Effect of High-Intensity Interval Training vs. Moderate-Intensity Continuous Training on Fat Loss and Cardiorespiratory Fitness in the Young and Middle-Aged a Systematic Review and Meta-Analysis
Abstract
1. Introduction
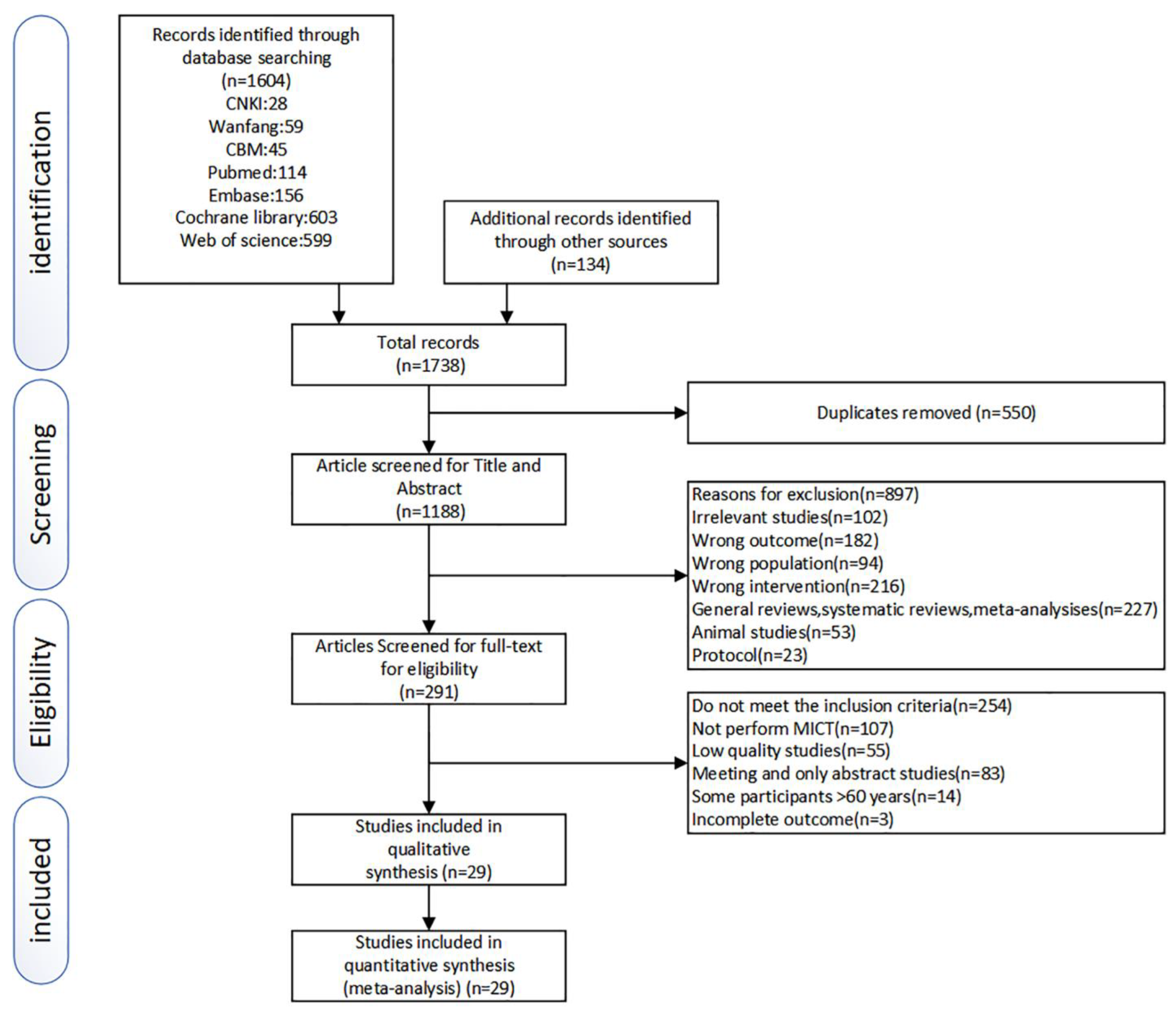
2. Materials and Methods
2.1. Literature Search Strategy
2.2. Inclusion and Exclusion Criteria
- Participants
- Intervention
- Comparison
- Outcomes
- Study
2.3. Data Extraction
2.4. Study Quality Assessment
2.5. Statistical Analysis
3. Results
3.1. This Included Studies
3.2. Participant and Intervention Characteristics
3.3. Outcome Assessment
3.4. Quality Assessment
3.5. Meta-Analysis
3.6. Subgroup Analysis
3.7. Sensitivity Analysis and Publication Bias
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Seidell, J.C.; Halberstadt, J. The Global Burden of Obesity and the Challenges of Prevention. Ann. Nutr. Metab. 2015, 66 (Suppl. S2), 7–12. [Google Scholar] [CrossRef] [PubMed]
- GBD 2015 Obesity Collaborators; Afshin, A.; Forouzanfar, M.H.; Reitsma, M.B.; Sur, P.; Estep, K.; Lee, A.; Marczak, L.; Mokdad, A.H.; Moradi-Lakeh, M.; et al. Health Effects of Overweight and Obesity in 195 Countries over 25 Years. N. Engl. J. Med. 2017, 377, 13–27. [Google Scholar] [CrossRef] [PubMed]
- Heymsfield, S.B.; Wadden, T.A. Mechanisms, Pathophysiology, and Management of Obesity. N. Engl. J. Med. 2017, 376, 254–266. [Google Scholar] [CrossRef] [PubMed]
- Stefan, N.; Häring, H.-U.; Hu, F.B.; Schulze, M.B. Metabolically healthy obesity: Epidemiology, mechanisms, and clinical implications. Lancet Diabetes Endocrinol. 2013, 1, 152–162. [Google Scholar] [CrossRef]
- Berkowitz, R.I.; Fabricatore, A.N. Obesity, Psychiatric Status, and Psychiatric Medications. Psychiatr. Clin. N. Am. 2011, 34, 747–764. [Google Scholar] [CrossRef]
- Phelan, S.M.; Burgess, D.J.; Yeazel, M.W.; Hellerstedt, W.L.; Griffin, J.M.; Ryn, M. Impact of weight bias and stigma on quality of care and outcomes for patients with obesity. Obes. Rev. 2015, 16, 319–326. [Google Scholar] [CrossRef]
- Brown, R.E.; Kuk, J.L. Consequences of obesity and weight loss: A devil’s advocate position. Obes. Rev. 2015, 16, 77–87. [Google Scholar] [CrossRef]
- Chao, A.M.; Quigley, K.M.; Wadden, T.A. Dietary interventions for obesity: Clinical and mechanistic findings. J. Clin. Investig. 2021, 131, 140065. [Google Scholar] [CrossRef]
- Wadden, T.A.; Tronieri, J.S.; Butryn, M.L. Lifestyle modification approaches for the treatment of obesity in adults. Am. Psychol. 2020, 75, 235–251. [Google Scholar] [CrossRef]
- Swift, D.L.; McGee, J.E.; Earnest, C.P.; Carlisle, E.; Nygard, M.; Johannsen, N.M. The Effects of Exercise and Physical Activity on Weight Loss and Maintenance. Prog. Cardiovasc. Dis. 2018, 61, 206–213. [Google Scholar] [CrossRef]
- Smit, C.; De Hoogd, S.; Brüggemann, R.J.; Knibbe, C.A.J. Obesity and drug pharmacology: A review of the influence of obesity on pharmacokinetic and pharmacodynamic parameters. Expert Opin. Drug Metab. Toxicol. 2018, 14, 275–285. [Google Scholar] [CrossRef] [PubMed]
- Jackson, V.M.; Breen, D.M.; Fortin, J.-P.; Liou, A.; Kuzmiski, J.B.; Loomis, A.K.; Rives, M.-L.; Shah, B.; Carpino, P.A. Latest approaches for the treatment of obesity. Expert Opin. Drug Discov. 2015, 10, 825–839. [Google Scholar] [CrossRef] [PubMed]
- Camilleri, M.; Acosta, A. Combination Therapies for Obesity. Metab. Syndr. Relat. Disord. 2018, 16, 390–394. [Google Scholar] [CrossRef] [PubMed]
- Hainer, V.; Toplak, H.; Mitrakou, A. Treatment Modalities of Obesity: What fits whom? Diabetes Care 2008, 31 (Suppl. S2), S269–S277. [Google Scholar] [CrossRef]
- Elagizi, A.; Kachur, S.; Carbone, S.; Lavie, C.J.; Blair, S.N. A Review of Obesity, Physical Activity, and Cardiovascular Disease. Curr. Obes. Rep. 2020, 9, 571–581. [Google Scholar] [CrossRef]
- Stiegler, P.; Cunliffe, A. The Role of Diet and Exercise for the Maintenance of Fat-Free Mass and Resting Metabolic Rate During Weight Loss. Sports Med. 2006, 36, 239–262. [Google Scholar] [CrossRef]
- Harber, M.P.; Kaminsky, L.A.; Arena, R.; Blair, S.N.; Franklin, B.A.; Myers, J.; Ross, R. Impact of Cardiorespiratory Fitness on All-Cause and Disease-Specific Mortality: Advances Since 2009. Prog. Cardiovasc. Dis. 2017, 60, 11–20. [Google Scholar] [CrossRef]
- Petridou, A.; Siopi, A.; Mougios, V. Exercise in the management of obesity. Metabolism 2019, 92, 163–169. [Google Scholar] [CrossRef]
- Carbone, S.; Del Buono, M.G.; Ozemek, C.; Lavie, C.J. Obesity, risk of diabetes and role of physical activity, exercise training and cardiorespiratory fitness. Prog. Cardiovasc. Dis. 2019, 62, 327–333. [Google Scholar] [CrossRef]
- Yumuk, V.; Tsigos, C.; Fried, M.; Schindler, K.; Busetto, L.; Micic, D.; Toplak, H. European Guidelines for Obesity Management in Adults. Obes. Facts 2015, 8, 402–424, Erratum in Obes Facts. 2016, 9, 64. [Google Scholar] [CrossRef]
- Schroeder, E.C.; Franke, W.D.; Sharp, R.L.; Lee, D.-C. Comparative effectiveness of aerobic, resistance, and combined training on cardiovascular disease risk factors: A randomized controlled trial. PLoS ONE 2019, 14, e0210292. [Google Scholar] [CrossRef] [PubMed]
- Jeffery, R.W.; Wing, R.R.; Sherwood, N.E.; Tate, D.F. Physical activity and weight loss: Does prescribing higher physical activity goals improve outcome? Am. J. Clin. Nutr. 2003, 78, 684–689. [Google Scholar] [CrossRef] [PubMed]
- Tate, D.F.; Jeffery, R.W.; Sherwood, N.E.; Wing, R.R. Long-term weight losses associated with prescription of higher physical activity goals. Are higher levels of physical activity protective against weight regain? Am. J. Clin. Nutr. 2007, 85, 954–959. [Google Scholar] [CrossRef] [PubMed]
- Štajer, V.; Milovanović, I.M.; Todorović, N.; Ranisavljev, M.; Pišot, S.; Drid, P. Let’s (Tik) Talk About Fitness Trends. Front. Public Health 2022, 10, 899949. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Tong, T.K.; Qiu, W.; Zhang, X.; Zhou, S.; Liu, Y.; He, Y. Comparable Effects of High-Intensity Interval Training and Prolonged Continuous Exercise Training on Abdominal Visceral Fat Reduction in Obese Young Women. J. Diabetes Res. 2017, 2017, 5071740. [Google Scholar] [CrossRef]
- Berge, J.; Hjelmesæth, J.; Hertel, J.K.; Gjevestad, E.; Småstuen, M.C.; Johnson, L.K.; Martins, C.; Andersen, E.; Helgerud, J.; Støren, Ø. Effect of Aerobic Exercise Intensity on Energy Expenditure and Weight Loss in Severe Obesity—A Randomized Controlled Trial. Obesity 2021, 29, 359–369. [Google Scholar] [CrossRef] [PubMed]
- Dias, K.A.; Ingul, C.B.; Tjønna, A.E.; Keating, S.E.; Gomersall, S.R.; Follestad, T.; Hosseini, M.S.; Hollekim-Strand, S.M.; Ro, T.B.; Haram, M.; et al. Effect of High-Intensity Interval Training on Fitness, Fat Mass and Cardiometabolic Biomarkers in Children with Obesity: A Randomised Controlled Trial. Sports Med. 2018, 48, 733–746. [Google Scholar] [CrossRef]
- Guiraud, T.; Nigam, A.; Gremeaux, V.; Meyer, P.; Juneau, M.; Bosquet, L. High-Intensity Interval Training in Cardiac Rehabilitation. Sports Med. 2012, 42, 587–605. [Google Scholar] [CrossRef]
- Morales-Palomo, F.; Ramirez-Jimenez, M.; Ortega, J.F.; Moreno-Cabañas, A.; Mora-Rodriguez, R. Exercise Training Adaptations in Metabolic Syndrome Individuals on Chronic Statin Treatment. J. Clin. Endocrinol. Metab. 2020, 105, dgz304. [Google Scholar] [CrossRef]
- Ryan, B.J.; Schleh, M.W.; Ahn, C.; Ludzki, A.C.; Gillen, J.B.; Varshney, P.; Van Pelt, D.W.; Pitchford, L.M.; Chenevert, T.L.; Gioscia-Ryan, R.A.; et al. Moderate-Intensity Exercise and High-Intensity Interval Training Affect Insulin Sensitivity Similarly in Obese Adults. J. Clin. Endocrinol. Metab. 2020, 105, e2941–e2959. [Google Scholar] [CrossRef]
- de Oliveira, G.H.; Boutouyrie, P.; Simões, C.F.; Locatelli, J.C.; Mendes, V.H.S.; Reck, H.B.; Costa, C.E.; Okawa, R.T.P.; Lopes, W.A. The impact of high-intensity interval training (HIIT) and moderate-intensity continuous training (MICT) on arterial stiffness and blood pressure in young obese women: A randomized controlled trial. Hypertens. Res. 2020, 43, 1315–1318. [Google Scholar] [CrossRef] [PubMed]
- Hood, M.S.; Little, J.P.; Tarnopolsky, M.A.; Myslik, F.; Gibala, M.J. Low-Volume Interval Training Improves Muscle Oxidative Capacity in Sedentary Adults. Med. Sci. Sports Exerc. 2011, 43, 1849–1856. [Google Scholar] [CrossRef] [PubMed]
- Gibala, M.J.; Little, J.P.; Van Essen, M.; Wilkin, G.P.; Burgomaster, K.A.; Safdar, A.; Raha, S.; Tarnopolsky, M.A. Short-term sprint interval versus traditional endurance training: Similar initial adaptations in human skeletal muscle and exercise performance. J. Physiol. 2006, 575, 901–911. [Google Scholar] [CrossRef]
- Jung, M.E.; Bourne, J.E.; Beauchamp, M.R.; Robinson, E.; Little, J.P. High-Intensity Interval Training as an Efficacious Alternative to Moderate-Intensity Continuous Training for Adults with Prediabetes. J. Diabetes Res. 2015, 2015, 191595. [Google Scholar] [CrossRef] [PubMed]
- Hagberg, L.; Lundqvist, S.; Lindholm, L. What is the time cost of exercise? Cost of time spent on exercise in a primary health care intervention to increase physical activity. Cost Eff. Resour. Alloc. 2020, 18, 14–17. [Google Scholar] [CrossRef]
- Shamseer, L.; Moher, D.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: Elaboration and explanation. BMJ 2015, 350, g7647. [Google Scholar] [CrossRef]
- Viana, R.B.; Naves, J.P.A.; Coswig, V.S.; de Lira, C.A.B.; Steele, J.; Fisher, J.P.; Gentil, P. Is interval training the magic bullet for fat loss? A systematic review and meta-analysis comparing moderate-intensity continuous training with high-intensity interval training (HIIT). Br. J. Sports Med. 2019, 53, 655–664. [Google Scholar] [CrossRef]
- Wewege, M.; Van Den Berg, R.; Ward, R.E.; Keech, A. The effects of high-intensity interval training vs. moderate-intensity continuous training on body composition in overweight and obese adults: A systematic review and meta-analysis. Obes. Rev. 2017, 18, 635–646. [Google Scholar] [CrossRef]
- Keating, S.E.; Johnson, N.; Mielke, G.; Coombes, J.S. A systematic review and meta-analysis of interval training versus moderate-intensity continuous training on body adiposity. Obes. Rev. 2017, 18, 943–964. [Google Scholar] [CrossRef]
- Maher, C.G.; Sherrington, C.; Herbert, R.D.; Moseley, A.M.; Elkins, M. Reliability of the PEDro Scale for Rating Quality of Randomized Controlled Trials. Phys. Ther. 2003, 83, 713–721. [Google Scholar] [CrossRef]
- Atan, T.; Karavelioğlu, Y. Effectiveness of High-Intensity Interval Training vs. Moderate-Intensity Continuous Training in Patients with Fibromyalgia: A Pilot Randomized Controlled Trial. Arch. Phys. Med. Rehabil. 2020, 101, 1865–1876. [Google Scholar] [CrossRef] [PubMed]
- Benham, J.L.; Booth, J.E.; Corenblum, B.; Doucette, S.; Friedenreich, C.M.; Rabi, D.M.; Sigal, R.J. Exercise training and reproductive outcomes in women with polycystic ovary syndrome: A pilot randomized controlled trial. Clin. Endocrinol. 2021, 95, 332–343. [Google Scholar] [CrossRef] [PubMed]
- Boff, W.; da Silva, A.M.; Farinha, J.B.; Rodrigues-Krause, J.; Reischak-Oliveira, A.; Tschiedel, B.; Puñales, M.; Bertoluci, M.C. Superior Effects of High-Intensity Interval vs. Moderate-Intensity Continuous Training on Endothelial Function and Cardiorespiratory Fitness in Patients with Type 1 Diabetes: A Randomized Controlled Trial. Front. Physiol. 2019, 10, 450. [Google Scholar] [CrossRef] [PubMed]
- Cheema, B.S.; Davies, T.B.; Stewart, M.; Papalia, S.; Atlantis, E. The feasibility and effectiveness of high-intensity boxing training versus moderate-intensity brisk walking in adults with abdominal obesity: A pilot study. BMC Sports Sci. Med. Rehabil. 2015, 7, 3. [Google Scholar] [CrossRef] [PubMed]
- Cocks, M.; Shaw, C.; Shepherd, S.O.; Fisher, J.; Ranasinghe, A.; Barker, T.A.; Wagenmakers, A.J.M. Sprint interval and moderate-intensity continuous training have equal benefits on aerobic capacity, insulin sensitivity, muscle capillarisation and endothelial eNOS/NAD(P)Hoxidase protein ratio in obese men. J. Physiol. 2016, 594, 2307–2321. [Google Scholar] [CrossRef]
- Connolly, L.; Bailey, S.; Krustrup, P.; Fulford, J.; Smietanka, C.; Jones, A.M. Effects of self-paced interval and continuous training on health markers in women. Eur. J. Appl. Physiol. 2017, 117, 2281–2293. [Google Scholar] [CrossRef]
- D’Amuri, A.; Sanz, J.M.; Capatti, E.; Di Vece, F.; Vaccari, F.; Lazzer, S.; Zuliani, G.; Nora, E.D.; Passaro, A. Effectiveness of high-intensity interval training for weight loss in adults with obesity: A randomised controlled non-inferiority trial. BMJ Open Sport Exerc. Med. 2021, 7, e001021. [Google Scholar] [CrossRef]
- Evangelista, A.L.; Teixeira, C.L.S.; Machado, A.F.; Pereira, P.E.; Rica, R.L.; Bocalini, D.S. Effects of a short-term of whole-body, high-intensity, intermittent training program on morphofunctional parameters. J. Bodyw. Mov. Ther. 2019, 23, 456–460. [Google Scholar] [CrossRef]
- Gao, Y.M.; Wang, G.M.; Yang, W.L.; Qiao, X.F. Effects of high intensity interval training and aerobic exercise on lipid metabolism and chronic inflammation in obese youth. Chin. J Sport. Med. 2017, 36, 628–632, 650. [Google Scholar] [CrossRef]
- Gilbertson, N.M.; Mandelson, J.A.; Hilovsky, K.; Akers, J.D.; Hargens, T.A.; Wenos, D.L.; Edwards, E.S. Combining supervised run interval training or moderate-intensity continuous training with the diabetes prevention program on clinical outcomes. Eur. J. Appl. Physiol. 2019, 119, 1503–1512. [Google Scholar] [CrossRef]
- Hesketh, K.; Jones, H.; Kinnafick, F.; Shepherd, S.O.; Wagenmakers, A.J.M.; Strauss, J.A.; Cocks, M. Home-Based HIIT and Traditional MICT Prescriptions Improve Cardiorespiratory Fitness to a Similar Extent within an Exercise Referral Scheme for At-Risk Individuals. Front. Physiol. 2021, 12, 750283. [Google Scholar] [CrossRef] [PubMed]
- Higgins, S.; Fedewa, M.V.; Hathaway, E.; Schmidt, M.; Evans, E.M. Sprint interval and moderate-intensity cycling training differentially affect adiposity and aerobic capacity in overweight young-adult women. Appl. Physiol. Nutr. Metab. 2016, 41, 1177–1183. [Google Scholar] [CrossRef] [PubMed]
- Hu, M.; Kong, Z.; Sun, S.; Zou, L.; Shi, Q.; Chow, B.C.; Nie, J. Interval training causes the same exercise enjoyment as moderate-intensity training to improve cardiorespiratory fitness and body composition in young Chinese women with elevated BMI. J. Sports Sci. 2021, 39, 1677–1686. [Google Scholar] [CrossRef]
- Keating, S.E.; Machan, E.A.; O’Connor, H.T.; Gerofi, J.A.; Sainsbury, A.; Caterson, I.D.; Johnson, N.A. Continuous Exercise but Not High Intensity Interval Training Improves Fat Distribution in Overweight Adults. J. Obes. 2014, 2014, 834865. [Google Scholar] [CrossRef]
- Liu, H.F.; Liu, Z.M.; Wang, C.M. Effect of high intensity interval training on lose weight in obese young women. J Shandong Sport Univ. 2016, 32, 95–98. [Google Scholar] [CrossRef]
- Mazurek, K.; Krawczyk, K.; Zmijewski, P.; Norkowski, H.; Czajkowska, A. Effects of aerobic interval training versus continuous moderate exercise programme on aerobic and anaerobic capacity, somatic features and blood lipid profile in collegate females. Ann. Agric. Environ. Med. 2014, 21, 844–849. [Google Scholar] [CrossRef]
- Middelbeek, R.J.W.; Motiani, P.; Brandt, N.; Nigro, P.; Zheng, J.; Virtanen, K.A.; Kalliokoski, K.K.; Hannukainen, J.C.; Goodyear, L.J. Exercise intensity regulates cytokine and klotho responses in men. Nutr. Diabetes 2021, 11, 5. [Google Scholar] [CrossRef] [PubMed]
- Nie, J.; Zhang, H.; Kong, Z.; George, K.; Little, J.P.; Tong, T.K.; Li, F.; Shi, Q. Impact of high-intensity interval training and moderate-intensity continuous training on resting and postexercise cardiac troponin T concentration. Exp. Physiol. 2018, 103, 370–380. [Google Scholar] [CrossRef]
- Petrick, H.L.; King, T.J.; Pignanelli, C.; Vanderlinde, T.E.; Cohen, J.N.; Holloway, G.P.; Burr, J.F. Endurance and Sprint Training Improve Glycemia and VO2peak but only Frequent Endurance Benefits Blood Pressure and Lipidemia. Med. Sci. Sports Exerc. 2021, 53, 1194–1205. [Google Scholar] [CrossRef]
- Ram, A.; Marcos, L.; Jones, M.D.; Morey, R.; Hakansson, S.; Clark, T.; Ristov, M.; Franklin, A.; McCarthy, C.; De Carli, L.; et al. The effect of high-intensity interval training and moderate-intensity continuous training on aerobic fitness and body composition in males with overweight or obesity: A randomized trial. Obes. Med. 2020, 17, 100187. [Google Scholar] [CrossRef]
- Saanijoki, T.; Nummenmaa, L.; Eskelinen, J.-J.; Savolainen, A.M.; Vahlberg, T.; Kalliokoski, K.; Hannukainen, J. Affective Responses to Repeated Sessions of High-Intensity Interval Training. Med. Sci. Sports Exerc. 2015, 47, 2604–2611. [Google Scholar] [CrossRef] [PubMed]
- Scott, S.N.; Cocks, M.; Andrews, R.C.; Narendran, P.; Purewal, T.S.; Cuthbertson, D.J.; Wagenmakers, A.J.M.; Shepherd, S.O. High-Intensity Interval Training Improves Aerobic Capacity without a Detrimental Decline in Blood Glucose in People with Type 1 Diabetes. J. Clin. Endocrinol. Metab. 2019, 104, 604–612. [Google Scholar] [CrossRef] [PubMed]
- Sijie, T.; Hainai, Y.; Fengying, Y.; Jianxiong, W. High intensity interval exercise training in overweight young women. J. Sports Med. Phys. Fit. 2012, 52, 255–262. [Google Scholar]
- Sjöros, T.J.; Heiskanen, M.A.; Motiani, K.K.; Löyttyniemi, E.; Eskelinen, J.; Virtanen, K.A.; Savisto, N.J.; Solin, O.; Hannukainen, J.C.; Kalliokoski, K.K. Increased insulin-stimulated glucose uptake in both leg and arm muscles after sprint interval and moderate-intensity training in subjects with type 2 diabetes or prediabetes. Scand. J. Med. Sci. Sports 2018, 28, 77–87. [Google Scholar] [CrossRef]
- Tsai, H.-H.; Lin, C.-P.; Lin, Y.-H.; Hsu, C.-C.; Wang, J.-S. High-intensity Interval training enhances mobilization/functionality of endothelial progenitor cells and depressed shedding of vascular endothelial cells undergoing hypoxia. Eur. J. Appl. Physiol. 2016, 116, 2375–2388. [Google Scholar] [CrossRef]
- Wang, J.J.; Han, H.; Zhang, H. Effects of High-intensity Interval Training and Continuous Training on Abdominal Fat in ObeseYoung Women. Chin. J Sport. Med. 2015, 34, 15–20. [Google Scholar] [CrossRef]
- Way, K.L.; Sabag, A.; Sultana, R.N.; Baker, M.K.; Keating, S.E.; Lanting, S.; Gerofi, J.; Chuter, V.H.; Caterson, I.D.; Twigg, S.M.; et al. The effect of low-volume high-intensity interval training on cardiovascular health outcomes in type 2 diabetes: A randomised controlled trial. Int. J. Cardiol. 2020, 320, 148–154. [Google Scholar] [CrossRef]
- Winn, N.C.; Liu, Y.; Rector, R.S.; Parks, E.J.; Ibdah, J.A.; Kanaley, J.A. Energy-matched moderate and high intensity exercise training improves nonalcoholic fatty liver disease risk independent of changes in body mass or abdominal adiposity—A randomized trial. Metabolism 2018, 78, 128–140. [Google Scholar] [CrossRef]
- Hang, Y.; Heng, Y. The significant improvement effect of uHIIT on reducing fat in men. Genom. Appl. Biol. 2019, 38, 409–415. [Google Scholar] [CrossRef]
- Ramos, J.S.; Dalleck, L.C.; Tjonna, A.E.; Beetham, K.; Coombes, J.S. The Impact of High-Intensity Interval Training Versus Moderate-Intensity Continuous Training on Vascular Function: A Systematic Review and Meta-Analysis. Sports Med. 2015, 45, 679–692. [Google Scholar] [CrossRef]
- Walberg, J.L. Aerobic exercise and resistance weight-training during weight reduction. Implications for obese persons and athletes. Sports Med. 1989, 7, 343–356. [Google Scholar] [CrossRef] [PubMed]
- Poon, E.T.-C.; Sun, F.-H.; Chung, A.P.-W.; Wong, S.H.-S. Post-Exercise Appetite and Ad Libitum Energy Intake in Response to High-Intensity Interval Training versus Moderate- or Vigorous-Intensity Continuous Training among Physically Inactive Middle-Aged Adults. Nutrients 2018, 10, 1408. [Google Scholar] [CrossRef] [PubMed]
- Jurado-Fasoli, L.; De-La-O, A.; Molina-Hidalgo, C.; Migueles, J.H.; Castillo, M.J.; Amaro-Gahete, F.J. Exercise training improves sleep quality: A randomized controlled trial. Eur. J. Clin. Investig. 2020, 50, e13202. [Google Scholar] [CrossRef] [PubMed]
- Geiker, N.R.W.; Astrup, A.; Hjorth, M.F.; Sjödin, A.; Pijls, L.; Markus, C.R. Does stress influence sleep patterns, food intake, weight gain, abdominal obesity and weight loss interventions and vice versa? Obes. Rev. 2018, 19, 81–97. [Google Scholar] [CrossRef]
- O’Donoghue, G.; Blake, C.; Cunningham, C.; Lennon, O.; Perrotta, C. What exercise prescription is optimal to improve body composition and cardiorespiratory fitness in adults living with obesity? A network meta-analysis. Obes. Rev. 2021, 22, e13137. [Google Scholar] [CrossRef]
- Vieira, A.F.; Costa, R.R.; Macedo, R.C.O.; Coconcelli, L.; Kruel, L.F.M. Effects of aerobic exercise performed in fasted v. fed state on fat and carbohydrate metabolism in adults: A systematic review and meta-analysis. Br. J. Nutr. 2016, 116, 1153–1164. [Google Scholar] [CrossRef]
- Maughan, R.J.; Greenhaff, P.L.; Leiper, J.B.; Ball, D.; Lambert, C.P.; Gleeson, M. Diet composition and the performance of high-intensity exercise. J. Sports Sci. 1997, 15, 265–275. [Google Scholar] [CrossRef]
- Viitasalo, A.; Schnurr, T.M.; Pitkänen, N.; Hollensted, M.; Nielsen, T.R.H.; Pahkala, K.; Atalay, M.; Lind, M.V.; Heikkinen, S.; Frithioff-Bøjsøe, C.; et al. Abdominal adiposity and cardiometabolic risk factors in children and adolescents: A Mendelian randomization analysis. Am. J. Clin. Nutr. 2019, 110, 1079–1087. [Google Scholar] [CrossRef]
- Cerhan, J.R.; Moore, S.C.; Jacobs, E.J.; Kitahara, C.M.; Rosenberg, P.S.; Adami, H.-O.; Ebbert, J.O.; English, D.R.; Gapstur, S.M.; Giles, G.G.; et al. A Pooled Analysis of Waist Circumference and Mortality in 650,000 Adults. Mayo Clin. Proc. 2014, 89, 335–345. [Google Scholar] [CrossRef]
- Smith, U. Abdominal obesity: A marker of ectopic fat accumulation. J. Clin. Investig. 2015, 125, 1790–1792. [Google Scholar] [CrossRef]
- Andreato, L.V.; Esteves, J.V.; Coimbra, D.R.; Moraes, A.J.P.; De Carvalho, T. The influence of high-intensity interval training on anthropometric variables of adults with overweight or obesity: A systematic review and network meta-analysis. Obes. Rev. 2019, 20, 142–155. [Google Scholar] [CrossRef]
- Maillard, F.; Pereira, B.; Boisseau, N. Effect of High-Intensity Interval Training on Total, Abdominal and Visceral Fat Mass: A Meta-Analysis. Sports Med. 2017, 48, 269–288. [Google Scholar] [CrossRef] [PubMed]
- Rebuffé-Scrive, M.; Andersson, B.; Olbe, L.; Björntorp, P. Metabolism of adipose tissue in intraabdominal depots of nonobese men and women. Metabolism 1989, 38, 453–458. [Google Scholar] [CrossRef] [PubMed]
- Dun, Y.; Thomas, R.J.; Smith, J.R.; Medina-Inojosa, J.R.; Squires, R.W.; Bonikowske, A.R.; Huang, H.; Liu, S.; Olson, T.P. High-intensity interval training improves metabolic syndrome and body composition in outpatient cardiac rehabilitation patients with myocardial infarction. Cardiovasc. Diabetol. 2019, 18, 104. [Google Scholar] [CrossRef] [PubMed]
- Padwal, R.; Leslie, W.D.; Lix, L.M.; Majumdar, S.R. Relationship Among Body Fat Percentage, Body Mass Index, and All-Cause Mortality: A Cohort Study. Ann. Intern. Med. 2016, 164, 532–541. [Google Scholar] [CrossRef]
- Zhuang, Z.; Yao, M.; Wong, J.Y.Y.; Liu, Z.; Huang, T. Shared genetic etiology and causality between body fat percentage and cardiovascular diseases: A large-scale genome-wide cross-trait analysis. BMC Med. 2021, 19, 100. [Google Scholar] [CrossRef]
- Slimani, M.; Znazen, H.; Hammami, A.; Bragazzi, N.L. Comparison of body fat percentage of male soccer players of different competitive levels, playing positions and age groups: A meta-analysis. J. Sports Med. Phys. Fit. 2018, 58, 857–866. [Google Scholar] [CrossRef]
- Boutcher, S.H. High-Intensity Intermittent Exercise and Fat Loss. J. Obes. 2011, 2011, 868305. [Google Scholar] [CrossRef]
- Stevens, J.; Truesdale, K.P.; McClain, J.E.; Cai, J. The definition of weight maintenance. Int. J. Obes. 2006, 30, 391–399. [Google Scholar] [CrossRef]
- Sedlmeier, A.M.; Baumeister, S.E.; Weber, A.; Fischer, B.; Thorand, B.; Ittermann, T.; Dörr, M.; Felix, S.B.; Völzke, H.; Peters, A.; et al. Relation of body fat mass and fat-free mass to total mortality: Results from 7 prospective cohort studies. Am. J. Clin. Nutr. 2021, 113, 639–646. [Google Scholar] [CrossRef]
- Merchant, R.A.; Seetharaman, S.; Au, L.; Wong, M.W.K.; Wong, B.L.L.; Tan, L.F.; Chen, M.Z.; Ng, S.E.; Soong, J.T.Y.; Hui, R.J.Y.; et al. Relationship of Fat Mass Index and Fat Free Mass Index with Body Mass Index and Association with Function, Cognition and Sarcopenia in Pre-Frail Older Adults. Front. Endocrinol. 2021, 12, 765415. [Google Scholar] [CrossRef] [PubMed]
- Larsson, S.C.; Burgess, S. Fat mass and fat-free mass in relation to cardiometabolic diseases: A two-sample Mendelian randomization study. J. Intern. Med. 2020, 288, 260–262. [Google Scholar] [CrossRef] [PubMed]
- Callahan, M.J.; Parr, E.B.; Snijders, T.; Conceição, M.S.; Radford, B.E.; Timmins, R.G.; Devlin, B.L.; Hawley, J.A.; Camera, D.M. Skeletal Muscle Adaptive Responses to Different Types of Short-Term Exercise Training and Detraining in Middle-Age Men. Med. Sci. Sports Exerc. 2021, 53, 2023–2036. [Google Scholar] [CrossRef] [PubMed]
- Scoubeau, C.; Bonnechère, B.; Cnop, M.; Faoro, V.; Klass, M. Effectiveness of Whole-Body High-Intensity Interval Training on Health-Related Fitness: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2022, 19, 9559. [Google Scholar] [CrossRef]
- Trapp, E.G.; Chisholm, D.J.; Boutcher, S.H. Metabolic response of trained and untrained women during high-intensity intermittent cycle exercise. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2007, 293, R2370–R2375. [Google Scholar] [CrossRef]
- Lavie, C.J.; Ozemek, C.; Carbone, S.; Katzmarzyk, P.T.; Blair, S.N. Sedentary Behavior, Exercise, and Cardiovascular Health. Circ. Res. 2019, 124, 799–815. [Google Scholar] [CrossRef]
- Holmlund, T.; Ekblom, B.; Börjesson, M.; Andersson, G.; Wallin, P.; Ekblom-Bak, E. Association between change in cardiorespiratory fitness and incident hypertension in Swedish adults. Eur. J. Prev. Cardiol. 2021, 28, 1515–1522. [Google Scholar] [CrossRef]
- Buscemi, S.; Canino, B.; Batsis, J.A.; Buscemi, C.; Calandrino, V.; Mattina, A.; Arnone, M.; Caimi, G.; Cerasola, G.; Verga, S. Relationships between maximal oxygen uptake and endothelial function in healthy male adults: A preliminary study. Acta Diabetol. 2013, 50, 135–141. [Google Scholar] [CrossRef]
- Davison, K.; Bircher, S.; Hill, A.; Coates, A.M.; Howe, P.; Buckley, J. Relationships between Obesity, Cardiorespiratory Fitness, and Cardiovascular Function. J. Obes. 2010, 2010, 191253. [Google Scholar] [CrossRef]
- Howden, E.J.; Leano, R.; Petchey, W.; Coombes, J.S.; Isbel, N.M.; Marwick, T.H. Effects of Exercise and Lifestyle Intervention on Cardiovascular Function in CKD. Clin. J. Am. Soc. Nephrol. 2013, 8, 1494–1501. [Google Scholar] [CrossRef]
- Batacan, R.B., Jr.; Duncan, M.J.; Dalbo, V.J.; Tucker, P.S.; Fenning, A.S. Effects of high-intensity interval training on cardiometabolic health: A systematic review and meta-analysis of intervention studies. Br. J. Sports Med. 2017, 51, 494–503. [Google Scholar] [CrossRef] [PubMed]
- Soylu, Y.; Arslan, E.; Sogut, M.; Kilit, B.; Clemente, F.M. Effects of self-paced high-intensity interval training and moderateintensity continuous training on the physical performance and psychophysiological responses in recreationally active young adults. Biol. Sport 2021, 38, 555–562. [Google Scholar] [CrossRef] [PubMed]
- Mitranun, W.; Deerochanawong, C.; Tanaka, H.; Suksom, D. Continuous vs. interval training on glycemic control and macro- and microvascular reactivity in type 2 diabetic patients. Scand. J. Med. Sci. Sports 2014, 24, e69–e76. [Google Scholar] [CrossRef]
- Wisløff, U.; Støylen, A.; Loennechen, J.P.; Bruvold, M.; Rognmo, Ø.; Haram, P.M.; Tjønna, A.E.; Helgerud, J.; Slørdahl, S.A.; Lee, S.J.; et al. Superior cardiovascular effect of aerobic interval training versus moderate continuous training in heart failure patients: A randomized study. Circulation 2007, 115, 3086–3094. [Google Scholar] [CrossRef] [PubMed]
- Eather, N.; Riley, N.; Miller, A.; Smith, V.; Poole, A.; Vincze, L.; Morgan, P.J.; Lubans, D. Efficacy and feasibility of HIIT training for university students: The Uni-HIIT RCT. J. Sci. Med. Sport 2019, 22, 596–601. [Google Scholar] [CrossRef] [PubMed]
- Blackwell, J.; Atherton, P.J.; Smith, K.; Doleman, B.; Williams, J.P.; Lund, J.; Phillips, B. The efficacy of unsupervised home-based exercise regimens in comparison to supervised laboratory-based exercise training upon cardio-respiratory health facets. Physiol. Rep. 2017, 5, e13390. [Google Scholar] [CrossRef] [PubMed]
- Guo, Z.; Cai, J.; Wu, Z.; Gong, W. Effect of High-Intensity Interval Training Combined with Fasting in the Treatment of Overweight and Obese Adults: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2022, 19, 4638. [Google Scholar] [CrossRef] [PubMed]
- Brown, J.C.; Sarwer, D.B.; Troxel, A.B.; Sturgeon, K.; DeMichele, A.M.; Denlinger, C.S.; Schmitz, K.H. A randomized trial of exercise and diet on health-related quality of life in survivors of breast cancer with overweight or obesity. Cancer 2021, 127, 3856–3864. [Google Scholar] [CrossRef]
- Bartlett, J.D.; Close, G.; MacLaren, D.P.M.; Gregson, W.; Drust, B.; Morton, J.P. High-intensity interval running is perceived to be more enjoyable than moderate-intensity continuous exercise: Implications for exercise adherence. J. Sports Sci. 2011, 29, 547–553. [Google Scholar] [CrossRef]
- Martinez, N.; Kilpatrick, M.W.; Salomon, K.; Jung, M.E.; Little, J.P. Affective and Enjoyment Responses to High-Intensity Interval Training in Overweight-to-Obese and Insufficiently Active Adults. J. Sport Exerc. Psychol. 2015, 37, 138–149. [Google Scholar] [CrossRef]
- Oliveira, B.R.R.; Santos, T.; Kilpatrick, M.; Pires, F.O.; Deslandes, A.C. Affective and enjoyment responses in high intensity interval training and continuous training: A systematic review and meta-analysis. PLoS ONE 2018, 13, e0197124. [Google Scholar] [CrossRef] [PubMed]


| PICOS | Inclusion | Exclusion |
|---|---|---|
| Participant | young and middle-aged (18–60 years old) | Age-incompatible |
| Intervention | HIIT | Intensity < 80–100% VO2peak or HRmax; Other intervention |
| Comparison | MICT | Duration < 15 min; Other intervention |
| Outcome | BM; BMI; WC; PFM; FM; FFM; VO2peak; SBP; DBP | Other outcomes |
| Study | RCT | Books; opinion articles; observational studies; reviews; prospective cohort studies; studies and abstracts without adequate data |
| Study | Duration | Age (Years) | Mela/ Female or Total | Participant | Types of Sport | HIIT | MICT | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sample Size | Exercise Intensity | Exercise Time per Times | Frequency | Dropouts (Attendance Rate) | Sample Size | Exercise Intensity | Exercise Time per Times | Frequency | Dropouts (Attendance Rate) | ||||||
| Atan 2020 [41] | 6 weeks | 47.6 ± 8.7 | 0/40 | Fibromyalgia | Bicycle | 19 | 4 min 80–95% HRmax; 3 min 70% HRmax | 25 min | 5 times/week | 1 (95%) | 19 | 65–70% HRmax | 45 min | 5 times/week | 1 (95%) |
| Benham 2021 [42] | 6 months | 18–40 | 0/30 | Polycystic ovary syndrome | Bicycle | 16 | 30 s 90% HRmax; 90 s low-intensity aerobic exercise | 20 min | 3 times/week | 0 | 14 | 50–60% HRmax | 40 min | 3 times/week | 0 |
| Boff 2019 [43] | 2 months | 23.5 ± 6 | 8/10 | Type 1 diabete | Bicycle | 9 | 1 min 80–85% HRmax; 4 min 50% HRmax | 30 min | 3 times/week | 0 | 9 | 60–65% HRmax | 20–30 min | 3 times/week | 0 |
| Cheema 2015 [44] | 3 months | 39 ± 17 | 5/7 | Sedentary obesity | Boxing/walking | 6 | 2 min 15–20 RPE; 1 min passive recovery | 30 min | 1 times/week | 0 | 6 | 4 MET | 45 min | 1 times/week | 0 |
| Cocks 2014 [45] | 4 weeks | 25 ± 1 | 16/0 | Sedentary obesity | Bicycle | 8 | 30 s 200% Wmax; 2 min 30 W for recovery | 10–15 min | 5 times/week | 0 | 8 | 65% VO2peak | 40–60 min | 5 times/week | 0 |
| Connolly 2017 [46] | 3 months | 43.5 ± 7 | 0/36 | Sedentary obesity | Bicycle | 15 | 30 s 30% maximum effort; 20 s 50–60% maximum effort; 10 s 90% maximum effort | 15–25 min | 3 times/week | 1 (94%) | 15 | A self-paced intensity | 30–50 min | 3 times/week | 1 (94%) |
| D’Amuri 2021 [47] | 3 months | 38.7 ± 8.1 | 17/15 | Sedentary obesity | Running | 16 | 3 min 100% VO2peak; 1.5 min 50% VO2peak | 13.5–31.5 min | 3 times/week | 0 | 16 | 60% VO2peak | 30 min | 3 times/week | 0 |
| Evangelista 2019 [48] | 6 weeks | 28.5 ± 5.6 | 25 | Sedentary obesity | Whole body HIIT/Running | 14 | 30 s all-out exercise; 30 s passive recovery | 20 min | 3 times/week | 0 | 11 | 80% HRmax | 20 min | 3 times/week | 0 |
| Gao 2017 [49] | 3 months | 21.6 ± 1.4 | 25/25 | Sedentary obesity | Running | 17 | 4min 85% VO2peak; 2 min 50% VO2peak | 30 min | 5 times/week | 8 (67%) | 17 | 60% VO2peak | 40 min | 5 times/week | 8 (67%) |
| Gilbertson 2019 [50] | 4 months | 48.3 ± 4.4 | 29 | Prediabetes | Running | 6 | 30 s 19–20 RPE; 4 min active rest | 18–45 min | 3 times/week | 11 (35%) | 9 | 45–55% HRmax | 30–60 min | 3 times/week | 3 (75%) |
| Hesketh 2021 [51] | 3 months | 48 ± 10 | 88/66 | Sedentary obesity | Home-based HIIT/ Running | 21 | 1 min ≥ 80 HRmax; 1 min passive recovery | 8–18 min | 3 times/week | 66 (24%) | 29 | 50–70% HRmax | 15–45 min | 3 times/week | 38 (43%) |
| Higgins 2016 [52] | 6 weeks | 20.4 ± 1.5 | 0/52 | Sedentary obesity | Bicycle | 23 | 30 s all-out exercise; 4 min active recovery | 22.5–31.5 min | 3 times/week | 0 | 29 | 60–70% HRmax | 20–30 min | 3 times/week | 0 |
| Hu 2021 [53] | 3 months | 21.1 ± 1.4 | 0/33 | Sedentary obesity | Bicycle | 15 | 4 min 90% VO2peak; 3 min passive recovery | 28–54 min | 3 times/week | 2 (88%) | 15 | 60% VO2peak | 40–60 min | 3 times/week | 1 (89%) |
| Keating 2014 [54] | 3 months | 43 ± 8.3 | 5/21 | Sedentary obesity | Bicycle | 11 | 30–45 s 120% VO2peak; 2–3 min low intensity | 14–18 min | 3 times/week | 2 (85%) | 11 | 50–65% VO2peak | 30–42 min | 3 times/week | 2 (85%) |
| Liu 2016 [55] | 3 months | 20–23 | 0/40 | Sedentary obesity | Bicycle | 20 | 1 min 90% VO2peak; 1 min 20% VO2peak | 30 min | 4 times/week | 0 | 20 | 50% VO2peak | 30 min | 4 times/week | 0 |
| Mazurek 2014 [56] | 2 months | 19.5 ± 0.6 | 0/46 | Sedentary | Bicycle | 24 | 10 s maximal sprinting 1 min 65–75% HRmax | 32 min | 3 times/week | 0 | 22 | 65–75% HRmax | 32 min | 3 times/week | 0 |
| Middelbeek 2021 [57] | 2 weeks | 48 ± 5 | 22/0 | Sedentary obesity | Bicycle | 12 | 30 s all-out exercise; 4 min passive recovery | 27 min | 3 times/week | 0 | 10 | 60% VO2peak | 40–60 min | 3 times/week | 0 |
| Nie 2017 [58] | 3 months | 21 ± 1.4 | 0/32 | Sedentary obesity | Bicycle | 16 | 4 min 90% VO2peak; 3 min passive recovery | 300 kJ | 3–4 times/week | 1 (88%) | 14 | 60% VO2peak | 300 kJ | 3–4 times/week | 1 (93%) |
| Petrick 2020 [59] | 6 weeks | 37.4 ± 15.1 | 23/0 | Sedentary obesity | Bicycle | 12 | 30 s 170% Wpeak; 2 min passive recovery | 10–15 min | 3 times/week | 0 | 11 | 60% Wpeak | 30–40 min | 5 times/week | 0 |
| Ram 2020 [60] | 6 weeks | 28 ± 7 | 28/0 | Sedentary obesity | Bicycle | 16 | 1 min 90% HRmax; 1 min 15% Wpeak | 20 min | 3 times/week | 0 | 12 | 65–75% HRmax | 30 min | 3 times/week | 0 |
| Saanijoki 2015 [61] | 2 weeks | 48 ± 5 | 26/0 | Sedentary obesity | Bicycle | 13 | 30 s 180% peak workload sprints; 4min passive recovery | 18–27 min | 3 times/week | 1 (93%) | 13 | 60% peak workload | 40–60 min | 3 times/week | 1 (93%) |
| Scott 2019 [62] | 6 weeks | 29 ± 10.6 | 10/4 | Type 1 diabete | Bicycle | 7 | 1 min 100% VO2peak; 1 min recovery at 50W | 12–20 min | 3 times/week | 0 | 7 | 65% VO2peak | 30–50 min | 3 times/week | 0 |
| Sijie 2012 [63] | 3 months | 19.6 ± 0.8 | 0/40 | Sedentary obesity | Running | 17 | 3 min 85% VO2peak; 3 min 50% VO2peak | 30 min | 5 times/week | 3 (85%) | 16 | 50% VO2peak | 40 min | 5 times/week | 4 (80%) |
| Sjöros 2018 [64] | 2 weeks | 49 ± 4 | 16/10 | Type 2 diabete or prediabetes | Bicycle | 11 | 30 s all-out exercise; 4 min passive recovery | 18–27 min | 3 times/week | 2 (85%) | 10 | 60% VO2peak | 40–60 min | 3 times/week | 3 (77%) |
| Tsai 2016 [65] | 6 weeks | 22.3 ± 5.9 | 40/0 | Sedentary | Bicycle | 20 | 3 min 80% VO2peak; 3 min 40% VO2peak | 30 min | 5 times/week | 0 | 20 | 60% VO2peak | 30 min | 5 times/week | 0 |
| Wang 2015 [66] | 3 months | 20.8 ± 1.1 | 0/24 | Sedentary obesity | Running | 12 | 4min 85–95% HRmax; 7 min 50–60% HRmax | 44 min | 4 times/week | 0 | 12 | 60–70% HRmax | 33 min | 4 times/week | 0 |
| Way 2020 [67] | 3 months | 55.9 ± 2.3 | 26 | Type 2 diabete | Bicycle | 12 | 4 min 90% VO2peak; 5 min 50% VO2peak | 9 min | 3 times/week | 0 | 12 | 60% VO2peak | 45 min | 3 times/week | 2 (86%) |
| Winn 2017 [68] | 4 weeks | 43.5 ± 11.5 | 18 | Sedentary obesity | Bicycle | 8 | 4 min 80% VO2peak; 3 min 50% VO2peak | 400 kJ | 4 times/week | 1 (89%) | 8 | 55% VO2peak | 400 kJ | 4 times/week | 1 (89%) |
| Ying 2019 [69] | 3 months | 35–45 | 18/0 | Sedentary obesity | Running | 8 | 2 min 90% HRmax; 1 min passive recovery | 21 min | 3 times/week | 1 (89%) | 8 | 65–70% HRmax | 40 min | 3 times/week | 1 (89%) |
| Outcome | Within-Group Effects | Between-Group Effects | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Included Studies (n) | HIIT | MICT | HIIT vs. MICT | Heterogeneity | ||||||||
| n | MD | p | n | MD | p | MD | 95% CI | p | I2 (%) | p | ||
| BM (kg) | 28 | 383 | −2 | 0.0019 * | 374 | −2.19 | 0.0011 * | −0.32 | −0.86 to −0.26 | 0.2514 | 0 | 1 |
| BMI (kg/m2) | 25 | 353 | −0.9 | 0.000 * | 346 | −0.92 | 0.000 * | 0.17 | −0.11 to 0.46 | 0.2511 | 0 | 1 |
| WC (cm) | 12 | 172 | −4.41 | 0.002 * | 161 | −2.96 | 0.000 * | −0.96 | −1.84 to −0.08 | 0.0367 | 0 | 1 |
| PFM (%) | 21 | 276 | −2.03 # | 0.000 * | 286 | −1.89 # | 0.000 * | −0.48 | −0.86 to −0.1 | 0.0135 | 0 | 1 |
| FM (kg) | 14 | 183 | −1.79 # | 0.0028 * | 182 | −2.33 # | 0.0002 * | −0.22 | −0.98 to 0.55 | 0.5578 | 0 | 0.78 |
| FFM (kg) | 16 | 210 | −0.36 # | 0.4867 | 208 | −0.38 # | 0.4577 | −0.12 | −0.48 to 0.25 | 0.5348 | 0 | 1 |
| VO2peak | 27 | 371 | 0.83 $ | 0.000 * | 373 | 0.6 $ | 0.000 * | 0.19 $ | 0.03 to 0.34 | 0.0211 | 9 | 0.33 |
| SBP (mmHg) | 14 | 166 | −3.83 | 0.0097 * | 165 | −3.56 | 0.002 * | 0.55 | −1.92 to 3.02 | 0.6626 | 26 | 0.17 |
| DBP (mmHg) | 14 | 166 | −1.59 | 0.034 | 165 | −1.88 | 0.024 | 0.68 | −0.76 to 2.13 | 0.3523 | 2 | 0.96 |
| Outcome | Studies (n) | MD | (95% CI) | p | Heterogeneity | |
|---|---|---|---|---|---|---|
| I2 (%) | p | |||||
| BM (kg) | ||||||
| Age: 18–45 years | 21 | MD = 0.19 | −0.72 to 1.1 | 0.6841 | 0% | 0.9993 |
| Age: 45–60 years | 7 | MD = −0.46 | −1.25 to 0.32 | 0.249 | 0% | 0.9819 |
| Complications: obesity | 19 | MD = −0.47 | −1.15 to 0.22 | 0.1846 | 0% | 0.9938 |
| Complications: other chronic disease | 7 | MD = −0.31 | −1.26 to 0.65 | 0.5321 | 0% | 0.9985 |
| Duration: ≤6 weeks | 12 | MD = 0.02 | −1.03 to 1.06 | 0.9723 | 0% | 0.9954 |
| Duration: >6 weeks | 16 | MD = −0.44 | −1.08 to 0.19 | 0.1727 | 0% | 0.981 |
| Frequency: ≤3 times/week | 19 | MD = −0.53 | −1.14 to 0.07 | 0.0829 | 0% | 1 |
| Frequency: >3 times/week | 9 | MD = 0.62 | −0.64 to 1.88 | 0.3348 | 0% | 0.9098 |
| HIIT interval: 1−3 min | 15 | MD = −0.1 | −0.93 to 0.73 | 0.8124 | 0% | 0.9995 |
| HIIT interval: ≥3 min | 13 | MD = −0.47 | −1.21 to 0.27 | 0.2093 | 0% | 0.9239 |
| BMI (kg/m2) | ||||||
| Age: 18−45 years | 18 | MD = 0.05 | −0.24 to 0.33 | 0.7494 | 0% | 0.5159 |
| Age: 45−60 years | 7 | MD = 0.28 | −0.1 to 0.66 | 0.1525 | 0% | 0.9916 |
| Complications: obesity | 17 | MD = 0.12 | −0.12 to 035 | 0.3427 | 0% | 0.9971 |
| Complications: other chronic disease | 6 | MD = 0.63 | 0.1 to 1.16 | 0.0189 | 0% | 0.9426 |
| Duration: ≤6 weeks | 11 | MD = 0.11 | −0.26 to 0.49 | 0.5575 | 0% | 0.9983 |
| Duration: >6 weeks | 14 | MD = 0.12 | −0.18 to 0.42 | 0.4225 | 29% | 0.1459 |
| Frequency: ≤3 times/week | 16 | MD = 0.26 | −0.04 to 0.55 | 0.0855 | 0% | 0.9608 |
| Frequency: >3 times/week | 9 | MD = −0.03 | −0.33 to 0.27 | 0.8313 | 0% | 0.5479 |
| HIIT interval: 1−3 min | 12 | MD = 0.12 | −0.17 to 0.41 | 0.4084 | 0% | 0.9991 |
| HIIT interval: ≥3 min | 13 | MD = 0.12 | −0.28 to 0.53 | 0.5521 | 27% | 0.1711 |
| WC (cm) | ||||||
| Age: 18−45 years | 11 | MD = −0.96 | −1.85 to −0.07 | 0.0338 | 0% | 0.9909 |
| Age: 45−60 years | 1 | MD = −0.9 | −10.06 to 8.26 | NA | NA | NA |
| Complications: obesity | 9 | MD = −0.95 | −1.88 to −0.02 | 0.0461 | 0% | 0.9652 |
| Complications: other chronic disease | 2 | MD = −0.55 | −5.49 to 4.4 | 0.8288 | 0% | 0.9283 |
| Duration: ≤6 weeks | 3 | MD = −1.36 | −3.58 to 0.86 | 0.229 | 0% | 0.9696 |
| Duration: >6 weeks | 9 | MD = −0.89 | −1.85 to 0.08 | 0.0717 | 0% | 0.9709 |
| Frequency: ≤3 times/week | 8 | MD = −1.03 | −3.07 to 0.99 | 0.3164 | 0% | 0.9657 |
| Frequency: >3 times/week | 4 | MD = −0.94 | −1.92 to −0.08 | 0.0397 | 0% | 0.8962 |
| HIIT interval: 1−3 min | 4 | MD = −0.92 | −2.35 to 0.52 | 0.2113 | 0% | 0.8198 |
| HIIT interval: ≥3 min | 8 | MD = −0.99 | −2.11 to 0.13 | 0.0839 | 0% | 0.9798 |
| PFM (%) | ||||||
| Age: 18−45 years | 16 | MD = −0.5 | −0.89 to −0.11 | 0.0112 | 0% | 0.9969 |
| Age: 45−60 years | 4 | MD = −0.1 | −1.82 to 1.61 | 0.9074 | 0% | 0.8989 |
| Complications: obesity | 18 | MD = −0.54 | −0.94 to −0.14 | 0.0085 | 0% | 0.9989 |
| Complications: other chronic disease | 2 | MD = 0.48 | −1.92 to 2.88 | 0.6953 | 0% | 0.7335 |
| Duration: ≤6 weeks | 9 | MD = −0.01 | −0.89 to 0.88 | 0.995 | 0% | 0.9844 |
| Duration: >6 weeks | 11 | MD = −0.62 | −1.15 to −0.08 | 0.0252 | 0% | 0.9977 |
| Frequency: ≤3 times/week | 12 | MD = −0.61 | −1.24 to 0.01 | 0.0576 | 0% | 1 |
| Frequency: >3 times/week | 8 | MD = −0.45 | −0.96 to 0.06 | 0.086 | 0% | 0.7558 |
| HIIT interval: 1−3 min | 9 | MD = −0.43 | −0.92 to 0.06 | 0.0823 | 0% | 0.8745 |
| HIIT interval: ≥3 min | 11 | MD = −0.67 | −1.36 to −0.06 | 0.0276 | 0% | 0.9996 |
| FM (kg) | ||||||
| Age: 18−45 years | 11 | MD = −0.45 | −1.2 to 0.3 | 0.2443 | 0% | 0.8256 |
| Age: 45−60 years | 3 | MD = 1.33 | −0.79 to 3.45 | 0.2174 | 0% | 0.9593 |
| Complications: obesity | 12 | MD = −0.27 | −1.04 to 0.49 | 0.485 | 0% | 0.7089 |
| Complications: other chronic disease | 2 | MD = 1.43 | −2.8 to 5.67 | 0.507 | 0% | 0.7771 |
| Duration: ≤6 weeks | 6 | MD = −0.32 | −1.8 to 1.16 | 0.6695 | 0% | 0.4261 |
| Duration: >6 weeks | 8 | MD = −0.05 | −0.84 to 0.75 | 0.9105 | 0% | 0.9652 |
| Frequency: ≤3 times/week | 10 | MD = −0.25 | −1.4 to 0.9 | 0.666 | 0% | 0.6651 |
| Frequency: >3 times/week | 4 | MD = −0.06 | −0.99 to 0.86 | 0.8909 | 0% | 0.7852 |
| HIIT interval: 1−3 min | 8 | MD = −0.41 | −1.19 to 0.37 | 0.3026 | 0% | 0.4914 |
| HIIT interval: ≥3 min | 6 | MD = 0.9 | −1.03 to 2.83 | 0.3587 | 0% | 0.9954 |
| FFM (kg) | ||||||
| Age: 18−45 years | 11 | MD = −0.15 | −0.52 to 0.23 | 0.4425 | 0% | 0.9979 |
| Age: 45−60 years | 5 | MD = 0.48 | −1.16 to 2.13 | 0.5663 | 0% | 0.9758 |
| Complications: obesity | 13 | MD = −0.12 | −0.49 to 0.25 | 0.5208 | 0% | 0.9976 |
| Complications: other chronic disease | 3 | MD = 0.11 | −2.26 to 2.47 | 0.9298 | 0% | 0.9555 |
| Duration: ≤6 weeks | 8 | MD = 0.02 | −0.62 to 0.66 | 0.9475 | 0% | 1 |
| Duration: >6 weeks | 8 | MD = −0.18 | −0.63 to 0.26 | 0.4209 | 0% | 0.9374 |
| Frequency: ≤3 times/week | 12 | MD = 0.12 | −0.41 to 0.65 | 0.6578 | 0% | 1 |
| Frequency: >3 times/week | 4 | MD = −0.33 | −0.83 to 0.18 | 0.2036 | 0% | 0.9213 |
| HIIT interval: 1−3 min | 9 | MD = 0 | −0.45 to 0.45 | 0.9994 | 0% | 0.9999 |
| HIIT interval: ≥3 min | 7 | MD = −0.34 | −0.97 to 0.29 | 0.2864 | 0% | 0.9554 |
| VO2peak | ||||||
| Age: 18−45 years | 20 | SMD = 0.28 | 0.1 to 0.46 | 0.0025 | 9% | 0.3316 |
| Age: 45−60 years | 7 | SMD = −0.08 | −0.36 to 0.21 | 0.5956 | 0% | 0.8155 |
| Complications: obesity | 18 | SMD = 0.16 | −0.04 to 0.35 | 0.1084 | 11% | 0.3231 |
| Complications: other chronic disease | 7 | SMD = 0.12 | −0.23 to 0.46 | 0.5061 | 10% | 0.3521 |
| Duration: ≤6 weeks | 11 | SMD = 0.17 | −0.1 to 0.45 | 0.2271 | 22% | 0.23 |
| Duration: >6 weeks | 16 | SMD = 0.17 | −0.01 to 0.36 | 0.0703 | 4% | 0.4054 |
| Frequency: ≤3 times/week | 19 | SMD = 0.24 | 0.03 to 0.44 | 0.0219 | 18% | 0.2324 |
| Frequency: >3 times/week | 8 | SMD = 0.08 | −0.17 to 0.34 | 0.5196 | 0% | 0.5765 |
| HIIT interval: 1−3 min | 15 | SMD = 0.27 | 0.04 to 0.5 | 0.0228 | 24% | 0.1807 |
| HIIT interval: ≥3 min | 12 | SMD = 0.08 | −0.14 to 0.29 | 0.4981 | 0% | 0.702 |
| SBP (mmHg) | ||||||
| Age: 18−45 years | 11 | MD = 0.15 | −3.32 to 3.62 | 0.9327 | 40% | 0.0798 |
| Age: 45−60 years | 4 | MD = 1.47 | −2.31 to 5.25 | 0.4461 | 0% | 0.6178 |
| Complications: obesity | 8 | MD = −1.05 | −4.78 to 2.67 | 0.5804 | 38% | 0.1231 |
| Complications: other chronic disease | 6 | MD = 3.27 | −0.48 to 7.01 | 0.0873 | 0% | 0.4631 |
| Duration: ≤6 weeks | 5 | MD = 0.7 | −3.76 to 5.17 | 0.7585 | 0% | 0.9592 |
| Duration: >6 weeks | 10 | MD = 0.13 | −3.59 to 3.85 | 0.9447 | 50% | 0.0333 |
| Frequency: ≤3 times/week | 11 | MD = 0.15 | −3.45 to 3.75 | 0.9353 | 45% | 0.0513 |
| Frequency: >3 times/week | 4 | MD = 0.65 | −3.59 to 4.89 | 0.7645 | 0% | 0.9025 |
| HIIT interval: 1−3 min | 7 | MD = 1.88 | −1.25 to 5.01 | 0.2397 | 0% | 0.451 |
| HIIT interval: ≥3 min | 8 | MD = −0.74 | −4.82 to 3.34 | 0.721 | 41% | 0.1018 |
| DBP (mmHg) | ||||||
| Age: 18−45 years | 11 | MD = 0.58 | −1.22 to 2.39 | 0.5268 | 4% | 0.4041 |
| Age: 45−60 years | 4 | MD = 0.96 | −1.89 to 3.81 | 0.5105 | 23% | 0.2729 |
| Complications: obesity | 8 | MD = 0.36 | −1.39 to 2.11 | 0.6866 | 23% | 0.2421 |
| Complications: other chronic disease | 6 | MD = 1.64 | −1.17 to 4.45 | 0.2517 | 0% | 0.4985 |
| Duration: ≤6 weeks | 5 | MD = 0.67 | −2.53 to 3.87 | 0.683 | 0% | 0.5807 |
| Duration: >6 weeks | 10 | MD = 0.68 | −0.93 to 2.29 | 0.4048 | 21% | 0.2438 |
| Frequency: ≤3 times/week | 11 | MD = 0.74 | −1.15 to 2.64 | 0.4177 | 18% | 0.2699 |
| Frequency: >3 times/week | 4 | MD = 0.58 | −1.75 to 2.92 | 0.6244 | 0% | 0.55 |
| HIIT interval: 1−3 min | 7 | MD = 1.31 | −0.67 to 3.29 | 0.1956 | 0% | 0.584 |
| HIIT interval: ≥3 min | 8 | MD = −0.02 | −2.11 to 2.07 | 0.9853 | 21% | 0.2639 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Guo, Z.; Li, M.; Cai, J.; Gong, W.; Liu, Y.; Liu, Z. Effect of High-Intensity Interval Training vs. Moderate-Intensity Continuous Training on Fat Loss and Cardiorespiratory Fitness in the Young and Middle-Aged a Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2023, 20, 4741. https://doi.org/10.3390/ijerph20064741
Guo Z, Li M, Cai J, Gong W, Liu Y, Liu Z. Effect of High-Intensity Interval Training vs. Moderate-Intensity Continuous Training on Fat Loss and Cardiorespiratory Fitness in the Young and Middle-Aged a Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health. 2023; 20(6):4741. https://doi.org/10.3390/ijerph20064741
Chicago/Turabian StyleGuo, Zhicheng, Meng Li, Jianguang Cai, Weiqi Gong, Yin Liu, and Ze Liu. 2023. "Effect of High-Intensity Interval Training vs. Moderate-Intensity Continuous Training on Fat Loss and Cardiorespiratory Fitness in the Young and Middle-Aged a Systematic Review and Meta-Analysis" International Journal of Environmental Research and Public Health 20, no. 6: 4741. https://doi.org/10.3390/ijerph20064741
APA StyleGuo, Z., Li, M., Cai, J., Gong, W., Liu, Y., & Liu, Z. (2023). Effect of High-Intensity Interval Training vs. Moderate-Intensity Continuous Training on Fat Loss and Cardiorespiratory Fitness in the Young and Middle-Aged a Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health, 20(6), 4741. https://doi.org/10.3390/ijerph20064741






