Psychopathology, Protective Factors, and COVID-19 among Adolescents: A Structural Equation Model
Abstract
1. Introduction
2. Materials and Methods
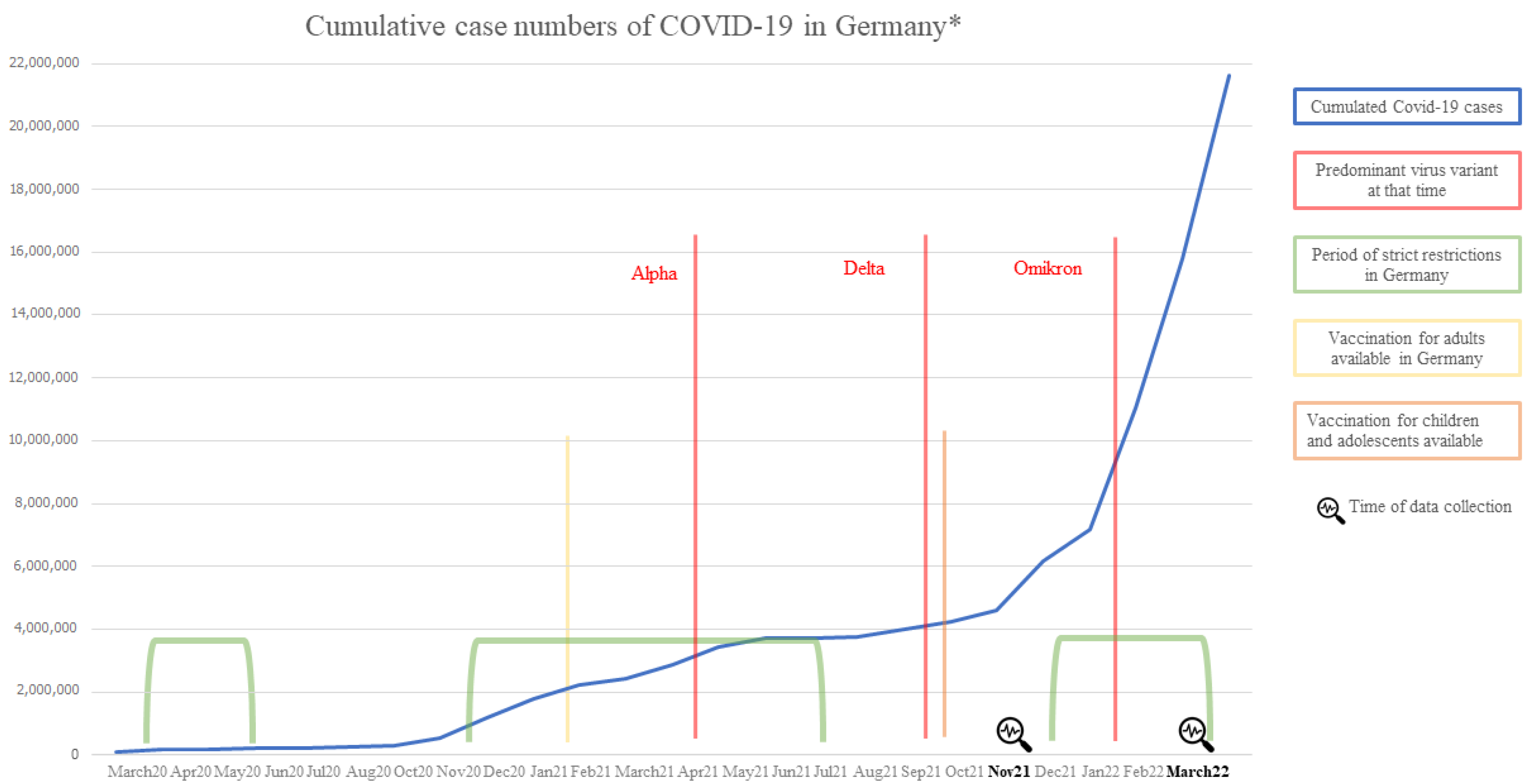
2.1. Participants & Procedure
2.2. Questionnaires
2.2.1. To Measure the First Latent Variable “Protective Factors”
2.2.2. To Measure the Second Latent Variable “Psychopathology”
2.2.3. To Measure the Third Latent Variable “Impact of COVID-19”
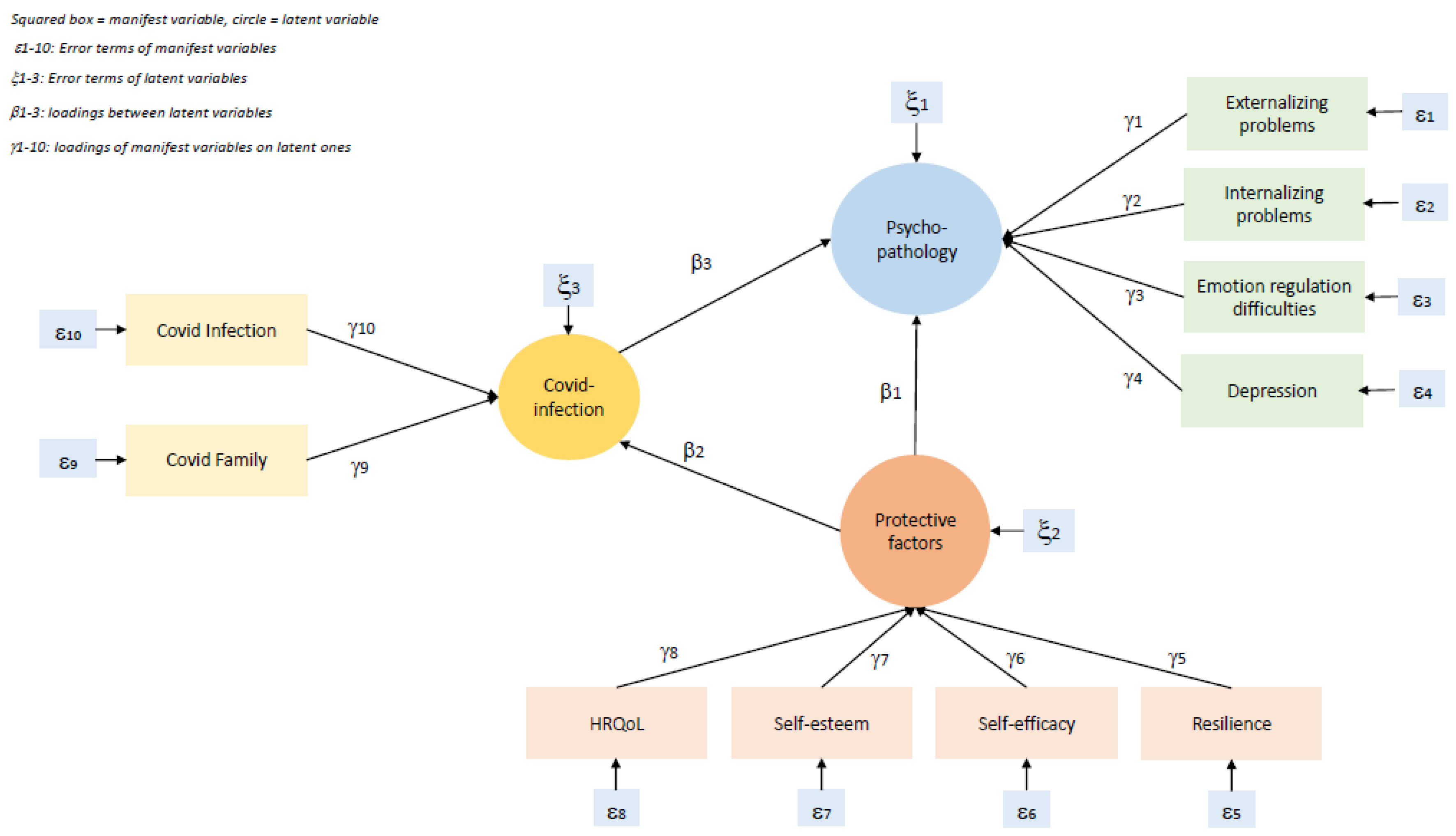
2.3. Statistical Analysis
2.4. Research Question and Hypotheses
2.5. Measures of Model Fit
3. Results
3.1. Sample Description
3.2. Correlation Matrix
3.3. SEM
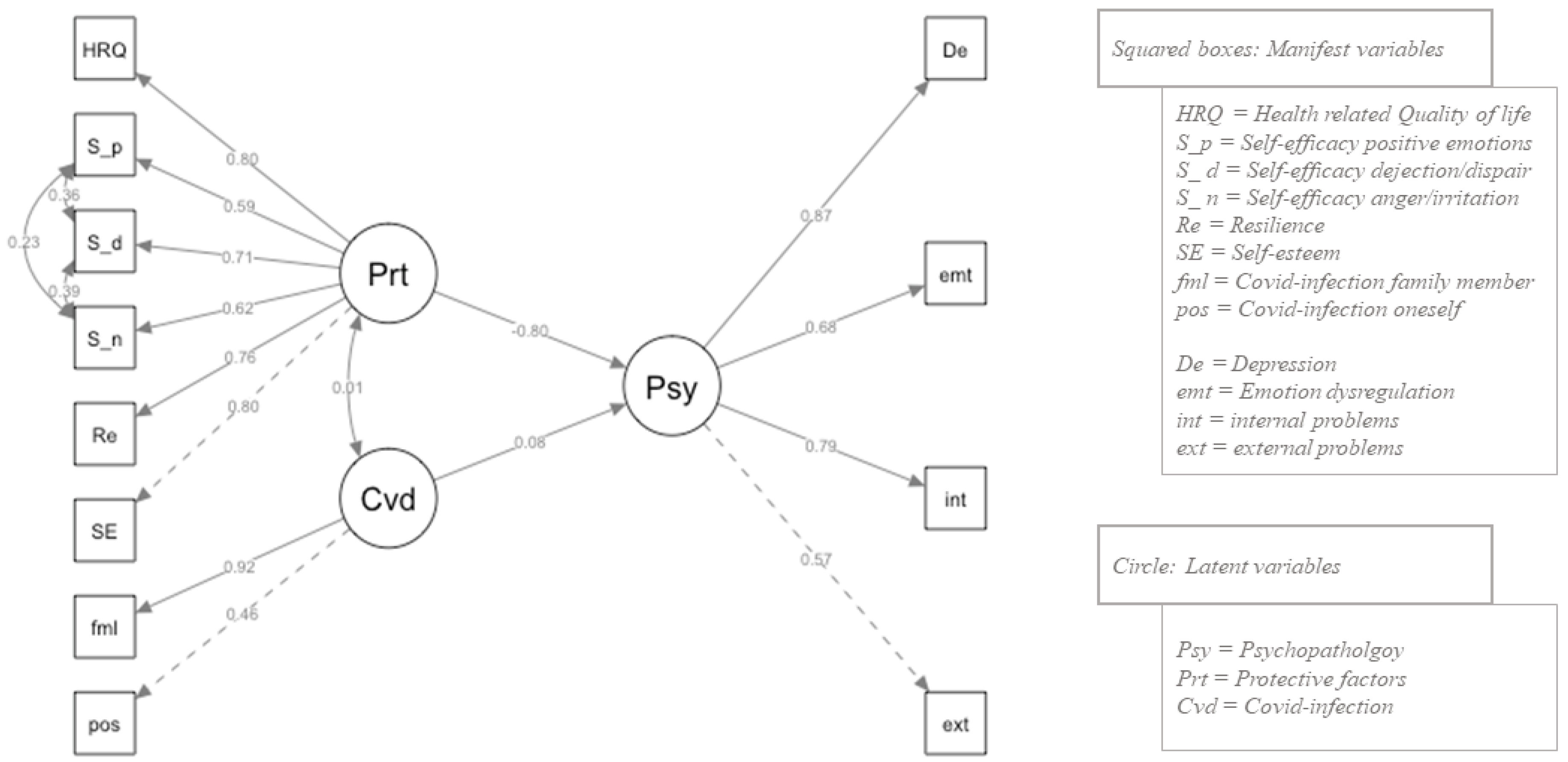
3.3.1. Final Model
3.3.2. Overall Effects
3.3.3. Loadings on Manifest Variables
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hawes, M.T.; Szenczy, A.K.; Klein, D.N.; Hajcak, G.; Nelson, B.D.L. Increases in depression and anxiety symptoms in adolescents and young adults during the COVID-19 pandemic. Psychol. Med. 2022, 52, 3222–3230. [Google Scholar] [CrossRef] [PubMed]
- Schilling, J.; Tolksdorf, K.; Marquis, A.; Faber, M.; Pfoch, T.; Buda, S.; Haas, W.; Schuler, E.; Altmann, D.; Grote; et al. Die verschiedenen Phasen der COVID-19-Pandemie in Deutschland: Eine deskriptive analyse von Januar 2020 bis Februar 2021. Bundesgesundheitsblatt-Gesundh.-Gesundh. 2021, 64, 1093–1106. [Google Scholar] [CrossRef] [PubMed]
- Octavius, G.S.; Silviani, F.R.; Lesmandjaja, A.; Angelina; Juliansen, A. Impact of COVID-19 on adolescents’ mental health: A systematic review. Middle East Curr. Psychiatry 2020, 27, 72. [Google Scholar]
- WHO Health Emergency Dashboard. Globally Confirmed Cases of COVID-19. 2022. Available online: https://covid19.who.int (accessed on 1 July 2022).
- Janssens, U.; Kluge, S.; Marx, G.; Hermes, C.; Salzberger, B.; Karagiannidis, C. Einstellung zur Impfung gegen SARS-CoV-2. Med. Klin.-Intensivmed. Notf. 2021, 116, 421–430. [Google Scholar] [CrossRef]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef] [PubMed]
- Cullen, W.; Gulati, G.; Kelly, B. Mental health in the COVID-19 pandemic. QJM Int. J. Med. 2020, 113, 311–312. [Google Scholar] [CrossRef]
- Pfefferbaum, B.; North, C. Mental health and the COVID-19 pandemic. N. Engl. J. Med. 2020, 383, 510–512. [Google Scholar] [CrossRef] [PubMed]
- Fegert, J.M.; Vitiello, B.; Plener, P.L.; Clemens, V. Challenges and burden of the Coronavirus 2019 (COVID-19) pandemic for child and adolescent mental health: A narrative review to highlight clinical and research needs in the acute phase and the long return to normality. Child Adolesc. Psychiatry Ment. Health 2020, 14, 20. [Google Scholar] [CrossRef]
- Loades, M.E.; Chatburn, E.; Higson-Seeney, N.; Reynolds, S.; Shafran, R.; Brigden, A.; Linney, C.; McManus, M.N.; Borwick, C.; Crawley, E. Rapid systematic review: The impact of social isolation and loneliness on the mental health of children and adolescents in the context of COVID-19. J. Am. Acad. Child Adolesc. Psychiatry 2020, 59, 1218–1239. [Google Scholar] [CrossRef] [PubMed]
- Deighton, J.; Lereya, S.T.; Casey, P.; Patalay, P.; Humphrey, N.; Wolpert, M. Prevalence of mental health problems in schools: Poverty and other risk factors among 28 000 adolescents in England. Br. J. Psychiatry 2019, 215, 565–567. [Google Scholar] [CrossRef]
- Panchal, U.; Salazar de Pbalo, G.; Franco, M.; Moreno, C.; Parellada, M.; Arango, C.; Fusar-Poli, P. The impact of COVID-19 lockdown on child and adolescent mental health: Systematic review. Eur. Child Adolesc. Psychiatry 2021, 1–27. [Google Scholar] [CrossRef] [PubMed]
- Weissman, D.G.; Rodman, A.M.; Rosen, M.L.; Kasparek, S.; Mayes, M.; Sheridan, M.A.; Lengua, L.J.; Meltzoff, A.N.; McLaughlin, K.A. Contributions of emotion regulation and brain structure and function to adolescent internalizing problems and stress vulnerability during the COVID-19 pandemic: A longitudinal study. Biol. Psychiatry Glob. Open Sci. 2021, 1, 272–282. [Google Scholar] [CrossRef] [PubMed]
- Rodman, A.M.; Rosen, M.L.; Kasparek, S.W.; Mayes, M.; Lengua, L.; McLaughlin, K.A.; Meltzoff, A.N. Social behavior and youth psychopathology during the COVID-19 pandemic: A longitudinal study. PsyArXiv 2022. [Google Scholar] [CrossRef]
- Bernasco, E.L.; Nelemans, S.A.; Graff, J.; Branje, S. Friend support and internalizing symptoms in early adolescence during COVID-19. J. Res. Adolesc. 2021, 31, 692–702. [Google Scholar]
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; Ho, C.S.; Ho, R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health 2020, 17, 1729. [Google Scholar] [CrossRef]
- Hawke, L.D.; Barbic, S.P.; Voineskos, A.; Szatmari, P.; Cleverley, K.; Hayes, E.; Relihan, J.; Dalex, M.; Courtney, D.; Cheung, A.; et al. Impacts of COVID-19 on Youth Mental Health, Substance Use, and Well-being: A Rapid Survey of Clinical and Community Samples. Can. J. Psychiatry 2020, 65, 701–709. [Google Scholar] [CrossRef]
- Chen, F.; Zheng, D.; Liu, J.; Gong, Y.; Guan, Z.; Lou, D. Depression and anxiety among adolescents during COVID-19: A cross-sectional study. Brain Behav. Immun. 2020, 88, 36–38. [Google Scholar] [CrossRef]
- Ellis, W.E.; Dumas, T.M.; Forbes, L.M. Physically isolated but socially connected: Psychological adjustment and stress among adolescents during the initial COVID-19 crisis. Can. J. Behav. Sci. 2020, 52, 177. [Google Scholar] [CrossRef]
- Magson, N.R.; Freeman, J.Y.; Rapee, R.M.; Richardson, C.E.; Oar, E.L.; Fardouly, J. Risk and protective factors for prospective changes in adolescent mental health during the COVID-19 pandemic. J. Youth Adolesc. 2021, 50, 44–57. [Google Scholar] [CrossRef]
- Chulia, A.T.; de la Barrera, U.; Mónaco, E.; Schoeps, K.; Castilla, I.M. Psychological impact of COVID-19 pandemic in Spanish adolescents: Risk and protective factors of emotional symptoms. Rev. De Psicol. Clínica Con Niños Y Adolesc. 2020, 7, 73–80. [Google Scholar]
- Snape, M.D.; Viner, R. COVID-19 in children and young people. Science 2020, 370, 286–288. [Google Scholar] [CrossRef]
- Waite, P.; Pearcey, S.; Shum, A.; Raw, J.A.L.; Patalay, P.; Creswell, C. How did the mental health symptoms of children and adolescents change over early lockdown during the COVID-19 pandemic in the UK? JCPP Adv. 2021, 1, e12009. [Google Scholar] [CrossRef] [PubMed]
- Ravens-Sieberer, U.; Kaman, A.; Erhart, M.; Devine, J.; Schlack, R.; Otto, C. Impact of the COVID-19 pandemic on quality of life and mental health in children and adolescents in Germany. Eur. Child Adolesc. Psychiatry 2022, 31, 879–889. [Google Scholar] [CrossRef] [PubMed]
- Rider, E.A.; Ansari, E.; Varrin, P.H.; Sparrow, J. Mental health and wellbeing of children and adolescents during the COVID-19 pandemic. BMJ 2021, 374. [Google Scholar] [CrossRef] [PubMed]
- Baumann, M. COVID-19 and mental health in children and adolescents: A diagnostic panel to map psycho-social consequences in the pandemic context. Discov. Ment. Health 2021, 1, 2. [Google Scholar] [CrossRef] [PubMed]
- Gruhn, M.A.; Compas, B.E. Effects of maltreatment on coping and emotion regulation in childhood and adolescence: A meta-analytic review. Child Abus. Negl. 2020, 103, 104446. [Google Scholar] [CrossRef] [PubMed]
- Compas, B.E.; Jaser, S.S.; Bettis, A.H.; Watson, K.H.; Gruhn, M.A.; Dunbar, J.P.; Williams, E.; Thigpen, J.C. Coping, emotion regulation, and psychopathology in childhood and adolescence: A meta-analysis and narrative review. Psychol. Bull. 2017, 143, 939. [Google Scholar] [CrossRef]
- Breaux, R.; Dvorsky, M.R.; Marsh, N.P.; Green, C.D.; Cash, A.R.; Shroff, D.M.; Buchen, N.; Langberg, J.M.; Becker, S.P. Prospective impact of COVID-19 on mental health functioning in adolescents with and without ADHD: Protective role of emotion regulation abilities. J. Child Psychol. Psychiatry 2021, 62, 1132–1139. [Google Scholar] [CrossRef] [PubMed]
- Ravens-Sieberer, U.; Erhart, M.; Devine, J.; Gilbert, M.; Reiss, F.; Barkmann, C.; Siegel, N.A.; Simon, A.M.; Hurrelmann, K.; Schlack, R.; et al. Child and Adolescent Mental Health During the COVID-19 Pandemic: Results of the Three-Wave Longitudinal COPSY Study. J. Adolesc. Health 2022, 71, 570–578. [Google Scholar] [CrossRef]
- Otto, C.; Haller, A.-C.; Klasen, F.; Hölling, H.; Bullinger, M.; Ravens-Sieberer, U. Risk and protective factors of health-related quality of life in children and adolescents: Results of the longitudinal BELLA study. PLoS ONE 2017, 12, e0190363. [Google Scholar] [CrossRef]
- Arima, M.; Takamija, Y.; Furuta, A.; Siriratsivawong, K.; Tsuchiya, S.; Izumi, M. Factors associated with the mental health status of medical students during the COVID-19 pandemic: A cross-sectional study in Japan. BMJ Open 2020, 10, e043728. [Google Scholar] [CrossRef]
- Rossi, A.; Panzeri, A.; Pietrabissa, G.M.; Manzoni, G.M.; Castelnuovo, G.; Mannarini, S. The anxiety-buffer hypothesis in the time of COVID-19: When self-esteem protects from the impact of loneliness and fear on anxiety and depression. Front. Psychol. 2020, 11, 2177. [Google Scholar] [CrossRef] [PubMed]
- Keith, T.Z. Multiple Regression and Beyond: An Introduction to Multiple Regression and Structural Equation Modeling, 3rd ed.; Routledge: Abingdon, UK, 2019. [Google Scholar] [CrossRef]
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 2009, 42, 377–381. [Google Scholar] [CrossRef]
- Buerger, A.; Emser, T.; Seidel, A.; Scheiner, C.; Schoenfeld, C.; Ruecker, V.; Heuschmann, P.U.; Romanos, R. DUDE—A universal prevention program for non-suicidal self-injurious behavior in adolescence based on effective emotion regulation: Study protocol of a cluster-randomized controlled trial. Trials 2022, 23, 97. [Google Scholar] [CrossRef]
- Ravens-Sieberer, U.; Auquier, P.; Erhart, M.; Gosch, A.; Rajmil, L.; Bruil, J.; Power, M.; Duer, W.; Cloetta, B.; Czemy, L.; et al. The KIDSCREEN-27 quality of life measure for children and adolescents: Psychometric results from a cross-cultural survey in 13 European countries. Qual. Life Res. 2007, 16, 1347–1356. [Google Scholar] [CrossRef] [PubMed]
- Ravens-Sieberer, U.; Erhart, M.; Rajmil, L.; Herdman, M.; Auquier, P.; Bruil, J.; Power, M.; Duer, W.; Abel, T.; Czemy, L.; et al. Reliability, construct and criterion validity of the KIDSCREEN-10 score: A short measure for children and adolescents’ well-being and health-related quality of life. Qual. Life Res. 2010, 19, 1487–1500. [Google Scholar] [CrossRef]
- Gunzenhauser, C.; Heikamp, T.; Gerbino, M.; Alessandri, G.; Suchodoletz, A.; Giunta, L.; Caprara, G.V.; Trommsdorff, G. Self-efficacy in regulating positive and negative emotions: A validation study in Germany. Eur. J. Psychol. Assess. 2013, 29, 197. [Google Scholar] [CrossRef]
- Caprara, G.V.; Di Giunta, L.; Eisenberg, N.; Gerbino, M.; Pastorelli, C.; Ramontano, C. Assessing regulatory emotional self-efficacy in three countries. Psychol. Assess. 2008, 20, 227. [Google Scholar] [CrossRef] [PubMed]
- Robins, R.W.; Trzesniewski, K.H.; Tracy, J.L.; Gosling, S.D.; Potter, J. Global self-esteem across the life span. Psychol. Aging 2002, 17, 423. [Google Scholar] [CrossRef]
- Wollny, A.I.; Jacobs, I. Validity and reliability of the German versions of the CD-RISC-10 and CD-RISC-2. Curr. Psychol. 2021, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Goodman, R. The Strengths and Difficulties Questionnaire: A research note. J. Child Psychol. Psychiatry 1997, 38, 581–586. [Google Scholar] [CrossRef]
- Ravens-Sieberer, U.; Herdman, M.; Devine, J.; Otto, C.; Bullinger, M.; Rose, M.; Klasen, F. The European KIDSCREEN approach to measure quality of life and well-being in children: Development, current application, and future advances. Qual. Life Res. 2014, 23, 791–803. [Google Scholar] [CrossRef] [PubMed]
- Essau, C.A.; Olaya, B.; Anastassiou-Hadjicharalambous, X.; Pauli, G.; Gilvarry, C.; Bray, D.; O’callaghan, J.; Ollendick, T.H. Psychometric properties of the Strength and Difficulties Questionnaire from five European countries: The Strength and Difficulties Questionnaire. Int. J. Methods Psychiatr. Res. 2012, 21, 232–245. [Google Scholar] [CrossRef] [PubMed]
- Richardson, L.P.; McCauley, E.; Grossman, D.C.; McCarty, C.A.; Richards, J.; Russo, J.E.; Rockhill, C.; Katon, W. Evaluation of the Patient Health Questionnaire-9 Item for detecting major depression among adolescents. Pediatrics 2010, 126, 1117–1123. [Google Scholar] [CrossRef]
- Bell, C.C. DSM-IV: Diagnostic and statistical manual of mental disorders. Jama 1994, 272, 828–829. [Google Scholar] [CrossRef]
- Ganguly, S.; Samanta, M.; Roy, P.; Chatterjee, S.; Kaplan, D.W.; Basu, B. Patient health questionnaire-9 as an effective tool for screening of depression among Indian adolescents. J. Adolesc. Health 2013, 52, 546–551. [Google Scholar] [CrossRef] [PubMed]
- Kaufman, E.A.; Xia, M.; Fosco, G.; Yaptangco, M.; Skidmore, C.R.; Crowell, S.E. The Difficulties in Emotion Regulation Scale Short Form (DERS-SF): Validation and replication in adolescent and adult samples. J. Psychopathol. Behav. Assess. 2016, 38, 443–455. [Google Scholar] [CrossRef]
- Gratz, K.L. Measurement of deliberate self-harm: Preliminary data on the Deliberate Self-Harm Inventory. J. Psychopathol. Behav. Assess. 2001, 23, 253–263. [Google Scholar] [CrossRef]
- Ehring, T.; Svaldi, J.; Tuschen-Caffier, B.; Berking, M. Validierung der Difficulties in Emotion Regulation Scale–deutsche Version (DERS-D); Unveröffentlichtes Manuskript; Universität Münster: Münster, Germany, 2013. [Google Scholar]
- Moreira, H.; Gouveia, M.; Canavarro, M. A bifactor analysis of the Difficulties in Emotion Regulation Scale-Short Form (DERS-SF) in a sample of adolescents and adults. Curr. Psychol. 2022, 41, 757–782. [Google Scholar] [CrossRef]
- Beierle, F.; Schobel, J.; Vogel, C.; Allgaier, J.; Mulansky, L.; Haug, F.; Haug, J.; Schlee, W.; Holfelder, M.; Stach, M.; et al. Corona Health. A Study- and Sensor-Based Mobile App Plattform Exploring Aspects of the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2021, 18, 10–3390. [Google Scholar] [CrossRef] [PubMed]
- Wolf, C.; Best, H. Handbuch der Sozialwissenschaftlichen Datenanalyse; Springer Wiesbaden; VS Verlag für Sozialwissenschaften: Wiesbaden, Germany, 2010; pp. 333–365. [Google Scholar]
- Bollen, K.A. Structural Equations with Latent Variables; John Wiley & Sons: Hoboken, NJ, USA, 1989; Volume 210. [Google Scholar]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2017; Available online: https://www.R-project.org/ (accessed on 1 February 2021).
- R Studio Team. RStudio: Integrated Development for R; RStudio Inc.: Boston, MA, USA, 2019; Available online: http://www.rstudio.com/ (accessed on 1 February 2021).
- Rosseel, Y. Lavaan: An R package for structural equation modeling. J. Stat. Softw. 2012, 48, 1–36. [Google Scholar] [CrossRef]
- Ciarrochi, J.; Parker, P.; Kashdan, T.B.; Heaven, P.C.L.; Barkus, E. Hope and emotional well-being: A six-year study to distinguish antecedents, correlates, and consequences. J. Posit. Psychol. 2015, 10, 520–532. [Google Scholar] [CrossRef]
- Weston, R.; Gore, P., Jr. A brief guide to structural equation modeling. Couns. Psychol. 2006, 34, 719–751. [Google Scholar] [CrossRef]
- Lee, S.-Y.; Xia, Y.-M. Maximum likelihood methods in treating outliers and symmetrically heavy-tailed distributions for nonlinear structural equation models with missing data. Psychometrika 2006, 71, 565–585. [Google Scholar] [CrossRef]
- Hu, L.t.; Bentler, P. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Model. A Multidiscip. J. 1999, 6, 1–55. [Google Scholar] [CrossRef]
- Bentler, P.M. Comparative fit indexes in structural models. Psychol. Bull. 1990, 107, 238. [Google Scholar] [CrossRef] [PubMed]
- Heene, M.; Hilbert, S.; Draxler, C.; Matthias, Z.; Bühner, M. Masking misfit in confirmatory factor analysis by increasing unique variances: A cautionary note on the usefulness of cutoff values of fit indices. Psychol. Methods 2011, 16, 319. [Google Scholar] [CrossRef]
- Orgilés, M.; Morales, A.; Delvecchio, E.; Mazzeschi, C.; Espada, J.P. Immediate psychological effects of the COVID-19 quarantine in youth from Italy and Spain. Front. Psychol. 2020, 11, 2986. [Google Scholar] [CrossRef]
- Wunsch, K.; Nigg, C.; Niessner, C.; Schmidt, S.C.E.; Oriwol, D.; Hanssen-Doose, A.; Burchartz, A.; Eichsteller, A.; Kolb, S.; Worth, A.; et al. The Impact of COVID-19 on the Interrelation of Physical Activity, Screen Time and Health-Related Quality of Life in Children and Adolescents in Germany: Results of the Motorik-Modul Study. Children 2021, 8, 98. [Google Scholar] [CrossRef]
- Racine, N.; McArthur, B.A.; Cooke, J.E.; Eirich, R.; Zhu, J.; Madigan, S. Global prevalence of depressive and anxiety symptoms in children and adolescents during COVID-19: A meta-analysis. JAMA Pediatr. 2021, 175, 1142–1150. [Google Scholar] [CrossRef] [PubMed]
- Panda, P.K.; Gupta, J.; Chowdhury, S.R.; Kumar, R.; Meena, A.K.; Madaan, P.; Sharawat, I.K.; Gulati, S.G. Psychological and behavioral impact of lockdown and quarantine measures for COVID-19 pandemic on children, adolescents and caregivers: A systematic review and meta-analysis. J. Trop. Pediatr. 2021, 67, fmaa122. [Google Scholar] [CrossRef]
- Felfe, C.; Saurer, J.; Schneider, P.; Vornberger, J.; Klotzbuecher, V.; Erhart, M.; Kaman, A.; Ravens-Sieberer, U. The youth mental health crisis during the COVID-19 pandemic: The role of school closures. Res. Sq. 2022. Preprint (Version 2). [Google Scholar] [CrossRef]
- Lee, J. Mental health effects of school closures during COVID-19. Lancet Child Adolesc. Health 2020, 4, 421. [Google Scholar] [CrossRef] [PubMed]
- Blanco, V.; Guisande, M.A.; Sánchez, M.T.; Otero, P.; Vázquez, F.L. Spanish validation of the 10-item Connor–Davidson Resilience Scale (CD-RISC 10) with nonprofessional caregivers. Aging Ment. Health 2019, 23, 183–188. [Google Scholar] [CrossRef] [PubMed]
- Dray, J.; Bowman, J.; Campbell, E.; Freund, M.; Wolfenden, L.; Hodder, R.K.; McElwaine, K.; Trmain, D.; Bartlem, K.; Bailey, J.; et al. Systematic review of universal resilience-focused interventions targeting child and adolescent mental health in the school setting. J. Am. Acad. Child Adolesc. Psychiatry 2017, 56, 813–824. [Google Scholar] [CrossRef]
- Williams, K.; Lisi, A.M.-D. Coping strategies in adolescents. J. Appl. Dev. Psychol. 1999, 20, 537–549. [Google Scholar] [CrossRef]
- Frydenberg, E.; Lewis, R. Adolescent coping: The different ways in which boys and girls cope. J. Adolesc. 1991, 14, 119–133. [Google Scholar] [CrossRef] [PubMed]
- Pedrini, L.; Meloni, S.; Lanfredi, M.; Ferrari, C.; Geviti, A.; Cattaneo, A.; Rossi, R. Adolescents’ mental health and maladaptive behaviors before the COVID-19 pandemic and 1-year after: Analysis of trajectories over time and associated factors. Child Adolesc. Psychiatry Ment. Health 2022, 16, 42. [Google Scholar] [CrossRef]
- Ye, Y.; Wang, C.; Zhu, Q.; He, M.; Havawala, M.; Bai, X.; Wang, T. Parenting and teacher–student relationship as protective factors for Chinese adolescent adjustment during COVID-19. Sch. Psychol. Rev. 2022, 51, 187–205. [Google Scholar] [CrossRef]
| Problem | Example |
|---|---|
| Separation, loss and grief | Separation from or loss of attachment figures due to COVID-19 illnesses, no normal way of grieving possible (e.g., ban on funerals). |
| Social determinants of health | Financial, housing, or food problems caused by the pandemic. |
| Social isolation, quarantine and loneliness | School closures, loss of contact with teachers, friends, peers, disrupted contact with potential support systems, domestic conflicts and violence, fewer recreational opportunities. |
| Physical, intellectual, and/or learning disability | Problems accessing appropriate therapies, closure of appropriate facilities. |
| Disrupted daily and school routines | Higher media use, less physical activity, change in sleep patterns. |
| Previous traumas | Pre-existing trauma caused by, e.g., caregivers (abuse, neglect). |
| Previous mental health | Pre-existing psychological impairments and problems in accessing appropriate forms of therapy. |
| M | SD | Range | ||
|---|---|---|---|---|
| HRQoL (KIDSCREEN-10) | 44.68 | 6.21 | 0–55 | |
| Self-efficacy (RESE-R) | positive emotions (S_p) | 4.31 | 0.82 | 0–5 |
| dejection/despair (S_d) | 3.65 | 0.97 | 0–5 | |
| anger/irritation (S_a) | 3.56 | 1.02 | 0–5 | |
| Self-esteem (SISE) | 2.57 | 0.87 | 0–4 | |
| Resilience (CD-RISC-10) | 24.70 | 6.95 | 0–40 | |
| Externalizing problems (SDQ) | 5.93 | 3.17 | 0–18 | |
| Internalizing problems (SDQ) | 5.24 | 3.28 | 0–19 | |
| Depression score (PHQ-9) | 4.75 | 4.49 | 0–27 | |
| Emotion dysregulation (DERS-SF) | 39.30 | 10.67 | 0–88 | |
| Yes | ||||
| COVID-19 | infection (pos) | 18.98% (n = 404) | ||
| inf. family (fml) | 46.83% (n = 997) | |||
| QoL | Self-Efficacy | SE | Re | Ex | In | De | Emt | COVID-19 | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| POS | DES | ANG | pos | fml | |||||||||
| HRQoL | 1 | ||||||||||||
| Self-efficacy | positive emotions | 0.45 ** | 1 | ||||||||||
| dejection/dispair | 0.50 ** | 0.63 ** | 1 | ||||||||||
| anger/irritation | 0.46 ** | 0.51 ** | 0.66 ** | 1 | |||||||||
| Self-esteem (SE) | 0.63 ** | 0.61 ** | 0.63 ** | 0.51 ** | 1 | ||||||||
| Resilience (Re) | 0.61 ** | 0.42 ** | 0.62 ** | 0.51 ** | 0.58 ** | 1 | |||||||
| External difficulties (ext) | −0.42 ** | −0.14 ** | −0.23 ** | −0.40 ** | −0.29 ** | −0.35 ** | 1 | ||||||
| Internal difficulties (int) | −0.60 ** | −0.33 ** | −0.44 ** | −0.37 ** | −0.50 ** | −0.53 ** | 0.41 ** | 1 | |||||
| Depression score (De) | −0.67 ** | −0.33 ** | −0.43 ** | −0.39 ** | −0.54 ** | −0.51 ** | 0.50 ** | 0.67 ** | 1 | ||||
| Emotion dysregulation (Emt) | −0.42 ** | −0.14 ** | −0.33 ** | −0.37 ** | −0.34 ** | −0.39 ** | 0.43 ** | 0.55 ** | 0.60 ** | 1 | |||
| COVID-19 | infection (pos) | −0.01 | 0.05 * | 0.05 * | 0.01 | 0.03 | 0.00 | 0.06 * | −0.02 | 0.03 | 0.02 | 1 | |
| inf. family (fml) | −0.04 | 0.07 ** | 0.04 * | 0.03 | 0.03 | −0.01 | 0.08 ** | 0.03 | 0.07 ** | 0.04 | 0.43 ** | 1 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Scheiner, C.; Seis, C.; Kleindienst, N.; Buerger, A. Psychopathology, Protective Factors, and COVID-19 among Adolescents: A Structural Equation Model. Int. J. Environ. Res. Public Health 2023, 20, 2493. https://doi.org/10.3390/ijerph20032493
Scheiner C, Seis C, Kleindienst N, Buerger A. Psychopathology, Protective Factors, and COVID-19 among Adolescents: A Structural Equation Model. International Journal of Environmental Research and Public Health. 2023; 20(3):2493. https://doi.org/10.3390/ijerph20032493
Chicago/Turabian StyleScheiner, Christin, Christian Seis, Nikolaus Kleindienst, and Arne Buerger. 2023. "Psychopathology, Protective Factors, and COVID-19 among Adolescents: A Structural Equation Model" International Journal of Environmental Research and Public Health 20, no. 3: 2493. https://doi.org/10.3390/ijerph20032493
APA StyleScheiner, C., Seis, C., Kleindienst, N., & Buerger, A. (2023). Psychopathology, Protective Factors, and COVID-19 among Adolescents: A Structural Equation Model. International Journal of Environmental Research and Public Health, 20(3), 2493. https://doi.org/10.3390/ijerph20032493







