Reliability and Validity of Laboratory and Field Cardiorespiratory Exercise Tests for Wheelchair Users: A Systematic Review
Abstract
1. Introduction
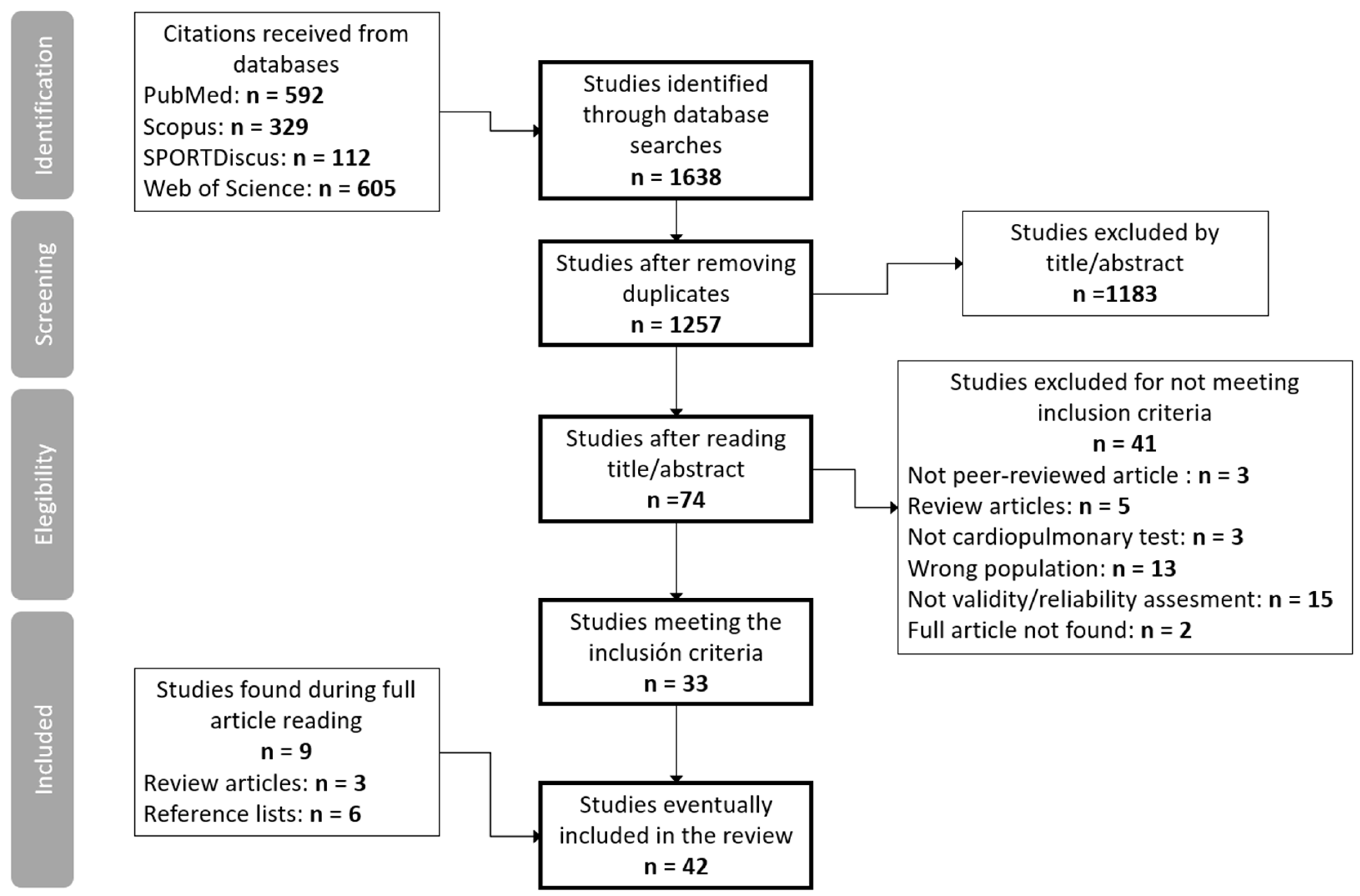
2. Materials and Methods
2.1. Search Strategy
2.2. Eligibility Criteria
2.3. Screening
2.4. Data Extraction
2.5. Quality Assessment
2.6. Level of Evidence
3. Results
3.1. Quality of Included Studies
3.2. Characteristics of the Participants
3.3. Laboratory Tests
3.4. Field Tests
4. Discussion
Study Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Selph, S.S.; Skelly, A.C.; Wasson, N.; Dettori, J.R.; Brodt, E.D.; Ensrud, E.; Elliot, D.; Dissinger, K.M.; McDonagh, M. Physical Activity and the Health of Wheelchair Users: A Systematic Review in Multiple Sclerosis, Cerebral Palsy, and Spinal Cord Injury. Arch. Phys. Med. Rehabil. 2021, 102, 2464–2481.e33. [Google Scholar] [CrossRef] [PubMed]
- Gauthier, C.; Arel, J.; Brosseau, R.; Hicks, A.L.; Gagnon, D.H. Reliability and minimal detectable change of a new treadmill-based progressive workload incremental test to measure cardiorespiratory fitness in manual wheelchair users. J. Spinal Cord. Med. 2017, 40, 759–767. [Google Scholar] [CrossRef] [PubMed]
- Kressler, J.; Cowan, R.E.; Bigford, G.E.; Nash, M.S. Reducing cardiometabolic disease in spinal cord injury. Phys. Med. Rehabil. Clin. N. Am. 2014, 25, 573–604. [Google Scholar] [CrossRef]
- Van der Scheer, J.W.; Martin Ginis, K.A.; Ditor, D.S.; Goosey-Tolfrey, V.L.; Hicks, A.L.; West, C.R.; Wolfe, D.L. Effects of exercise on fitness and health of adults with spinal cord injury: A systematic review. Neurology 2017, 89, 736–745. [Google Scholar] [CrossRef] [PubMed]
- Al-Mallah, M.H.; Sakr, S.; Al-Qunaibet, A. Cardiorespiratory Fitness and Cardiovascular Disease Prevention: An Update. Curr. Atheroscler. Rep. 2018, 20, 1. [Google Scholar] [CrossRef]
- Bermejo-Cantarero, A.; Álvarez-Bueno, C.; Martinez-Vizcaino, V.; García-Hermoso, A.; Torres-Costoso, A.I.; Sánchez-López, M. Association between physical activity, sedentary behavior, and fitness with health related quality of life in healthy children and adolescents: A protocol for a systematic review and meta-analysis. Medicine 2017, 96, e6407. [Google Scholar] [CrossRef]
- Kodama, S.; Saito, K.; Tanaka, S.; Maki, M.; Yachi, Y.; Asumi, M.; Sugawara, A.; Totsuka, K.; Shimano, H.; Ohashi, Y.; et al. Cardiorespiratory fitness as a quantitative predictor of all-cause mortality and cardiovascular events in healthy men and women: A meta-analysis. JAMA 2009, 301, 2024–2035. [Google Scholar] [CrossRef]
- Bouzas, S.; Molina, A.J.; Fernández-Villa, T.; Miller, K.; Sanchez-Lastra, M.A.; Ayán, C. Effects of exercise on the physical fitness and functionality of people with amputations: Systematic review and meta-analysis. Disabil. Health J. 2021, 14, 100976. [Google Scholar] [CrossRef]
- Carroll, D.D.; Courtney-Long, E.A.; Stevens, A.C.; Sloan, M.L.; Lullo, C.; Visser, S.N.; Fox, M.H.; Armour, B.S.; Campbell, V.A.; Brown, D.R.; et al. Vital signs: Disability and physical activity—United States, 2009–2012. MMWR Morb. Mortal. Wkly Rep. 2014, 63, 407–413. [Google Scholar]
- Tawashy, A.E.; Eng, J.J.; Krassioukov, A.V.; Miller, W.C.; Sproule, S. Aerobic exercise during early rehabilitation for cervical spinal cord injury. Phys. Ther. 2010, 90, 427–437. [Google Scholar] [CrossRef]
- Van den Berg-Emons, R.J.; Bussmann, J.B.; Haisma, J.A.; Sluis, T.A.; van der Woude, L.H.; Bergen, M.P.; Stam, H.J. A prospective study on physical activity levels after spinal cord injury during inpatient rehabilitation and the year after discharge. Arch. Phys. Med. Rehabil. 2008, 89, 2094–2101. [Google Scholar] [CrossRef] [PubMed]
- Remes, L.; Isoaho, R.; Vahlberg, T.; Hiekkanen, H.; Korhonen, K.; Viitanen, M.; Rautava, P. Major lower extremity amputation in elderly patients with peripheral arterial disease: Incidence and survival rates. Aging Clin. Exp. Res. 2008, 20, 385–393. [Google Scholar] [CrossRef] [PubMed]
- Wezenberg, D.; van der Woude, L.H.; Faber, W.X.; de Haan, A.; Houdijk, H. Relation between aerobic capacity and walking ability in older adults with a lower-limb amputation. Arch. Phys. Med. Rehabil. 2013, 94, 1714–1720. [Google Scholar] [CrossRef] [PubMed]
- Davis, G.M. Exercise capacity of individuals with paraplegia. Med. Sci. Sports Exerc. 1993, 25, 423–432. [Google Scholar] [CrossRef]
- Stoboy, H.; Rich, B.W.; Lee, M. Workload and energy expenditure during wheelchair propelling. Paraplegia 1971, 8, 223–230. [Google Scholar] [CrossRef][Green Version]
- Wicks, J.R.; Lymburner, K.; Dinsdale, S.M.; Jones, N.L. The use of multistage exercise testing with wheelchair ergometry and arm cranking in subjects with spinal cord lesions. Paraplegia 1977, 15, 252–261. [Google Scholar] [CrossRef]
- Langbein, W.E.; Robinson, C.J.; Reid, C.M. Validation of the wheelchair aerobic fitness trainer and test protocol. Proc. Annu. Conf. Eng. Med. Biol. 1991, 13, 1839–1840. [Google Scholar] [CrossRef]
- Bhambhani, Y.N.; Holland, L.J.; Eriksson, P.; Steadward, R.D. Physiological responses during wheelchair racing in quadriplegics and paraplegics. Paraplegia 1994, 32, 253–260. [Google Scholar] [CrossRef][Green Version]
- Bhambhani, Y.N.; Eriksson, P.; Steadward, R.D. Reliability of peak physiological responses during wheelchair ergometry in persons with spinal cord injury. Arch. Phys. Med. Rehabil. 1991, 72, 559–562. [Google Scholar]
- Bhambhani, Y.N.; Holland, L.J.; Steadward, R.D. Maximal aerobic power in cerebral palsied wheelchair athletes: Validity and reliability. Arch. Phys. Med. Rehabil. 1992, 73, 246–252. [Google Scholar]
- Bhambhani, Y.N.; Holland, L.J.; Steadward, R.D. Anaerobic threshold in wheelchair athletes with cerebral palsy: Validity and reliability. Arch. Phys. Med. Rehabil. 1993, 74, 305–311. [Google Scholar] [PubMed]
- Christensen, J.; Tang, L.; Doherty, P.; Langhorn, C.; Langberg, H. Test-retest reliability of a maximal arm cycle exercise test for younger individuals with traumatic lower limb amputations. Eur. J. Physiother. 2019, 22, 115–120. [Google Scholar] [CrossRef]
- Hol, A.T.; Eng, J.J.; Miller, W.C.; Sproule, S.; Krassioukov, A.V. Reliability and validity of the six-minute arm test for the evaluation of cardiovascular fitness in people with spinal cord injury. Arch. Phys. Med. Rehabil. 2007, 88, 489–495. [Google Scholar] [CrossRef]
- Morgan, K.A.; Taylor, K.L.; Tucker, S.M.; Cade, W.T.; Klaesner, J.W. Exercise testing protocol using a roller system for manual wheelchair users with spinal cord injury. J. Spinal Cord. Med. 2019, 42, 288–297. [Google Scholar] [CrossRef]
- Granados, C.; Yanci, J.; Badiola, A.; Iturricastillo, A.; Otero, M.; Olasagasti, J.; Bidaurrazaga-Letona, I.; Gil, S.M. Anthropometry and Performance in Wheelchair Basketball. J. Strength. Cond. Res. 2015, 29, 1812–1820. [Google Scholar] [CrossRef] [PubMed]
- Mayorga-Vega, D.; Bocanegra-Parrilla, R.; Ornelas, M.; Viciana, J. Criterion-Related Validity of the Distance- and Time-Based Walk/Run Field Tests for Estimating Cardiorespiratory Fitness: A Systematic Review and Meta-Analysis. PLoS ONE 2016, 11, e0151671. [Google Scholar] [CrossRef]
- Eerden, S.; Dekker, R.; Hettinga, F.J. Maximal and submaximal aerobic tests for wheelchair-dependent persons with spinal cord injury: A systematic review to summarize and identify useful applications for clinical rehabilitation. Disabil. Rehabil. 2018, 40, 497–521. [Google Scholar] [CrossRef]
- Goosey-Tolfrey, V.L.; Leicht, C.A. Field-based physiological testing of wheelchair athletes. Sports Med. 2013, 43, 77–91. [Google Scholar] [CrossRef]
- Wouters, M.; Evenhuis, H.M.; Hilgenkamp, T.I. Systematic review of field-based physical fitness tests for children and adolescents with intellectual disabilities. Res. Dev. Disabil. 2017, 61, 77–94. [Google Scholar] [CrossRef]
- Eriksson, P.; Löfström, L.; Ekblom, B. Aerobic power during maximal exercise in untrained and well-trained persons with quadriplegia and paraplegia. Scand. J. Rehabil. Med. 1988, 20, 141–147. [Google Scholar]
- Klaesner, J.; Morgan, K.A.; Gray, D.B. The development of an instrumented wheelchair propulsion testing and training device. Assist. Technol. 2014, 26, 24–32. [Google Scholar] [CrossRef]
- Knechtle, B.; Köpfli, W. Treadmill exercise testing with increasing inclination as exercise protocol for wheelchair athletes. Spinal Cord. 2001, 39, 633–636. [Google Scholar] [CrossRef] [PubMed]
- De Groot, S.; Valent, L.J.; Fickert, R.; Pluim, B.M.; Houdijk, H. An Incremental Shuttle Wheel Test for Wheelchair Tennis Players. Int. J. Sports Physiol. Perform. 2016, 11, 1111–1114. [Google Scholar] [CrossRef] [PubMed]
- Vanderthommen, M.; Francaux, M.; Colinet, C.; Lehance, C.; Lhermerout, C.; Crielaard, J.M.; Theisen, D. A multistage field test of wheelchair users for evaluation of fitness and prediction of peak oxygen consumption. J. Rehabil. Res. Dev. 2002, 39, 685–692. [Google Scholar]
- Léger, L.; Boucher, R. An indirect continuous running multistage field test: The Université de Montréal track test. Can. J. Appl. Sport. Sci. 1980, 5, 77–84. [Google Scholar]
- Yanci, J.; Granados, C.; Otero, M.; Badiola, A.; Olasagasti, J.; Bidaurrazaga-Letona, I.; Iturricastillo, A.; Gil, S.M. Sprint, agility, strength and endurance capacity in wheelchair basketball players. Biol. Sport 2015, 32, 71–78. [Google Scholar] [CrossRef]
- Currell, K.; Jeukendrup, A.E. Validity, reliability and sensitivity of measures of sporting performance. Sports Med. 2008, 38, 297–316. [Google Scholar] [CrossRef] [PubMed]
- Ruiz, J.R.; Castro-Piñero, J.; Artero, E.G.; Ortega, F.B.; Sjöström, M.; Suni, J.; Castillo, M.J. Predictive validity of health-related fitness in youth: A systematic review. Br. J. Sports Med. 2009, 43, 909–923. [Google Scholar] [CrossRef]
- Laskin, J.J.; Slivka, D.; Frogley, M. A cadence based sub-maximal field test for the prediction of peak oxygen consumption in elite wheelchair basketball athletes. J. Exerc. Physiol. Online 2004, 7, 8–18. [Google Scholar]
- Cowan, R.E.; Callahan, M.K.; Nash, M.S. The 6-min push test is reliable and predicts low fitness in spinal cord injury. Med. Sci. Sports Exerc. 2012, 44, 1993–2000. [Google Scholar] [CrossRef]
- Dwyer, G.B.; Davis, R.W. The relationship between a twelve minute wheelchair push test and VO2peak in women wheelchair athletes. Sport. Med. Train. Rehabil. 1998, 8, 1–11. [Google Scholar] [CrossRef]
- Longmuir, P.E.; Shephard, R.J. Refinement of the arm CAFT protocol for assessing aerobic fitness in adults with mobility impairments. Adapt. Phys. Act. Q. 1995, 12, 362–376. [Google Scholar] [CrossRef]
- Verschuren, O.; Ketelaar, M.; De Groot, J.; Vila Nova, F.; Takken, T. Reproducibility of two functional field exercise tests for children with cerebral palsy who self-propel a manual wheelchair. Dev. Med. Child. Neurol. 2013, 55, 185–190. [Google Scholar] [CrossRef]
- Hartung, G.H.; Lally, D.A.; Blancq, R.J. Comparison of treadmill exercise testing protocols for wheelchair users. Eur. J. Appl. Physiol. Occup. Physiol. 1993, 66, 362–365. [Google Scholar] [CrossRef]
- Kelly, V.G.; Chen, K.K.; Oyewale, M. Reliability of the 30-15 intermittent fitness test for elite wheelchair rugby players. Sci. Med. Footb. 2018, 2, 191–195. [Google Scholar] [CrossRef]
- Ayán Pérez, C.; Martínez-Lemos, I.; Lago-Ballesteros, J.; Cancela Carral, J.M.; Loira-Camiña, N. Reliability and Validity of Physical Fitness Field-Based Tests in Down Syndrome: A Systematic Review. J. Policy Pract. Intellect. Disabil. 2016, 13, 142–156. [Google Scholar] [CrossRef]
- Balemans, A.C.; Fragala-Pinkham, M.A.; Lennon, N.; Thorpe, D.; Boyd, R.N.; O’Neil, M.E.; Bjornson, K.; Becher, J.G.; Dallmeijer, A.J. Systematic review of the clinimetric properties of laboratory- and field-based aerobic and anaerobic fitness measures in children with cerebral palsy. Arch. Phys. Med. Rehabil. 2013, 94, 287–301. [Google Scholar] [CrossRef] [PubMed]
- Lennon, N.; Thorpe, D.; Balemans, A.C.; Fragala-Pinkham, M.; O’Neil, M.; Bjornson, K.; Boyd, R.; Dallmeijer, A.J. The clinimetric properties of aerobic and anaerobic fitness measures in adults with cerebral palsy: A systematic review of the literature. Res. Dev. Disabil. 2015, 45–46, 316–328. [Google Scholar] [CrossRef]
- Oppewal, A.; Hilgenkamp, T.I.M.; van Wijck, R.; Evenhuis, H.M. Cardiorespiratory fitness in individuals with intellectual disabilities-A review. Res. Dev. Disabil. 2013, 34, 3301–3316. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. J. Clin. Epidemiol. 2009, 62, 1006–1012. [Google Scholar] [CrossRef]
- Mokkink, L.B.; Prinsen, C.A.; Patrick, D.; Alonso, J.; Bouter, L.M.; de Vet, H.C.W.; Terwee, C.B. COSMIN Study Design Checklist for Patient-Reported Outcome Measurement Instruments; Department of Epidemiology and Biostatistics, Amsterdam Public Health Research Institute, Amsterdam University Medical Centers, Location VUmc: Amsterdam, The Netherlands, 2019; pp. 1–32. [Google Scholar]
- Kofsky, P.R.; Davis, G.M.; Shephard, R.J.; Jackson, R.W.; Keene, G.C. Field testing: Assessment of physical fitness of disabled adults. Eur. J. Appl. Physiol. Occup. Physiol. 1983, 51, 109–120. [Google Scholar] [CrossRef]
- Holland, L.J.; Bhambhani, Y.N.; Ferrara, M.S.; Steadward, R.D. Reliability of the maximal aerobic power and ventilatory threshold in adults with cerebral palsy. Arch. Phys. Med. Rehabil. 1994, 75, 687–691. [Google Scholar] [CrossRef] [PubMed]
- Vinet, A.; Bernard, P.L.; Poulain, M.; Varray, A.; Le Gallais, D.; Micallef, J.P. Validation of an incremental field test for the direct assessment of peak oxygen uptake in wheelchair-dependent athletes. Spinal Cord. 1996, 34, 288–293. [Google Scholar] [CrossRef]
- Poulain, M.; Vinet, A.; Bernard, P.L.; Varray, A. Reproducibility of the adapted leger and boucher test for wheelchair-dependent athletes. Spinal Cord. 1999, 37, 129–135. [Google Scholar] [CrossRef] [PubMed]
- Vanlandewijck, Y.C.; Daly, D.J.; Theisen, D.M. Field test evaluation of aerobic, anaerobic, and wheelchair basketball skill performances. Int. J. Sports Med. 1999, 20, 548–554. [Google Scholar] [CrossRef]
- Stewart, M.W.; Melton-Rogers, S.L.; Morrison, S.; Figoni, S.F. The measurement properties of fitness measures and health status for persons with spinal cord injuries. Arch. Phys. Med. Rehabil. 2000, 81, 394–400. [Google Scholar] [CrossRef]
- Vinet, A.; Le Gallais, D.; Bouges, S.; Bernard, P.L.; Poulain, M.; Varray, A.; Micallef, J.P. Prediction of VO2peak in wheelchair-dependent athletes from the adapted Léger and Boucher test. Spinal Cord. 2002, 40, 507–512. [Google Scholar] [CrossRef] [PubMed]
- Goosey-Tolfrey, V.L.; Tolfrey, K. The multi-stage fitness test as a predictor of endurance fitness in wheelchair athletes. J. Sports Sci. 2008, 26, 511–517. [Google Scholar] [CrossRef]
- Leicht, C.A.; Tolfrey, K.; Lenton, J.P.; Bishop, N.C.; Goosey-Tolfrey, V.L. The verification phase and reliability of physiological parameters in peak testing of elite wheelchair athletes. Eur. J. Appl. Physiol. 2013, 113, 337–345. [Google Scholar] [CrossRef]
- Verschuren, O.; Zwinkels, M.; Ketelaar, M.; Reijnders-van Son, F.; Takken, T. Reproducibility and validity of the 10-meter shuttle ride test in wheelchair-using children and adolescents with cerebral palsy. Phys. Ther. 2013, 93, 967–974. [Google Scholar] [CrossRef]
- Goosey-Tolfrey, V.L.; Paulson, T.A.W.; Tolfrey, K.; Eston, R.G. Prediction of peak oxygen uptake from differentiated ratings of perceived exertion during wheelchair propulsion in trained wheelchair sportspersons. Eur. J. Appl. Physiol. 2014, 114, 1251–1258. [Google Scholar] [CrossRef]
- Weissland, T.; Faupin, A.; Borel, B.; Berthoin, S.; Leprêtre, P.M. Effects of modified multistage field test on performance and physiological responses in wheelchair basketball players. Biomed. Res. Int. 2015, 2015, 245378. [Google Scholar] [CrossRef]
- Bloemen, M.A.T.; De Groot, J.F.; Backx, F.J.G.; Westerveld, R.A.; Takken, T. Arm cranking versus wheelchair propulsion for testing aerobic fitness in children with spina bifida who are wheelchair dependent. J. Rehabil. Med. 2015, 47, 432–437. [Google Scholar] [CrossRef] [PubMed]
- Weissland, T.; Faupin, A.; Borel, B.; Lepretre, P.-M. Comparison Between 30-15 Intermittent Fitness Test and Multistage Field Test on Physiological Responses in Wheelchair Basketball Players. Front. Physiol. 2015, 6, 380. [Google Scholar] [CrossRef]
- Bongers, B.C.; Rijks, E.B.G.; Harsevoort, A.G.J.; Takken, T.; van Brussel, M. 10-m shuttle ride test in youth with osteogenesis imperfecta who use wheelchairs: Feasibility, reproducibility, and physiological responses. Phys. Ther. 2016, 96, 679–686. [Google Scholar] [CrossRef] [PubMed]
- Bloemen, M.A.T.; De Groot, J.F.; Backx, F.J.G.; Benner, J.; Kruitwagen, C.L.J.J.; Takken, T. Wheelchair shuttle test for assessing aerobic fitness in youth with spina bifida: Validity and reliability. Phys. Ther. 2017, 97, 1020–1029. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Tejero, J.; Coterón, J.; Rabadán, M.; Sampedro, J. Field test validation for wheelchair basketball players’ aerobic capacity assessment. Eur. J. Hum. Mov. 2018, 40, 136–148. [Google Scholar]
- Simmelink, E.K.; Wempe, J.B.; Geertzen, J.H.B.; van der Woude, L.H.V.; Dekker, R. Feasibility, safety, and reliability of exercise testing using the combined arm-leg (Cruiser) ergometer in subjects with a lower limb amputation. PLoS ONE 2018, 13, e0202264. [Google Scholar] [CrossRef]
- Qi, L.; Zhang, L.; Lin, X.-B.; Ferguson-Pell, M. Wheelchair propulsion fatigue thresholds in electromyographic and ventilatory testing. Spinal Cord. 2020, 58, 1104–1111. [Google Scholar] [CrossRef]
- Damen, K.M.S.; Takken, T.; De Groot, J.F.; Backx, F.J.G.; Radder, B.; Roos, I.C.P.M.; Bloemen, M.A.T. 6-minute push test in youth who have spina bifida and who self-propel a wheelchair: Reliability and physiologic response. Phys. Ther. 2020, 100, 1852–1861. [Google Scholar] [CrossRef]
- Goosey-Tolfrey, V.L.; Groot, S.; De Tolfrey, K.; Paulson, T.A.W. Criterion Validity of a Field-Based Assessment of Aerobic Capacity in Wheelchair Rugby Athletes. Int. J. Sports Physiol. Perform. 2021, 16, 1341–1346. [Google Scholar] [CrossRef] [PubMed]
- Holm, N.J.; Biering-Sorensen, F.; Schou, L.H.; Møller, T. The test-retest reliability of individualized VO2peak test modalities in people with spinal cord injury undergoing rehabilitation. Spinal Cord. 2021, 59, 82–91. [Google Scholar] [CrossRef] [PubMed]
- Shushan, T.; Lovell, R.; McLaren, S.J.; Buchheit, M.; Dello Iacono, A.; Arguedas-Soley, A.; Norris, D. Assessing criterion and longitudinal validity of submaximal heart rate indices as measures of cardiorespiratory fitness: A preliminary study in football. J. Sci. Med. Sport. 2024, 27, 565–571. [Google Scholar] [CrossRef] [PubMed]
- Janssen, R.J.F.; De Groot, S.; Van Der Woude, L.H.V.; Houdijk, H.; Vegter, R.J.K. Toward a Standardized and Individualized Laboratory-Based Protocol for Wheelchair-Specific Exercise Capacity Testing in Wheelchair Athletes: A Scoping Review. Am. J. Phys. Med. Rehabil. 2023, 102, 261–269. [Google Scholar] [CrossRef]
- Ham, S.A.; Yore, M.M.; Fulton, J.E.; Kohl, I.I.I.H.W. Prevalence of No Leisure-Time Physical Activity—35 States and the District of Columbia, 1988–2002. JAMA 2004, 291, 1693. [Google Scholar] [CrossRef][Green Version]
- Jack, L.P.; Purcell, M.; Allan, D.B.; Hunt, K.J. Comparison of peak cardiopulmonary performance parameters during robotics-assisted treadmill exercise and arm crank ergometry in incomplete spinal cord injury. Technol. Health Care 2010, 18, 285–296. [Google Scholar] [CrossRef]
| Study | OR | OV | R1 | R2 | R3 | R4 | R5 | R6 | R7 | R8 | R9 | V1 | V2 | V3 | V4 | V5 | V6 * | V7 * |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Wicks et al. [16] | - | 4 | 3 | 2 | 1 | 4 | 2 | 2 | 1 | |||||||||
| Kofsky et al. [52] | - | 3 | 2 | 2 | 3 | 1 | 1 | |||||||||||
| Bhambhani et.al. [19] | 4 | - | 1 | 1 | 2 | 1 | 1 | 4 | - | 3 | 1 | |||||||
| Langbein et al. [17] | 3 | 2 | 1 | 1 | 2 | 1 | 3 | 2 | - | 3 | 1 | 2 | 1 | 2 | 1 | 1 | ||
| Bhambhani et al. [20] | 4 | 3 | 1 | 1 | 2 | 1 | 2 | 4 | - | 3 | 1 | 3 | 3 | 1 | 1 | 1 | ||
| Bhambhani et al. [21] | 4 | - | 1 | 1 | 2 | 1 | 2 | 4 | - | 3 | 1 | |||||||
| Hartung et al. [44] | 4 | 4 | 1 | 1 | 2 | 3 | 2 | 4 | - | 2 | 1 | 3 | 2 | 1 | 4 | 2 | 2 | 1 |
| Bhambhani et al. [18] | - | 3 | 1 | 3 | 2 | 1 | 1 | |||||||||||
| Holland et al. [53] | 4 | - | 1 | 1 | 2 | 1 | 4 | 4 | - | 3 | 1 | |||||||
| Longimuir et al. [42] | 3 | 4 | 1 | 1 | 1 | 1 | 1 | 3 | - | 3 | 1 | 2 | 2 | 4 | 4 | 1 | ||
| Vinet et al. [54] | - | 3 | 2 | 3 | 3 | 1 | 1 | |||||||||||
| Dwyer et al. [41] | - | 3 | 1 | 3 | 3 | 1 | 3 | |||||||||||
| Poulain et al. [55] | 4 | - | 1 | 1 | 2 | 1 | 1 | 4 | 1 | 4 | 1 | |||||||
| Vanlandewijck et al. [56] | 4 | 3 | 1 | 1 | 2 | 1 | 1 | 4 | - | 3 | 1 | 2 | 3 | 2 | 1 | 1 | ||
| Stewart et al. [57] | 4 | - | 1 | 1 | 3 | 4 | 2 | 1 | - | 2 | 1 | |||||||
| Vinet et al. [58] | - | 2 | 2 | 2 | 1 | 1 | 1 | |||||||||||
| Vanderthomen et al. [34] | 4 | 3 | 1 | 1 | 1 | 1 | 1 | 4 | 1 | 2 | 1 | 2 | 3 | 1 | 1 | 1 | ||
| Laskin et al. [39] | 4 | 3 | 1 | 1 | 2 | 1 | 2 | 4 | 1 | 1 | 1 | 2 | 3 | 2 | 1 | 1 | ||
| Hol et al. [23] | 3 | 2 | 1 | 1 | 2 | 1 | 2 | 3 | 2 | 1 | 1 | 2 | 2 | 2 | 1 | 1 | ||
| Goosey-Tolfrey et al. [59] | 4 | 3 | 1 | 1 | 2 | 1 | 1 | 4 | 1 | 1 | 1 | 1 | 3 | 2 | 1 | 1 | ||
| Leicht et al. [60] | 4 | - | 1 | 1 | 1 | 1 | 1 | 4 | 2 | 2 | 1 | |||||||
| Cowan et al. [40] | 3 | 4 | 1 | 1 | 2 | 1 | 2 | 3 | 1 | 1 | 1 | 1 | 2 | 2 | 4 | 3 | ||
| Verschuren et al. [61] | 4 | 3 | 1 | 1 | 2 | 1 | 1 | 4 | 1 | 1 | 1 | 2 | 3 | 2 | 1 | 1 | ||
| Verschuren et al. [43] | 2 | - | 1 | 1 | 2 | 1 | 1 | 2 | 1 | 1 | 1 | |||||||
| Goosey-Tolfrey et al. [62] | - | 4 | 1 | 3 | 2 | 4 | 1 | |||||||||||
| Weissland et al. [63] | - | 4 | 1 | 1 | 1 | 4 | 2 | 2 | 1 | |||||||||
| Bloemen et al. [64] | 4 | 4 | 1 | 1 | 1 | 1 | 1 | 4 | 1 | 1 | 1 | 3 | 3 | 3 | 4 | 1 | ||
| Yanci et al. [36] | 4 | - | 1 | 1 | 1 | 1 | 1 | 4 | - | 2 | 1 | |||||||
| Weissland et al. [65] | - | 4 | 3 | 1 | 3 | 4 | 2 | 2 | 1 | |||||||||
| de Groot et al. [33] | - | 3 | 2 | 3 | 1 | 1 | 1 | |||||||||||
| Bongers et al. [66] | 4 | 3 | 1 | 1 | 2 | 1 | 1 | 4 | 1 | 1 | 1 | 2 | 3 | 1 | 1 | 1 | ||
| Gauthier et al. [4] | 4 | - | 1 | 1 | 1 | 1 | 1 | 4 | 1 | 1 | 1 | |||||||
| Bloemen et al. [67] | 4 | 2 | 1 | 1 | 2 | 1 | 1 | 4 | 1 | 1 | 1 | 1 | 2 | 2 | 1 | 1 | ||
| Kelly et al. [45] | 4 | - | 1 | 1 | 1 | 1 | 1 | 4 | 2 | 2 | 1 | |||||||
| Pérez Tejero et al. [68] | - | 3 | 2 | 3 | 2 | 1 | 1 | |||||||||||
| Simmelink et al. [69] | 4 | - | 1 | 1 | 2 | 1 | 3 | 4 | 1 | 1 | 1 | |||||||
| Christensen et al. [22] | 4 | - | 1 | 1 | 2 | 1 | 2 | 4 | 1 | 1 | 1 | |||||||
| Morgan et al. [24] | 4 | 3 | 1 | 1 | 2 | 1 | 1 | 4 | 1 | 1 | 1 | 2 | 3 | 2 | 1 | 1 | ||
| Qi et al. [70] | - | 4 | 1 | 3 | 1 | 4 | 1 | |||||||||||
| Damen et al. [71] | 4 | 4 | 1 | 1 | 2 | 1 | 1 | 4 | 1 | 1 | 1 | 1 | 1 | 2 | 4 | 1 | ||
| Goosey-Tolfrey et al. [72] | - | 4 | 2 | 3 | 2 | 4 | 1 | |||||||||||
| Holm et al. [73] | 4 | - | 1 | 1 | 1 | 1 | 1 | 4 | - | 1 | 1 |
| Study | Test | Tests Characteristics | Disability/Sport | Participants Sex and Age (Years) | Reliability (Relative and/or Absolute) | Criterion (CRI) or Convergent (CON) Validity |
|---|---|---|---|---|---|---|
| Wicks et al. [16] | Maximal WE speed test | 20 rpm + 10 or 5 rpm/min with low resistance | SCI (n = 2M were able-bodied) | n = 3F 4M 28.1 ± 4.1 (23–34) | CON No significant differences | |
| Maximal WE speed test | 20 rpm + 10 or 5 rpm/min with high resistance | |||||
| Maximal ACE resistance test | 60 rpm + 25-50-100 kpm/min | |||||
| Bhambhani et al. [19] | Maximal WE cadence test | 40 strikes/min + 8 strikes/min/2 min | PP and TT | n = 2F 5M 26.5 ± 3.5 (22–32) | r = 0.98 * t test no differences | |
| Langbein et al. [17] | Maximal WE resistance test | 6 W + 5-20 W/3 min (continuous and intermittent) | TT, PP, amputations and lower limb fractures | n = 51M (17–69) | r = 0.9 * | CRI No significant differences r = 0.91 * |
| Bhambhani et al. [20] | Maximal WE speed test | 5 km/h + 2 km/h/2 min | CP athletes, national and international level | n = 6M 24.8 ± 3.7 (19–29) | r = 0.89 * | CRI r < 0.31 (n = 4) |
| Bhambhani et al. [21] | Maximal WE speed test | 5 km/h + 2 km/h/2 min with 1 min rest | CP athletes, national and international level | n = 11M 25.1 ± 4.3 (19–33) | r = 0.89 *, 0.9 * | |
| Hartung et al. [44] | Maximal TM grade and speed test | 3.2 km/h + 1.6 km/h & 0.5% every 2 min | PP and low extremity polio disability | n = 7M 33 (21–44) | ICC = 0.86 *, 0.87 * | CON ANOVA, no differences |
| Maximal TM grade test | 0 + 1%/2 min at 4.8 km/h | ICC = 0.41 *, 0.44 * | ||||
| Maximal TM speed test | 3.2 + 3.2 km/h/2 min | ICC = 0.40 *, 0.83 * | ||||
| Bhambhani et al. [18] | Simulated 1.6 km race in WE | 1.6 km simulated race | TT Actives | n = 7M 30.6 ± 5.2 | CRI r = 0.79 *, 0.81 *, 0.23, 0.32 | |
| Simulated 3.2 km race in WE | 3.2 km simulated race | PP Actives | n = 6M 29.0 ± 4.6 | CRI r = 0.82 *, 0.88 *, 0.19, 0.61 | ||
| Holland et al. [53] | Maximal WE speed test | 4 km/h + 1 km/h/2 min | CP | n = 1F 4M 25.6 ± 3.7 (21–31) | r = 0.79 *, 0.83 * (Data mixed with cycle ergometer test) | |
| Longimuir et al. [42] | Arm CAFT | Submaximal 3 × 3 min in ACE (Stopping when achieving a certain HR, load dependant on sex and age) | Different physical disabilities | n = 18F 17 M (21–59) | r = 0.97 * (n = 30) | CRI Paired t test, no differences |
| Stewart et al. [57] | Maximal ACE resistance test/maximal WE resistance test | 15 W + 15 W/3 min +7.5 W/3 min (after RPE15) with 2 min recovery | SCI | n = 19F 83M 29.7 ± 10.3 | ICC = 0.82 * | |
| Hol et al. [23] | 6-MAT | Submaximal 6 min at 60–70% HR max in ACE | PP and TT | n = 5F 25M 36.3 ± 9.3 (19–49) | ICC = 0.81 * (0.58–0.92) SEM = 1.62 mL/kg/min | CRI r = 0.92 *, 0.73 *, 0.63 * |
| Leicht et al. [60] | Maximal TM grade test | Individualized speed 1% + 0.3/min or 0.1/40 s | WR, WB and WT; national and international | n = 24M 28.1 ± 5.2 (TT) 31.7 ± 8.7 (PP) 24.0 ± 6.2 (non-SCI) | ICC = 0.84–0.99 * CV = 9.3% (TT), 4.5% (PP), 3.3% (non-SCI) | |
| Goosey-Tolfrey et al. [62] | Submaximal TM speed test | 6 × 4 min | WR and WB players; elite level | n = 26M 30 ± 5 (TT) 29 ± 9 (PP) 27 ± 8 (non-SCI) | CRI TE = 0.14–0.16 L/min (TT) 0.19–0.22 L/min (PP) 0.54–68 L/min (non-SCI) CV = 10.1–11.1% (TT) 6.5–7.5% (PP) 16.8–20.2% (non-SCI) | |
| Bloemen et al. [64] | Maximal WE resistance test | 0 + 0.1 torque/min at 60–80 rpm | Spina bifida wheelchair users | n = 4F 9M 13.4 ± 3.5 (8–17) | CRI t test, no difference VO2peak 15% greater than ACE test | |
| n = 11F 13M 14.8 ± 3.0 (8–19) | ICC = 0.93 * (0.83–0.97) SEM = 1.87 mL/kg/min SDC = 5.18 mL/kg/min | |||||
| Gauthier et al. [4] | Maximal TM grade and speed test | Different slope and speed increases every 1 min | Wheelchair users | n = 21F 4M 35.3 ± 14.9 (18–63) | ICC = 0.84 * (0.66–0.92), 0.86 * (0.70–0.93) SDC = 2.27 mL/kg/min, 157.9 mL/min SEM = 5.3 mL/kg/min, 368.5 mL/min | |
| Simmelink et al. [69] | Maximal ALE resistance test | 3 min 20 W + 10 W/min at 50 rpm | Unilateral lower limb amputation | n = 3F 14M 54.5 ± 18.6 (25–80) | ICC = 0.84 * (0.61–0.94), 0.91 * (0.77–0.97) LoA = −0.56 to 0.60 L/min | |
| Christensen et al. [22] | Maximal ACE resistance test | 40 W+ 20 W/min | Unilateral lower limb amputation | n = 8M 32.5 ± 4.6 (18–40) | ICC = 0.51 * (0.11–0.85), 0.73 * (0.40–0.93), 0.74 * (0.40–0.93) CV = 14.48% SEM = 0.18 L/min LoA = −0.66 to 0.40 L/min | |
| Morgan et al. [24] | Maximal WE resistance test | Increasing resistance every minute at 70% of max speed | SCI 70% athletes | n = 10M 33 ± 19.6 (18–60) | ICC = 0.82 *, 0.97 * LoA = −6 to 4.5 mL/kg/min | CRI r = 0.79 *, 0.77 * t test, no differences LoA = −4.1 to 3.6 mL/kg/min |
| Qi et al. [70] | Maximal WE resistance test | 10 W + 5 or 10 W/min at 1 m/s | SCI | n = 3F 7M 42.1 ± 8.4 (29–55) | CRI ICC = 0.91 * | |
| Holm et al. [73] | Maximal ACE resistance test | 5 W + 10 W/min at 60 rpm | SCI | n = 1F 4M 47 ± 25.6 (21–83) | ICC = 0.99 * | |
| mTBRS-XT | 25 W + 15 W/2 min in ALE | SCI | n = 3F 6M 61.7 ± 13.3 (41–76) | ICC = 0.96 * | ||
| TBRS-XT | 50 W + 25 W/2 min in ALE | SCI | n = 1F 7M 44.3 ± 15.6 (27–75) | ICC = 0.99 * |
| Studies | Test | Reliability | Validity |
|---|---|---|---|
| Langbein et al. [17] | Maximal WE resistance test | Limited | Moderate |
| Hol et al. [23] | 6-MAT | Limited | Moderate |
| Bhambhani et al. [20] | Maximal WE speed test | ? | Limited |
| Morgan et al. [24] | Maximal WE resistance test | ? | Limited |
| Bhambhani et al. [18] | Simulated 1.6 km race in WE | N/A | Limited |
| Bhambhani et al. [18] | Simulated 3.2 km race in WE | N/A | Limited |
| Longimuir et al. [42] | Arm CAFT | Limited | ? |
| Study | Test | Tests Characteristics | Disability/Sport | Participants Sex and Age (Average, Standard Deviation and Range) | Reliability (Relative and Absolute) | Criterion (CRI) or Convergent (CON) Validity |
|---|---|---|---|---|---|---|
| Kofsky et al. [52] | Submaximal field test | 3 × 5 min at 40-60-80% HRmax with 2 min rest | Lower limb disabilities; sedentary individuals, active individuals and athletes | n = 7F 28.7 ± 3.4 (18–55) | CRI r = 0.61 * | |
| n = 42M 28.2 ± 1.3 (18–55) | CRI r = 0.67 * | |||||
| Vinet et al. [54] | ALBT | 4 km/h + 1 km/h/min in 400 m tartan | WT and WRA | n = 9M 28.9 ± 4.2 (24–35) | CRI r = 0.65 * Wilcoxon, no differences LoA ≃ −7 to 14 mL/kg/min | |
| Dwyer et al. [41] | 12WPT | Maximal distance in 12 min in 200 m indoor tartan | WB national level | n = 13F 26 ± 6 (19–40) | CRI r = 0.46 *, 0.30 | |
| Poulain et al. (1999) [55] | ALBT | 4 km/h + 1 km/h/min in 400 m tartan | WT, WRA, WTT; regional, national and international level | n = 8M 30.8 ± 5.1 (24–39) | No significant differences (MANOVA) LoA ≃ −2 to 1.2 km/h CV = 2% | |
| Vanlandewijck et al. [56] | SWT | 5 km/h + 0.5 km/h/min between two marks 25 m away | WB national level | n = 20M 31.7 ± 10.4 (14–46) | r = 0.97 * | CRI r = 0.64 *, 0.87 *, (n = 15) |
| Vinet et al. [58] | ALBT | 4 km/h + 1 km/h/min in 400 m tartan | WB, WRA, WF or AS | n = 9F 40M 30.3 ± 0.4 (18–47) | CRI r = 0.81 * | |
| Vanderthomen et al. [34] | MFT in octagon | 6 km/h + 0.37 km/h/min in a 15 m × 15 m octagon | PP and post-polio | n = 10M 38.2 ± 13.0 | ICC = 0.99 *, 0.88 * LoA ≃ −1.4 to 1.8 stages −4.4/4.6 mL/kg/min | CRI r = 0.77 * |
| Laskin et al. [39] | Cadence-based submaximal field test | 5 min 60 pushes/min in a basketball court | WB, elite level | n = 24M 26.1 ± 6.6 | ICC = 0.50 * LoA = −0.83/1.05 L/min (n = 16) | CRI r = 0.49 * t test, no differences |
| Cadence-based submaximal field test | 5 min 80 pushes/min in a basketball court | WB, elite level | n = 24M 26.1 ± 6.6 | ICC = 0.62 * LoA = −0.66 to 1.06 L/min (n = 16) | CRI r = 0.56 * t test, no differences | |
| Goosey-Tolfrey et al. [59] | SWT | 8.5 km/h + 0.5 km/h/min between two marks 20 m away | WB, international level | n = 24M 29 ± 6 | ICC = 0.88 * (0.58–0.97), 0.91 * (0.69–0.98) SEM = 2.4 beats/min, 86 m CV = 1.3%, 4.4% (n = 10) | CRI r = 0.57 * |
| Cowan et al. [40] | 6MPT | Maximal distance in 6 min surrounding two cones 15 m away | PP and TT | n = 6F 34M 34 ± 10 (20–45) | ICC = 0.97 * (0.94–0.98) (All), 0.93 (0.80–0.98) (TT), 0.97 (0.93–0.99) (PP) LoA ≈ −70 to 65 m (All) | CRI ICC = 0.86 * (0.75–0.92) (All), 0.86 (0.70–0.93) (PP), 0.65 (0.17–0.87) (TT) |
| Verschuren et al. [61] | SWT | 2 km/h + 0.25 km/h/min between two marks 10 m away | Spastic CP | n = 5F 18M 13.3 ± 3.6 | ICC = 0.99 * (0.98–1.00) SEM = 0.5 min SDC = 1.4 min LoA ≃ −1.45 to 1.45 stages | CRI r = 0.84 * (n = 15) |
| Verschuren et al. [43] | 6MPT | Maximal distance in 6 min surrounding two marks 10 m away | Spastic CP | n = 22F 51M 11.8 ± 3.6 (4–18) | ICC = 0.97 * (0.96–0.98) SEM = 20.9 m SDC = 57.9 m LoA ≃ −54.8 to 62.2 m | |
| Weissland et al. [63] | MFT in octagon | 6 km/h + 0.37 km/h/min in a 15 m × 15 m octagon | WB, national level | n = 2F 14M 32.4 ±5.3 (23–41) | CON Student’s t test, differences r = 0.93 *, 0.84 * | |
| MFT in 8 figure | 6 km/h + 0.37 km/h/min in 32 m × 15 m “8 figure” | |||||
| Yanci et al. [36] | Yoyo intermittent recovery test | 2 × 10 m with 10 s active recovery increasing speed | WB, national level | n = 2F 14 M 33.1 ± 7.4 (21–46) | ICC = 0.94 * | |
| Weissland et al. [65] | MFT in octagon | 6 km/h + 0.37 km/h/min in a 15 m × 15 m octagon | WB, national level | n = 2F 16M 32.0 ± 5.7 (22–41) | CON Student’s t test, no differences r = 0.84 * LoA ≃ −8 to 7 mL/kg/min | |
| 30-15ITF | 6 km/h + 0.5 km/h/45 s in 40 m (30 s push–15 s rest) | |||||
| de Groot et al. [33] | SWT | 5 km/h + 0.32 km/h/min between two marks 20 m away | WT, national and international level | n = 15M 21.2 ± 8.4 | CON r = 0.40, 0.47 | |
| Bongers et al. [66] | SWT | 2 km/h + 0.25 km/h/min between two marks 10 m away | Osteogenesis imperfecta wheelchair users | n = 5F 8 M 15.5 ± 6.4 (9–25) | ICC = 0.95 * (0.83–0.98), 0.97 * (0.89–0.99), 0.92 * (0.71–0.98) SEM = 0.7 stages SDC = 1.9 stages LoA = −2.5 to 1.35 stages t test no differences | CRI r = 0.61 *, 0.45 |
| Bloemen et al. [67] | SWT | 2 km/h + 0.25 km/h/min between two marks 10 m away | Spina bifida wheelchair users, in daily life or in sports | n = 17F 16M 14.5 ± 3.1 (5–18) | CRI r = 0.85 *, 0.84 * t test, no differences | |
| n = 12F 16M 14.7 ± 3.3 (5–18) | ICC = 0.96 * (0.92–0.98), 0.93 * (0.84–0.97), 0.98 * (0.96–0.99) CV = 6.2%, 6.4% SDC = 1.5 shuttles SEM = 0.5 shuttles | |||||
| Kelly et al. [45] | 30-15IFT-28m | 8 km/h + 0.5 km/h/min in 28 m (30 s push–15 s rest) | WR, international level | n = 10M 31.8 ± 7.3 (20–44) | ICC = 0.99 * SEM = 1.02 km/h CV = 1.9% LoA = −0.51 to 0.61 km/h | |
| Pérez Tejero et al. [68] | SWT | 6 km/h + 0.5 km/h/min between two marks at 28 m | WB, elite level | n = 7M 33.3 ± 6.0 (27–44) | CRI r = 0.85 * | |
| Damen et al. [71] | 6MPT | Maximal distance in 6 min surrounding two cones 10 m away | Spina bifida wheelchair users, in daily life or in sport | n = 21F 32M (n = 8 lost) 13.6 ± 3.8 (5–19) | CRI 86% (18.5) of maximal VO2 | |
| n = 14F 12M (n = 5 lost) 13.6 ± 3.8 (5–19) | ICC = 0.95 * (0.83–0.98) SDC = 60.7 m SEM = 21.9 m | |||||
| Goosey-Tolfrey et al. [72] | MFT in 8 figure | 6.5 km/h + 0.36 km/h/min in 28.2 m × 10.8 m “8 figure” | WR, national level | n = 16M 28 ± 6 | CRI Paired t test, no differences |
| Studies | Test | Reliability | Validity |
|---|---|---|---|
| Bloemen et al. [67]; Bongers et al. [66]; Verschuren et al. [61] | SWT | ? | Moderate |
| Vinet et al. [54]; Vinet et al. [58] | ALBT | N/A | Moderate |
| Verschuren et al. [43] | 6MPT | Moderate | ? |
| Vanlandewijck et al. [56] | SWT | ? | Limited |
| Vanderthomen et al. [34] | MFT in octagon | ? | Limited |
| Laskin et al. [39] | Cadence-based submaximal field test | ? | Limited |
| Goosey-Tolfrey et al. [59] | SWT | ? | Limited |
| Kofsky et al. [52] | Submaximal field test | N/A | Limited |
| Dwyer et al. [41] | 12WPT | N/A | Limited |
| de Groot et al. [33] | SWT | N/A | Limited |
| Pérez Tejero et al. [68] | SWT | N/A | Limited |
| Cowan et al. [40] | 6MPT | Limited | ? |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Garate, I.; Yanci, J.; Ascondo, J.; Iturricastillo, A.; Granados, C. Reliability and Validity of Laboratory and Field Cardiorespiratory Exercise Tests for Wheelchair Users: A Systematic Review. Int. J. Environ. Res. Public Health 2025, 22, 384. https://doi.org/10.3390/ijerph22030384
Garate I, Yanci J, Ascondo J, Iturricastillo A, Granados C. Reliability and Validity of Laboratory and Field Cardiorespiratory Exercise Tests for Wheelchair Users: A Systematic Review. International Journal of Environmental Research and Public Health. 2025; 22(3):384. https://doi.org/10.3390/ijerph22030384
Chicago/Turabian StyleGarate, Iker, Javier Yanci, Josu Ascondo, Aitor Iturricastillo, and Cristina Granados. 2025. "Reliability and Validity of Laboratory and Field Cardiorespiratory Exercise Tests for Wheelchair Users: A Systematic Review" International Journal of Environmental Research and Public Health 22, no. 3: 384. https://doi.org/10.3390/ijerph22030384
APA StyleGarate, I., Yanci, J., Ascondo, J., Iturricastillo, A., & Granados, C. (2025). Reliability and Validity of Laboratory and Field Cardiorespiratory Exercise Tests for Wheelchair Users: A Systematic Review. International Journal of Environmental Research and Public Health, 22(3), 384. https://doi.org/10.3390/ijerph22030384








