SARS-CoV-2 and Adolescent Psychiatric Emergencies at the Tübingen University Hospital: Analyzing Trends, Diagnoses, and Contributing Factors
Abstract
1. Introduction
1.1. The SARS-CoV-2 Pandemic as a Social-Emotional Crisis for Children and Adolescents
1.2. Child and Adolescent Psychiatric Emergencies
1.3. Developmental Areas of Children and Adolescents and Mental Illness
- How did the number of emergency presentations, including outpatient emergency visits, inpatient emergency admissions, and telephone consultations, change between Restriction Phase 1 (October 2020–January 2021), Restriction Phase 2, and the endemic phase? We hypothesized that the numbers would increase in all categories over the time periods;
- How did the age of the patients change in the time between Restriction Phase 1, Restriction Phase 2, and the endemic phase? We hypothesized that there would be a shift toward more older adolescents;
- How did the respective number of patients with the following diagnoses change in the time period between Restriction Phase 1, Restriction Phase 2, and endemic phase?
- 3a.
- Eating disorders;
- 3b.
- Obsessive–compulsive disorders.
- 3c.
- Affective disorders;
- 3d.
- Expansive disorders;
- 3e.
- Anxiety disorders;
- 3f.
- Mental and behavioral disorders due to substance abuse over time;
- 3g.
- Psychoses.
2. Materials and Methods
2.1. Mixed-Methods Approach
2.1.1. Data Collection
2.1.2. Sample
2.1.3. Survey Period
2.2. Quantitative Data Analysis
2.2.1. Measurement Instruments
2.2.2. Evaluation of the Data
2.3. Qualitative Data Analysis
2.3.1. Measurement Instruments
2.3.2. Analysis of the Data
3. Results
3.1. Quantitative Results
3.1.1. Differences in the Number of Emergency Presentations over Time
| Kind of Emergency Presentation | Time Period | N Total and by Age Group a | Mean Age Differences between the Groups | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| All | ≤12.99 Years | 13.00–15.99 Years | ≥16.00 Years | χ2(2) | p | M | SD | Min | Max | F | df | p | c η2 | ||
| All | 2019/2020 | 246 | 66 (27%) | 93 (38%) | 87 (35%) | 37.48 | <0.001 * | 14.32 | 2.70 | 7.12 | 18.32 | 15.02 | 1540 | <0.001 * | <0.01 |
| 2020/2021 | 319 | 48 (15%) | 153 (48%) | 118 (37%) | 14.99 | 2.03 | 6.67 | 18.00 | |||||||
| 2021/2022 | 485 b | 57 (12%) | 249 (51%) | 178 (37%) | 15.06 | 2.07 | 6.90 | 18.21 | |||||||
| 2022/2023 | 493 | 67 (14%) | 214 (43%) | 212 (43%) | 15.10 | 2.41 | 4.71 | 18.65 | |||||||
| Telephone | 2019/2020 | 126 | 43 (34%) | 39 (31%) | 44 (35%) | 28.82 | <0.001 * | 14.06 | 2.97 | 7.12 | 18.32 | 8.71 | 802 | 0.005 * | 0.01 |
| 2020/2021 | 163 | 29 (18%) | 80 (49%) | 54 (33%) | 14.78 | 2.17 | 6.67 | 17.99 | |||||||
| 2021/2022 | 257 b | 38 (15%) | 126 (49%) | 92 (36%) | 14.95 | 2.18 | 6.90 | 18.21 | |||||||
| 2022/2023 | 259 | 41 (16%) | 111 (43%) | 107 (41%) | 14.93 | 2.65 | 4.71 | 18.65 | |||||||
| Outpatient | 2019/2020 | 48 | 15 (31%) | 19 (40%) | 14 (29%) | 11.21 | 0.082 | 13.83 | 2.91 | 7.15 | 17.83 | 1.84 | 309 | 0.020 * | <0.01 |
| 2020/2021 | 64 | 8 (13%) | 27 (42%) | 29 (45%) | 15.23 | 1.89 | 9.39 | 17.99 | |||||||
| 2021/2022 | 104 | 13 (12%) | 53(51%) | 38 (37%) | 14.84 | 2.22 | 8.63 | 17.99 | |||||||
| 2022/2023 | 95 | 17 (18%) | 40 (42%) | 38 (40%) | 14.77 | 2.49 | 6.22 | 17.84 | |||||||
| Admission | 2019/2020 | 72 | 8 (11%) | 35 (49%) | 29 (40%) | 8.30 | 0.217 | 15.10 | 1.77 | 9.68 | 17.84 | 6.35 | 425 | 0.090 | 0.01 |
| 2020/2021 | 92 | 11 (12%) | 46 (50%) | 35 (38%) | 15.20 | 1.83 | 9.92 | 18.00 | |||||||
| 2021/2022 | 124 | 6 (5%) | 70 (56%) | 48 (39%) | 15.49 | 1.60 | 10.54 | 18.00 | |||||||
| 2022/2023 | 139 | 9 (7%) | 63 (45%) | 67 (48%) | 16.64 | 1.73 | 6.22 | 18.01 | |||||||
3.1.2. Differences in Patients’ Ages in Emergency Presentations over Time
3.1.3. Differences in the Number of EDs over Time
3.1.4. Differences in the Number of OCDs over Time
3.1.5. Differences in the Number of Affective Disorders over Time
3.1.6. Differences in the Number of Expansive Disorders over Time
3.1.7. Differences in the Number of Anxiety Disorders over Time
3.1.8. Differences in the Number of Mental and Behavioral Disorders Due to Substance Abuse over Time
3.1.9. Differences in the Number of Psychoses over Time
3.2. Qualitative Results
- (1)
- Specific reasons for presentation—The reason for the presentation consisted of the acute and usually specific cause of a child’s or adolescent’s emergency outpatient emergency visit or inpatient emergency admission;
- (2)
- Stressors—Stress factors consisted of burdens, issues, situations, circumstances, events, or conditions described by the patient themselves or a significant other. Such stressors were reported beyond the specific reason for presentation or admission. Upon closer examination of the described stressors and considering the existing literature [46], the stressors were divided into subcategories, specifically describing social contexts that represent the developmental areas of children and adolescents. It became evident that further differentiation into various life domains was possible. The categories that emerged as meaningful were school, peers, family, and self. We confirmed that the stress factors could be assigned to different life contexts in which the development of children and adolescents takes place:
- (a)
- School—Social context within the learning environment where children and adolescents spend a significant portion of their daily lives;
- (b)
- Peers—Social context with flexible conditions, within which children and adolescents move to varying extents, but which play a significant role in their development. Peers typically refer to individuals of the same age with whom individuals have relationships;
- (c)
- Family—Social context in which children and adolescents grow up and must navigate through in their daily lives. Various relationship groups exist, with a focus on the central living place of children and adolescents;
- (d)
- Self—Biographical experiences, topics, and symptom areas that are individually described by the patient and caregivers as a current stress factor [59] and not directly related to a social context (a–c).
- (3)
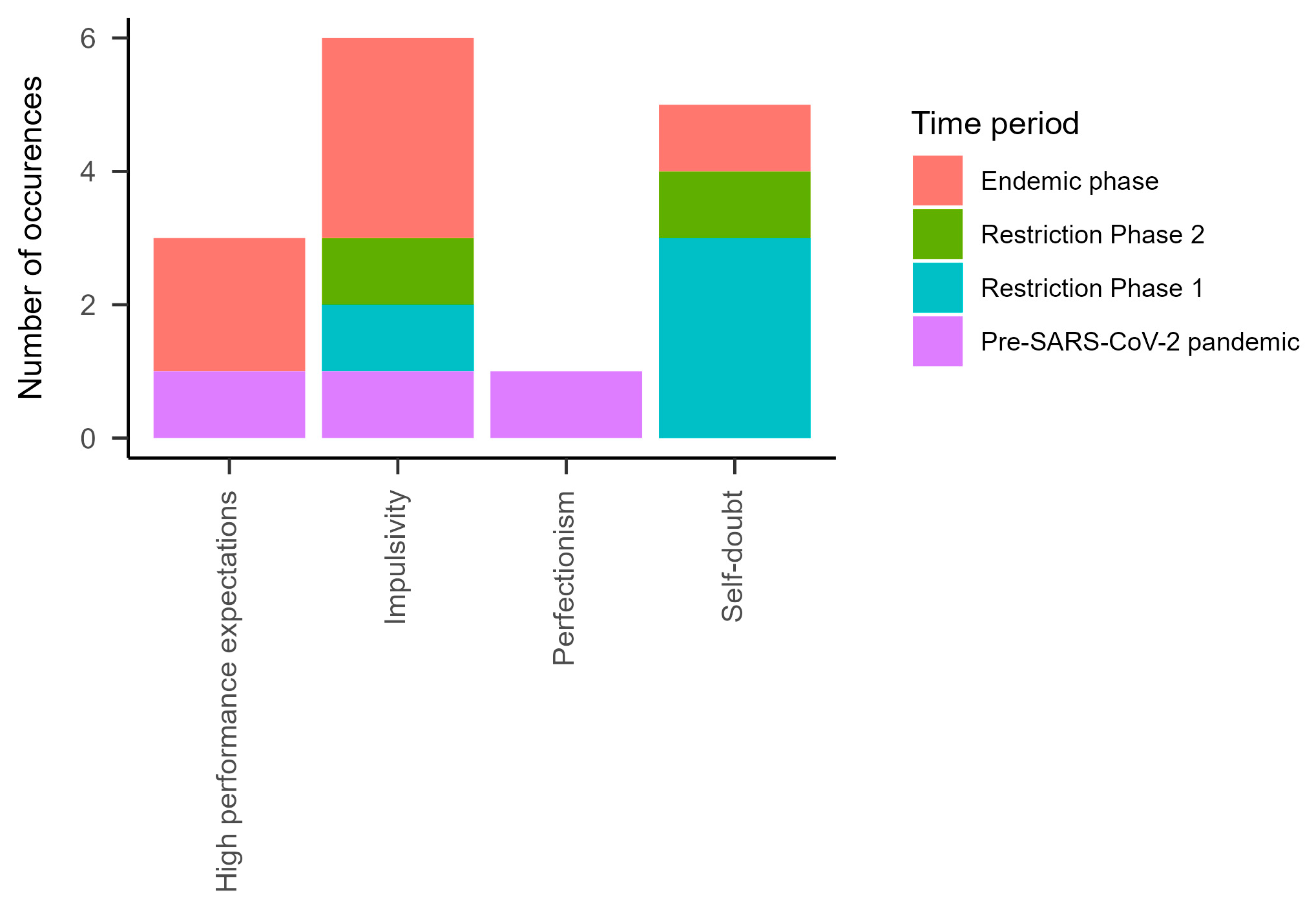
- Personality characteristics—Other than patient’s biographical experience or symptoms, this category includes the patient’s personality. Personality characteristics, by definition, represent relatively stable characteristics of individuals. They persist over time and in situations and generally have an influence on experiences and behavior [59,60].
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Widnall, E.; Adams, E.A.; Plackett, R.; Winstone, L.; Haworth, C.M.A.; Mars, B.; Kidger, J. Adolescent experiences of the COVID-19 pandemic and school closures and implications for mental health, peer relationships and learning: A qualitative study in south-west England. Int. J. Environ. Res. Public Health 2022, 19, 7163. [Google Scholar] [CrossRef]
- Fountoulakis, K.N.; Karakatsoulis, G.; Abraham, S.; Adorjan, K.; Ahmed, H.U.; Alarcón, R.D.; Arai, K.; Auwal, S.S.; Berk, M.; Bjedov, S.; et al. Results of the COVID-19 mental health international for the general population (COMET-G) study. Eur. Neuropsychopharmacol. 2022, 54, 21–40. [Google Scholar] [CrossRef] [PubMed]
- Samji, H.; Wu, J.; Ladak, A.; Vossen, C.; Stewart, E.; Dove, N.; Long, D.; Snell, G. Review: Mental health impacts of the COVID-19 pandemic on children and youth—A systematic review. Child Adolesc. Ment. Health 2022, 27, 173–189. [Google Scholar] [CrossRef]
- Walker, S.; Barnett, P.; Srinivasan, R.; Abrol, E.; Johnson, S. Clinical and social factors associated with involuntary psychiatric hospitalisation in children and adolescents: A systematic review, meta-analysis, and narrative synthesis. Lancet Child Adolesc. Health 2021, 5, 501–512. [Google Scholar] [CrossRef]
- Sudarsanan, S.; Chaudhury, S.; Pawar, A.A.; Salujha, S.K.; Srivastava, K. Psychiatric emergencies. Med. J. Armed Forces India 2004, 60, 59–62. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Hagmann, D.; Allgaier, K.; Wolf, J.; Chiumento, O.; Bürkle, L.; Conzelmann, A.; Renner, T.J. Entwicklung der Charakteristika von Notaufnahmen in der Kinder-und Jugendpsychiatrie. Z. Kinder Jugendpsychiatr. Psychother. 2022, 50, 286–297. [Google Scholar] [CrossRef] [PubMed]
- Allgaier, K.; Schneider, P.S.; Buck, S.; Reusch, P.A.; Hagmann, D.; Barth, G.M.; Renner, T.J. Kinder-und jugendpsychiatrische Notfälle während der zweiten Welle der SARS-CoV2-19-Pandemie. Z. Kinder Jugendpsychiatr. Psychother. 2022, 50, 275–285. [Google Scholar] [CrossRef] [PubMed]
- Panchal, U.; de Pablo, G.S.; Franco, M.; Moreno, C.; Parellada, M.; Arango, C.; Fusar-Poli, P. The impact of COVID-19 lockdown on child and adolescent mental health: Systematic review. Eur. Child Adolesc. Psychiatry 2023, 32, 1151–1177. [Google Scholar] [CrossRef] [PubMed]
- Wong, B.H.C.; Cross, S.; Zavaleta-Ramírez, P.; Bauda, I.; Hoffman, P.; Ibeziako, P.; Nussbaum, L.; Berger, G.E.; Hassanian-Moghaddam, H.; Kapornai, K.; et al. Self-harm in children and adolescents who presented at emergency units during the COVID-19 pandemic: An international retrospective cohort study. J. Am. Acad. Child Adolesc. Psychiatry 2023, 62, 998–1009. [Google Scholar] [CrossRef]
- Brakemeier, E.L.; Wirkner, J.; Knaevelsrud, C.; Wurm, S.; Christiansen, H.; Lueken, U.; Schneider, S. Die COVID-19-Pandemie als Herausforderung für die psychische Gesundheit. Z. Klin. Psychol. Psychother. 2020, 49, 1–31. [Google Scholar] [CrossRef]
- Fegert, J.M.; Vitiello, B.; Plener, P.L.; Clemens, V. Challenges and burden of the Coronavirus 2019 (COVID-19) pandemic for child and adolescent mental health: A narrative review to highlight clinical and research needs in the acute phase and the long return to normality. Child Adolesc. Psychiatry Ment. Health 2020, 14, 1–11. [Google Scholar] [CrossRef]
- Lăzăroiu, G.; Horak, J.; Valaskova, K. Scaring ourselves to death in the time of COVID-19: Pandemic awareness, virus anxiety, and contagious fear. Linguist. Philos. Investig. 2020, 19, 114–120. [Google Scholar] [CrossRef]
- Corona-Rückblick 2022, 2021 und 2020. Available online: https://www.gew-bw.de/aktuelles/detailseite/corona-rueckblick-2020 (accessed on 28 November 2023).
- Laczkovics, C.; Lozar, A.; Bock, M.M.; Reichmann, A.; Pfeffer, B.; Bauda, I.; Goreis, A.; Kothgassner, O. Psychische Gesundheit und Social Media-Nutzungsverhalten von Jugendlichen und jungen Erwachsenen während der COVID-19-Pandemie. Prax. Kinderpsychol. Kinderpsychiatr. 2023, 72, 591–604. [Google Scholar] [CrossRef] [PubMed]
- Tri Sakti, A.M.; Mohd Ajis, S.Z.; Azlan, A.A.; Kim, H.J.; Wong, E.; Mohamad, E. Impact of COVID-19 on school populations and associated factors: A systematic review. Int. J. Environ. Res. Public Health 2022, 19, 4024. [Google Scholar] [CrossRef] [PubMed]
- Vidal, C.; Hinson, L.; Bartolini, E. School Absenteeism and the COVID-19 Pandemic: The Role of Pediatricians. Clin. Pediatr. 2023, 63, 5–9. [Google Scholar] [CrossRef]
- Ruth, U.; Freisleder, F.J.; Heinrich, H. Outpatient emergency admissions to a child and adolescent psychiatry hospital, and following immediate hospitalization. Ger. J. Psychiatry 2013, 16, 1–6. [Google Scholar]
- Franzen, M.; Keller, F.; Brown, R.C.; Plener, P.L. Emergency presentations to child and adolescent psychiatry: Nonsuicidal self-injury and suicidality. Front. Psychiatry 2020, 10, 979. [Google Scholar] [CrossRef]
- Ougrin, D. Debate: Emergency mental health presentations of young people during the COVID-19 lockdown. Child Adolesc. Ment. Health 2020, 25, 171–172. [Google Scholar] [CrossRef] [PubMed]
- Eichinger, T.; Marte, E.; Thun-Hohenstein, L.; Santner, F.; Plattner, B. Akutversorgung psychisch kranker Kinder und Jugendlicher: Eine Pilotstudie an 257 PatientInnen. Neuropsychiatrie 2021, 35, 199–205. [Google Scholar] [CrossRef]
- Lauwerie, L.; Sibut, R.; Maillet-Vioud, C.; Monteiro, S.; Alauze, F.; Martinez, E.; Sauniere, D.; Legrand-Vyskoc, A.; Lachal, J. A retrospective cohort study comparing the social, familial and clinical characteristics of adolescents admitted to a French emergency department in suicidal crisis before and during the COVID-19 pandemic. Psychiatry Res. 2023, 321, 115080. [Google Scholar] [CrossRef]
- Victor, S.; Thorup, A.A.E. Demographic trends in a paediatric psychiatric emergency room in Copenhagen. Dan. Med. J. 2021, 68, A10200785. [Google Scholar] [PubMed]
- Fegert, J.M.; Kölch, M.; Krüger, U. Versorgung Psychisch Kranker Kinder und Jugendlicher in Deutschland—Bestandsaufnahme und Bedarfsanalyse. Available online: https://www.apk-ev.de/fileadmin/downloads/Abschlussbericht_Versorgung_psychisch_kranke_Kinder_u_Jugendliche.pdf (accessed on 24 January 2024).
- Burchard, F.; Diebenbusch, T. Krisenintervention in einer Versorgungsklinik für Kinder-und Jugendpsychiatrie. Prax. Kinderpsychol. Kinderpsychiatr. 2017, 66, 5–25. [Google Scholar] [CrossRef]
- Gandhi, S.; Chiu, M.; Lam, K.; Cairney, J.C.; Guttmann, A.; Kurdyak, P. Mental health service use among children and youth in Ontario: Population-based trends over time. Can. J. Psychiatry 2016, 61, 119–124. [Google Scholar] [CrossRef] [PubMed]
- Sheridan, D.C.; Spiro, D.M.; Fu, R.; Johnson, K.P.; Sheridan, J.S.; Oue, A.A.; Wang, W.; Van Nes, R.; Hansen, M.L. Mental health utilization in a pediatric emergency department. Pediatr. Emerg. Care 2015, 31, 555–559. [Google Scholar] [CrossRef] [PubMed]
- Sevecke, K.; Wenter, A.; Schickl, M.; Kranz, M.; Krstic, N.; Fuchs, M. Stationäre Versorgungskapazitäten in der Kinder-und Jugendpsychiatrie–Zunahme der Akutaufnahmen während der COVID-19 Pandemie? Neuropsychiatrie 2023, 37, 12–21. [Google Scholar] [CrossRef] [PubMed]
- Holtmann, M.; Lehmkuhl, G.; Plener, P.; Kölch, M. Die COVID-19-Pandemie und seelische Gesundheit bei Minderjährigen: Herausforderungen für die Kinder- und Jugendpsychiatrie und -psychotherapie. Z. Kinder Jugendpsychiatr. Psychother. 2023, 51, 1–7. [Google Scholar] [CrossRef]
- Taastrøm, A.; Klahn, J.; Staal, N.; Thomsen, P.H.; Johansen, A. Children and adolescents in the Psychiatric Emergency Department: A 10-year survey in Copenhagen County. Nord. J. Psychiatry 2014, 68, 385–390. [Google Scholar] [CrossRef]
- Milliren, C.E.; Richmond, T.K.; Hudgins, J.D. Emergency Department Visits and Hospitalizations for Eating Disorders During the COVID-19 Pandemic. Pediatrics 2023, 151, e2022058198. [Google Scholar] [CrossRef]
- Linde, E.S.; Varga, T.V.; Clotworthy, A. Obsessive-compulsive disorder during the COVID-19 pandemic—A systematic review. Front. Psychiatry 2022, 13, 806872. [Google Scholar] [CrossRef]
- Zaccari, V.; D’Arienzo, M.C.; Caiazzo, T.; Magno, A.; Amico, G.; Mancini, F. Narrative review of COVID-19 impact on obsessive-compulsive disorder in child, adolescent and adult clinical populations. Front. Psychiatry 2021, 12, 673161. [Google Scholar] [CrossRef]
- Davico, C.; Marcotulli, D.; Lux, C.; Calderoni, D.; Cammisa, L.; Bondone, C.; Rosa-Brusin, M.; Secci, I.; Porro, M.; Campanile, R.; et al. Impact of the COVID-19 pandemic on child and adolescent psychiatric emergencies. J. Clin. Psychiatry 2021, 82, 31960. [Google Scholar] [CrossRef]
- Ferro, V.; Averna, R.; Murciano, M.; Raucci, U.; Cristaldi, S.; Musolino, A.M.C.; Pontillo, M.; Della Vecchia, N.; Labonia, M.; Pisani, M.; et al. Has Anything Changed in the Frequency of Emergency Department Visits and the Profile of the Adolescent Seeking Emergency Mental Care during the COVID-19 Pandemic? Children 2023, 10, 578. [Google Scholar] [CrossRef]
- Shankar, L.G.; Habich, M.; Rosenman, M.; Arzu, J.; Lales, G.; Hoffmann, J.A. Mental health emergency department visits by children before and during the COVID-19 pandemic. Acad. Pediatr. 2022, 22, 1127–1132. [Google Scholar] [CrossRef]
- Loades, M.E.; Chatburn, E.; Higson-Sweeney, N.; Reynolds, S.; Shafran, R.; Brigden, A.; Linney, C.; McManus, M.N.; Borwick, C.; Crawley, E. Rapid systematic review: The impact of social isolation and loneliness on the mental health of children and adolescents in the context of COVID-19. J. Am. Acad. Child Adolesc. Psychiatry 2020, 59, 1218–1239. [Google Scholar] [CrossRef] [PubMed]
- Ma, L.; Mazidi, M.; Li, K.; Li, Y.; Chen, S.; Kirwan, R.; Zhou, H.; Yan, N.; Rahman, A.; Wang, W.; et al. Prevalence of mental health problems among children and adolescents during the COVID-19 pandemic: A systematic review and meta-analysis. J. Affect. Disord. 2021, 293, 78–89. [Google Scholar] [CrossRef] [PubMed]
- Dragovic, M.; Pascu, V.; Hall, T.; Ingram, J.; Waters, F. Emergency department mental health presentations before and during the COVID-19 outbreak in Western Australia. Australas. Psychiatry 2020, 28, 627–631. [Google Scholar] [CrossRef]
- Chadi, N.; Spinoso-Di Piano, C.; Osmanlliu, E.; Gravel, J.; Drouin, O. Mental Health–related emergency department visits in adolescents before and during the COVID-19 pandemic: A multicentric retrospective study. J. Adolesc. Health 2021, 69, 847–850. [Google Scholar] [CrossRef] [PubMed]
- Ferrando, S.J.; Klepacz, L.; Lynch, S.; Shahar, S.; Dornbush, R.; Smiley, A.; Miller, I.; Tavakkoli, M.; Regan, J.; Bartell, A. Psychiatric emergencies during the height of the COVID-19 pandemic in the suburban New York City area. J. Psychiatr. Res. 2021, 136, 552–559. [Google Scholar] [CrossRef] [PubMed]
- Steinhoff, A.; Bechtiger, L.; Ribeaud, D.; Eisner, M.; Shanahan, L. Stressful Life Events in Different Social Contexts Are Associated With Self-Injury From Early Adolescence to Early Adulthood. Front. Psychiatry 2020, 11, 487200. [Google Scholar] [CrossRef]
- Eschenbeck, H.; Knauf, R.K. Entwicklungsaufgaben und ihre Bewältigung. In Entwicklungspsychologie des Jugendalters; Lohaus, A., Ed.; Springer: Berlin/Heidelberg, Germany, 2018; pp. 23–50. [Google Scholar]
- Epstein, S.; Roberts, E.; Sedgwick, R.; Polling, C.; Finning, K.; Ford, T.; Dutta, R.; Downs, J. School absenteeism as a risk factor for self-harm and suicidal ideation in children and adolescents: A systematic review and meta-analysis. Eur. Child Adolesc. Psychiatry 2020, 29, 1175–1194. [Google Scholar] [CrossRef]
- Mattejat, F.; Simon, B.; König, U.; Quaschner, K.; Barchewitz, C.; Felbel, D.; Herpertz-Dahlmann, B.; Höhne, D.; Janthur, B.; Jungmann, J.; et al. Lebensqualität bei psychisch kranken Kindern und Jugendlichen. Ergebnisse der ersten multizentrischen Studie mit dem Inventar zur Erfassung der Lebensqualität bei Kindern und Jugendlichen (ILK) [Quality of life of children and adolescents with psychiatric disorders. Results of the 1st multicenter study with an inventory to assess the quality of life in children and adolescents]. Z. Kinder Jugendpsychiatr. Psychother. 2003, 31, 293–303. [Google Scholar] [CrossRef] [PubMed]
- Huebner, E.S.; Gilman, R. An introduction to the multidimensional students’ life satisfaction scale. Soc. Indic. Res. 2002, 60, 115–122. [Google Scholar] [CrossRef]
- Carballo, J.J.; Llorente, C.; Kehrmann, L.; Flamarique, I.; Zuddas, A.; Purper-Ouakil, D.; Hoekstra, P.J.; Coghill, D.; Schulze, U.M.E.; Dittmann, R.W.; et al. Psychosocial risk factors for suicidality in children and adolescents. Eur. Child Adolesc. Psychiatry 2020, 29, 759–776. [Google Scholar] [CrossRef] [PubMed]
- Devoe, D.J.; Han, A.; Anderson, A.; Katzman, D.K.; Patten, S.B.; Soumbasis, A.; Flanagan, J.; Paslakis, G.; Vyver, E.; Marcoux, G.; et al. The impact of the COVID-19 pandemic on eating disorders: A systematic review. Int. J. Eat. Disord. 2023, 56, 5–25. [Google Scholar] [CrossRef] [PubMed]
- Palinkas, L.A.; Horwitz, S.M.; Green, C.A.; Wisdom, J.P.; Duan, N.; Hoagwood, K. Purposeful sampling for qualitative data collection and analysis in mixed method implementation research. Adm. Policy Ment. Health 2015, 42, 533–544. [Google Scholar] [CrossRef]
- The R Project for Statistical Computing. Available online: https://www.r-project.org/ (accessed on 30 November 2023).
- Girden, E.R. ANOVA: Repeated Measures; Sage: Newcastle upon Tyne, UK, 1992. [Google Scholar]
- Pearson, K. On the criterion that a given system of deviations from the probable in the case of a correlated system of variables is such that it can be reasonably supposed to have arisen from random sampling. Lond. Edinb. Dublin Philos. Mag. J. Sci. 1990, 50, 157–175. [Google Scholar] [CrossRef]
- Fisher, R.A. Statistical Methods for Research Workers, 5th ed.; Oliver & Boyd: Edinburgh, UK, 1934. [Google Scholar]
- Hennink, M.; Kaiser, B.N. Sample sizes for saturation in qualitative research: A systematic review of empirical tests. Soc. Sci. Med. 2022, 292, 114523. [Google Scholar] [CrossRef]
- Saunders, B.; Sim, J.; Kingstone, T.; Baker, S.; Waterfield, J.; Bartlam, B.; Burroughs, H.; Jinks, C. Saturation in qualitative research: Exploring its conceptualization and operationalization. Qual. Quant. 2018, 52, 1893–1907. [Google Scholar] [CrossRef]
- Kukartz, U.; Rädiker, S. Qualitative Inhaltsanalyse: Methoden, Praxis, Computerunterstützung; Beltz Juventa: Weilheim, Germany, 2022. [Google Scholar]
- Kuckartz, U. Qualitative Text Analysis: A Systematic Approach. In Compendium for Early Career Researchers in Mathematics Education ICME-13 Monographs; Kaiser, G., Presmeg, N., Eds.; Springer: Berlin/Heidelberg, Germany, 2019. [Google Scholar] [CrossRef]
- Kuckartz, U. Mixed Methods: Methodologie, Forschungsdesigns und Analyseverfahren; Springer: Berlin/Heidelberg, Germany, 2014. [Google Scholar]
- Ellis, P.D. The Essential Guide to Effect Sizes: Statistical Power, Meta-Analysis, and the Interpretation of Research Results; Cambridge University Press: New York, NY, USA, 2010. [Google Scholar]
- Schmitt, M.; Blum, G.S. State/Trait Interactions. In Encyclopedia of Personality and Individual Differences; Zeigler-Hill, V., Shackelford, T.K., Eds.; Springer: Cham, Switzerland, 2020. [Google Scholar] [CrossRef]
- Chen, X.; Schmidt, L.A. Temperament and personality. In Handbook of Child Psychology and Developmental Science, 7th ed.; Lamb, M.E., Lerner, R.M., Eds.; John Wiley & Sons: Hoboken, NJ, USA, 2015; Volume 3, pp. 1–49. [Google Scholar]
- Flik, L.; Schneider, P.; Pantis, M.; Hagmann, D.; Allgaier, K.; Barth, G.; Dürrwächter, U.; Conzelmann, A.; Renner, T. Emergencies of children and adolescents with AD(H)D before and during the SARS-CoV2-19 Pandemic: Is there a change? In Proceedings of the 9th World Congress on ADHD, Amsterdam, The Netherlands, 18–21 May 2023. [Google Scholar]


| Age group | Under 13—13 patients; 13–16—41 patients; over 16—23 patients |
| Gender | Female—41 patients; male—36 patients No patients were stored in the system with a different gender. |
| Period of presentation | October 2019–January 2020—17 patients; October 20–January 21—19 patients; October 2021–January 2022—22 patients; October 22–January 23—19 patients |
| Weekday/Weekend | Weekday—64 patients; weekend—13 patients |
| Time of school year | School in session—62 patients School not in session—15 patients |
| Time of day | Day—51 patients; night—23 patients 3 missing values |
| Type of emergency presentation | Outpatients—30 patients; inpatients—47 patients |
| Number of emergency presentations | M = 4.88; Med = 5.50; Min = 1; Max = 20 |
| Different medical personnel | Different physicians wrote the medical report. |
| Kind of Emergency Presentation | Time Period | N Total and by Age Group a | Mean Age Differences between the Groups | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| All | ≤12.99 Years | 13.00–15.99 Years | ≥16.00 Years | χ2(2) | p | M | SD | Min | Max | F | df | p | c η2 | ||
| All | 2019/2020 | 165 | 46 (28%) | 68 (41%) | 51 (31%) | 18.05 | 0.006 * | 14.15 | 2.75 | 7.12 | 18.32 | 9.14 | 787 | 0.004 * | 0.01 |
| 2020/2021 | 172 | 30 (17%) | 84 (49%) | 58 (34%) | 14.76 | 2.20 | 6.67 | 17.99 | |||||||
| 2021/2022 | 222 | 30 (14%) | 112 (50%) | 80 (36%) | 15.01 | 2.19 | 6.90 | 18.21 | |||||||
| 2022/2023 | 240 | 41 (17%) | 99 (41%) | 100 (42%) | 14.92 | 2.54 | 4.71 | 18.65 | |||||||
| Telephone | 2019/2020 | 105 | 37 (35%) | 33 (31%) | 35 (33%) | 24.85 | <0.001 * | 13.96 | 2.97 | 7.12 | 18.32 | 7.87 | 616 | 0.009 * | 0.01 |
| 2020/2021 | 132 | 26 (20%) | 65 (49%) | 41 (31%) | 14.63 | 2.26 | 6.67 | 17.99 | |||||||
| 2021/2022 | 186 | 26 (14%) | 95 (51%) | 65 (35%) | 14.96 | 2.20 | 16.90 | 18.21 | |||||||
| 2022/2023 | 196 | 34 (17%) | 84 (43%) | 78 (40%) | 14.84 | 2.65 | 4.71 | 18.65 | |||||||
| Outpatient | 2019/2020 | 43 | 13 (30%) | 18 (42%) | 12 (28%) | 7.77 | 0.255 | 13.83 | 2.86 | 7.15 | 17.83 | 1.45 | 268 | 0.229 | <0.01 |
| 2020/2021 | 56 | 8 (14%) | 24 (43%) | 24 (43%) | 15.13 | 1.99 | 9.39 | 17.99 | |||||||
| 2021/2022 | 87 | 11 (13%) | 43 (49%) | 33 (38%) | 14.92 | 2.21 | 8.63 | 17.99 | |||||||
| 2022/2023 | 84 | 16 (19%) | 35 (42%) | 33 (39%) | 4.65 | 2.52 | 6.22 | 17.84 | |||||||
| Admission | 2019/2020 | 61 | 7 (11%) | 31 (51%) | 23 (38%) | 5.39 | 0.495 | 15.07 | 1.73 | 9.68 | 17.84 | 4.35 | 353 | 0.038 * | 0.01 |
| 2020/2021 | 78 | 8 (10%) | 42 (54%) | 28 (36%) | 15.14 | 1.88 | 9.92 | 18.00 | |||||||
| 2021/2022 | 107 | 6 (6%) | 59 (55%) | 42 (39%) | 15.47 | 1.16 | 10.54 | 18.00 | |||||||
| 2022/2023 | 109 | 8 (7%) | 49 (45%) | 52 (48%) | 15.56 | 1.86 | 6.22 | 18.01 | |||||||
| Presentation Level | Case Level | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Emergency Presentation | All | Telephone | Outpatient | Admission | All | Telephone | Outpatient | Admission | |
| Eating disorders | |||||||||
| n | all | 142 (10.0%) | 67 (9.7%) | 24 (7.9%) | 51 (12.0%) | 65 (9.5%) | 34 (9.7%) | 20 (9.1%) | 11 (9.7%) |
| 2019/2020 | 5 (2.2%) | 1 (0.9%) | 0 | 4 (5.6%) | 3 (2.2%) | 1 (1.6%) | 0 | 2 (2.7%) | |
| 2020/2021 | 24 (8.3%) | 10 (7.4%) | 6 (9.8%) | 8 (8.7%) | 14 (9.7%) | 6 (7.9%) | 5 (11.9%) | 3 (11.1%) | |
| 2021/2022 | 61 (13.3%) | 32 (13.7%) | 11 (10.8%) | 18 (14.5%) | 26 (12.9%) | 15 (14.2%) | 10 (14.7%) | 1 (3.7%) | |
| 2022/2023 | 52 (11.6%) | 24 (10.9%) | 7 (7.5%) | 21 (15.3%) | 22 (10.8%) | 12 (11.5%) | 5 (7.1%) | 5 (17.4%) | |
| p | <0.001 * | <0.001 * | 0.076 | 0.108 | 0.003 * | 0.031 * | 0.035 * | 0.351 | |
| φc | 0.09 | 0.10 | 0.08 | 0.09 | 0.13 | ||||
| Obsessive–compulsive disorders | |||||||||
| n | all | 38 (2.7%) | 21 (3.0%) | 6 (2.0%) | 11 (2.6%) | 17 (2.5%) | 12 (3.4%) | 2 (0.9%) | 3 (2.7%) |
| 2019/2020 | 9 (4%) | 4 (3.8%) | 1 (2.1%) | 4 (5.6%) | 5 (3.7%) | 3 (4.8%) | 0 | 2 (6.7%) | |
| 2020/2021 | 2 (0.7%) | 1 (0.7%) | 0 | 1 (1.1%) | 2 (1.4%) | 1 (1.3%) | 0 | 1 (3.7%) | |
| 2021/2022 | 5 (1.1%) | 3 (1.3%) | 1 (1.0%) | 1 (0.8%) | 2 (1.0%) | 2 (1.9%) | 0 | 0 | |
| 2022/2023 | 22 (4.9%) | 13 (5.9%) | 4 (4.3%) | 5 (3.6%) | 8 (3.9%) | 6 (5.7%) | 2 (2.8%) | 0 | |
| p | <0.001 * | 0.026 * | 0.234 | 0.125 | 0.155 | 0.330 | 0.333 | .510 | |
| φc | 0.08 | 0.08 | |||||||
| Affective disorders | |||||||||
| n | all | 801 (56.4%) | 382 (55.2%) | 137 (45.1%) | 282 (66.4%) | 384 (45.2%) | 205 (58.8%) | 104 (47.1%) | 75 (66.4%) |
| 2019/2020 | 115 (51.3%) | 51 (49.0%) | 19 (39.6%) | 45 (62.5%) | 66 (49.3%) | 31 (49.2%) | 16 (39.0%) | 19 (63.3%) | |
| 2020/2021 | 147 (51.0%) | 67 (49.6%) | 25 (41.0%) | 55 (59.8%) | 72 (49.7%) | 40 (52.6%) | 17 (40.5%) | 15 (55.6%) | |
| 2021/2022 | 280 (61.0%) | 140 (60.1%) | 52 (51.0%) | 88 (71.0%) | 123 (61.2%) | 67 (63.2%) | 37 (54.4%) | 19 (70.4%) | |
| 2022/2023 | 259 (57.6%) | 124 (56.4%) | 41 (44.1%) | 94 (68.6%) | 123 (60.6%) | 67 (64.4%) | 34 (48.6%) | 22 (75.9%) | |
| p | 0.019 * | 0.129 | 0.484 | 0.288 | 0.033 * | 0.124 | 0.351 | 0.417 | |
| φc | 0.06 | 0.08 | |||||||
| Expansive disorders | |||||||||
| n | all | 216 (15.2%) | 116 (16.8%) | 49 (16.1%) | 51 (12.0%) | 114 (16.7%) | 61 (17.5%) | 34 (15.4%) | 19 (16.8%) |
| 2019/2020 | 55 (24.6%) | 31 (29.8%) | 12 (25.0%) | 12 (16.7%) | 34 (25.4%) | 20 (31.7%) | 9 (22.0%) | 5 (16.7%) | |
| 2020/2021 | 60 (20.8%) | 29 (21.5%) | 12 (19.7%) | 19 (20.7%) | 32 (22.1%) | 18 (23.7%) | 9 (21.4%) | 5 (18.5%) | |
| 2021/2022 | 54 (11.8%) | 29 (12.4%) | 17 (16.7%) | 8 (6.5%) | 22 (10.9%) | 9 (8.5%) | 9 (13.2%) | 4 (14.8%) | |
| 2022/2023 | 47(10.4%) | 27 (12.3%) | 8 (8.6%) | 12 (8.8%) | 26 (12.8%) | 14 (13.5%) | 7 (10.0%) | 5 (17.2%) | |
| p | <0.001 * | <0.001 * | 0.052 | 0.005* | <0.001 * | <0.001 * | 0.215 | 1.000 | |
| φc | 0.11 | 0.12 | 0.12 | 0.11 | 0.14 | ||||
| Presentation Level | Case Level | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Emergency Presentation | All | Telephone | Outpatient | Admission | All | Telephone | Outpatient | Admission | |
| Anxiety disorders | |||||||||
| n | all | 159 (11.2%) | 84 (12.1%) | 31 (10.2%) | 44 (10.4%) | 84 (12.3%) | 51 (14.6%) | 20 (9.0%) | 13 (11.5%) |
| 2019/2020 | 16 (7.1%) | 9 (9.7%) | 3 (6.3%) | 4 (5.6%) | 10 (7.5%) | 7 (11.1%) | 1 (2.4%) | 2 (6.7%) | |
| 2020/2021 | 30 (10.4%) | 14 (10.4%) | 6 (9.8%) | 10 (10.9%) | 14 (9.7%) | 7 (9.2%) | 4 (9.5%) | 3 (11.1%) | |
| 2021/2022 | 54 (11.8%) | 31 (13.3%) | 8 (7.8%) | 15 (12.1%) | 29 (14.4%) | 21 (19.8%) | 4 (5.9%) | 4 (14.8%) | |
| 2022/2023 | 59 (13.1%) | 30 (13.6%) | 13 (15.1%) | 15 (10.9%) | 31 (15.3%) | 16 (15.4%) | 11 (15.7%) | 4 (13.8%) | |
| p | 0.120 | 0.527 | 0.312 | 0.515 | 0.092 | 0.209 | 0.093 | 0.761 | |
| φc | |||||||||
| Substance abuse | |||||||||
| n | all | 103 (7.2%) | 46 (6.6%) | 29 (9.5%) | 29 (6.6%) | 47 (6.9%) | 17 (4.9%) | 20 (9.0%) | 10 (8.8%) |
| 2019/2020 | 19 (8.5%) | 6 (5.8%) | 4 (8.3%) | 9 (12.5%) | 14 (10.4%) | 4 (6.3%) | 4 (9.8%) | 6 (20.0%) | |
| 2020/2021 | 26 (9.0%) | 12 (8.9%) | 9 (14.8%) | 5 (5.4%) | 15 (10.3%) | 5 (6.6%) | 8 (19.0%) | 2 (7.4%) | |
| 2021/2022 | 26 (5.7%) | 14 (6.0%) | 8 (7.8%) | 4 (3.2%) | 10 (5.0%) | 5 (4.7%) | 5 (7.4%) | 0 | |
| 2022/2023 | 32 (7.1%) | 14 (6.4%) | 8 (8.6%) | 10 (7.3%) | 8 (3.9%) | 3 (2.9%) | 3 (4.3%) | 2 (6.9%) | |
| p | 0.290 | 0.718 | 0.503 | 0.089 | 0.025 * | 0.615 | 0.079 | 0.057 | |
| φc | 0.08 | ||||||||
| Psychoses | |||||||||
| n | all | 33 (2.3%) | 12 (1.7%) | 9 (3.0%) | 12 (2.8%) | 12 (1.8%) | 4 (1.1%) | 5 (2.3%) | 3 (2.7%) |
| 2019/2020 | 3 (1.3%) | 0 | 2 (4.2%) | 1 (1.4%) | 2 (1.5%) | 0 | 1 (2.4%) | 1 (3.3%) | |
| 2020/2021 | 10 (3.5%) | 3 (2.2%) | 3 (4.9%) | 4 (4.3%) | 4 (2.8%) | 0 | 2 (4.8%) | 2 (7.4%) | |
| 2021/2022 | 7 (1.5%) | 2 (0.9%) | 2 (2.0%) | 3 (2.4%) | 3 (1.5%) | 1 (0.9%) | 2 (2.9%) | 0 | |
| 2022/2023 | 13 (2.9%) | 7 (3.25) | 2 (2.1%) | 4 (2.9%) | 3 (1.5%) | 3 (2.9%) | 0 | 0 | |
| p | 0.214 | 0.128 | 0.630 | 0.751 | 0.831 | 0.395 | 0.264 | 0.316 | |
| φc | |||||||||
| Indicators of Risk/Specific Reason for Visit | Stressors | Personality Characteristics | |||
|---|---|---|---|---|---|
| School | Peers | Family | Self | ||
| Underweight | School closures due to the pandemic | Concerns about friends | Out-of-home placement | Psychotic symptoms | High performance expectations |
| Eating disorder symptoms | School absenteeism | Relationship terminations | Deaths | Risk to others | Perfectionism |
| Pathological use of media | Academic overwhelm | Conflict with friends/relationship | Financial difficulties | Mental health crisis | Impulsivity |
| Substance abuse | Performance pressure | No friends | Violent confrontation | Absenteeism | Self-doubt |
| Absenteeism | Decline in performance | Social withdrawal | History of abuse in the family | Eating disorder symptoms | |
| Mental health crisis | Concentration problems | Mental disorder, deviant behavior, or disability within the family | Suicidality | ||
| Self-injury | Conflict with classmates | Parental separation | Self-injury | ||
| Psychotic symptoms | Bullying | Parental conflicts | Refugee | ||
| Risk to others | Parent´s lack of understanding towards the children | Criminal behavior | |||
| Suicide attempt | Conflict with family member/caregiver | Flashbacks | |||
| Suicidality | Loss of appetite | ||||
| Underweight | Sleep disorders | ||||
| Substance abuse | |||||
| SARS-CoV-2 pandemic | |||||
| Physical symptoms | |||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schneider, P.S.; Pantis, M.; Preiser, C.; Hagmann, D.; Barth, G.M.; Renner, T.J.; Allgaier, K. SARS-CoV-2 and Adolescent Psychiatric Emergencies at the Tübingen University Hospital: Analyzing Trends, Diagnoses, and Contributing Factors. Int. J. Environ. Res. Public Health 2024, 21, 216. https://doi.org/10.3390/ijerph21020216
Schneider PS, Pantis M, Preiser C, Hagmann D, Barth GM, Renner TJ, Allgaier K. SARS-CoV-2 and Adolescent Psychiatric Emergencies at the Tübingen University Hospital: Analyzing Trends, Diagnoses, and Contributing Factors. International Journal of Environmental Research and Public Health. 2024; 21(2):216. https://doi.org/10.3390/ijerph21020216
Chicago/Turabian StyleSchneider, Priska S., Michelle Pantis, Christine Preiser, Daniela Hagmann, Gottfried M. Barth, Tobias J. Renner, and Katharina Allgaier. 2024. "SARS-CoV-2 and Adolescent Psychiatric Emergencies at the Tübingen University Hospital: Analyzing Trends, Diagnoses, and Contributing Factors" International Journal of Environmental Research and Public Health 21, no. 2: 216. https://doi.org/10.3390/ijerph21020216
APA StyleSchneider, P. S., Pantis, M., Preiser, C., Hagmann, D., Barth, G. M., Renner, T. J., & Allgaier, K. (2024). SARS-CoV-2 and Adolescent Psychiatric Emergencies at the Tübingen University Hospital: Analyzing Trends, Diagnoses, and Contributing Factors. International Journal of Environmental Research and Public Health, 21(2), 216. https://doi.org/10.3390/ijerph21020216






