Comienzo Saludable Puerto Rico: A Community-Based Network of Care to Improve Maternal, Newborn, and Child Health Outcomes
Abstract
1. Introduction
1.1. Maternal and Newborn/Child Health in Puerto Rico
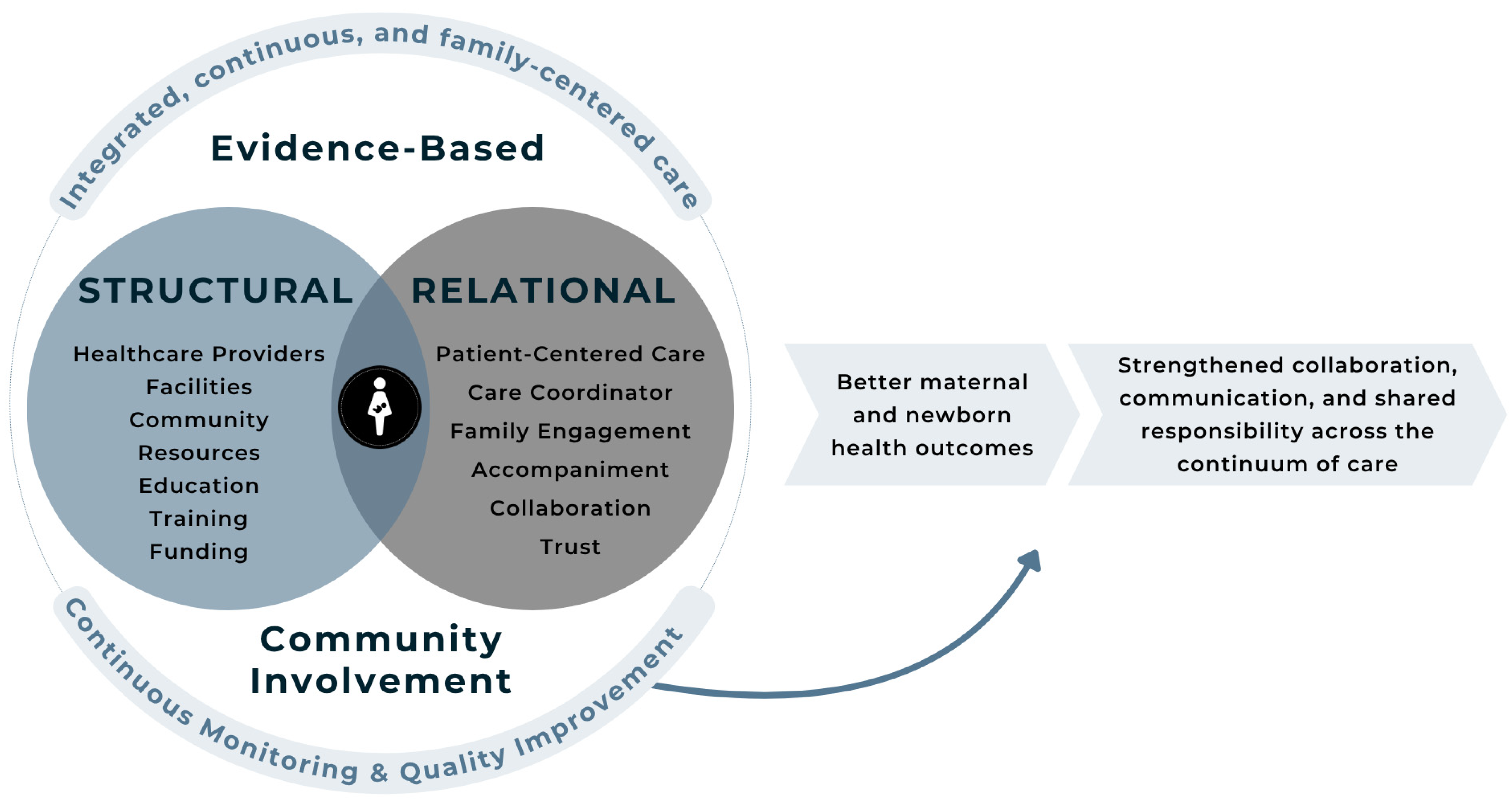
1.2. Networks of Care Framework
1.3. Purpose
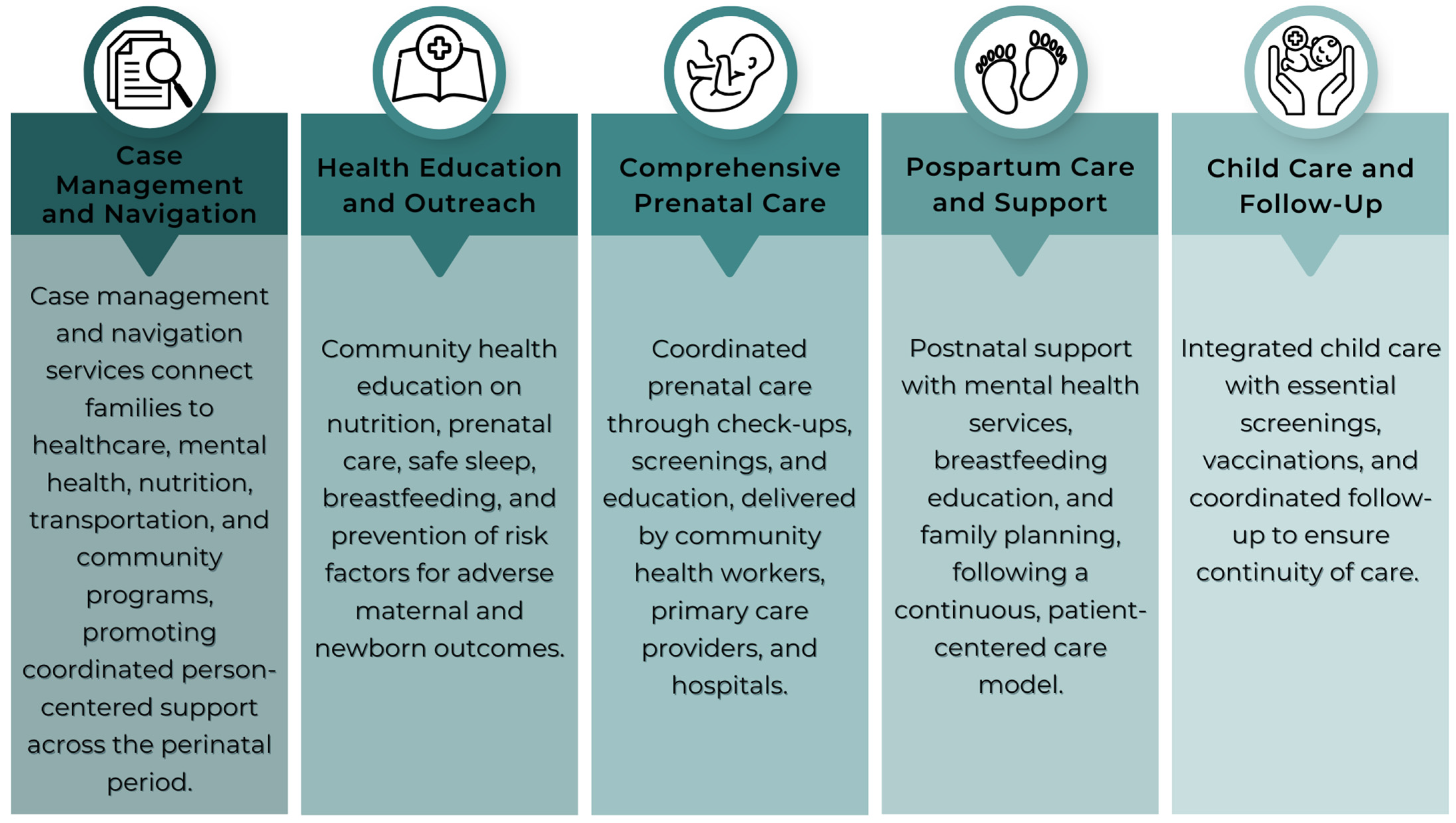
1.4. Cuidado Compartio Model: Key Program Components
2. Materials and Methods
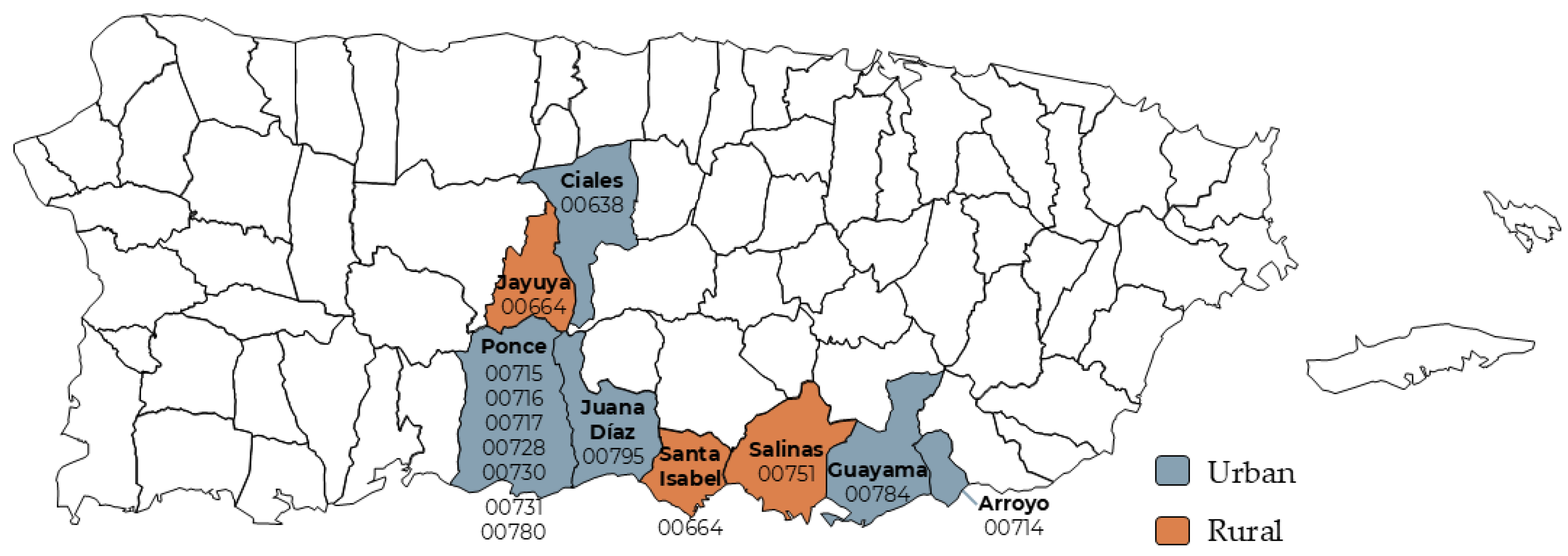
2.1. Population and Setting
2.2. Data Collection and Analysis
2.2.1. Participant Intake and Enrollment
2.2.2. Assessment Tools
2.2.3. Psychosocial and Behavioral Screening
2.3. Qualitative Data Collection and Analysis
3. Results: Program Outcomes and Impact
3.1. Sociodemographic Characteristics
3.2. Impact on Maternal, Paternal, Newborn, and Child Health
3.2.1. Impact on Maternal Health
3.2.2. Impact on Newborn/Child Health
3.2.3. Health Gaps
3.3. Healthcare Provider Outcomes
3.4. Qualitative Findings: Participants’ Feelings and Plans
3.4.1. Feelings
“I feel stronger and better prepared to take care of myself and my baby.”
“I’m thankful to have someone checking on me—it makes a big difference.”
“I’m scared about how I’ll manage when I go back to work.”
“Even though I feel better, I’m scared about how I’ll manage when I go back to work.”
3.4.2. Plans
“I plan to keep all my baby’s appointments and mine too—not just when something is wrong.”
“I want to finish my degree and find a job that gives me time with my child.”
“I want to help other women like me—if I can do it, they can too.”
“We are saving to move into a safer neighborhood for our baby.”
4. Discussion
- Low birth weight among participants declined from 6.25% in 2019 to 6.76% in 2023, representing a 27.2% improvement compared to the community baseline (10.21%).
- Premature birth rates dropped from 13.54% to 6.80%, a 30.9% reduction compared to the baseline (11.34%).
- Infant mortality among children receiving Healthy Start services fell from 6.25% to 0%, representing a 75% reduction compared to the community baseline (8.89%).
4.1. Strengthening Networks of Care Through Emotional Support and Empowerment
4.2. Implications for Policy and Practice
4.3. Challenges and Barriers
4.4. Limitations and Future Directions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AAPI-2 | Adult Adolescent Parenting Inventory-2 |
| ACE | Adverse Childhood Experiences |
| ASQ-3 | Ages and Stages Questionnaire, Third Edition |
| ASQ-SE:2 | Ages and Stages Questionnaire: Social and Emotional Second Edition |
| ASSIST | Alcohol, Smoking and Substance Involvement Screening Test |
| CHW | Community Healthcare Worker |
| CQI | Continuous Quality Improvement |
| EPDS | Edinburg Postnatal Depression Scale |
| GAD-7 | Generalized Anxiety Disorder 7-Item |
| GN | Grupo Nexos, Inc |
| HRSA | Department of Health and Human Services’ Healthy Start Initiative |
| HS | Healthy Start |
| IPV | Intimate Partner Violence |
| ISP | Individualized Service Plan |
| NOC | Networks of Care |
| PHQ-9 | Patient Health Questionnaire-9 |
| US | Urban Strategies LLC |
References
- Lebron, C.N.; Pérez-Ramos, J.; Cardona-Cordero, N.; Morales, V.; Rivera-Joseph, S. Social justice is overdue for Puerto Rican Mothers. Am. J. Public Health 2024, 114 (Suppl. S1), S450–S452. [Google Scholar] [CrossRef] [PubMed]
- Matos-Moreno, A.; Santos-Lozada, A.R.; Mehta, N.; Mendes de Leon, C.F.; Lê-Scherban, F.; De Lima Friche, A.A. Migration is the driving force of rapid aging in Puerto Rico: A research brief. J. Public Health 2022, 41, 801–810. [Google Scholar] [CrossRef] [PubMed]
- Matos-Moreno, A.; Verdery, A.M.; Mendes de Leon, C.F.; De Jesús-Monge, V.M.; Santos-Lozada, A.R. Aging and the left behind: Puerto Rico and its unconventional rapid aging. Gerontologist 2022, 62, 964–973. [Google Scholar] [CrossRef] [PubMed]
- March of Dimes. Available online: https://www.marchofdimes.org/peristats/assets/s3/reports/mcd/Maternity-Care-Report-PuertoRico.pdf (accessed on 27 February 2025).
- Penchi, L. Medicina y Salud Pública. Available online: https://medicinaysaludpublica.com/noticias/salud-publica/asociacion-de-hospitales-solicita-la-intervencion-del-gobierno-ante-el-posible-cierre-de-salas-de-partos/25461 (accessed on 27 February 2025).
- Puerto Rico Health Department, Office of Demographic Records and Vital Statistics. Database of Births-Preliminary Data, 2020–2023; Puerto Rico Health Department, Office of Demographic Records and Vital Statistics: San Juan, Puerto Ric, 2024. [Google Scholar]
- Kalaris, K.; Radovich, E.; Carmone, A.E.; Smith, J.M.; Hyre, A.; Baye, M.L.; Vougmo, C.; Banerjee, A.; Liljestrand, J.; Moran, A.C. Networks of Care: An Approach to Improving Maternal and Newborn Health. Glob. Health: Sci. Pract. 2022, 10, e2200162. Available online: https://www.ghspjournal.org/content/ghsp/10/6/e2200162.full.pdf (accessed on 14 March 2025). [CrossRef] [PubMed]
- Byatt, N.; Levin, L.L.; Ziedonis, D.; Moore Simas, T.A.; Allison, J. Enhancing participation in depression care in outpatient perinatal care settings: A systematic review. Obstet. Gynecol. 2015, 126, 1048–1058. [Google Scholar] [CrossRef] [PubMed]
- Cabrera, N.J.; Shannon, J.D.; Tamis-LeMonda, C. Fathers’ influence on their children’s cognitive and emotional development: From toddlers to pre-K. Appl. Dev. Sci. 2007, 11, 208–213. [Google Scholar] [CrossRef]
- Gau, M.L.; Chang, C.Y.; Tian, S.H.; Lin, K.C. Effects of birth ball exercise on pain and self-efficacy during childbirth: A randomised controlled trial in Taiwan. Midwifery 2011, 27, e293–e300. [Google Scholar] [CrossRef] [PubMed]
- Walker, D.; Fasawe, O.; Jenny, A.; Networks of Care Framework for Maternal and Newborn Health: Examining and Contextualizing the Relational Elements for Low and Middle-Income Countries. UCSF Institute of Global Health Sciences, USAID’s Health Evaluation and Applied Research Development Project. 2024. Available online: https://iscollab.org/wp-content/uploads/Networks-of-Care-for-Maternal-and-Newborn-Health-Report-Feb-2024.pdf (accessed on 14 March 2025).
- Sultan, M.A.; Miller, E.; Tikkanen, R.S.; Singh, S.; Kullu, A.; Cometto, G.; Fitzpatrick, S.; Ajuebor, O.; Gillon, N.; Edward, A.; et al. Competency-based education and training for Community Health Workers: A scoping review. BMC Health Serv. Res. 2025, 25, 263. [Google Scholar] [CrossRef] [PubMed]
- Anderson, C.M.; Robins, C.S.; Greeno, C.G.; Cahalane, H.; Copeland, V.C.; Andrews, R.M. Why lower income mothers do not engage with the formal mental health care system: Perceived barriers to care. Qual. Health Res. 2006, 16, 926–943. [Google Scholar] [CrossRef] [PubMed]
- United States. Public Health Service Act, Title III, Part D, § 330H, 42 U.S.C. § 254c-8. 2018. Available online: https://grants.hrsa.gov/2010/Web2External/Interface/Common/EHBDisplayAttachment.aspx?dm_rtc=16&dm_attid=d3c378a4-b07d-48e5-ab36-38f05a7eeb48 (accessed on 14 March 2025).
- Brady, S. Building Many Stories into Collective Impact. Stanf. Soc. Innov. Rev. 2015. [Google Scholar] [CrossRef]
- Kania, J.; Kramer, M. Collective Impact. Stanf. Soc. Innov. Rev. 2011, 9, 36–41. [Google Scholar] [CrossRef]
- Kozhimannil, K.B.; Hardeman, R.R.; Attanasio, L.B.; Blauer-Peterson, C.; O’Brien, M. Doula care, birth outcomes, and costs among Medicaid beneficiaries. Am. J. Public Health 2016, 103, e113–e121. [Google Scholar] [CrossRef] [PubMed]
- Agency for Healthcare Research and Quality. Available online: https://www.ahrq.gov/ncepcr/care/coordination.html (accessed on 4 March 2025).
- Centers for Disease Control and Prevention (CDC). Available online: https://www.cdc.gov/public-health-gateway/php/about/social-determinants-of-health.html (accessed on 14 March 2025).
- National Partnership for Women & Families. Available online: https://nationalpartnership.org/ (accessed on 4 March 2025).
- Krans, E.E.; Davis, M.M. Preventing Low Birthweight: 25 years, prenatal risk, and the failure to reinvent prenatal care. Am. J. Obstet. Gynecol. 2012, 206, 398–403. [Google Scholar] [CrossRef] [PubMed]
- Howell, E.A. Reducing disparities in severe maternal morbidity and mortality. Clin. Obstet. Gynecol. 2018, 61, 387–399. [Google Scholar] [CrossRef] [PubMed]
- Lu, M.C.; Halfon, N. Racial and ethnic disparities in birth outcomes: A life-course perspective. Matern. Child Health J. 2003, 7, 13–30. [Google Scholar] [CrossRef] [PubMed]
- Cimino, S.; Tafà, M.; Cerniglia, L. Fathers as Key Figures Shaping the Foundations of Early Childhood Development: An Exploratory Longitudinal Study on Web-Based Intervention. J. Clin. Med. 2024, 13, 7167. Available online: https://pmc.ncbi.nlm.nih.gov/articles/PMC11642843/ (accessed on 14 March 2025). [CrossRef] [PubMed]
- Tabb, K.M.; Gavin, A.R.; Smith, D.C.; Huang, H.; Debbink, M. Role of mobile technology in addressing maternal and child health disparities. Matern. Child Health J. 2016, 20, 1023–1030. [Google Scholar]
- World Health Organization (WHO). Available online: https://healthynewbornnetwork.org/hnn-content/uploads/9789240098633-eng.pdf (accessed on 14 March 2025).[Green Version]
| Indicator | Community Baseline 1 (2020) | Healthy Start Initiative (HSI) Participants | Percent Change 2023 Against Community Baseline 4 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| 2019 2 | 2020 | 2021 | 2022 | 2023 | Trend | Percentage Change in HSI in 2019 and 2023 3 | |||
| Low Birth Weight among Children receiving Healthy Start Services before Birth | 10.21% | 6.25% | 5.58% | 7.12% | 7.35% | 6.76% |  | −9.59% | −27.21% |
| Premature Births among pregnant participants receiving Healthy Start Services before Birth | 11.34% | 13.54% | 11.49% | 8.30% | 10.69% | 6.80% |  | −29.99% | −30.94% |
| Infant Mortality Rate of Children receiving Healthy Start Services before Birth | 8.89% | 6.25% | 0.66% | 0.00% | 0.00% | 0.00% |  | −12.50% | −75% |
| Indicators | Baseline * | 2020 | 2021 | 2022 | 2023 | 2024 |
|---|---|---|---|---|---|---|
| 132 | 421 | 524 | 579 | 549 | 263 | |
| Depression screening | 123/123 (100%) | 371/372 (99.7%) | 445/454 (98%) | 491/493 (99.6%) | 470/472 (99.6%) | 230/230 (100%) |
| Depression referral | 26/29 (89.6%) | 56/60 (93.3%) | 68/70 (97.1%) | 58/79 (73.4%) | 41/77 (53.2%) | 26/36 (72.2%) |
| Father and/or partner involvement during pregnancy | 47/54 (87%) | 180/204 (88.2%) | 276/292 (94.5%) | 264/288 (91.7%) | 239/258 (92.6%) | 56/63 (88.9%) |
| Father and/or partner involvement with their child | 48/65 (73.8%) | 214/237 (90.3%) | 274/267 (93%) | 332/352 (94.3%) | 340/360 (94.4%) | 174/183 (95.1%) |
| Interconception period (18 months between pregnancies) | 0/0 (0%) | 2/3 (66.7%) | 29/116 (25%) | 47/134 (35.1%) | 40/116 (34.5%) | 11/23 (47.8%) |
| Intimate partner violence screening | 123/123 (100%) | 376/380 (98.9%) | 448/454 (98.7%) | 494/494 (100%) | 472/473 (99.8%) | 230/231 (99.6%) |
| Postpartum visit (first month postpartum) | 12/14 (85.7%) | 33/83 (39.8%) | 59/233 (25.3%) | 72/322 (22.4%) | 57/207 (27.5%) | - |
| Reproductive life plan | 50/123 (40.6%) | 292/312 (93.6%) | 363/454 (80%) | 257/461 (55.7%) | 368/473 (77.8%) | 221/231 (95.7%) |
| Tobacco use during prenatal stage | 27/27 (100%) | 47/47 (100%) | 201/203 (99%) | 184/187 (98.4%) | 351/359 (97.8%) | 134/135 (99.3%) |
| Usual source of medical care | 98/109 (89.9%) | 355/355 (100%) | 274/452 (60.6%) | 312/471 (66.2%) | 351/458 (76.6%) | 185/223 (83%) |
| Well-woman visit | 95/114 (83.3%) | 372/374 (99.5%) | 418/457 (91.5%) | 455/492 (92.5%) | 443/470 (94.3%) | 220/230 (95.7%) |
| Indicators % | Baseline | 2020 | 2021 | 2022 | 2023 | 2024 |
|---|---|---|---|---|---|---|
| 80 | 287 | 306 | 368 | 368 | 186 | |
| Breastfed ever (0–12 months) | 53/63 (84.1%) | 182/187 (97.3%) | 192/207 (92.8%) | 278/289 (96.2%) | 296/312 (94.9%) | 147/154 (95.5%) |
| Breastfeeding at 6 months (6–12 months) | 6/20 (30%) | 19/29 (65.5%) | 45/71 (63.4%) | 92/129 (71.3%) | 45/85 (52.9%) | 21/41 (51.2%) |
| Safe sleep practices (0–12 months) | 8/18 (44.4%) | 107/187 (57.2%) | 36/77 (46.8) | 159/331 (51.1%) | 172/304 (56.6%) | 97/159 (61%) |
| Regular source of medical care | 63/74 (85.1%) | 236/254 (92.9%) | 233/275 (84.7) | 335/354 (94.6%) | 354/366 (96.7%) | 179/186 (96.2%) |
| Well-child visit | 54/70 (77.1%) | 219/238 (92%) | 189/210 (90%) | 282/311 (90.7%) | 309/341 (90.6%) | 158/174 (90.8%) |
| Validated Screening Tool | 2019 | 2020 | 2021 | 2022 | 2023 | 2024 * | Total |
|---|---|---|---|---|---|---|---|
| ASQ | 0 | 5 | 152 | 193 | 210 | 81 | 641 |
| Edinburgh | 120 | 575 | 344 | 338 | 296 | 23 | 1696 |
| GAD | 131 | 351 | 296 | 312 | 310 | 16 | 1416 |
| PHQ-9 | 41 | 111 | 68 | 39 | 71 | 13 | 343 |
| Depression Scale for Males | 0 | 0 | 0 | 13 | 9 | 0 | 22 |
| Total measures administered | 292 | 1042 | 860 | 895 | 896 | 133 | 4118 |
| Service | 2019 | 2020 | 2021 | 2022 | 2023 | 2024 * | Total |
|---|---|---|---|---|---|---|---|
| Breastfeeding support and education | 22 | 317 | 21 | 37 | 71 | 13 | 481 |
| Doulas | 2 | 202 | 815 | 1170 | 807 | 208 | 3204 |
| Father individual encounter | 2 | 51 | 15 | 106 | 4 | 0 | 178 |
| Parenting Fundamentals | 5 | 124 | 84 | 100 | 70 | 0 | 383 |
| GGK Growing Great Kids | 0 | 111 | 247 | 192 | 185 | 45 | 780 |
| Home visit | 52 | 723 | 1837 | 1963 | 1565 | 509 | 6649 |
| Individual service plan | 74 | 272 | 235 | 253 | 221 | 4 | 1059 |
| Mental health session | 36 | 298 | 212 | 217 | 363 | 72 | 1198 |
| Father figure group session | 0 | 32 | 12 | 9 | 15 | 0 | 68 |
| Parenting Fundamentals group session | 7 | 91 | 55 | 69 | 56 | 0 | 278 |
| Prenatal group session | 0 | 8 | 42 | 37 | 30 | 2 | 119 |
| Other group services | 0 | 5 | 4 | 4 | 25 | 1 | 39 |
| Theme or Competencies | Sample Activities | Reach and Impact |
|---|---|---|
| CHW core training | Conducted standardized core competencies training for community health workers (CHWs), including modules on maternal mental health, reproductive life planning, safe sleep, and breastfeeding support | 32 CHWs trained across seven municipalities; 100% completed core competencies; 87% increased confidence in maternal health knowledge |
| Parenting education | Growing Great Kids Curriculum©, Parenting Fundamentals Curriculum©, FatherIn15© | Delivered in cycles with up to 48 contact hours |
| Maternal and infant health practices | Breastfeeding certification, safe sleep, perinatal mental health, birth preparation | 78 contact hours; >85% satisfaction |
| Violence and crisis response | Domestic and sexual violence, crisis intervention, IPV legal aspects | Response rates > 85%; high satisfaction reported |
| Communication and education | Effective communication, engaging fathers, team integration | Broad CHWs, doulas, and care coordinators |
| Leadership development | Coaching, supervision training, HR policy workshops | Two regional cohorts in 2024 |
| Technology and tools | Canva training, data system revisions, Fathering 15©, ASQ and AAPI form use | Enhanced monitoring and reporting capacity |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Acosta-Pérez, E.; Díaz, C.; Gómez-Reyes, A.; Vega, S.; Noboa Ramos, C.; Justinianes-Pérez, R.; Ferran, G.; Carnivali-García, J.; Grau, F.J.; Sardiñas, L.M.; et al. Comienzo Saludable Puerto Rico: A Community-Based Network of Care to Improve Maternal, Newborn, and Child Health Outcomes. Int. J. Environ. Res. Public Health 2025, 22, 1204. https://doi.org/10.3390/ijerph22081204
Acosta-Pérez E, Díaz C, Gómez-Reyes A, Vega S, Noboa Ramos C, Justinianes-Pérez R, Ferran G, Carnivali-García J, Grau FJ, Sardiñas LM, et al. Comienzo Saludable Puerto Rico: A Community-Based Network of Care to Improve Maternal, Newborn, and Child Health Outcomes. International Journal of Environmental Research and Public Health. 2025; 22(8):1204. https://doi.org/10.3390/ijerph22081204
Chicago/Turabian StyleAcosta-Pérez, Edna, Cristina Díaz, Atisha Gómez-Reyes, Samaris Vega, Carlamarie Noboa Ramos, Rosario Justinianes-Pérez, Glamarie Ferran, Jessica Carnivali-García, Fabiola J. Grau, Lili M. Sardiñas, and et al. 2025. "Comienzo Saludable Puerto Rico: A Community-Based Network of Care to Improve Maternal, Newborn, and Child Health Outcomes" International Journal of Environmental Research and Public Health 22, no. 8: 1204. https://doi.org/10.3390/ijerph22081204
APA StyleAcosta-Pérez, E., Díaz, C., Gómez-Reyes, A., Vega, S., Noboa Ramos, C., Justinianes-Pérez, R., Ferran, G., Carnivali-García, J., Grau, F. J., Sardiñas, L. M., Campos, M., & Sánchez Cesareo, M. (2025). Comienzo Saludable Puerto Rico: A Community-Based Network of Care to Improve Maternal, Newborn, and Child Health Outcomes. International Journal of Environmental Research and Public Health, 22(8), 1204. https://doi.org/10.3390/ijerph22081204











