From Health-in-All-Policies to Climate-in-All-Policies: Using the Synergies between Health Promotion and Climate Protection to Take Action
Abstract
1. Introduction
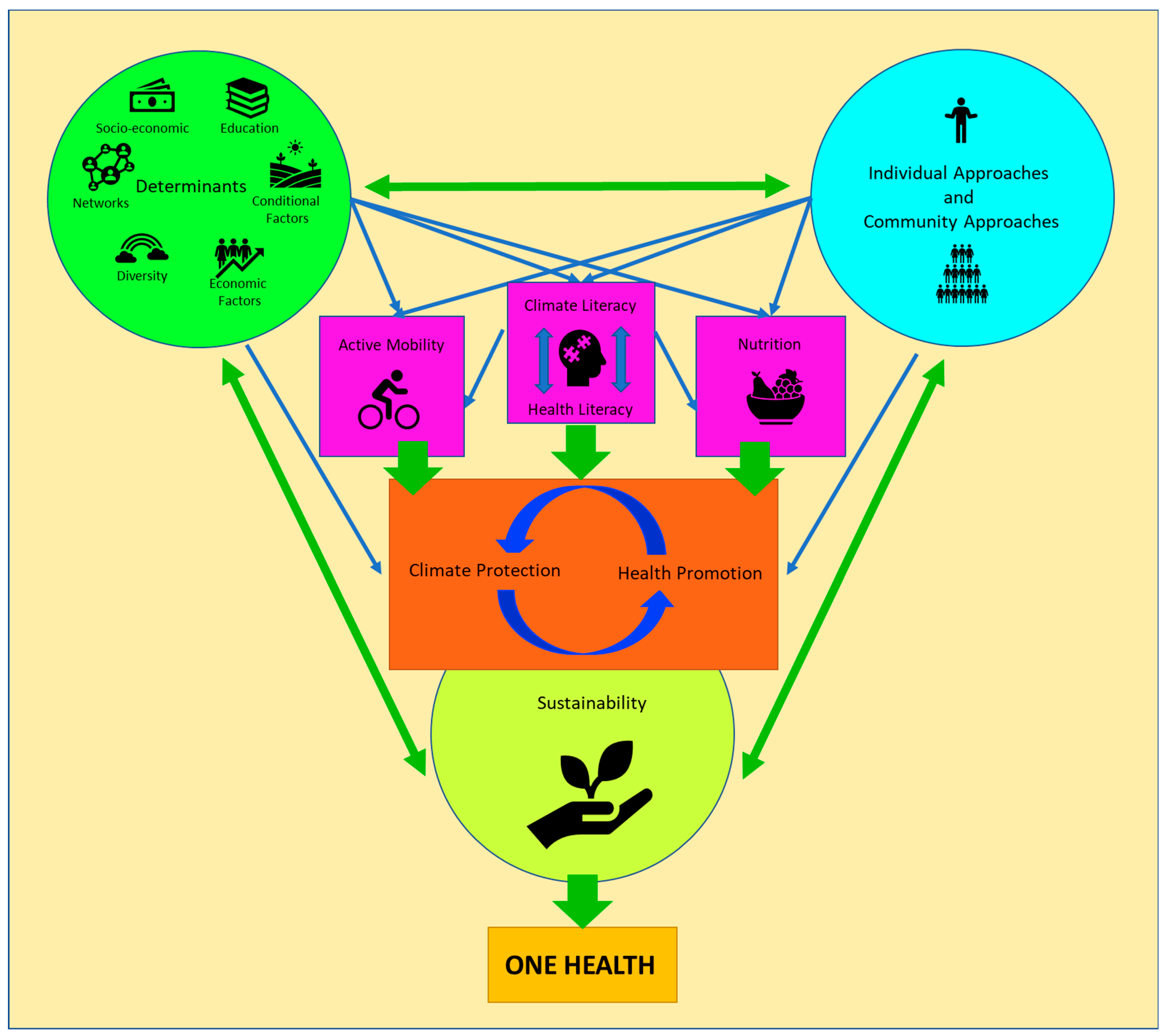
2. The Relationship between Health Promotion and Climate Protection
3. Breaking Down the Complexity—Three Principles to Protect the Climate and Promote Health
- (1)
- Sustainability
- (2)
- Focus on determinants
- (3)
- Individual as well as community approaches
4. Examples for Common Domains of Health Promotion and Climate Protection
- (1)
- Literacy
- (2)
- Physical activity
- (3)
- Nutrition and dietary habits
5. From Policy to Practice
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. COP26 Special Report on Climate Change and Health: The Health Argument for Climate Action; World Health Organization: Geneva, Switzerland, 2021. [Google Scholar]
- Prüss-Ustün, A.; Wolf, J.; Corvalán, C.; Bos, R.; Neira, M. Preventing Disease through Healthy Environments: A Global Assessment of the Burden of Disease from Environmental Risks; World Health Organization: Geneva, Switzerland, 2016; Available online: https://www.who.int/publications/i/item/9789241565196 (accessed on 25 September 2023).
- World Health Organization. Geneva Charter for Well-Being; World Health Organization: Geneva, Switzerland, 2021; Available online: https://www.who.int/publications/m/item/the-geneva-charter-for-well-being (accessed on 25 September 2023).
- Romanello, M.; Di Napoli, C.; Drummond, P.; Green, C.; Kennard, H.; Lampard, P.; Scamman, D.; Arnell, N.; Ayeb-Karlsson, S.; Ford, L.B.; et al. The 2022 report of the Lancet Countdown on health and climate change: Health at the mercy of fossil fuels. Lancet 2021, 397, 129–170. [Google Scholar]
- United Nations. Transforming our World: The 2030 Agenda for Sustainable Development; United Nations: New York, NY, USA, 2015; Available online: https://sdgs.un.org/publications/transforming-our-world-2030-agenda-sustainable-development-17981 (accessed on 25 September 2023).
- World Health Organization. Fast Facts on Climate Change and Health; World Health Organization: Geneva, Switzerland, 2021; Available online: https://www.who.int/publications/m/item/fast-facts-on-climate-change-and-health (accessed on 25 September 2023).
- Whitmee, S.; Haines, A.; Beyrer, C.; Boltz, F.; Capon, A.G.; de Souza Dias, B.F.; Ezeh, A.; Frumkin, H.; Gong, P.; Head, P.; et al. Safeguarding human health in the Anthropocene epoch: Report of The Rockefeller Foundation–Lancet Commission on planetary health. Lancet 2015, 386, 1973–2028. [Google Scholar]
- International Labour Organization. Working on a Warmer Planet. The Impact of Heat Stress on Labour Productivity and Decent Work; World Health Organization: Geneva, Switzerland, 2019; Available online: https://www.ilo.org/wcmsp5/groups/public/---dgreports/---dcomm/---publ/documents/publication/wcms_711919.pdf (accessed on 25 September 2023).
- World Health Organization. Achieving Well-Being. A Global Framework for Integrating Well-Being into Public Health Utilizing a Health Promotion Approach; World Health Organization: Geneva, Switzerland, 2023; Available online: https://www.who.int/publications/m/item/wha-76---achieving-well-being--a-global-framework-for-integrating-well-being-into-public-health-utilizing-a-health-promotion-approach (accessed on 25 September 2023).
- World Health Organization. The Ottawa Charter for Health Promotion; World Health Organization: Geneva, Switzerland, 1987; Available online: https://www.who.int/publications/i/item/WH-1987 (accessed on 25 September 2023).
- Patz, J.A.; Campbell-Lendrum, D.; Holloway, T.; Foley, J.A. Impact of regional climate change on human health. Nature 2005, 438, 310–317. [Google Scholar] [CrossRef] [PubMed]
- Mailloux, N.A.; Henegan, C.P.; Lsoto, D.; Patterson, K.P.; West, P.C.; Foley, J.A.; Patz, J.A. Climate Solutions Double as Health Interventions. Int. J. Environ. Res. Public Health 2021, 18, 13339. [Google Scholar] [CrossRef]
- World Health Organization. WHO Global Strategy on Health, Environment and Climate Change: The Transformation Needed to Improve Lives and Well-Being Sustainably through Healthy Environments; World Health Organization: Geneva, Switzerland, 2020; Available online: https://www.who.int/publications/i/item/9789240000377 (accessed on 20 December 2023).
- Lee, I.M.; Shiroma, E.J.; Lobelo, F.; Puska, P.; Blair, S.N.; Katzmarzyk, P.T.; Lancet Physical Activity Series Working Group. Effect of physical inactivity on major non-communicable diseases worldwide: An analysis of burden of disease and life expectancy. Lancet 2012, 380, 219–229. [Google Scholar] [CrossRef] [PubMed]
- Kardan, O.; Gozdyra, P.; Misic, B.; Moola, F.; Palmer, L.J.; Paus, T.; Berman, M.G. Neighborhood greenspace and health in a large urban center. Sci. Rep. 2015, 5, 11610. [Google Scholar] [PubMed]
- Gascon, M.; Triguero-Mas, M.; Martínez, D.; Dadvand, P.; Rojas-Rueda, D.; Plasència, A.; Nieuwenhuijsen, M.J. Residential green spaces and mortality: A systematic review. Environ. Int. 2016, 86, 60–67. [Google Scholar] [PubMed]
- Springmann, M.; Godfray, H.C.; Rayner, M.; Scarborough, P. Analysis and valuation of the health and climate change cobenefits of dietary change. Proc. Natl. Acad. Sci. USA 2016, 113, 4146–4151. [Google Scholar] [PubMed]
- Borowy, I. Defining Sustainable Development: The World Commission on Environment and Development (Brundtland Commission); Routledge: London, UK, 2013. [Google Scholar]
- Moore, J.E.; Mascarenhas, A.; Bain, J.; Straus, S.E. Developing a comprehensive definition of sustainability. Implement. Sci. 2017, 12, 110. [Google Scholar] [CrossRef] [PubMed]
- Bodkin, A.; Hakimi, S. Sustainable by design: A systematic review of factors for health promotion program sustainability. BMC Public Health 2020, 20, 964. [Google Scholar] [CrossRef] [PubMed]
- Prochaska, J.O.; DiClemente, C.C. Transtheoretical therapy: Toward a more integrative model of change. Psychother. Theory Res. Pract. 1982, 19, 276–288. [Google Scholar] [CrossRef]
- Dahlgren, G.; Whitehead, M. Policies and Strategies to Promote Social Equity in Health; Institute for Futures Studies: Stockholm, Sweden, 1991. [Google Scholar]
- Gnadinger, T. Health Policy Brief: The Relative Contribution of Multiple Determinants to Health Outcomes; Health Affairs Blog: 2014. Available online: https://www.healthaffairs.org/do/10.1377/hblog20140822.040952/full/ (accessed on 25 September 2023).
- Hood, C.M.; Gennuso, K.P.; Swain, G.R.; Catlin, B.B. County health rankings: Relationships between determinant factors and health outcomes. Am. J. Prev. Med. 2016, 50, 129–135. [Google Scholar] [CrossRef]
- Marmot, M.; Allen, J.; Bell, R.; Bloomer, E.; Goldblatt, P. Consortium for the European Review of Social Determinants of Health and the Health Divide. WHO European review of social determinants of health and the health divide. Lancet 2012, 380, 1011–1029. [Google Scholar] [CrossRef] [PubMed]
- Wolf, J.; Adger, W.N.; Lorenzoni, I.; Abrahamson, V.; Raine, R. Social capital, individual responses to heat waves and climate change adaptation: An empirical study of two UK cities. Glob. Environ. Change 2010, 20, 44–52. [Google Scholar]
- Belay, D.; Fekadu, G. Influence of social capital in adopting climate change adaptation strategies: Empirical evidence from rural areas of Ambo district in Ethiopia. Clim. Dev. 2021, 13, 857–868. [Google Scholar] [CrossRef]
- Saptutyningsih, E.; Diswandi, D.; Jaung, W. Does social capital matter in climate change adaptation? A lesson from agricultural sector in Yogyakarta, Indonesia. Land Use Policy 2020, 95, 104189. [Google Scholar]
- World Health Organization. The Shanghai Declaration on Promoting Health in the 2030 Agenda for Sustainable Development. In Proceedings of the Ninth Global Conference on Health Promotion, Shanghai, China, 21–24 November 2016; World Health Organization: Geneva, Switzerland, 2016. Available online: https://www.who.int/publications/i/item/WHO-NMH-PND-17.5 (accessed on 25 September 2023).
- Ferrer, L. Engaging Patients, Carers and Communities for the Provision of Coordinated/Integrated Health Services: Strategies and Tools; WHO Regional Office for Europe: Copenhagen, Denmark, 2015. [Google Scholar]
- Stein, K.V.; Amelung, V.E. Refocussing Care—What Does People-Centredness Mean? In Handbook Integrated Care; Amelung, V.E., Stein, K.V., Suter, E., Goodwin, N., Nolte, E., Balicer, R., Eds.; Springer Nature: Berlin/Heidelberg, Germany, 2021. [Google Scholar]
- World Health Organization. Framework on Integrated, People-Centred Health Services. In Report by the Secretariat, 69th World Health Assembly; World Health Organization: Geneva, Switzerland, 2016. [Google Scholar]
- van Ede, A.; Minderhout, R.; Stein, K.V.; Bruijnzeels, M. How to implement Population Health Management: A scoping review. BMC Health Serv. Res. 2023, 23, 910. [Google Scholar]
- Steenkamer, B.M.; Drewes, H.W.; Heijink, R.; Baan, C.A.; Struijs, J.N. Defining Population Health Management: A Scoping Review of the Literature. Popul. Health Manag. 2017, 20, 74–85. [Google Scholar] [CrossRef] [PubMed]
- Chastonay, P.; Zybach, U.; Simos, J.; Mattig, T. Climate change: An opportunity for health promotion practitioners? Int. J. Public Health 2015, 60, 763–764. [Google Scholar] [CrossRef]
- OECD. Adult Health Literacy. Available online: https://www.oecd.org/education/innovation-education/adultliteracy.htm (accessed on 25 September 2023).
- Nutbeam, D.; Muscat, D.M. Health Promotion Glossary 2021. Health Promot. Int. 2021, 36, 1578–1598. [Google Scholar] [CrossRef] [PubMed]
- Nutbeam, D.; Lloyd, J.E. Understanding and Responding to Health Literacy as a Social Determinant of Health. Annu. Rev. Public Health 2021, 42, 159–173. [Google Scholar] [CrossRef] [PubMed]
- Nutbeam, D.; McGill, B.; Premkumar, P. Improving health literacy in community populations: A review of progress. Health Promot. Int. 2018, 33, 901–911. [Google Scholar] [CrossRef] [PubMed]
- U.S. Global Change Research Program. Climate Literacy: The Essential Principles of Climate Science; U.S. Global Change Research Program: Washington, DC, USA, 2009. Available online: https://downloads.globalchange.gov/Literacy/climate_literacy_highres_english.pdf (accessed on 25 September 2023).
- Antonovsky, A. Unraveling The Mystery of Health—How People Manage Stress and Stay Well; Jossey-Bass Publishers: San Francisco, CA, USA, 1987. [Google Scholar]
- Frumkin, H.; Hess, J.; Luber, G.; Malilay, J.; McGeehin, M. Climate Change: The Public Health Response. Am. J. Public Health 2008, 98, 435–445. [Google Scholar]
- Limaye, V.S.; Grabow, M.L.; Stull, V.J.; Patz, J.A. Developing A Definition Of Climate And Health Literacy: Study seeks to develop a definition of climate and health literacy. Health Aff. 2020, 39, 2182–2188. [Google Scholar]
- U.S. Department of health and Human Services. 2018 Physical Activity Guidelines Advisory Committee. 2018 Physical Activity Guidelines Advisory Committee Scientific Report. Available online: https://health.gov/sites/default/files/2019-09/PAG_Advisory_Committee_Report.pdf (accessed on 25 September 2023).
- Leyk, D. Health Risks and Interventions in Exertional Heat Stress. Dtsch. Arztebl. Int. 2019, 116, 537–544. [Google Scholar] [PubMed]
- Gardner, J.W.; Kark, J.A.; Karnei, K.; Sanborn, J.S.; Gastaldo, E.; Burr, P.; Wenger, C.B. Risk factors predicting exertional heat illness in male Marine Corps recruits. Med. Sci. Sports Exerc. 1996, 28, 939–944. [Google Scholar]
- Reis, C.; Lopes, A. Evaluating the Cooling Potential of Urban Green Spaces to Tackle Urban Climate Change in Lisbon. Sustainability 2019, 11, 2480. [Google Scholar] [CrossRef]
- Dorner, T.E.; Haider, S.; Lackinger, C.; Kapan, A.; Titze, S. Determinants of Exercise, Fulfilling the Recommendations for Aerobic Physical Activity and Health Status: Results of a Correlation Study in the Federal States of Austria. Gesundheitswesen 2020, 82, S207–S216. [Google Scholar]
- Obradovich, N.; Fowler, J.H. Climate change may alter human physical activity patterns. Nat. Hum. Behav. 2017, 1, 97. [Google Scholar] [CrossRef]
- Frühauf, A.; Niedermeier, M.; Kopp, M. Intention to Engage in Winter Sport in Climate Change Affected Environments. Front. Public Health 2020, 8, 598297. [Google Scholar] [CrossRef] [PubMed]
- Abu-Omar, K.; Gelius, P.; Messing, S. Physical activity promotion in the age of climate change. F1000Research 2020, 9, 349. [Google Scholar]
- Tilman, D.; Clark, M. Global diets link environmental sustainability and human health. Nature 2014, 515, 518–522. [Google Scholar] [PubMed]
- Poore, J.; Nemecek, T. Reducing food’s environmental impacts through producers and consumers. Science 2018, 360, 987–992. [Google Scholar] [CrossRef]
- Hayek, M.N.; Harwatt, H.; Ripple, W.J.; Mueller, N.D. The carbon opportunity cost of animal-sourced food production on land. Nat. Sustain. 2021, 4, 21–24. [Google Scholar] [CrossRef]
- FAO. One Health. Available online: https://www.fao.org/one-health/en (accessed on 25 September 2023).
- Wallace, T.C.; Bailey, R.L.; Blumberg, J.B.; Burton-Freeman, B.; Chen, C.O.; Crowe-White, K.M.; Drewnowski, A.; Hooshmand, S.; Johnson, E.; Lewis, R.; et al. Fruits, vegetables, and health: A comprehensive narrative, umbrella review of the science and recommendations for enhanced public policy to improve intake. Crit. Rev. Food Sci. Nutr. 2020, 60, 2174–2211. [Google Scholar]
- Angelino, D.; Godos, J.; Ghelfi, F.; Tieri, M.; Titta, L.; Lafranconi, A.; Marventano, S.; Alonzo, E.; Gambera, A.; Sciacca, S.; et al. Fruit and vegetable consumption and health outcomes: An umbrella review of observational studies. Int. J. Food Sci. Nutr. 2019, 70, 652–667. [Google Scholar] [CrossRef] [PubMed]
- Fanzo, J.; Rudie, C.; Sigman, I.; Grinspoon, S.; Benton, T.G.; Brown, M.E.; Covic, N.; Fitch, K.; Golden, C.D.; Grace, D.; et al. Sustainable food systems and nutrition in the 21st century: A report from the 22nd annual Harvard Nutrition Obesity Symposium. Am. J. Clin. Nutr. 2022, 115, 18–33. [Google Scholar] [CrossRef]
- Vermeulen, S.J.; Campbell, B.M.; Ingram, J.S.I. Climate Change and Food Systems. Annu. Rev. Environ. Resour. 2012, 37, 195–222. [Google Scholar]
- Duchin, F. Sustainable Consumption of Food: A Framework for Analyzing Scenarios about Changes in Diets. J. Ind. Ecol. 2008, 9, 99–114. [Google Scholar] [CrossRef]
- Stehfest, E. Food choices for health and planet. Nature 2014, 515, 501–502. [Google Scholar] [CrossRef]
- Salm, L.; Nisbett, N.; Cramer, L.; Gillespie, S.; Thornton, P. How climate change interacts with inequity to affect nutrition. WIREs Clim. Chang. 2021, 12, e696. [Google Scholar]
- Binns, C.W.; Lee, M.K.; Maycock, B.; Torheim, L.E.; Nanishi, K.; Duong, D.T.T. Climate Change, Food Supply, and Dietary Guidelines. Annu. Rev. Public Health 2021, 42, 233–255. [Google Scholar] [CrossRef] [PubMed]

| SEM 1 | SDG 2 |
|---|---|
| Environmental conditions | Affordable and clean energy (7), sustainable cities and communities (11), climate action (13), life below water (14), and life on land (15) |
| Agriculture and food production | Zero hunger (2) and responsible consumption and production (12) |
| Education | Quality education (4) |
| Work environment | Decent work and economic growth (8) |
| Unemployment | No poverty (1) |
| Water and sanitation | Clean water and sanitation (6) |
| Health care services | Good health and well-being (3) |
| Social and community networks | Social and community networks |
| Sex | Gender equality (5) |
| Conditional factors | Industry innovation and infrastructure (9), reduced inequalities (10), and peace, justice, and strong institutions (16) |
| Sustainability | Determinants | Individual and Community Approaches | |
|---|---|---|---|
| Literacy | Adaptation of the dimensions of the sense of coherence, as a prerequisite for salutogenesis (comprehensibility, manageability, and meaningfulness) can also be seen as a prerequisite for sustainability in the genesis of climate protection. | Social determinants, especially education, play a key part in the levels of health and climate literacy. Easy access to evidence-based information in lay language is another important determinant. Facilitating these levers through active policies in education and health and climate promotion can mitigate negative impact of determinants. | Address individuals, patients, health professionals, and society as a whole to increase health literacy and climate literacy. Furthermore, the people, patients and public must be seen as important and equal partners for health promotion and climate protection. Including comprehensive education on health and climate from kindergarten, continuing to geriatric care, would establish a baseline understanding across society. |
| Physical activity | Bottom-up instead of top-down approaches and orientation on individual stages of change can promote a change in physical activity behaviour towards sustainable, active mobility. | The orientation of policies and strategies towards social, economic, cultural, individual, and health- and fitness-related determinants is an important prerequisite for the promotion of active mobility. | Encourage individuals towards physically active transportation as alternative for daily distances and create the conditions for it like green spaces and a traffic system which is safe and inviting for physically active transportation. |
| Nutrition and dietary habits | A sustainable change and maintenance of healthy eating habits is very difficult for many people. The best results can be achieved by considering all established pillars of health promotion (empowerment, participation, orientation towards determinants, personal needs and believes, and stages of change, etc.). | Social, economic, individual, and cultural determinants of eating habits must be taken into account for a healthy and climate-friendly change in diet. | Develop sustainable nutrition guidelines for healthy nutrition with focus on local, organic, and plant-based food and communicate them to individuals, stakeholders, and the public. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stein, K.V.; Dorner, T.E. From Health-in-All-Policies to Climate-in-All-Policies: Using the Synergies between Health Promotion and Climate Protection to Take Action. Int. J. Environ. Res. Public Health 2024, 21, 110. https://doi.org/10.3390/ijerph21010110
Stein KV, Dorner TE. From Health-in-All-Policies to Climate-in-All-Policies: Using the Synergies between Health Promotion and Climate Protection to Take Action. International Journal of Environmental Research and Public Health. 2024; 21(1):110. https://doi.org/10.3390/ijerph21010110
Chicago/Turabian StyleStein, K. Viktoria, and Thomas E. Dorner. 2024. "From Health-in-All-Policies to Climate-in-All-Policies: Using the Synergies between Health Promotion and Climate Protection to Take Action" International Journal of Environmental Research and Public Health 21, no. 1: 110. https://doi.org/10.3390/ijerph21010110
APA StyleStein, K. V., & Dorner, T. E. (2024). From Health-in-All-Policies to Climate-in-All-Policies: Using the Synergies between Health Promotion and Climate Protection to Take Action. International Journal of Environmental Research and Public Health, 21(1), 110. https://doi.org/10.3390/ijerph21010110







