Falls and fall injuries among adults aged ≥ 65 years—United States, 2014. MMWR Morb. Mortal. Wkly. Rep. 2016, 65, 993–998. [Google Scholar] [CrossRef]
- Lord, S.R.; Sherrington, C.; Menz, H.B.; Close, J.C.T. Falls in Older People: Risk Factors and Strategies for Prevention, 2nd ed.; Cambridge University Press: Cambridge, UK, 2007. [Google Scholar]
- El-Khoury, F.; Cassou, B.; Charles, M.A.; Dargent-Molina, P. The effect of fall prevention exercise programmes on fall induced injuries in community dwelling older adults: Systematic review and meta-analysis of randomised controlled trials. BMJ 2013, 347, f6234. [Google Scholar] [CrossRef]
- Kim, T.; Choi, S.D.; Xiong, S. Epidemiology of fall and its socioeconomic risk factors in community-dwelling Korean elderly. PLoS ONE 2020, 15, e0234787. [Google Scholar] [CrossRef]
- Brown, J.; Hirsch, J.A.; Tabb, L.P.; Judd, S.E.; Bennett, A.; Rundle, A.; Lovasi, G.S. A Segmented Regression Analysis of House-hold Income and Recurrent Falls Among Adults in a National Cohort Study. Am. J. Epidemiol. 2024, 193, 516–526. [Google Scholar] [CrossRef]
- Chen, X.; Lin, Z.; Gao, R.; Yang, Y.; Li, L. Prevalence and Associated Factors of Falls among Older Adults between Urban and Rural Areas of Shantou City, China. Int. J. Environ. Res. Public Health 2021, 18, 7050. [Google Scholar] [CrossRef]
- Atoyebi, O.A.; Elegbede, O.; Babatunde, O.A.; Adewoye, K.; Durowade, K.; Parakoyi, D.B. Prevalence and risk factors for falls in urban and rural older adults in Ekiti State. Nigeria. Ghana Med. J. 2021, 55, 265–272. [Google Scholar] [CrossRef]
- World Health Organization. Thailand’s Leadership and Innovations Towards Healthy Ageing. Available online: https://www.who.int/southeastasia/news/feature-stories/detail/thailands-leadership-and-innovation-towards-healthy-ageing (accessed on 25 January 2025).
- Phumplab, M. Thai Industrial Policies Towards the Challenges of an Aging Society. Jpn. Spotlight 2023, 42, 28–33. [Google Scholar]
- Department of Disease Controls, Ministry of Public Health, Thailand. Falls Data: Statistics on Falls. Available online: https://ddc.moph.go.th/dip/news.php?news=23567&deptcode= (accessed on 10 March 2025). (In Thailand)
- Zhang, L.; Ding, Z.; Qiu, L.; Li, A. Falls and risk factors of falls for urban and rural community-dwelling older adults in China. BMC Geriatr. 2019, 19, 379. [Google Scholar] [CrossRef] [PubMed]
- Boonkhao, L.; Choochouy, N.; Rattanachaikunsopon, P.; Laosupap, K.; Saenrueang, T.; Labcom, C.; Chakharum, N.; Boonsang, A.; Butsorn, A. Exploring factors contributing to falls in home-dwelling older adults: A cross-sectional study in Northeastern Thailand. Narra J. 2025, 5, e1545. [Google Scholar] [CrossRef] [PubMed]
- Tonchoy, P.; Tonchoy, P.; Seangpraw, K.; Ong-Artborirak, P.; Kantow, S.; Auttama, N.; Choowanthanapakorn, M.; Boonyathee, S. Mental health, fall prevention behaviors, and home environments related to fall experiences among older adults from ethnic groups in rural Northern Thailand. Heliyon 2024, 10, e37306. [Google Scholar] [CrossRef] [PubMed]
- Pantong, U.; Trapero, I.; Jareaprapal, U. Analysis and prevention of falls among community-dwelling older adults in southern Thailand. J. Adv. Nurs. 2024, 80, 2121–2136. [Google Scholar] [CrossRef]
- Kunset, P.; Punsawad, C.; Petsirasan, R.; Suwanbamrung, C.; Shohaimi, S.; Narkkul, U.; Noonil, N. Unhealthy dietary patterns and their associations with sociodemographic factors as predictors among underweight and overweight adolescents in southern Thailand. Int. J. Environ. Res. Public Health 2023, 20, 6703. [Google Scholar] [CrossRef]
- Hucteau, E.; Noize, P.; Pariente, A.; Helmer, C.; Pérès, K. ADL-dependent older adults were identified in medico-administrati ve databases. J. Clin. Epidemiol. 2021, 139, 297–306. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Buchner, A.; Lang, A.G. Statistical power analyses using G* Power 3.1: Tests for correlation and regress ion analyses. Behav. Res. Methods 2009, 41, 1149–1160. [Google Scholar] [CrossRef]
- Graf, C. The Lawton instrumental activities of daily living (IADL) scale. Medsurg. Nurs. 2009, 18, 315–316. [Google Scholar] [PubMed]
- World Health Organization. WHO Global Report on Falls Prevention in Older Age, 1st ed.; World Health Organization: Geneva, Switzerland, 2007; pp. 1–47. [Google Scholar]
- Ang, G.C.; Low, S.L.; How, C.H. Approach to falls among the elderly in the community. Singap. Med. J. 2020, 61, 116–121. [Google Scholar] [CrossRef] [PubMed]
- Nevitt, M.C.; Cummings, S.R.; Kidd, S.; Black, D. Risk factors for recurrent nonsyncopal falls: A prospective study. JAMA 1989, 261, 2663–2668. [Google Scholar] [CrossRef] [PubMed]
- Qian, X.X.; Chau, P.H.; Kwan, C.W.; Lou, V.W.; Leung, A.Y.; Ho, M.; Fong, D.Y.; Chi, I. Investigating risk factors for falls among community-dwelling older adults according to WHO’s risk factor model for falls. J. Nutr. Health Aging 2021, 25, 425–432. [Google Scholar] [CrossRef]
- Campani, D.; Caristia, S.; Amariglio, A.; Piscone, S.; Ferrara, L.I.; Barisone, M.; Bortoluzzi, S.; Faggiano, F.; Molin, A.D. Home and environmental hazards modification for fall prevention among the elderly. Public Health Nurs. 2020, 38, 493. [Google Scholar] [CrossRef]
- Keglovits, M.; Clemson, L.; Hu, Y.L.; Nguyen, A.; Neff, A.J.; Mandelbaum, C.; Hudson, M.; Williams, R.; Silianoff, T.; Stark, S. A scoping review of fall hazards in the homes of older adults and development of a framework for assessment and intervention. Aust. Occup. Ther. J. 2020, 67, 470–478. [Google Scholar] [CrossRef]
- Landis, J.R.; Koch, G.G. The measurement of observer agreement for categorical data. Biometrics 1977, 33, 159–174. [Google Scholar] [CrossRef]
- Choi, E.J.; Kim, S.A.; Kim, N.R.; Rhee, J.A.; Yun, Y.W.; Shin, M.H. Risk factors for falls in older Korean adults: The 2011 Community 423 Health Survey. J. Korean Med. Sci. 2014, 29, 1482–1487. [Google Scholar] [CrossRef]
- Masumoto, T.; Yamada, Y.; Yamada, M.; Nakaya, T.; Miyake, M.; Watanabe, Y.; Yoshida, T.; Yokoyama, K.; Yamagata, E.; Date, H.; et al. Fall risk factors and sex differences among community-dwelling elderly individuals in Japan: A Kameoka study. Nihon Koshu Eisei Zasshi 2015, 62, 390–401. [Google Scholar] [CrossRef]
- Zhang, K.; Yang, Z.; Zhang, X.; Li, L. Comparison of falls and risk factors among older adults in urban villages, urban and rural areas of Shantou, China. Heliyon 2024, 10, e30536. [Google Scholar] [CrossRef]
- Reyes-Ortiz, C.A.; Al Snih, S.; Markides, K.S. Falls among elderly persons in Latin America and the Caribbean and among elderly Mexican-Americans. Rev. Panam. Salud Publica 2005, 17, 362–369. [Google Scholar] [CrossRef] [PubMed]
- Meucci, R.D.; Runzer-Colmenares, F.M.; Parodi, J.F.; de Mola, C.L. Falls among the elderly in Peruvian Andean communities and the Rural far South of Brazil: Prevalence and associated factors. J. Community Health 2020, 45, 363–369. [Google Scholar] [CrossRef] [PubMed]
- Adanusa, M.; Pobee, S.K.; Zaabaar, E.; Mawuko, V.; Asiedu, K.; Amuzu, S.K.; Adubofour, W.; Bazayeya, C.; Senaya, E.E.Y.; Ofori, D.C.; et al. Prevalence and risk factors for falls among older adults in a primary care facility in Ghana. Malawi Med. J. 2022, 34, 225–230. [Google Scholar] [CrossRef] [PubMed]
- Lytras, D.; Sykaras, E.; Iakovidis, P.; Kasimis, K.; Myrogiannis, I.; Kottaras, A. Recording of falls in elderly fallers in Northern Greece and evaluation of aging health-related factors and environmental safety associated with falls: A cross-sectional study. Occup. Ther. Int. 2022, 2022, 9292673. [Google Scholar] [CrossRef]
- Iamtrakul, P.; Chayphong, S.; Jomnonkwao, S.; Ratanavaraha, V. The association of falls risk in older adults and their living environment: A case study of rural area, Thailand. Sustainability 2021, 13, 13756. [Google Scholar] [CrossRef]
- Lee, S.; Lee, C.; Rodiek, S. Neighborhood Factors and Fall-Related Injuries among Older Adults Seen by Emergency Medical Service Providers. Int. J. Environ. Res. Public Health 2017, 14, 163. [Google Scholar] [CrossRef]
- Howe, T.E.; Rochester, L.; Neil, F.; Skelton, D.A.; Ballinger, C. Exercise for Improving Balance in Older People. Cochrane Database Syst. Rev. 2011, 2012, CD004963. [Google Scholar] [CrossRef]
- Gavarkovs, A.G.; Burke, S.M.; Petrella, R.J. The Physical Activity-Related Barriers and Facilitators Perceived by Men Living in Rural Communities. Am. J. Mens Health 2017, 11, 1130–1132. [Google Scholar] [CrossRef]
- Yuan, Y.; Li, J.; Fu, P.; Jing, Z.; Wang, Y.; Zhou, C. Association between physical activity and falls among older adults in rural China: Are there gender and age related differences? BMC Public Health 2022, 22, 356. [Google Scholar] [CrossRef]
- Meier, C.; Maurer, J. Buddy or burden? Patterns, perceptions, and experiences of pet ownership among older adults in Switzerland. Eur. J. Ageing 2022, 19, 1201–1212. [Google Scholar] [CrossRef]
- Obradović, N.; Lagueux, É.; Latulippe, K.; Provencher, V. Understanding the benefits, challenges, and the role of pet ownership in the daily lives of community-dwelling older adults: A case study. Animals 2021, 11, 2628. [Google Scholar] [CrossRef] [PubMed]
- Friedmann, E.; Gee, N.R.; Simonsick, E.M.; Barr, E.; Resnick, B.; Werthman, E.; Adesanya, I. Pet ownership and maintenance of physical function in older adults—Evidence from the Baltimore longitudinal study of aging (BLSA). Innov. Aging 2023, 7, igac080. [Google Scholar] [CrossRef] [PubMed]
- Macauley, L.; Chur-Hansen, A. Human Health Benefits of Non-Conventional Companion Animals: A Narrative Review. Animals 2022, 13, 28. [Google Scholar] [CrossRef] [PubMed]
- Gallagher, E.; Lavan, A.; Kenny, R.A.; Briggs, R. The Association of Regular Dog Walking with Mobility, Falls and Fear of Falling in Later Life. J. Gerontol. A Biol. Sci. Med. Sci. 2025, 80, glaf010. [Google Scholar] [CrossRef]
- Hui Gan, G.Z.; Hill, A.-M.; Yeung, P.; Keesing, S.; Netto, J.A. Pet ownership and its influence on mental health in older adults. Aging Ment. Health 2020, 24, 1605–1612. [Google Scholar] [CrossRef]
- Hansen, P.R.; König, H.H.; Hajek, A. Pet ownership and psychosocial factors in adults aged 40 years and over: Results of a large nationally representative longitudinal survey. Societies 2024, 14, 132. [Google Scholar] [CrossRef]
- Gale, C.R.; Cooper, C.; Aihie Sayer, A. Prevalence and risk factors for falls in older men and women: The English Lon-gitudinal Study of Ageing. Age Ageing 2016, 45, 789–794. [Google Scholar] [CrossRef]
- Lin, W.Q.; Lin, L.; Sun, S.Y.; Yuan, L.X.; Sun, M.Y.; Wang, C.; Chen, J.M.; Li, Y.H.; Zhou, Q.; Wu, D.; et al. Prevalence of falls, injury from falls and associations with chronic diseases among community-dwelling older adults in Guangzhou, China: A cross-sectional study. Front. Public Health 2023, 11, 1251858. [Google Scholar] [CrossRef]
- Wang, J.; Li, Y.; Yang, G.Y.; Jin, K. Age-Related Dysfunction in Balance: A Comprehensive Review of Causes, Conse-quences, and Interventions. Aging Dis. 2024, 16, 714–737. [Google Scholar] [CrossRef]
- Ogliari, G.; Ryg, J.; Andersen-Ranberg, K.; Scheel-Hincke, L.L.; Masud, T. Perceived neighbourhood environment and falls among community-dwelling adults: Cross-sectional and prospective findings from the Survey of Health, Ageing and Retirement in Europe (SHARE). Eur. J. Ageing 2022, 19, 1121–1134. [Google Scholar] [CrossRef]
- Li, S.; Cui, G.; Er, Y.; Ye, P.; Xue, T.; Zhang, J.; Liu, X.; Duan, L.; Lv, F.; Yao, Y. Housing environmental factors driving falls among middle-aged and older adults: A national cohort study. Innov. Aging 2023, 7, igad121. [Google Scholar] [CrossRef]
- Rico, C.L.V.; Curcio, C.L. Fear of falling and environmental factors: A scoping review. Ann. Geriatr. Med. Res. 2022, 26, 83–93. [Google Scholar] [CrossRef] [PubMed]
- Romli, M.H.; Tan, M.P.; Mackenzie, L.; Lovarini, M.; Kamaruzzaman, S.B.; Clemson, L. Factors associated with home hazards: Findings from the Malaysian Elders Longitudinal Research study. Geriatr. Gerontol. Int. 2018, 18, 387–395. [Google Scholar] [CrossRef] [PubMed]
- Towne, S.D., Jr.; Smith, M.L.; Yoshikawa, A.; Ory, M.G. Geospatial distribution of fall-related hospitalization incidence in Texas. J. Saf. Res. 2015, 53, 11–16. [Google Scholar] [CrossRef] [PubMed]
- Natora, A.H.; Oxley, J.; Barclay, L.; Taylor, K.; Bolam, B.; Haines, T.P. Improving policy for the prevention of falls among community-dwelling older people—A scoping review and quality assessment of international national and state level public policies. Int. J. Public Health 2022, 67, 1604604. [Google Scholar] [CrossRef]
- Verma, S.K.; Willetts, J.L.; Corns, H.L.; Marucci-Wellman, H.R.; Lombardi, D.A.; Courtney, T.K. Falls and Fall-Related Injuries among Community-Dwelling Adults in the United States. PLoS ONE 2016, 11, e0150939. [Google Scholar] [CrossRef]
- Soh, S.L.H.; Tan, C.W.; Lane, J.; Yeh, T.T.; Soon, B. Near-falls in Singapore community-dwelling older adults: A feasibility study. Pilot Feasibility Stud. 2021, 7, 25. [Google Scholar] [CrossRef]
- Song, K.; Luo, J.; Cao, X.; Zhao, Z. Urban-rural differences in the successful aging among older adults in China. PLoS ONE 2025, 20, e0319105. [Google Scholar] [CrossRef]
| Variables | Total: n (%) | Falls: n (%) | p-Value | |
|---|---|---|---|---|
| Yes (n = 97) | No (n = 228) | |||
| Age | 0.915 | |||
| 60–69 years | 169 (52.0) | 50 (29.6) | 119 (70.4) | |
| 70–79 years | 156 (48.0) | 47 (30.1) | 109 (69.9) | |
| Sex | 0.008 | |||
| Male | 90 (27.7) | 17 (18.9) | 73 (81.1) | |
| Female | 235 (72.3) | 80 (34.0) | 155 (66.0) | |
| Employment status | 0.008 | |||
| Non-agricultural employment | 243 (74.8) | 82 (33.7) | 161 (66.3) | |
| Agricultural employment | 82 (25.2) | 15 (18.3) | 67 (81.7) | |
| Monthly Income | 0.011 | |||
| ≤700 THB | 183 (56.3) | 65 (35.5) | 118 (64.5) | |
| >700 THB | 142 (43.7) | 32 (22.5) | 110 (77.5) | |
| Chronic diseases a | 0.044 | |||
| ≤1 | 198 (60.9) | 51 (25.8) | 147 (74.2) | |
| >1 | 127 (39.1) | 46 (36.2) | 81 (63.8) | |
| Health issues b | 0.002 | |||
| ≤1 | 157 (48.3) | 34 (21.7) | 123 (78.3) | |
| >1 | 168 (51.7) | 63 (37.5) | 105 (62.5) | |
| Medication use c | 0.045 | |||
| No | 155 (47.7) | 38 (24.5) | 117 (75.5) | |
| Yes | 170 (52.3) | 59 (34.7) | 111 (65.3) | |
| Obstacles | 0.018 | |||
| No | 143 (44.0) | 33 (23.1) | 110 (76.9) | |
| Yes | 182 (56.0) | 64 (35.2) | 118 (64.8) | |
| Pets | 0.035 | |||
| No | 172 (52.9) | 60 (34.9) | 112 (65.1) | |
| Yes | 153 (47.1) | 37 (24.2) | 116 (75.8) | |
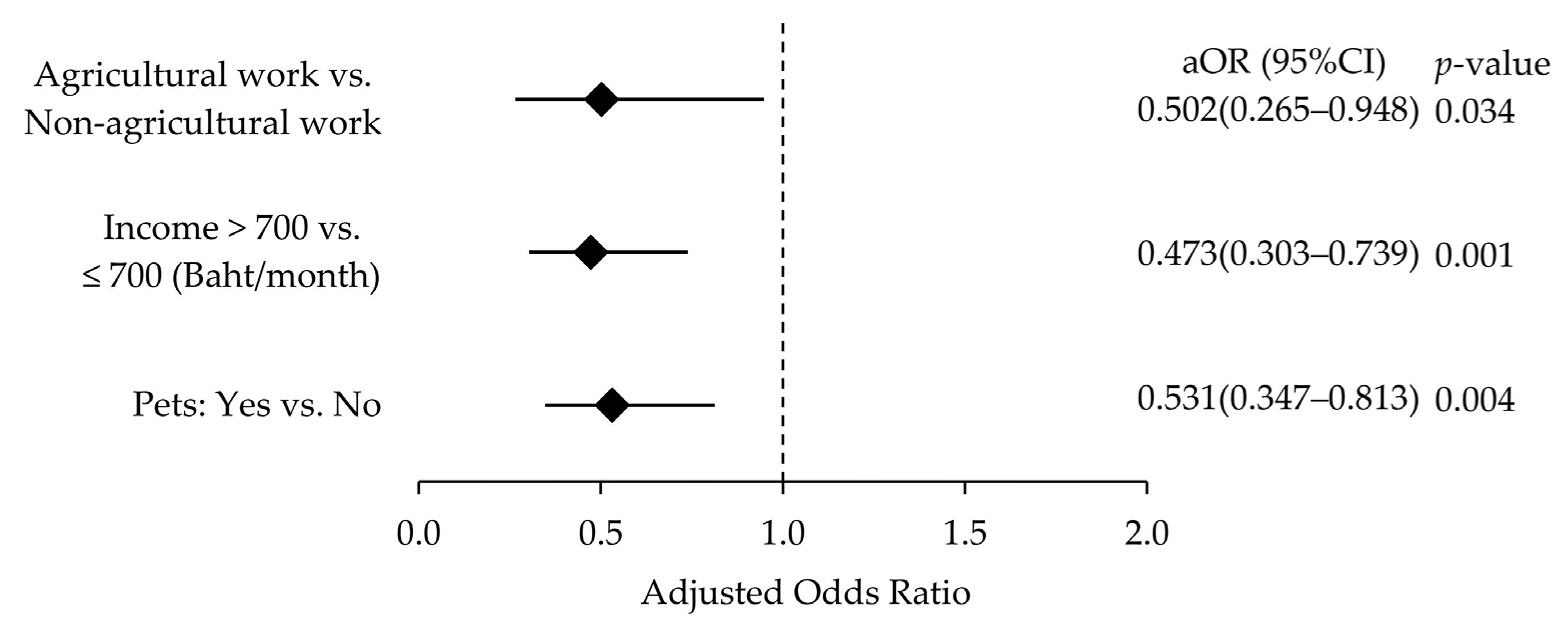
| Factor | Adjusted Odds Ratio | 95% CI | p-Value |
|---|---|---|---|
| Employment status | |||
| Non-agricultural work | 1 | - | - |
| Agricultural work | 0.502 | 0.265–0.948 | 0.034 |
| Income per month (Thai baht) | |||
| ≤700 | 1 | - | - |
| >700 | 0.473 | 0.303–0.739 | 0.001 |
| Pets | |||
| No | 1 | - | - |
| Yes | 0.531 | 0.347–0.813 | 0.004 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Srimoke, W.; Thanapop, C.; Sangchart, P.; Chitpong, S.; Hnoophet, J.; Rueangkhanap, N.; Jantep, K. Protective Factors for Falls Among Independent Older Adults: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2025, 22, 1202. https://doi.org/10.3390/ijerph22081202
Srimoke W, Thanapop C, Sangchart P, Chitpong S, Hnoophet J, Rueangkhanap N, Jantep K. Protective Factors for Falls Among Independent Older Adults: A Cross-Sectional Study. International Journal of Environmental Research and Public Health. 2025; 22(8):1202. https://doi.org/10.3390/ijerph22081202
Chicago/Turabian StyleSrimoke, Warangkana, Chamnong Thanapop, Pimpichaya Sangchart, Sopanat Chitpong, Jirasuta Hnoophet, Nattaya Rueangkhanap, and Kitipop Jantep. 2025. "Protective Factors for Falls Among Independent Older Adults: A Cross-Sectional Study" International Journal of Environmental Research and Public Health 22, no. 8: 1202. https://doi.org/10.3390/ijerph22081202
APA StyleSrimoke, W., Thanapop, C., Sangchart, P., Chitpong, S., Hnoophet, J., Rueangkhanap, N., & Jantep, K. (2025). Protective Factors for Falls Among Independent Older Adults: A Cross-Sectional Study. International Journal of Environmental Research and Public Health, 22(8), 1202. https://doi.org/10.3390/ijerph22081202







