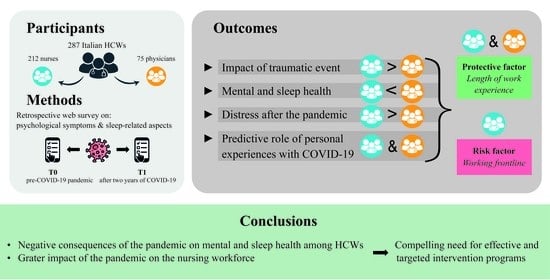
Healthcare Workers after Two Years of COVID-19: The Consequences of the Pandemic on Psychological Health and Sleep among Nurses and Physicians
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants and Protocol
2.2. Measures
- Socio-demographic, occupational and COVID-19-related information: A short section first collected socio-demographic information (i.e., age, gender, marital status, education level). Then, some questions investigated specific information about the healthcare career (i.e., healthcare profession, department, length of service, working on the frontline). Finally, we collected COVID-19-related information (i.e., COVID-19 positivity, forced quarantine period, COVID-19-infected relatives or friends, relatives or friends who died from COVID-19, satisfaction with governmental measures).
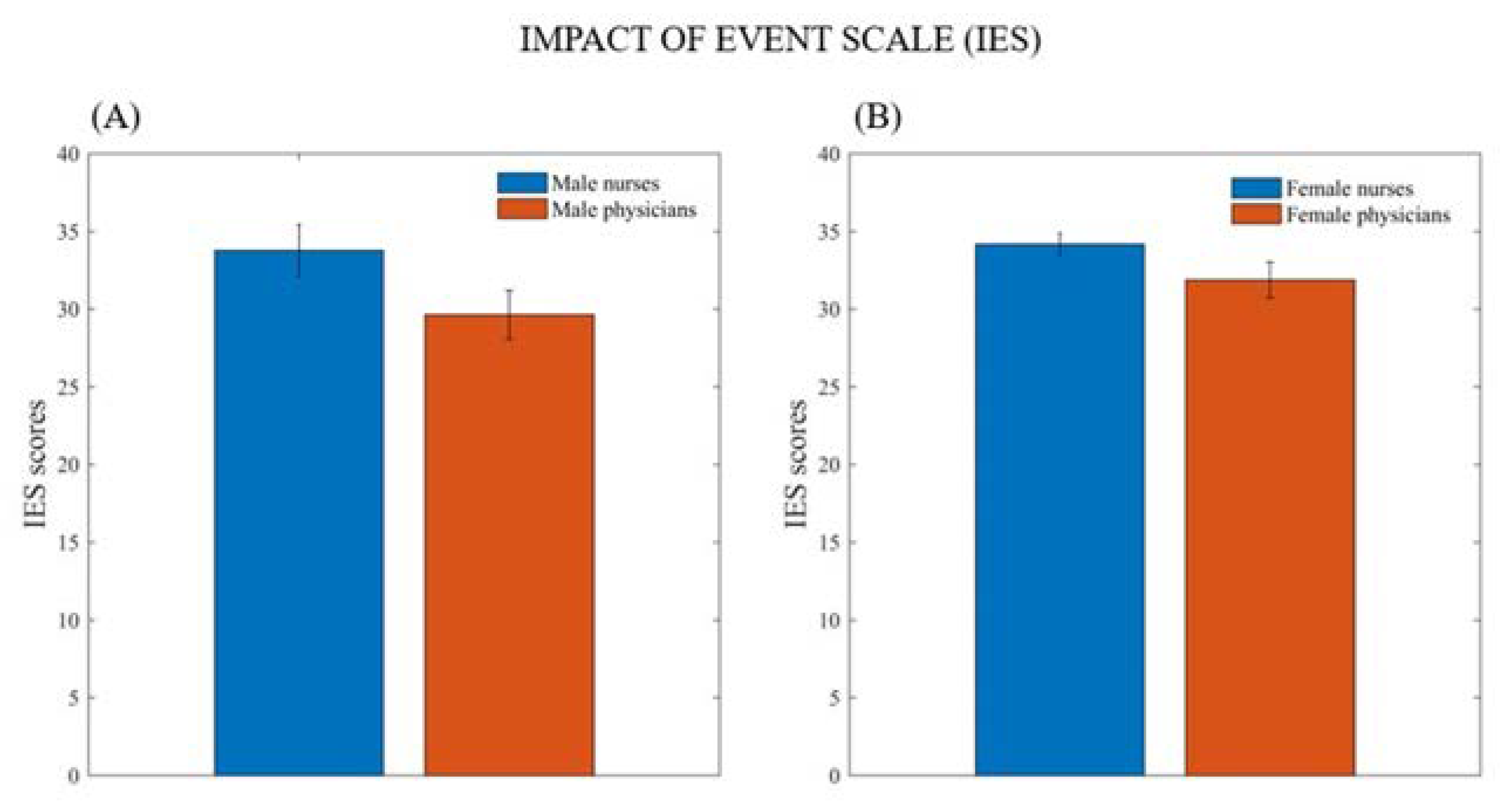
- Impact of Event Scale (IES) [26]: An Italian validation of a self-administered questionnaire to assess the symptoms of PTSD after previous traumatic event experiences. This 15-item scale is composed of different emotional reactions to which the respondent is asked to indicate how frequently each reaction was experienced from 0 to 4, where 0 indicates “Not at all” and 4 indicates “Extremely”.
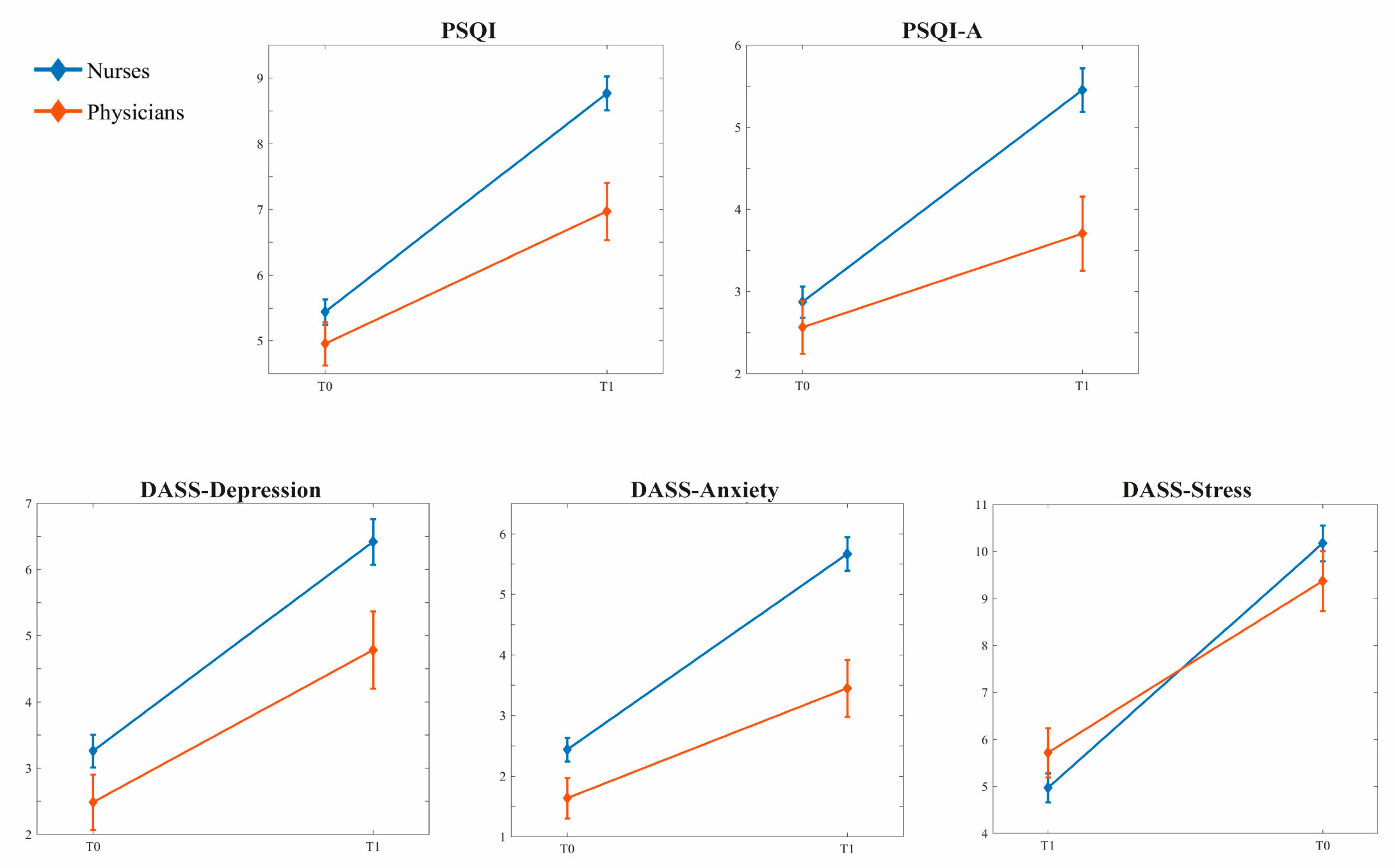
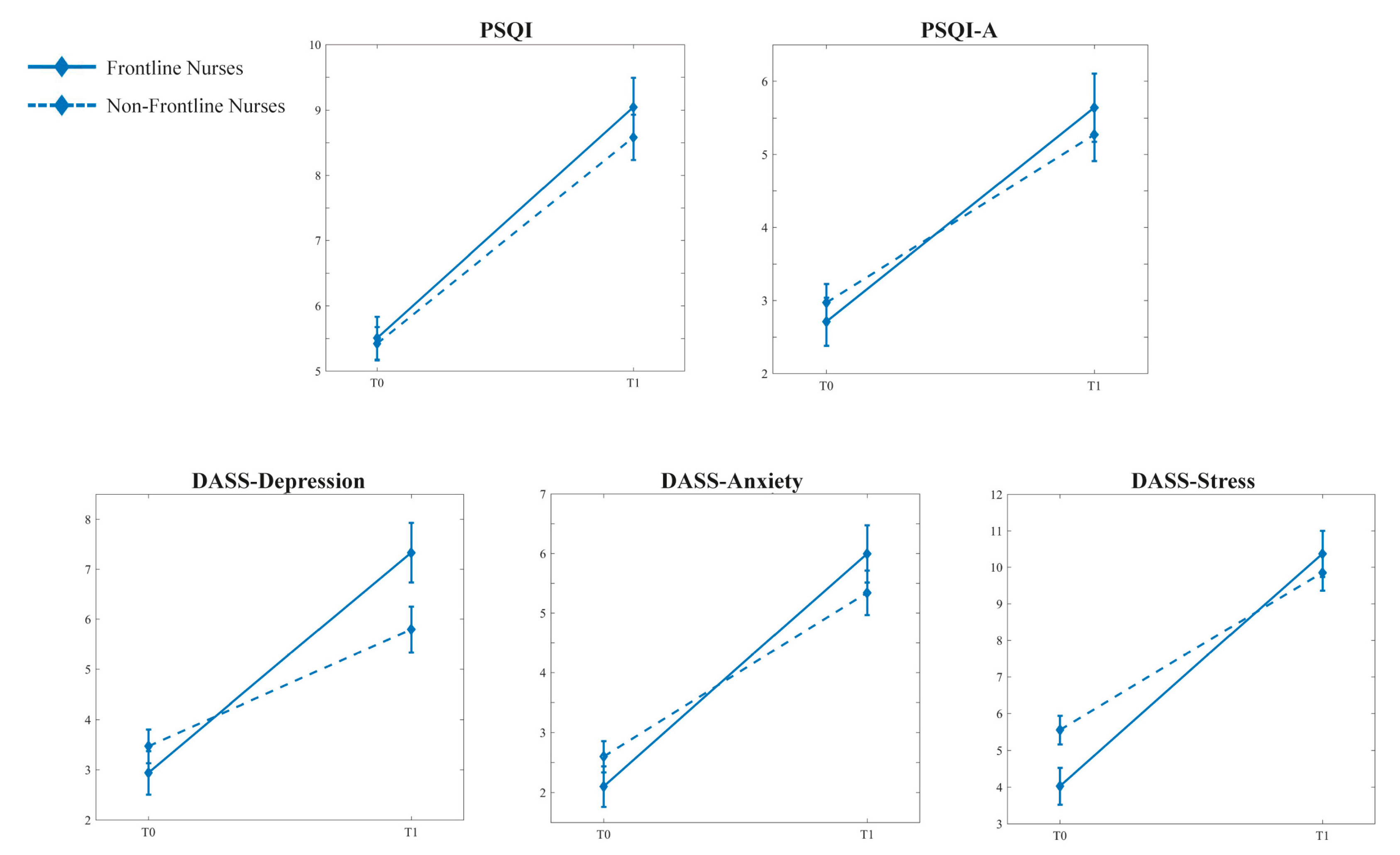
- Pittsburgh Sleep Quality Index (PSQI) [27]: An Italian validation of a self-reported questionnaire to investigate subjective sleep quality. The measure consists of 19 items, resulting in partial scores in 7 subscales (subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleep medications, daytime dysfunction) and a global score. A PSQI global score > 5 indicates poor subjective sleep quality.
- Pittsburgh Sleep Quality Index-Addendum (PSQI-A) [28]: A specific self-report measure for the assessment of seven disruptive nocturnal behaviors common among subjects with PTSD: flashes, general nervousness, memories or nightmares of traumatic experience, severe anxiety or panic not related to traumatic memories, bad dreams not related to traumatic memories, episodes of terror or screaming during sleep without fully awakening, and episodes of acting out dreams, such as kicking, punching, running, or screaming. A PSQI score > 4 is highly predictive for discriminating between subjects with and without PTSD.
- Depression Anxiety Stress Scale (DASS-21) short form [29]: An Italian validation of a self-report questionnaire in which participants rate the frequency and severity of depression, anxiety, and stress symptoms. The 21 Items consist of sentences about the previous week and each item is scored on a 4-point Likert scale, ranging from 0 (“I strongly disagree”) to 3 (“I totally agree”). Subscale scores are calculated as the sum of scores for the relevant seven items from each subscale. The cut-offs are obtained by multiplying the raw scores by two to suit the original 42 items and the scores indicative of severe rating of depression, anxiety, and stress are ≥21, ≥15, and ≥26, respectively.
2.3. Statistical Analyses
3. Results
3.1. Characteristics of the Sample and Their Distributions
3.2. The Effects of the Pandemic on Nurses and Physicians
3.3. The Impact of Frontline Engagement on Nurses and Physicians
3.4. COVID-19-Related Predictors of the Current Sleep and Psychological Conditions in Healthcare Workers
4. Discussion
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Arabi, Y.M.; Murthy, S.; Webb, S. COVID-19: A Novel Coronavirus and a Novel Challenge for Critical Care. Intensive Care Med. 2020, 46, 833–836. [Google Scholar] [CrossRef]
- Pietrantonio, F.; Rosiello, F.; Alessi, E.; Pascucci, M.; Rainone, M.; Cipriano, E.; Di Berardino, A.; Vinci, A.; Ruggeri, M.; Ricci, S. Burden of COVID-19 on Italian Internal Medicine Wards: Delphi, SWOT, and Performance Analysis after Two Pandemic Waves in the Local Health Authority “Roma 6” Hospital Structures. Int. J. Environ. Res. Public Health 2021, 18, 5999. [Google Scholar] [CrossRef] [PubMed]
- Rind, E.; Kimpel, K.; Preiser, C.; Papenfuss, F.; Wagner, A.; Alsyte, K.; Siegel, A.; Klink, A.; Steinhilber, B.; Kauderer, J. Adjusting Working Conditions and Evaluating the Risk of Infection during the COVID-19 Pandemic in Different Workplace Settings in Germany: A Study Protocol for an Explorative Modular Mixed Methods Approach. BMJ Open 2020, 10, e043908. [Google Scholar] [CrossRef] [PubMed]
- Pappa, S.; Sakkas, N.; Sakka, E. A Year in Review: Sleep Dysfunction and Psychological Distress in Healthcare Workers during the COVID-19 Pandemic. Sleep Med. 2022, 91, 237–245. [Google Scholar] [CrossRef] [PubMed]
- Aymerich, C.; Pedruzo, B.; Pérez, J.L.; Laborda, M.; Herrero, J.; Blanco, J.; Mancebo, G.; Andrés, L.; Estévez, O.; Fernandez, M. COVID-19 Pandemic Effects on Health Workers’mental Health: Systematic Review and Meta-Analysis. Eur. Psychiatry 2022, 65, e10. [Google Scholar] [CrossRef]
- Buresti, G.; Rondinone, B.M.; Gagliardi, D.; Petyx, M.; D’Ancona, F.P.; Pezzotti, P.; Riccardo, F.; Iavicoli, S. The Impact of the First Wave of the COVID-19 Pandemic on Healthcare Workers: An Italian Retrospective Study. Int. J. Environ. Res. Public Health 2022, 19, 5205. [Google Scholar] [CrossRef]
- Nguyen, L.H.; Drew, D.A.; Graham, M.S.; Joshi, A.D.; Guo, C.-G.; Ma, W.; Mehta, R.S.; Warner, E.T.; Sikavi, D.R.; Lo, C.-H. Risk of COVID-19 among Front-Line Health-Care Workers and the General Community: A Prospective Cohort Study. Lancet Public Health 2020, 5, e475–e483. [Google Scholar]
- Galanis, P.; Vraka, I.; Fragkou, D.; Bilali, A.; Kaitelidou, D. Seroprevalence of SARS-CoV-2 Antibodies and Associated Factors in Healthcare Workers: A Systematic Review and Meta-Analysis. J. Hosp. Infect. 2021, 108, 120–134. [Google Scholar] [CrossRef]
- Schwartz, K.L.; Achonu, C.; Buchan, S.A.; Brown, K.A.; Lee, B.; Whelan, M.; Wu, J.H.C.; Garber, G. COVID-19 Infections among Healthcare Workers and Transmission within Households. medRxiv 2020. [Google Scholar] [CrossRef]
- Bruria, A.; Maya, S.-T.; Gadi, S.; Orna, T. Impact of Emergency Situations on Resilience at Work and Burnout of Hospital’s Healthcare Personnel. Int. J. Disaster Risk Reduct. 2022, 76, 102994. [Google Scholar] [CrossRef]
- Rodrigues, H.; Cobucci, R.; Oliveira, A.; Cabral, J.V.; Medeiros, L.; Gurgel, K.; Souza, T.; Gonçalves, A.K. Burnout Syndrome among Medical Residents: A Systematic Review and Meta-Analysis. PLoS ONE 2018, 13, e0206840. [Google Scholar] [CrossRef] [PubMed]
- Cox, C.L. ‘Healthcare Heroes’: Problems with Media Focus on Heroism from Healthcare Workers during the COVID-19 Pandemic. J. Med. Ethics 2020, 46, 510–513. [Google Scholar] [CrossRef] [PubMed]
- Lai, J.; Ma, S.; Wang, Y.; Cai, Z.; Hu, J.; Wei, N.; Wu, J.; Du, H.; Chen, T.; Li, R. Factors Associated with Mental Health Outcomes among Health Care Workers Exposed to Coronavirus Disease 2019. JAMA Netw. Open 2020, 3, e203976. [Google Scholar] [CrossRef] [PubMed]
- Salari, N.; Khazaie, H.; Hosseinian-Far, A.; Khaledi-Paveh, B.; Kazeminia, M.; Mohammadi, M.; Shohaimi, S.; Daneshkhah, A.; Eskandari, S. The Prevalence of Stress, Anxiety and Depression within Front-Line Healthcare Workers Caring for COVID-19 Patients: A Systematic Review and Meta-Regression. Hum. Resour. Health 2020, 18, 100. [Google Scholar] [CrossRef]
- Minahan, J.; Falzarano, F.; Yazdani, N.; Siedlecki, K.L. The COVID-19 Pandemic and Psychosocial Outcomes across Age through the Stress and Coping Framework. Gerontologist 2021, 61, 228–239. [Google Scholar] [CrossRef]
- Işik, M.; Kirli, U.; Özdemiṙ, P.G. The Mental Health of Healthcare Professionals During the COVID-19 Pandemic. Turk Psikiyatr. Derg. 2021, 32, 225. [Google Scholar] [CrossRef]
- Franceschini, C.; Musetti, A.; Zenesini, C.; Palagini, L.; Scarpelli, S.; Quattropani, M.C.; Lenzo, V.; Freda, M.F.; Lemmo, D.; Vegni, E. Poor Sleep Quality and Its Consequences on Mental Health during the COVID-19 Lockdown in Italy. Front. Psychol. 2020, 11, 574475. [Google Scholar] [CrossRef]
- Scarpelli, S.; Alfonsi, V.; Mangiaruga, A.; Musetti, A.; Quattropani, M.C.; Lenzo, V.; Freda, M.F.; Lemmo, D.; Vegni, E.; Borghi, L. Pandemic Nightmares: Effects on Dream Activity of the COVID-19 Lockdown in Italy. J. Sleep Res. 2021, 30, e13300. [Google Scholar] [CrossRef]
- Sahebi, A.; Nejati-Zarnaqi, B.; Moayedi, S.; Yousefi, K.; Torres, M.; Golitaleb, M. The Prevalence of Anxiety and Depression among Healthcare Workers during the COVID-19 Pandemic: An Umbrella Review of Meta-Analyses. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2021, 107, 110247. [Google Scholar] [CrossRef]
- Salari, N.; Khazaie, H.; Hosseinian-Far, A.; Ghasemi, H.; Mohammadi, M.; Shohaimi, S.; Daneshkhah, A.; Khaledi-Paveh, B.; Hosseinian-Far, M. The Prevalence of Sleep Disturbances among Physicians and Nurses Facing the COVID-19 Patients: A Systematic Review and Meta-Analysis. Glob. Health 2020, 16, 92. [Google Scholar] [CrossRef]
- d’Ettorre, G.; Ceccarelli, G.; Santinelli, L.; Vassalini, P.; Innocenti, G.P.; Alessandri, F.; Koukopoulos, A.E.; Russo, A.; Tarsitani, L. Post-Traumatic Stress Symptoms in Healthcare Workers Dealing with the COVID-19 Pandemic: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 601. [Google Scholar] [CrossRef]
- Rosiello, D.F.; Anwar, S.; Yufika, A.; Adam, R.Y.; Ismaeil, M.I.H.; Ismail, A.Y.; Dahman, N.B.H.; Hafsi, M.; Ferjani, M.; Sami, F.S. Acceptance of COVID-19 Vaccination at Different Hypothetical Efficacy and Safety Levels in Ten Countries in Asia, Africa, and South America. Narra J. 2021, 1, 3. [Google Scholar] [CrossRef]
- Harapan, H.; Anwar, S.; Yufika, A.; Sharun, K.; Gachabayov, M.; Fahriani, M.; Husnah, M.; Raad, R.; Abdalla, R.Y.A.; Adam, R.Y. Vaccine Hesitancy among Communities in Ten Countries in Asia, Africa, and South America during the COVID-19 Pandemic. Pathog. Glob. Health 2022, 116, 236–243. [Google Scholar] [CrossRef]
- Kunz, M.; Strasser, M.; Hasan, A. Impact of the Coronavirus Disease 2019 Pandemic on Healthcare Workers: Systematic Comparison between Nurses and Medical Doctors. Curr. Opin. Psychiatry 2021, 34, 413. [Google Scholar] [CrossRef]
- Pietrantonio, F. Beyond Coronavirus: The Metamorphosis as the Essence of the Phenomenon. Med. Health Care Philos. 2022, 25, 299–304. [Google Scholar] [CrossRef]
- Pietrantonio, F.; De Gennaro, L.; Di Paolo, M.C.; Solano, L. The Impact of Event Scale: Validation of an Italian Version. J. Psychosom. Res. 2003, 55, 389–393. [Google Scholar] [CrossRef]
- Curcio, G.; Tempesta, D.; Scarlata, S.; Marzano, C.; Moroni, F.; Rossini, P.M.; Ferrara, M.; De Gennaro, L. Validity of the Italian Version of the Pittsburgh Sleep Quality Index (PSQI). Neurol. Sci. 2013, 34, 511–519. [Google Scholar] [CrossRef]
- Germain, A. Sleep Disturbances as the Hallmark of PTSD: Where Are We Now? Am. J. Psychiatry 2013, 170, 372–382. [Google Scholar] [CrossRef]
- Bottesi, G.; Ghisi, M.; Altoè, G.; Conforti, E.; Melli, G.; Sica, C. The Italian Version of the Depression Anxiety Stress Scales-21: Factor Structure and Psychometric Properties on Community and Clinical Samples. Compr. Psychiatry 2015, 60, 170–181. [Google Scholar] [CrossRef]
- Rossi, R.; Socci, V.; Pacitti, F.; Mensi, S.; Di Marco, A.; Siracusano, A.; Di Lorenzo, G. Mental health outcomes among healthcare workers and the general population during the COVID-19 in Italy. Front. Psychol. 2020, 11, 608986. [Google Scholar] [CrossRef]
- White, E.M.; Wetle, T.F.; Reddy, A.; Baier, R.R. Front-Line Nursing Home Staff Experiences during the COVID-19 Pandemic. J. Am. Med. Dir. Assoc. 2021, 22, 199–203. [Google Scholar] [CrossRef]
- Serrano-Ripoll, M.J.; Meneses-Echavez, J.F.; Ricci-Cabello, I.; Fraile-Navarro, D.; Fiol-deRoque, M.A.; Pastor-Moreno, G.; Castro, A.; Ruiz-Pérez, I.; Campos, R.Z.; Gonçalves-Bradley, D.C. Impact of Viral Epidemic Outbreaks on Mental Health of Healthcare Workers: A Rapid Systematic Review and Meta-Analysis. J. Affect. Disord. 2020, 277, 347–357. [Google Scholar] [CrossRef]
- Salfi, F.; Amicucci, G.; Corigliano, D.; D’Atri, A.; Viselli, L.; Tempesta, D.; Ferrara, M. Changes of Evening Exposure to Electronic Devices during the COVID-19 Lockdown Affect the Time Course of Sleep Disturbances. medRxiv 2020. [Google Scholar] [CrossRef]
- Alfonsi, V.; Gorgoni, M.; Scarpelli, S.; Zivi, P.; Sdoia, S.; Mari, E.; Quaglieri, A.; Ferlazzo, F.; Giannini, A.M.; De Gennaro, L. Changes in Sleep Pattern and Dream Activity across and after the COVID-19 Lockdown in Italy: A Longitudinal Observational Study. J. Sleep Res. 2022, 31, e13500. [Google Scholar] [CrossRef]
- Di Muzio, M.; Diella, G.; Di Simone, E.; Novelli, L.; Alfonsi, V.; Scarpelli, S.; Annarumma, L.; Salfi, F.; Pazzaglia, M.; Giannini, A.M.; et al. Nurses and Night Shifts: Poor Sleep Quality Exacerbates Psychomotor Performance. Front. Neurosci. 2020, 14, 1–9. [Google Scholar] [CrossRef]
- Ohayon, M.M.; Lemoine, P.; Arnaud-Briant, V.; Dreyfus, M. Prevalence and Consequences of Sleep Disorders in a Shift Worker Population. J. Psychosom. Res. 2002, 53, 577–583. [Google Scholar] [CrossRef]
- Bridgland, V.M.E.; Moeck, E.K.; Green, D.M.; Swain, T.L.; Nayda, D.M.; Matson, L.A.; Hutchison, N.P.; Takarangi, M.K.T. Why the COVID-19 Pandemic Is a Traumatic Stressor. PLoS ONE 2021, 16, e0240146. [Google Scholar] [CrossRef]
- Scarpelli, S.; Bartolacci, C.; D’Atri, A.; Gorgoni, M.; De Gennaro, L. The Functional Role of Dreaming in Emotional Processes. Front. Psychol. 2019, 10, 459. [Google Scholar] [CrossRef]
- Wang, Y.; Li, Y.; Jiang, J.; Feng, Y.; Lu, D.; Zhang, W.; Song, H. COVID-19 Outbreak–Related Psychological Distress among Healthcare Trainees: A Cross-Sectional Study in China. BMJ Open 2020, 10, e041671. [Google Scholar] [CrossRef]
- Li, Y.; Zhang, H.; Feng, Z.; Chen, S.; Liu, T.; Chen, X.; Tang, J.; Liao, Y. Life Events, Anxiety and Depression among Doctors and Nurses in the Emergency Department: A Study from Eleven General Hospital in Hunan Province, China. J. Psychiatry Brain Sci. 2016, 1, 2. [Google Scholar]
- Davey, A.; Sharma, P.; Davey, S.; Shukla, A. Is Work-Associated Stress Converted into Psychological Distress among the Staff Nurses: A Hospital-Based Study. J. Fam. Med. Prim. Care 2019, 8, 511. [Google Scholar] [CrossRef]
- Al Maqbali, M.; Al Sinani, M.; Al-Lenjawi, B. Prevalence of Stress, Depression, Anxiety and Sleep Disturbance among Nurses during the COVID-19 Pandemic: A Systematic Review and Meta-Analysis. J. Psychosom. Res. 2021, 141, 110343. [Google Scholar] [CrossRef]
- Shen, X.; Zou, X.; Zhong, X.; Yan, J.; Li, L. Psychological Stress of ICU Nurses in the Time of COVID-19. Crit. Care 2020, 24, 200. [Google Scholar] [CrossRef]
- Liu, Y.; Wang, H.; Chen, J.; Zhang, X.; Yue, X.; Ke, J.; Wang, B.; Peng, C. Emergency Management of Nursing Human Resources and Supplies to Respond to Coronavirus Disease 2019 Epidemic. Int. J. Nurs. Sci. 2020, 7, 135–138. [Google Scholar] [CrossRef]
- Salfi, F.; Lauriola, M.; Amicucci, G.; Corigliano, D.; Viselli, L.; Tempesta, D.; Ferrara, M. Gender-Related Time Course of Sleep Disturbances and Psychological Symptoms during the COVID-19 Lockdown: A Longitudinal Study on the Italian Population. Neurobiol. Stress 2020, 13, 100259. [Google Scholar] [CrossRef]
- Flaubert, J.L.; Le Menestrel, S.; Williams, D.R.; Wakefield, M.K.; National Academies of Sciences and Medicine, E. Nurses in Disaster Preparedness and Public Health Emergency Response. In The Future of Nursing 2020–2030: Charting a Path to Achieve Health Equity; National Academies Press: Washington, DC, USA, 2021. [Google Scholar]
- Di Muzio, M.; Diella, G.; Di Simone, E.; Pazzaglia, M.; Alfonsi, V.; Novelli, L.; Cianciulli, A.; Scarpelli, S.; Gorgoni, M.; Giannini, A. Comparison of Sleep and Attention Metrics Among Nurses Working Shifts on a Forward-vs Backward-Rotating Schedule. JAMA Netw. Open 2021, 4, e2129906. [Google Scholar] [CrossRef]
- Tull, M.T.; Edmonds, K.A.; Scamaldo, K.M.; Richmond, J.R.; Rose, J.P.; Gratz, K.L. Psychological Outcomes Associated with Stay-at-Home Orders and the Perceived Impact of COVID-19 on Daily Life. Psychiatry Res. 2020, 289, 113098. [Google Scholar] [CrossRef]
- Chemali, S.; Mari-Sáez, A.; El Bcheraoui, C.; Weishaar, H. Health Care Workers’ Experiences during the COVID-19 Pandemic: A Scoping Review. Hum. Resour. Health 2022, 20, 27. [Google Scholar] [CrossRef]
- y Rosas, V.G.S.; Moscoso-Porras, M.; Ormeño, R.; Artica, F.; Bayes, C.L.; Miranda, J.J. Gender Income Gap among Physicians and Nurses in Peru: A Nationwide Assessment. Lancet Glob. Health 2019, 7, e412–e413. [Google Scholar] [CrossRef]
- Eysenbach, G. Improving the quality of Web surveys: The Checklist for Reporting Results of Internet E-Surveys (CHERRIES). J. Med. Internet Res. 2004, 6, e34. [Google Scholar] [CrossRef]
| Total Sample (N = 287) | Nurses (n = 212) | Physicians (n = 75) | Nurses vs. Physicians | |
|---|---|---|---|---|
| Mean (SE) | t (p) | |||
| Age | 46.12 (0.66) | 45.41 (0.75) | 48.13 (1.34) | 1.829 (0.069) |
| Years on the job | 18.45 (0.72) | 19.71 (0.82) | 14.87 (1.40) | −3.007 (0.003) * |
| N° (%) | χ2 (p) | |||
| Gender | ||||
| Male | 73 (25.4) | 45 (21.2) | 28 (37.3) | 7.578 (0.006) * |
| Female | 214 (76.4) | 167 (78.8) | 47 (62.7) | |
| Marital status | ||||
| Single | 103 (35.9) | 76 (35.8) | 27 (36.0) | 8.841 (0.031) * |
| Married/Cohabitant | 135 (47.0) | 92 (43.4) | 43 (57.3) | |
| Divorced/Separated | 47 (16.4) | 42 (19.8) | 5 (6.7) | |
| Widower | 2 (0.7) | 2 (0.9) | 0 (0.0) | |
| Education level | ||||
| Until middle School | 7 (2.4) | 7 (3.3) | 0 (0.0) | 171.061 (<0.001) ** |
| High School | 51 (17.8) | 51 (24.1) | 0 (0.0) | |
| Bachelor’s Degree | 122 (42.5) | 122 (57.5) | 0 (0.0) | |
| Master’s Degree | 99 (34.5) | 29 (13.7) | 70 (93.3) | |
| PhD/postgraduate school | 8 (2.8) | 3 (1.4) | 5 (6.7) | |
| Currently working on the frontline | ||||
| Yes | 108 (37.6) | 80 (37.7) | 28 (37.3) | 0.004 (0.951) |
| No | 179 (62.4) | 132 (62.3) | 47 (62.7) | |
| COVID-19 positivity during the pandemic | ||||
| Yes | 123 (42.9) | 86 (40.6) | 37 (49.3) | 1.739 (0.187) |
| No | 164 (57.1) | 126 (59.4) | 38 (50.7) | |
| Forced quarantine period | ||||
| Yes | 148 (51.6) | 113 (53.3) | 35 (46.7) | 0.977 (0.323) |
| No | 139 (48.4) | 99 (46.7) | 40 (53.3) | |
| COVID-19-infected relatives or friends | ||||
| Yes | 208 (72.5) | 152 (71.7) | 56 (74.7) | 0.245 (0.621) |
| No | 79 (27.5) | 60 (28.3) | 19 (25.3) | |
| Relatives or friends who have died of COVID-19 | ||||
| Yes | 41 (14.3) | 36 (17.0) | 5 (6.7) | 4.813 (0.028) * |
| No | 246 (85.7) | 176 (83.0) | 70 (93.3) | |
| Satisfaction with governmental measures | ||||
| Yes | 204 (71.1) | 151 (71.2) | 53 (70.7) | 0.008 (0.927) |
| No | 83 (28.9) | 61 (28.8) | 22 (29.3) | |
| Time | Profession | Time * Profession | Covariate (Years on the Job) | |||||
|---|---|---|---|---|---|---|---|---|
| F1,284 | p | F1,284 | p | F1,284 | p | F1,284 | p | |
| PSQI | 61.558 | <0.001 ** | 8.951 | 0.003 * | 7.406 | 0.007 * | 0.002 | 0.961 |
| PSQI-A | 43.389 | <0.001 ** | 6.909 | 0.009 * | 9.096 | 0.003 * | 1.385 | 0.240 |
| DASS-Depression | 58.371 | <0.001 ** | 5.423 | 0.021 * | 2.200 | 0.139 | 0.506 | 0.478 |
| DASS-Anxiety | 70.281 | <0.001 ** | 14.018 | <0.001 ** | 8.006 | 0.005 * | 8.429 | 0.004 * |
| DASS-Stress | 122.702 | <0.001 ** | 0.002 | 0.966 | 4.629 | 0.032 * | 4.702 | 0.031 * |
| Time | Working Frontline | Time * Working Frontline | Covariate (Years on the Job) | |||||
|---|---|---|---|---|---|---|---|---|
| Nurses | ||||||||
| F1,209 | p | F1,209 | p | F1,209 | p | F1,209 | p | |
| PSQI | 62.036 | <0.001 ** | 0.426 | 0.515 | 0.473 | 0.492 | 0.010 | 0.920 |
| PSQI-A | 54.284 | <0.001 ** | 0.016 | 0.900 | 1.372 | 0.243 | 0.620 | 0.432 |
| DASS-Depression | 55.638 | <0.001 ** | 0.737 | 0.392 | 11.282 | 0.001 * | 1.103 | 0.295 |
| DASS-Anxiety | 75.426 | <0.001 ** | 0.030 | 0.863 | 4.333 | 0.039 * | 5.733 | 0.018 * |
| DASS-Stress | 122.662 | <0.001 ** | 0.659 | 0.418 | 7.311 | 0.007 * | 4.265 | 0.040 * |
| Physicians | ||||||||
| F1,72 | p | F1,72 | p | F1,72 | p | F1,72 | p | |
| PSQI | 12.884 | 0.001 * | 0.586 | 0.446 | 0.784 | 0.379 | 0.090 | 0.765 |
| PSQI-A | 3.113 | 0.082 | 0.056 | 0.814 | 0.023 | 0.880 | 0.881 | 0.351 |
| DASS-Depression | 11.272 | 0.001 * | 4.327 | 0.041 | 0.554 | 0.463 | 2.391 | 0.126 |
| DASS-Anxiety | 10.900 | 0.001 * | 0.903 | 0.345 | 1.944 | 0.168 | 1.827 | 0.181 |
| DASS-Stress | 20.850 | <0.001 ** | 0.164 | 0.687 | 1.031 | 0.313 | 0.749 | 0.390 |
| Dependent Variables | Predictors | β | Coefficients of Partial Correlation | t | p |
|---|---|---|---|---|---|
| PSQI | |||||
| R = 0.249 adjusted R2 = 0.045 F = 3.707 p = 0.003 * | COVID-19 positivity | −0.024 | −0.021 | −0.356 | 0.722 |
| Forced quarantine | −0.006 | −0.005 | −0.082 | 0.934 | |
| COVID-19-infected relatives/friends | 0.001 | 0.001 | 0.017 | 0.986 | |
| Relatives/friends who have died from COVID-19 | 0.175 | 0.173 | 2.938 | 0.004 * | |
| Satisfaction with governmental measures | −0.173 | −0.175 | −2.974 | 0.003 * | |
| PSQI-A | |||||
| R = 0.307 adjusted R2 = 0.078 F = 5.849 p = <0.001 ** | COVID-19 positivity | −0.015 | −0.013 | −0.219 | 0.826 |
| Forced quarantine | −0.004 | −0.003 | −0.059 | 0.953 | |
| COVID-19-infected relatives/friends | −0.038 | −0.037 | −0.627 | 0.531 | |
| Relatives/friends who have died from COVID-19 | 0.229 | 0.228 | 3.928 | <0.001 ** | |
| Satisfaction with governmental measures | −0.209 | −0.213 | −3.651 | <0.001 ** | |
| DASS-Depression | |||||
| R = 0.319 adjusted R2 = 0.086 F = 6.355 p < 0.001 ** | COVID-19 positivity | 0.013 | 0.011 | 0.190 | 0.849 |
| Forced quarantine | −0.019 | −0.016 | −0.273 | 0.785 | |
| COVID-19-infected relatives/friends | −0.106 | −0.105 | −1.764 | 0.079 | |
| Relatives/friends who have died from COVID-19 | 0.163 | 0.164 | 2.794 | 0.006 * | |
| Satisfaction with governmental measures | −0.275 | −0.276 | −4.821 | <0.001 ** | |
| DASS-Anxiety | |||||
| R = 0.360 adjusted R2 = 0.114 F = 8.342 p < 0.001 ** | COVID-19 positivity | −0.016 | −0.015 | −0.250 | 0.803 |
| Forced quarantine | 0.021 | 0.018 | 0.307 | 0.759 | |
| COVID-19-infected relatives/friends | −0.065 | −0.066 | −1.102 | 0.271 | |
| Relatives/friends who have died from COVID-19 | 0.226 | 0.229 | 3.937 | <0.001 ** | |
| Satisfaction with governmental measures | −0.283 | −0.288 | −5.047 | <0.001 ** | |
| DASS-Stress | |||||
| R = 0.344 adjusted R2 = 0.102 F = 7.522 p < 0.001 ** | COVID-19 positivity | −0.003 | −0.003 | −0.051 | 0.959 |
| Forced quarantine | −0.013 | −0.011 | −0.185 | 0.853 | |
| COVID-19-infected relatives/friends | −0.041 | −0.041 | −0.681 | 0.497 | |
| Relatives/friends who have died from COVID-19 | 0.187 | 0.190 | 3.249 | 0.001 * | |
| Satisfaction with governmental measures | −0.292 | −0.295 | −5.170 | <0.001 ** |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alfonsi, V.; Scarpelli, S.; Gorgoni, M.; Couyoumdjian, A.; Rosiello, F.; Sandroni, C.; Corsi, R.; Pietrantonio, F.; De Gennaro, L. Healthcare Workers after Two Years of COVID-19: The Consequences of the Pandemic on Psychological Health and Sleep among Nurses and Physicians. Int. J. Environ. Res. Public Health 2023, 20, 1410. https://doi.org/10.3390/ijerph20021410
Alfonsi V, Scarpelli S, Gorgoni M, Couyoumdjian A, Rosiello F, Sandroni C, Corsi R, Pietrantonio F, De Gennaro L. Healthcare Workers after Two Years of COVID-19: The Consequences of the Pandemic on Psychological Health and Sleep among Nurses and Physicians. International Journal of Environmental Research and Public Health. 2023; 20(2):1410. https://doi.org/10.3390/ijerph20021410
Chicago/Turabian StyleAlfonsi, Valentina, Serena Scarpelli, Maurizio Gorgoni, Alessandro Couyoumdjian, Francesco Rosiello, Cinzia Sandroni, Roberto Corsi, Filomena Pietrantonio, and Luigi De Gennaro. 2023. "Healthcare Workers after Two Years of COVID-19: The Consequences of the Pandemic on Psychological Health and Sleep among Nurses and Physicians" International Journal of Environmental Research and Public Health 20, no. 2: 1410. https://doi.org/10.3390/ijerph20021410
APA StyleAlfonsi, V., Scarpelli, S., Gorgoni, M., Couyoumdjian, A., Rosiello, F., Sandroni, C., Corsi, R., Pietrantonio, F., & De Gennaro, L. (2023). Healthcare Workers after Two Years of COVID-19: The Consequences of the Pandemic on Psychological Health and Sleep among Nurses and Physicians. International Journal of Environmental Research and Public Health, 20(2), 1410. https://doi.org/10.3390/ijerph20021410