Digital Mental Health Interventions: Differences in Diet Culture Intervention Framing
Abstract
:1. Introduction
2. Materials and Methods
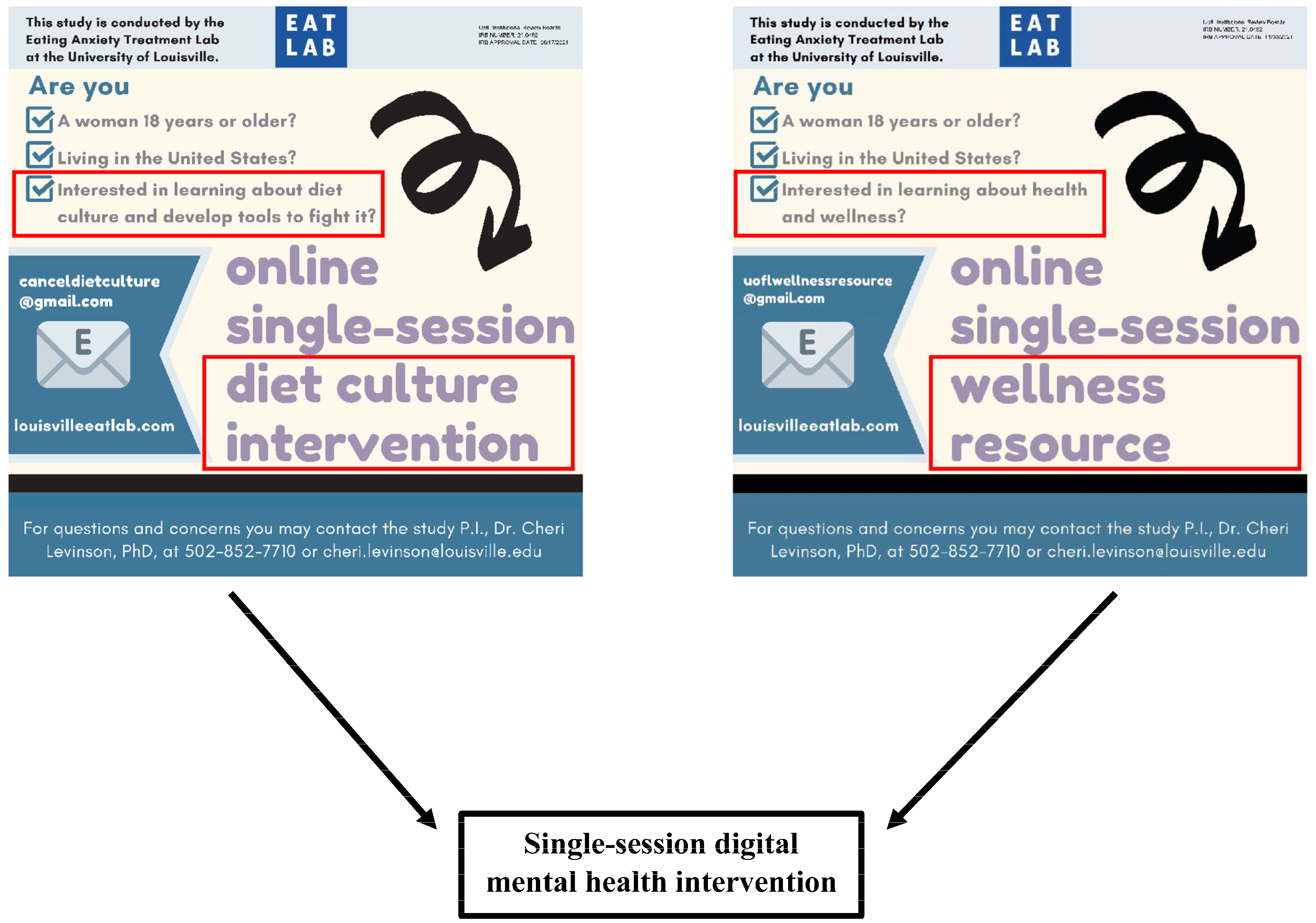
2.1. Procedures
2.2. Participants
2.3. Measures
2.3.1. ED Pathology
2.3.2. Body Image
2.3.3. Weight Stigma Concerns
2.3.4. Fat Acceptance
2.3.5. Scoring Thresholds
2.4. Data Analyses
3. Results
3.1. Overall Descriptives
3.2. Differences between Groups
3.3. Differences between Recruitment Sources
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Jovanovski, N.; Jaeger, T. Demystifying ‘diet culture’: Exploring the meaning of diet culture in online ‘anti-diet’ feminist, fat activist, and health professional communities. Women’s Stud. Int. Forum 2022, 90, 102558. [Google Scholar] [CrossRef]
- Bulik, C.M.; Blake, L.; Austin, J. Genetics of eating disorders: What the clinician needs to know. Psychiatr. Clin. 2019, 42, 59–73. [Google Scholar] [CrossRef]
- Asch, D.A.; Buresh, J.; Allison, K.C.; Islam, N.; Sheils, N.E.; Doshi, J.A.; Werner, R.M. Trends in US patients receiving care for eating disorders and other common behavioral health conditions before and during the COVID-19 pandemic. JAMA Netw. Open 2021, 4, e2134913. [Google Scholar] [CrossRef] [PubMed]
- Chesney, E.; Goodwin, G.M.; Fazel, S. Risks of all-cause and suicide mortality in mental disorders: A meta-review. World Psychiatry 2014, 13, 153–160. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.; Ata, R.N.; Brannick, M.T. Malleability of weight-biased attitudes and beliefs: A meta-analysis of weight bias reduction interventions. Body Image 2014, 11, 251–259. [Google Scholar] [CrossRef] [PubMed]
- Pearl, R.L.; Groshon, L.C.; Fitterman-Harris, H.F. Weight Stigma. In Encyclopedia of Mental Health, 3rd ed.; Markey, C., Friedman, H.S., Eds.; Elsevier Press: Amsterdam, The Netherlands, 2022. [Google Scholar]
- Brochu, P.M. Weight stigma as a risk factor for suicidality. Int. J. Obes. 2020, 44, 1979–1980. [Google Scholar] [CrossRef]
- Papadopoulos, S.; Brennan, L. Correlates of weight stigma in adults with overweight and obesity: A systematic literature review. Obesity 2015, 23, 1743–1760. [Google Scholar] [CrossRef]
- Pearl, R.L.; Puhl, R.M.; Lessard, L.M.; Himmelstein, M.S.; Foster, G.D. Prevalence and correlates of weight bias internalization in weight management: A multinational study. SSM-Popul. Health 2021, 13, 100755. [Google Scholar] [CrossRef]
- Tomiyama, A.J. Weight stigma is stressful. A review of evidence for the Cyclic Obesity/Weight-Based Stigma model. Appetite 2014, 82, 8–15. [Google Scholar] [CrossRef]
- Vartanian, L.R.; Porter, A.M. Weight stigma and eating behavior: A review of the literature. Appetite 2016, 102, 3–14. [Google Scholar] [CrossRef]
- Hunger, J.M.; Major, B. Weight stigma mediates the association between BMI and self-reported health. Health Psychol. 2015, 34, 172. [Google Scholar] [CrossRef] [PubMed]
- Alberga, A.S.; Edache, I.Y.; Forhan, M.; Russell-Mayhew, S. Weight bias and health care utilization: A scoping review. Prim. Health Care Res. Dev. 2019, 20, e116. [Google Scholar] [CrossRef] [PubMed]
- Graham, A.K.; Lattie, E.G.; Powell, B.J.; Lyon, A.R.; Smith, J.D.; Schueller, S.M.; Stadnick, N.A.; Brown, C.H.; Mohr, D.C. Implementation strategies for digital mental health interventions in health care settings. Am. Psychol. 2020, 75, 1080. [Google Scholar] [CrossRef] [PubMed]
- Hom, M.A.; Stanley, I.H.; Joiner, T.E., Jr. Evaluating factors and interventions that influence help-seeking and mental health service utilization among suicidal individuals: A review of the literature. Clin. Psychol. Rev. 2015, 40, 28–39. [Google Scholar] [CrossRef] [PubMed]
- Schleider, J.L.; Dobias, M.; Sung, J.; Mumper, E.; Mullarkey, M.C. Acceptability and utility of an open-access, online single-session intervention platform for adolescent mental health. JMIR Ment. Health 2020, 7, e20513. [Google Scholar] [CrossRef] [PubMed]
- Wasil, A.R.; Taylor, M.E.; Franzen, R.E.; Steinberg, J.S.; DeRubeis, R.J. Promoting graduate student mental health during COVID-19: Acceptability, feasibility, and perceived utility of an online single-session intervention. Front. Psychol. 2021, 12, 569785. [Google Scholar] [CrossRef]
- Kessler, R.C.; Demler, O.; Frank, R.G.; Olfson, M.; Pincus, H.A.; Walters, E.E.; Wang, P.; Wells, K.B.; Zaslavsky, A.M. Prevalence and treatment of mental disorders, 1990 to 2003. N. Engl. J. Med. 2005, 352, 2515–2523. [Google Scholar] [CrossRef]
- Baumel, A.; Muench, F.; Edan, S.; Kane, J.M. Objective user engagement with mental health apps: Systematic search and panel-based usage analysis. J. Med. Internet Res. 2019, 21, e14567. [Google Scholar] [CrossRef]
- Linardon, J.; Shatte, A.; Rosato, J.; Fuller-Tyszkiewicz, M. Efficacy of a transdiagnostic cognitive-behavioral intervention for eating disorder psychopathology delivered through a smartphone app: A randomized controlled trial. Psychol. Med. 2022, 52, 1679–1690. [Google Scholar] [CrossRef]
- Teo, A.R.; Liebow, S.B.; Chan, B.; Dobscha, S.K.; Graham, A.L. Reaching those at risk for psychiatric disorders and suicidal ideation: Facebook advertisements to recruit military veterans. JMIR Ment. Health 2018, 5, e10078. [Google Scholar] [CrossRef]
- Choi, I.; Milne, D.N.; Glozier, N.; Peters, D.; Harvey, S.B.; Calvo, R.A. Using different Facebook advertisements to recruit men for an online mental health study: Engagement and selection bias. Internet Interv. 2017, 8, 27–34. [Google Scholar] [CrossRef] [PubMed]
- Merriam-Webster. Wellness. Available online: https://www.merriam-webster.com/dictionary/wellness (accessed on 23 June 2023).
- Merriam-Webster. Health. Available online: https://www.merriam-webster.com/dictionary/health (accessed on 23 June 2023).
- Marks, R.J.; De Foe, A.; Collett, J. The pursuit of wellness: Social media, body image and eating disorders. Child. Youth Serv. Rev. 2020, 119, 105659. [Google Scholar] [CrossRef]
- Bardone-Cone, A.M.; Thompson, K.A.; Miller, A.J. The self and eating disorders. J. Personal. 2020, 88, 59–75. [Google Scholar] [CrossRef] [PubMed]
- Vanzhula, I.A. Manipulating Mindful Breathing Versus Mindful Eating: Examining the Effect of Specific Mindfulness Mechanisms on Food Intake and Eating Disorder Symptoms. Ph.D. Dissertation, University of Louisville, Louisville, KY, USA, 2021. [Google Scholar]
- Fairburn, C.G.; Beglin, S. Eating disorder examination questionnaire. In Cognitive Behavior Therapy for Eating Disorders; Fairburn, C.G., Ed.; Guilford Press: New York, NY, USA, 2008. [Google Scholar]
- Hohlstein, L.A.; Smith, G.T.; Atlas, J.G. An application of expectancy theory to eating disorders: Development and validation of measures of eating and dieting expectancies. Psychol. Assess. 1998, 10, 49. [Google Scholar] [CrossRef]
- Levinson, C.A.; Vanzhula, I.A.; Christian, C. Development and validation of the eating disorder fear questionnaire and interview: Preliminary investigation of eating disorder fears. Eat. Behav. 2019, 35, 101320. [Google Scholar] [CrossRef] [PubMed]
- Stice, E.; Schupak-Neuberg, E.; Shaw, H.E.; Stein, R.I. Relation of media exposure to eating disorder symptomatology: An examination of mediating mechanisms. J. Abnorm. Psychol. 1994, 103, 836. [Google Scholar] [CrossRef]
- Ralph-Nearman, C.; Filik, R. Development and validation of new figural scales for female body dissatisfaction assessment on two dimensions: Thin-ideal and muscularity-ideal. BMC Public Health 2020, 20, 1114. [Google Scholar] [CrossRef]
- Tylka, T.L.; Wood-Barcalow, N.L. The Body Appreciation Scale-2: Item refinement and psychometric evaluation. Body Image 2015, 12, 53–67. [Google Scholar] [CrossRef]
- Kase, C.A.; Mohr, J.J. The Fat Acceptance Scale: Development and initial validation. J. Couns. Psychol. 2022, 69, 311. [Google Scholar] [CrossRef]
- Field, A. Discovering Statistics Using IBM SPSS Statistics, 4th ed.; Carmichael, M., Ed.; SAGE Publications Ltd.: London, UK, 2013. [Google Scholar]
- Fiuza, A.; Rodgers, R.F. The effects of brief diet and anti-diet social media videos on body image and eating concerns among young women. Eat. Behav. 2023, 51, 101811. [Google Scholar] [CrossRef]
- Perrin, A. Social Media Usage: 2005–2015. Pew Research Center 2015. Available online: https://www.pewinternet.org/2015/10/08/2015/Social-Networking-Usage-2005-2015/ (accessed on 11 December 2023).
- Hynnä, K.; Kyrölä, K. “Feel in your body”: Fat activist affects in blogs. Soc. Media Soc. 2019, 5, 2056305119879983. [Google Scholar] [CrossRef]
- Warren, C.S.; Akoury, L.M. Emphasizing the “cultural” in sociocultural: A systematic review of research on thin-ideal internalization, acculturation, and eating pathology in US ethnic minorities. Psychol. Res. Behav. Manag. 2020, 13, 319–330. [Google Scholar] [CrossRef] [PubMed]
- Coffino, J.A.; Udo, T.; Grilo, C.M. Rates of help-seeking in US adults with lifetime DSM-5 eating disorders: Prevalence across diagnoses and differences by sex and ethnicity/race. Mayo Clin. Proc. 2019, 94, 1415–1426. [Google Scholar] [CrossRef] [PubMed]
- Silverman, J.J.; Galanter, M.; Jackson-Triche, M.; Jacobs, D.G.; Lomax, J.W.; Riba, M.B.; Tong, L.D.; Watkins, K.E.; Fochtmann, L.J.; Rhoads, R.S. The American Psychiatric Association practice guidelines for the psychiatric evaluation of adults. Am. J. Psychiatry 2015, 172, 798–802. [Google Scholar] [CrossRef] [PubMed]
- Johansson, R.; Nyblom, A.; Carlbring, P.; Cuijpers, P.; Andersson, G. Choosing between Internet-based psychodynamic versus cognitive behavioral therapy for depression: A pilot preference study. BMC Psychiatry 2013, 13, 268. [Google Scholar] [CrossRef]
- Renfrew, M.E.; Morton, D.P.; Morton, J.K.; Hinze, J.S.; Przybylko, G.; Craig, B.A. The influence of three modes of human support on attrition and adherence to a Web-and mobile app–based mental health promotion intervention in a nonclinical cohort: Randomized comparative study. J. Med. Internet Res. 2020, 22, e19945. [Google Scholar] [CrossRef]
- Linardon, J.; Shatte, A.; Messer, M.; McClure, Z.; Fuller-Tyszkiewicz, M. Effects of participant’s choice of different digital interventions on outcomes for binge-spectrum eating disorders: A pilot doubly randomized preference trial. Behav. Ther. 2023, 54, 303–314. [Google Scholar] [CrossRef]
- Barakat, S.; Maguire, S.; Smith, K.E.; Mason, T.B.; Crosby, R.D.; Touyz, S. Evaluating the role of digital intervention design in treatment outcomes and adherence to eTherapy programs for eating disorders: A systematic review and meta-analysis. Int. J. Eat. Disord. 2019, 52, 1077–1094. [Google Scholar] [CrossRef]
- Karekla, M.; Nikolaou, P.; Merwin, R.M. Randomized clinical trial evaluating AcceptME—A digital gamified acceptance and commitment early intervention program for individuals at high risk for eating disorders. J. Clin. Med. 2022, 11, 1775. [Google Scholar] [CrossRef]
- McClure, Z.; Fuller-Tyszkiewicz, M.; Messer, M.; Linardon, J. Predictors, mediators, and moderators of response to digital interventions for eating disorders: A systematic review. Int. J. Eat. Disord. 2023. [Google Scholar] [CrossRef]
- Forbush, K.T.; Wildes, J.E.; Hunt, T.K. Gender norms, psychometric properties, and validity for the Eating Pathology Symptoms Inventory. Int. J. Eat. Disord. 2014, 47, 85–91. [Google Scholar] [CrossRef] [PubMed]
| Groups—No. (%) or Mean (SD) | |||
|---|---|---|---|
| Categories | Diet Culture | Wellness Resource | Overall |
| (n = 201) | (n = 196) | (N = 397) | |
| Age | 30.77 (13.78) | 34.21 (17.24) | 32.47(15.66) |
| Gender | |||
| Cisgender woman | 199 (99.0%) | 192 (98.0%) | 391 (98.5%) |
| Transgender woman | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) |
| Nonbinary | 2 (1.0%) | 4 (2.0%) | 6 (1.5%) |
| Ethnicity | |||
| American Indian or Alaskan Native | 0 (0.0%) | 1 (0.5%) | 1 (0.4%) |
| Asian or Pacific Islander (includes Asian American) | 17 (8.5%) | 11 (5.6%) | 28 (7.1%) |
| Black, not of Hispanic origin (includes African American) | 27 (13.4%) | 30 (15.3%) | 57 (14.4%) |
| Hispanic | 12 (6.0%) | 17 (8.7%) | 29 (7.3%) |
| Biracial, multiple broad categories | 15 (7.5%) | 4 (2.0%) | 19 (4.8%) |
| White, not of Hispanic origin (includes Caucasian, European American, Middle Eastern) | 130 (64.7%) | 130 (66.3%) | 260 (65.5%) |
| Not listed | 0 (0.0%) | 3 (1.5%) | 3 (0.8%) |
| Body mass index | 27.18 (8.53) | 27.90 (8.94) | 27.53(8.73) |
| Sexual orientation | |||
| Lesbian or gay | 11 (5.5%) | 6 (3.1%) | 17 (4.3%) |
| Straight/Heterosexual | 145 (72.1%) | 158 (80.6%) | 303 (76.3%) |
| Bisexual | 35 (17.4%) | 27 (13.8%) | 62 (15.6%) |
| Don’t know | 6 (3.0%) | 1 (0.5%) | 7 (1.8%) |
| Other | 2 (1.0%) | 3 (1.5%) | 5 (1.3%) |
| Prefer not to disclose | 2 (1.0%) | 1 (0.5%) | 3 (0.8%) |
| Student status | |||
| Undergraduate student | 90 (44.8%) | 100 (51.0%) | 190 (47.9%) |
| Graduate student | 19 (9.5%) | 8 (4.1%) | 27 (6.8%) |
| Not a student | 92 (45.8%) | 88 (44.9%) | 180 (45.3%) |
| Groups—Mean (SD) | |||
|---|---|---|---|
| Categories | Diet Culture | Wellness Resource | Overall |
| (n = 201) | (n = 196) | (N = 397) | |
| Eating Disorder Pathology | |||
| SEDS | 2.68 (1.43) | 2.50 (1.41) | 2.59 (1.42) |
| TREI | 4.32 (1.59) | 4.26 (1.58) | 4.29 (1.58) |
| TREI Restriction | 3.92 (1.69) | 4.00 (1.61) | 3.96 (1.65) |
| EFQ Fear of Weight Gain | 5.55 (1.77) | 5.33 (1.86) | 5.44 (1.81) |
| Body Image | |||
| TIQ Body Dissatisfaction | 3.58 (0.91) | 3.45 (0.93) | 3.52 (0.92) |
| TIQ Body Ideal | 3.46 (0.88) | 3.48 (0.89) | 3.47 (0.89) |
| Female Body Scale | −1.76 (1.52) | −1.75 (1.62) | −1.75 (1.57) |
| FFBS | −0.48 (1.81) | −0.50 (1.95) | −0.49 (1.88) |
| FFBS Ideal Muscularity | 3.89 (1.31) | 4.03 (1.49) | 3.96 (1.41) |
| Body Appreciation Scale-2 | 2.91 (0.94) | 2.92 (0.95) | 2.92 (0.94) |
| Weight Stigma Concerns | |||
| Weight Stigma Concerns Scale a | 4.60 (3.40) | 4.20 (3.20) | 4.60 (3.35) |
| Fat Acceptance | |||
| Fat Acceptance Scale | 4.71 (0.62) | 4.47 (0.67) | 4.59 (0.66) |
| Instrument | t(ꭓ2) | df | p | Benjamini–Hochberg Critical p-Value | Cohen’s d |
|---|---|---|---|---|---|
| Fat Acceptance Scale | 3.56 | 362 | <0.001 * | 0.003 | 0.37 |
| Age | −2.20 | 372.61 | 0.029 | 0.006 | −0.22 |
| Ethnicity a | (12.19) | -- | 0.038 | 0.009 | -- |
| Student Status | (5.04) | 2 | 0.081 | 0.012 | -- |
| TIQ Body Dissatisfaction | 1.31 | 367 | 0.192 | 0.015 | 0.14 |
| Sexual Orientation a | (7.05) | -- | 0.197 | 0.018 | -- |
| EFQ Fear of Weight Gain | 1.19 | 372 | 0.237 | 0.021 | 0.12 |
| SEDS | 1.14 | 356 | 0.257 | 0.024 | 0.12 |
| Weight Stigma Concerns Scale b | 32,611.50 | -- | 0.268 | 0.026 | −0.06 c |
| FFBS Ideal Muscularity | −0.93 | 356 | 0.351 | 0.029 | −0.10 |
| Body Mass Index | −0.82 | 392 | 0.411 | 0.032 | −0.08 |
| TREI Restriction | −0.49 | 372 | 0.622 | 0.035 | −0.05 |
| TREI | 0.35 | 372 | 0.728 | 0.038 | 0.04 |
| TIQ Ideal Body | −0.13 | 367 | 0.895 | 0.041 | −0.01 |
| FFBS | 0.11 | 356 | 0.912 | 0.044 | 0.01 |
| Female Body Scale | −0.10 | 356 | 0.920 | 0.047 | −0.01 |
| Body Appreciation Scale-2 | −0.03 | 372 | 0.977 | 0.050 | −0.00 |
| Instrument | t(ꭓ2) | df | p | Benjamini–Hochberg Critical p-Value | Cohen’s d |
|---|---|---|---|---|---|
| Student Status | (260.36) | 2 | <0.001 * | 0.003 | -- |
| Age | 15.68 | 388.97 | <0.001 * | 0.006 | 1.48 |
| Female Body Scale | −5.93 | 356 | <0.001 * | 0.009 | −0.64 |
| TREI Restriction | 5.26 | 372 | <0.001 * | 0.012 | 0.55 |
| Body Mass Index | 5.22 | 371.84 | <0.001 * | 0.015 | 0.49 |
| FFBS | −5.40 | 352.02 | <0.001 * | 0.018 | −0.55 |
| TIQ Body Dissatisfaction | 4.94 | 367 | <0.001 * | 0.021 | 0.52 |
| EFQ Fear of Weight Gain | 4.96 | 276.37 | <0.001 * | 0.024 | 0.54 |
| Weight Stigma Concerns Scale b | 24,006.00 | -- | <0.001 * | 0.026 | −0.25 c |
| TREI | 4.79 | 298.33 | <0.001 * | 0.029 | 0.52 |
| SEDS | 3.89 | 283.32 | <0.001 * | 0.032 | 0.43 |
| Body Appreciation Scale-2 | −3.30 | 372 | 0.001 * | 0.035 | −0.35 |
| Ethnicity a | (17.97) | -- | 0.003 * | 0.038 | -- |
| TIQ Ideal Body | 2.94 | 367 | 0.004 * | 0.041 | 0.31 |
| FFBS Ideal Muscularity | 1.07 | 356 | 0.286 | 0.044 | 0.12 |
| Sexual Orientation a | (4.49) | -- | 0.488 | 0.047 | -- |
| Fat Acceptance Scale | −0.50 | 362 | 0.618 | 0.050 | −0.05 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fitterman-Harris, H.F.; Davis, G.G.; Bedard, S.P.; Cusack, C.E.; Levinson, C.A. Digital Mental Health Interventions: Differences in Diet Culture Intervention Framing. Int. J. Environ. Res. Public Health 2024, 21, 24. https://doi.org/10.3390/ijerph21010024
Fitterman-Harris HF, Davis GG, Bedard SP, Cusack CE, Levinson CA. Digital Mental Health Interventions: Differences in Diet Culture Intervention Framing. International Journal of Environmental Research and Public Health. 2024; 21(1):24. https://doi.org/10.3390/ijerph21010024
Chicago/Turabian StyleFitterman-Harris, Hannah F., Gabrielle G. Davis, Samantha P. Bedard, Claire E. Cusack, and Cheri A. Levinson. 2024. "Digital Mental Health Interventions: Differences in Diet Culture Intervention Framing" International Journal of Environmental Research and Public Health 21, no. 1: 24. https://doi.org/10.3390/ijerph21010024
APA StyleFitterman-Harris, H. F., Davis, G. G., Bedard, S. P., Cusack, C. E., & Levinson, C. A. (2024). Digital Mental Health Interventions: Differences in Diet Culture Intervention Framing. International Journal of Environmental Research and Public Health, 21(1), 24. https://doi.org/10.3390/ijerph21010024






