The Impact of Health and Social Care Professionals’ Education on the Quality of Serious Illness Conversations in Nursing Homes: Study Protocol of a Quality Improvement Project
Abstract
1. Introduction
2. Research Methods and Analysis
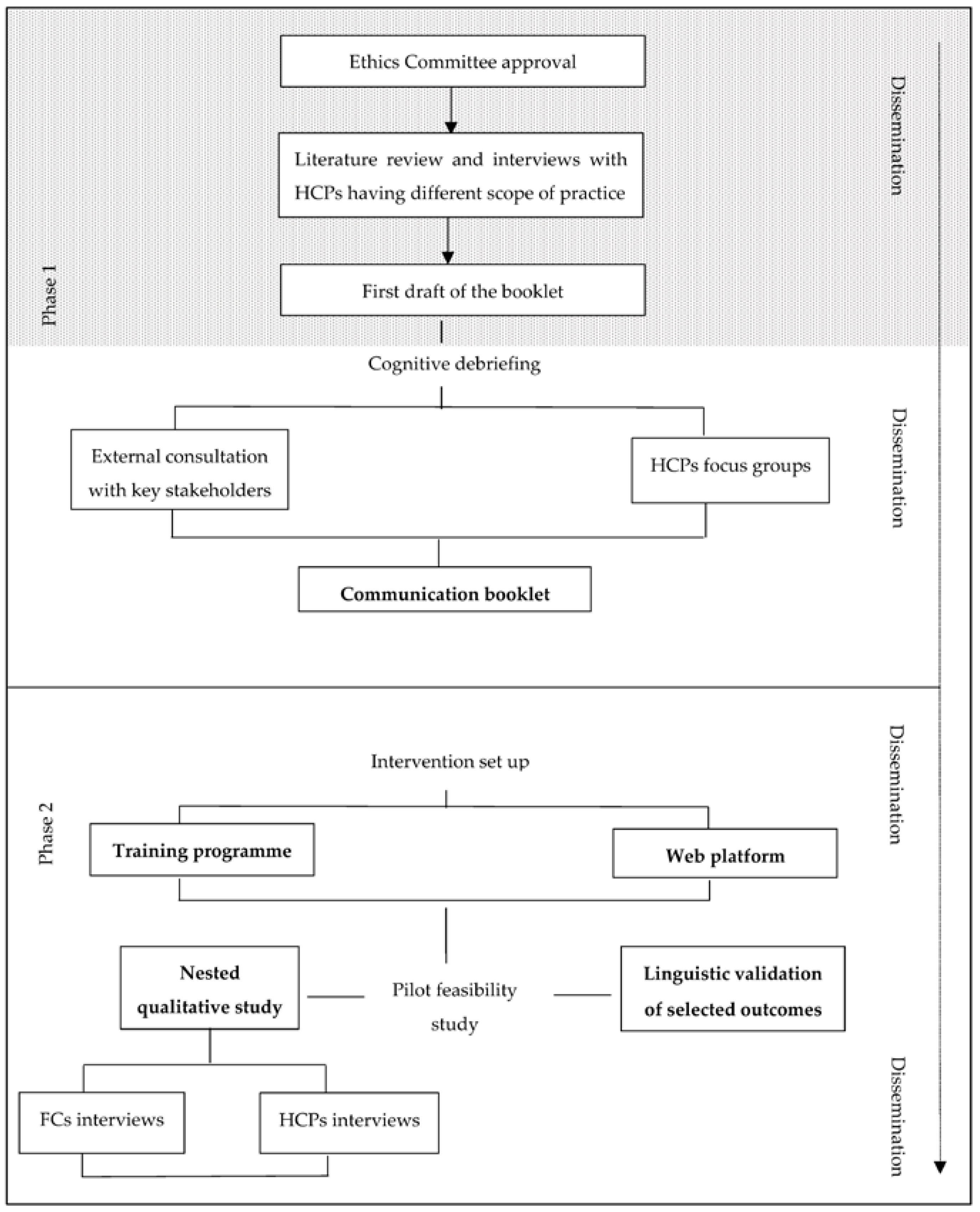
2.1. Study Design
2.1.1. Phase 1. Development of Written Resources
- ➢
- To determine how many healthcare professionals attend the training program compared to the eligible.
- ➢
- To determine how many participating healthcare professionals complete the 6-month training program.
- ➢
- To explore when the family meetings are conducted (i.e., working time vs off duty) and estimate the number of family meetings over a 6-month period.
- ➢
- To determine how many family carers of nursing home residents participate in the study.
- ➢
- To estimate refusal rate and 6-month follow-up rates.
- ➢
- To assess, qualitatively, the intervention delivery, implementation barriers, and suggestions for improvement.
- ➢
- To estimate the quality of communication perceived by family carers at 6-month follow-up (primary study outcome).
- ➢
- To assess changes in secondary outcome measures.
- ➢
- To inform the sample size estimation for subsequent studies.
Development of the Booklet
Assessment of the Booklet: Acceptability, Usefulness, and Feasibility to Use in Daily Practice
2.1.2. Phase 2. Multicenter Pilot Feasibility Pre-Post Study with Nested Qualitative Study
- (i)
- Intervention set up
Training Program
- First module (6 h, residential event): (a) a 2-h lecture on the clinical and ethical principles of end-of-life communication, general and situation-specific communication strategies, and content and use of the communication booklet (output of phase 1); (b) a brainstorming session on successful and failed communication; (c) videos pointing out different communication challenges and communication skills abilities; (d) a small group-based reflective discussion.
- 2.
- Second module (within 3 months from the first module, 4 h):
- a.
- Experiential workshop based on improvisational theater techniques (3 h) [34]. Trained team members acting as HCPs and patients will role-play difficult conversations. The scripts will be based on previous interviews with HCPs who work in NH to identify real-world situations. A facilitator will introduce the actors and encourage participants to note parts of the dialogue that do not help us overcome difficult conversations. Participants will be asked for their feedback, including specific parts of the dialogue that could be improved. The scene will be reenacted, and participants will be encouraged to shout “stop” if they want to change the HCP dialogue. When a participant yells “stop”, the performance will be suspended, and the facilitator will ask the person the reason(s) why they have interrupted the performance and to assume the role of the HCP and use the suggested approach, becoming a spectator-actor. After the performance, the facilitator will ask the spectator-actors if they have carried out what they planned and ask the audience to comment on the performance of the spectator-actors. The critics of the performance will be asked to explain what they would do differently and will be invited to play the encounter, including their suggestions. These scenarios will be repeated several times to allow most participants to practice these difficult conversations.
- b.
- Community of practice I (1 h): at the end of the experiential workshop, a member of the care team will facilitate a community of practice. Participants will share the feelings and challenges they experienced while playing the encounter. The facilitator will foster reflection on the difficulties in applying suggestions and communication protocols effectively in a real situation.
- 3.
- Third module (from 3 to 6 months from the first module, 10 h):
- a.
- On-site training (2 h): participants will conduct at least two family meetings in their clinical setting in a quiet room using the communication booklet. The care team will identify those family carers who could benefit from a family meeting and its goals (for example, communication of their relative’s worsening conditions). Family meetings must be planned and agreed with family carers in advance and may be conducted during the working time because they are part of good clinical practice; no minimum or maximum duration is set, and the duration depends on the specific situation.
- b.
- Community of practice II (4 h, in-presence or technology-based according to the facility preferences): a member of the care team will facilitate the community of practice. Participants will share problems that emerged during the family meetings and the strategies employed to overcome them in a community of practice encounter, followed by collective reflection. This final session is reserved for those who have completed all activities including at least two family meetings and self-learning activities (see paragraph web platform). Each participant will self-certify that they have conducted the minimum number of family meetings required.
Web Platform
Linguistic Validation of Measures
- (ii)
- Pilot pre-post study
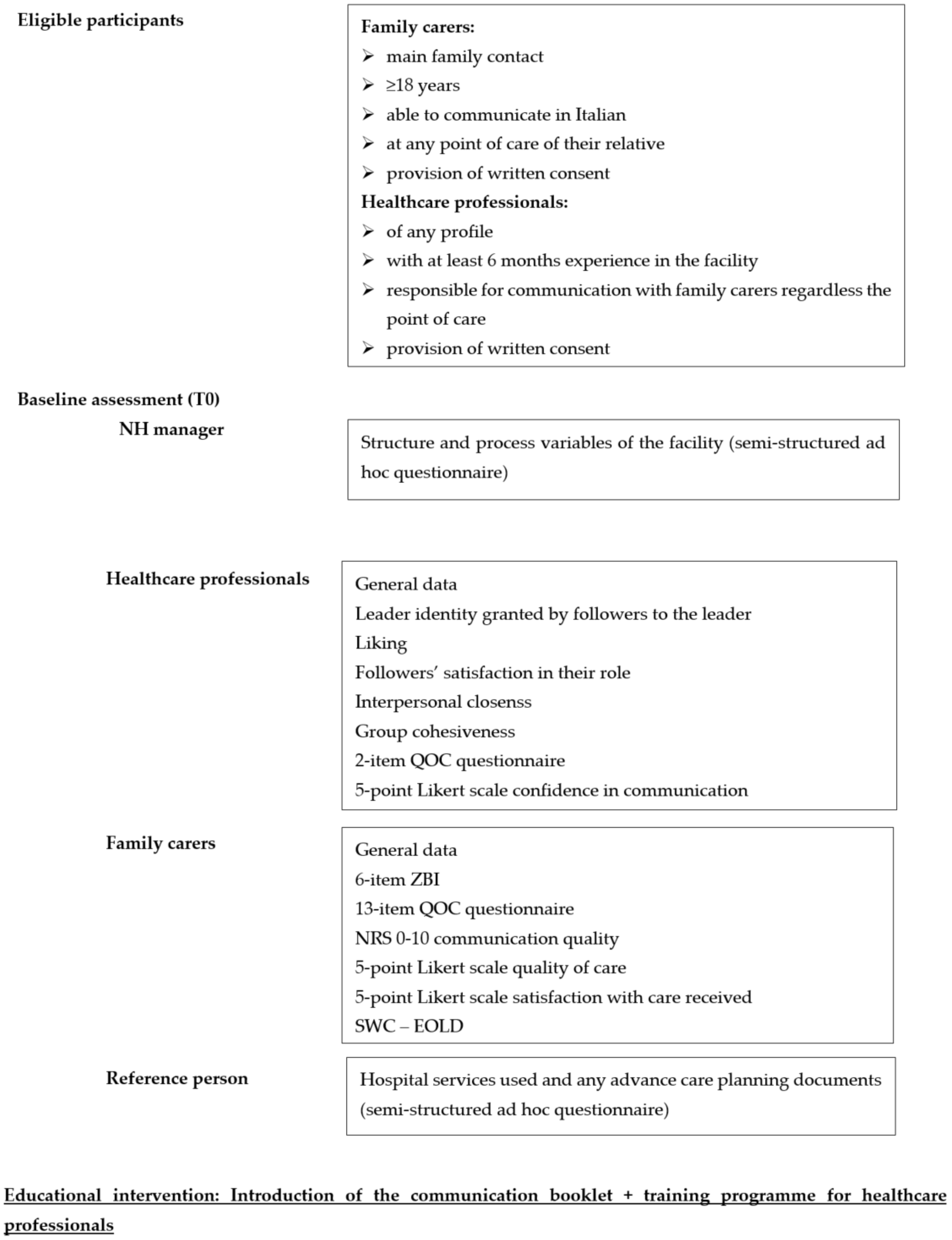
Eligibility and Screening
Baseline Assessment (T0)
Educational Intervention
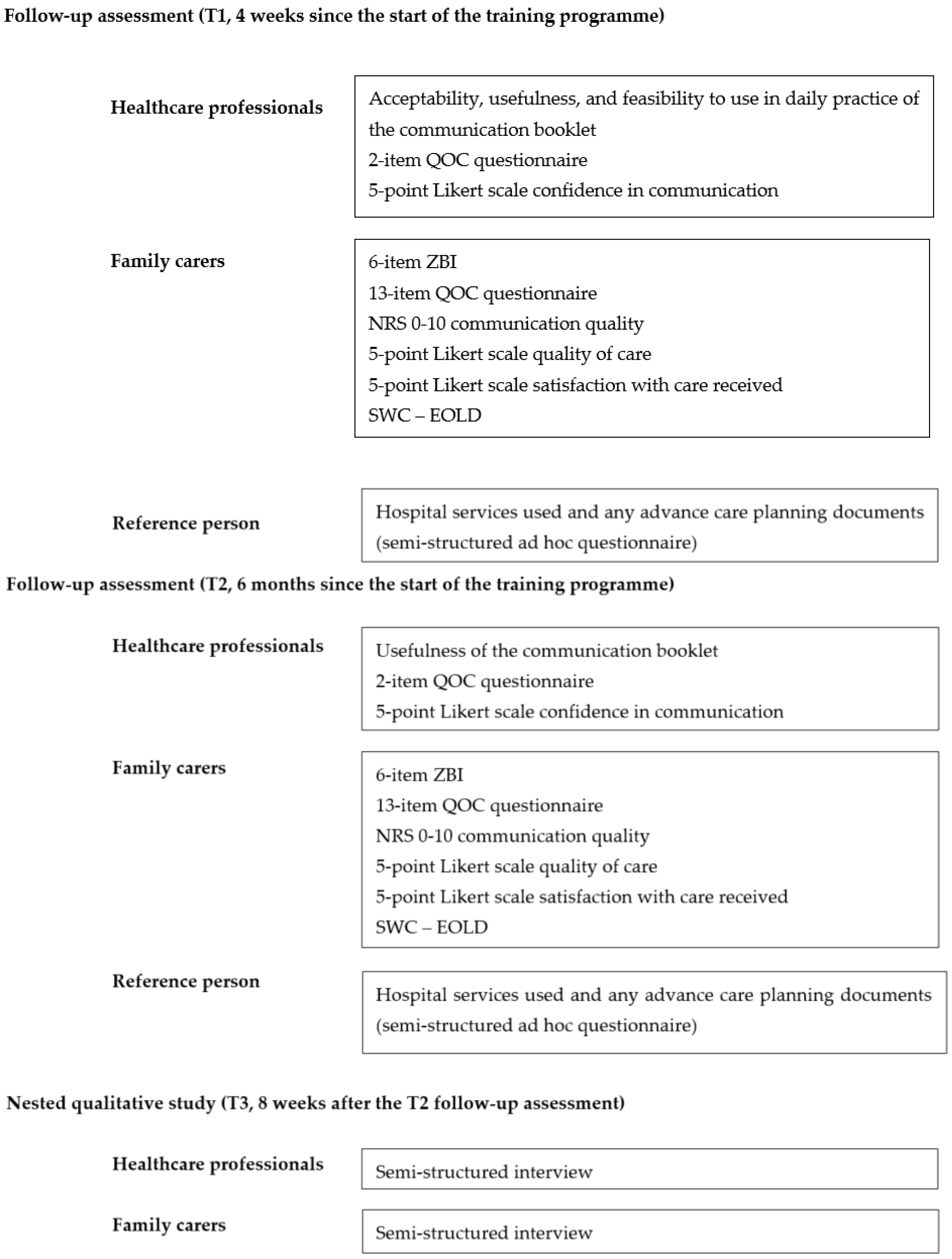
Follow-Up Assessment (T1, T2)
Outcome Measures
Quality of communication
Other Outcome Measures
Kick off and over-the-Project Meetings
- (iii)
- Nested qualitative study (T3)
2.2. Study Power
2.3. Data Analysis
2.3.1. Quantitative Data
2.3.2. Qualitative Data
2.4. Data Management
2.5. Public Involvement
3. Discussion
Limitations
4. Ethics and Dissemination
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Ekberg, S.; Parry, R.; Land, V.; Ekberg, K.; Pino, M.; Antaki, C.; Jenkins, L.; Whittaker, B. Communicating with patients and families about illness progression and end of life: A review of studies using direct observation of clinical practice. BMC Palliat. Care 2021, 20, 186. [Google Scholar] [CrossRef] [PubMed]
- Gonella, S.; Basso, I.; Dimonte, V.; Martin, B.; Berchialla, P.; Campagna, S.; Di Giulio, P. Association between end-of-life conversations in nursing homes and end-of-life care outcomes: A systematic review and meta-analysis. J. Am. Med. Dir. Assoc. 2019, 20, 249–261. [Google Scholar] [CrossRef] [PubMed]
- Toles, M.; Song, M.K.; Lin, F.C.; Hanson, L.C. Perceptions of family decision-makers of nursing home residents with advanced dementia regarding the quality of communication around end-of-life care. J. Am. Med. Dir. Assoc. 2018, 19, 879–883. [Google Scholar] [CrossRef] [PubMed]
- Wendrich-van Dael, A.; Bunn, F.; Lynch, J.; Pivodic, L.; Van den Block, L.; Goodman, C. Advance care planning for people living with dementia: An umbrella review of effectiveness and experiences. Int. J. Nurs. Stud. 2020, 107, 103576. [Google Scholar] [CrossRef] [PubMed]
- Gonella, S.; Basso, I.; Dimonte, V.; Di Giulio, P. The role of end-of-life communication in contributing to palliative-oriented care at the end-of-life in nursing home. Int. J. Palliat. Nurs. 2022, 28, 16–26. [Google Scholar] [CrossRef]
- De Vleminck, A.; Pardon, K.; Beernaert, K.; Deschepper, R.; Houttekier, D.; Van Audenhove, C.; Deliens, L.; Vander Stichele, R. Barriers to advance care planning in cancer, heart failure and dementia patients: A focus group study on general practitioners’ views and experiences. PLoS ONE 2014, 9, e84905. [Google Scholar] [CrossRef]
- Gonella, S.; Di Giulio, P.; Antal, A.; Cornally, N.; Martin, P.; Campagna, S.; Dimonte, V. Challenges experienced by Italian nursing home staff in end-of-life conversations with family caregivers during COVID-19 pandemic: A qualitative descriptive study. Int. J. Environ. Res. Public Health 2022, 19, 2504. [Google Scholar] [CrossRef]
- Travers, A.; Taylor, V. What are the barriers to initiating end-of-life conversations with patients in the last year of life? Int. J. Palliat. Nurs. 2016, 22, 454–462. [Google Scholar] [CrossRef]
- Martin, E.B., Jr.; Mazzola, N.M.; Brandano, J.; Luff, D.; Zurakowski, D.; Meyer, E.C. Clinicians’ recognition and management of emotions during difficult healthcare conversations. Patient Educ. Couns. 2015, 98, 1248–1254. [Google Scholar] [CrossRef] [PubMed]
- Reinke, L.F.; Feemster, L.C.; McDowell, J.; Gunnink, E.; Tartaglione, E.V.; Udris, E.; Curtis, J.R.; Au, D.H. The long term impact of an end-of-life communication intervention among veterans with COPD. Heart Lung 2017, 46, 30–34. [Google Scholar] [CrossRef]
- Morin, L.; Johnell, K.; Van den Block, L.; Aubry, R. Discussing end-of-life issues in nursing homes: A nationwide study in France. Age Ageing 2016, 45, 395–402. [Google Scholar] [CrossRef] [PubMed]
- Brighton, L.J.; Koffman, J.; Hawkins, A.; McDonald, C.; O’Brien, S.; Robinson, V.; Khan, S.A.; George, R.; Higginson, I.J.; Selman, L.E. A systematic review of end-of-life care communication skills training for generalist palliative care providers: Research quality and reporting guidance. J. Pain Symptom Manag. 2017, 54, 417–425. [Google Scholar] [CrossRef] [PubMed]
- Chung, H.O.; Oczkowski, S.J.; Hanvey, L.; Mbuagbaw, L.; You, J.J. Educational interventions to train healthcare professionals in end-of-life communication: A systematic review and meta-analysis. BMC Med. Educ. 2016, 16, 131. [Google Scholar] [CrossRef] [PubMed]
- Borghi, L.; Meyer, E.C.; Vegni, E.; Oteri, R.; Almagioni, P.; Lamiani, G. Twelve years of the Italian Program to Enhance Relational and Communication Skills (PERCS). Int. J. Environ. Res. Public Health 2021, 18, 439. [Google Scholar] [CrossRef] [PubMed]
- Bristowe, K.; Shepherd, K.; Bryan, L.; Brown, H.; Carey, I.; Matthews, B.; O’Donoghue, D.; Vinen, K.; Murtagh, F.E. The development and piloting of the REnal specific Advanced Communication Training (REACT) programme to improve Advance Care Planning for renal patients. Palliat. Med. 2014, 28, 360–366. [Google Scholar] [CrossRef]
- Curtis, J.R.; Back, A.L.; Ford, D.W.; Downey, L.; Shannon, S.E.; Doorenbos, A.Z.; Kross, E.K.; Reinke, L.F.; Feemster, L.C.; Edlund, B.; et al. Effect of communication skills training for residents and nurse practitioners on quality of communication with patients with serious illness: A randomized trial. JAMA 2013, 310, 2271–2281. [Google Scholar] [CrossRef]
- Dunlay, S.M.; Foxen, J.L.; Cole, T.; Feely, M.A.; Loth, A.R.; Strand, J.J.; Wagner, J.A.; Swetz, K.M.; Redfield, M.M. A survey of clinician attitudes and self-reported practices regarding end-of-life care in heart failure. Palliat. Med. 2015, 29, 260–267. [Google Scholar] [CrossRef]
- Powazki, R.; Walsh, D.; Cothren, B.; Rybicki, L.; Thomas, S.; Morgan, G.; Karius, D.; Davis, M.P.; Shrotriya, S. The care of the actively dying in an academic medical center: A survey of registered nurses’ professional capability and comfort. Am. J. Hosp. Palliat. Med. 2014, 31, 619–627. [Google Scholar] [CrossRef]
- Lamiani, G.; Meyer, E.C.; Leone, D.; Vegni, E.; Browning, D.M.; Rider, E.A.; Truog, R.D.; Moja, E.A. Cross-cultural adaptation of an innovative approach to learning about difficult conversations in healthcare. Med. Teach. 2011, 33, e57–e64. [Google Scholar] [CrossRef]
- Bell, S.K.; Langer, T.; Luff, D.; Rider, E.A.; Brandano, J.; Meyer, E.C. Interprofessional learning to improve communication in challenging healthcare conversations: What clinicians learn from each other. J. Contin. Educ. Health Prof. 2019, 39, 201–209. [Google Scholar] [CrossRef]
- Bays, A.M.; Engelberg, R.A.; Back, A.L.; Ford, D.W.; Downey, L.; Shannon, S.E.; Doorenbos, A.Z.; Edlund, B.; Christianson, P.; Arnold, R.W.; et al. Interprofessional communication skills training for serious illness: Evaluation of a small-group, simulated patient intervention. J. Palliat. Med. 2014, 17, 159–166. [Google Scholar] [CrossRef] [PubMed]
- Salmon, P.; Young, B. Creativity in clinical communication: From communication skills to skilled communication. Med. Educ. 2011, 45, 217–226. [Google Scholar] [CrossRef] [PubMed]
- Eggenberger, E.; Heimerl, K.; Bennett, M.I. Communication skills training in dementia care: A systematic review of effectiveness, training content, and didactic methods in different care settings. Int. Psychogeriatr. 2013, 25, 345–358. [Google Scholar] [CrossRef] [PubMed]
- Stiefel, F.; Barth, J.; Bensing, J.; Fallowfield, L.; Jost, L.; Razavi, D.; Kiss, A. Communication skills training in oncology: A position paper based on a consensus meeting among European experts in 2009. Ann. Oncol. 2010, 21, 204–207. [Google Scholar] [CrossRef] [PubMed]
- Rubinelli, S.; Myers, K.; Rosenbaum, M.; Davis, D. Implications of the current COVID-19 pandemic for communication in healthcare. Patient Educ. Couns. 2020, 103, 1067–1069. [Google Scholar] [CrossRef]
- Flint, L.; Kotwal, A. The new normal: Key considerations for effective serious illness communication over video or telephone during the Coronavirus Disease 2019 (COVID-19) Pandemic. Ann. Intern. Med. 2020, 173, 486–488. [Google Scholar] [CrossRef]
- Browning, D.M.; Meyer, E.C.; Truog, R.D.; Solomon, M.Z. Difficult conversations in health care: Cultivating relational learning to address the hidden curriculum. Acad. Med. 2007, 82, 905–913. [Google Scholar] [CrossRef]
- Chan, A.W.; Tetzlaff, J.M.; Altman, D.G.; Laupacis, A.; Gøtzsche, P.C.; Krleža-Jerić, K.; Hróbjartsson, A.; Mann, H.; Dickersin, K.; Berlin, J.A.; et al. SPIRIT 2013 statement: Defining standard protocol items for clinical trials. Ann. Intern. Med. 2013, 158, 200–207. [Google Scholar] [CrossRef] [PubMed]
- Des Jarlais, D.C.; Lyles, C.; Crepaz, N. Improving the reporting quality of nonrandomized evaluations of behavioral and public health interventions: The TREND statement. Am. J. Public Health 2004, 94, 361–366. [Google Scholar] [CrossRef]
- Tong, A.; Sainsbury, P.; Craig, J. Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int. J. Qual. Health Care 2007, 19, 349–357. [Google Scholar] [CrossRef]
- O’Connor, A.M. Cranney A: Patient Decision Aids—Evaluation Measures. User Manual for Acceptability; University of Ottawa, Ottawa Hospital Research Institute: Ottawa, ON, Canada, 2002; Available online: http://decisionaid.ohri.ca/docs/develop/User_Manuals/UM_Acceptability.pdf (accessed on 30 October 2021).
- Surr, C.A.; Gates, C.; Irving, D.; Oyebode, J.; Smith, S.J.; Parveen, S.; Drury, M.; Dennison, A. Effective dementia education and training for the health and social care workforce: A systematic review of the literature. Rev. Educ. Res. 2017, 87, 966–1002. [Google Scholar] [CrossRef] [PubMed]
- Schmitz, F.M.; Schnabel, K.P.; Stricker, D.; Fischer, M.R.; Guttormsen, S. Learning communication from erroneous video-based examples: A double-blind randomised controlled trial. Patient Educ. Couns. 2017, 100, 1203–1212. [Google Scholar] [CrossRef] [PubMed]
- Cullen, J.P.; Russ, S.; Russell, H.A. Theater for vaccine hesitancy—Setting the stage for difficult conversations. JAMA 2022, 328, 1018–1019. [Google Scholar] [CrossRef] [PubMed]
- Beaton, D.E.; Bombardier, C.; Guillemin, F.; Ferraz, M.B. Guidelines for the process of cross-cultural adaptation of self-report measures. Spine 2000, 25, 3186–3191. [Google Scholar] [CrossRef]
- Engelberg, R.; Downey, L.; Curtis, J.R. Psychometric characteristics of a quality of communication questionnaire assessing communication about end-of-life care. J. Palliat. Med. 2006, 9, 1086–1098. [Google Scholar] [CrossRef]
- Volicer, L.; Hurley, A.C.; Blasi, Z.V. Scales for evaluation of end-of-life care in dementia. Alzheimer Dis. Assoc. Disord. 2001, 15, 194–200. [Google Scholar] [CrossRef]
- Merla, C.; Wickson-Griffiths, A.; Kaasalainen, S.; Dal Bello-Haas, V.; Banfield, L.; Hadjistavropoulos, T.; Di Sante, E. Perspective of family members of transitions to alternative levels of care in Anglo-Saxon countries. Curr. Gerontol. Geriatr. Res. 2018, 2018, 4892438. [Google Scholar] [CrossRef]
- Gonella, S.; Clari, M.; Basso, I.; Di Giulio, P. What contributes to family carers’ decision to transition towards palliative-oriented care for their relatives in nursing homes? Qualitative findings from bereaved family carers’ experiences. Palliat. Support Care 2021, 19, 208–216. [Google Scholar] [CrossRef]
- White, N.; Kupeli, N.; Vickerstaff, V.; Stone, P. How accurate is the ‘Surprise Question’ at identifying patients at the end of life? A systematic review and meta-analysis. BMC Med. 2017, 15, 139. [Google Scholar] [CrossRef]
- Aron, A.; Aron, E.N.; Smollan, D. Inclusion of other in the self scale and the structure of interpersonal closeness. J. Personal. Soc. Psychol. 1992, 63, 596–612. [Google Scholar] [CrossRef]
- Dobbins, G.H.; Zaccaro, S.J. The effects of group cohesion and leader behavior on subordinate satisfaction. Group Organ. Stud. 1986, 11, 203–219. [Google Scholar] [CrossRef]
- Martinko, M.J.; Mackey, J.D.; Moss, S.E.; Harvey, P.; McAllister, C.P.; Brees, J.R. An exploration of the role of subordinate affect in leader evaluations. J. Appl. Psychol. 2018, 103, 738. [Google Scholar] [CrossRef] [PubMed]
- Gatti, P.; Hall, R.; Schyns, B. ‘Talking aloud’: Voice behaviors as an antecedent of satisfaction with supervisors and followers’ satisfaction with their role. In Proceedings of the Paper presented at the EAWOP—17th European Congress of Work and Organizational Psychology: Respectful and effective leadership. Managing People and Organizations in Turbulent Times, Oslo, Norway, 20–23 May 2015. [Google Scholar]
- Hébert, R.; Bravo, G.; Préville, M. Reliability, validity and reference values of the Zarit Burden Interview for assessing informal caregivers of community-dwelling older persons with dementia. Can. J. Aging 2000, 19, 494–507. [Google Scholar] [CrossRef]
- Chattat, R.; Cortesi, V.; Izzicupo, F.; Del Re, M.L.; Sgarbi, C.; Fabbo, A.; Bergonzini, E. The Italian version of the Zarit Burden interview: A validation study. Int. Psychogeriatr. 2011, 23, 797–805. [Google Scholar] [CrossRef] [PubMed]
- Guest, G.; Bunce, A.; Johnson, L. How many interviews are enough? An experiment with data saturation and variability. Field Methods 2006, 18, 59–82. [Google Scholar] [CrossRef]
- Graneheim, U.H.; Lundman, B. Qualitative content analysis in nursing research: Concepts, procedures and measures to achieve trustworthiness. Nurse Educ. Today 2004, 24, 105–112. [Google Scholar] [CrossRef]
- Hendricksen, M.; Mitchell, S.L.; Lopez, R.P.; Mazor, K.M.; McCarthy, E.P. Facility characteristics associated with intensity of care of nursing homes and hospital referral regions. J. Am. Med. Dir. Assoc. 2022, 23, 1367–1374. [Google Scholar] [CrossRef]
- Zoppi, K.; Epstein, R.M. Is communication a skill? Communication behaviors and being in relation. Fam. Med. 2002, 34, 319–324. [Google Scholar] [CrossRef][Green Version]
- Mitchell, T.D.; Richard, F.D.; Battistoni, R.M.; Rost-Banik, C.; Netz, R.; Zakoske, C. Reflective practice that persists: Connections between reflection in service-learning programs and in current life. Mich. J. Community Serv. Learn. 2015, 21, 49–63. [Google Scholar]
- Cheng, A.; LaDonna, K.; Cristancho, S.; Ng, S. Navigating difficult conversations: The role of self-monitoring and reflection-in-action. Med. Educ. 2017, 51, 1220–1231. [Google Scholar] [CrossRef]
- Anstey, S.; Powell, T.; Coles, B.; Hale, R.; Gould, D. Education and training to enhance end-of-life care for nursing home staff: A systematic literature review. BMJ Support Palliat. Care 2016, 6, 353–361. [Google Scholar] [CrossRef]
- van der Steen, J.T.; Radbruch, L.; Hertogh, C.M.; de Boer, M.E.; Hughes, J.C.; Larkin, P.; Francke, A.L.; Jünger, S.; Gove, D.; Firth, P.; et al. White paper defining optimal palliative care in older people with dementia: A Delphi study and recommendations from the European Association for Palliative Care. Palliat. Med. 2014, 28, 197–209. [Google Scholar] [CrossRef] [PubMed]
- Donesky, D.; Anderson, W.G.; Joseph, R.D.; Sumser, B.; Reid, T.T. TeamTalk: Interprofessional team development and communication skills training. J. Palliat. Med. 2020, 23, 40–47. [Google Scholar] [CrossRef] [PubMed]
- Anderson, R.J.; Bloch, S.; Armstrong, M.; Stone, P.C.; Low, J.T. Communication between healthcare professionals and relatives of patients approaching the end-of-life: A systematic review of qualitative evidence. Palliat. Med. 2019, 33, 926–941. [Google Scholar] [CrossRef] [PubMed]
- Rietjens, J.A.C.; Sudore, R.L.; Connolly, M.; van Delden, J.J.; Drickamer, M.A.; Droger, M.; van der Heide, A.; Heyland, D.K.; Houttekier, D.; Janssen, D.J.A.; et al. Definition and recommendations for advance care planning: An international consensus supported by the European Association for Palliative Care. Lancet Oncol. 2017, 18, e543–e551. [Google Scholar] [CrossRef] [PubMed]
- Sudore, R.L.; Lum, H.D.; You, J.J.; Hanson, L.C.; Meier, D.E.; Pantilat, S.Z.; Matlock, D.D.; Rietjens, J.A.C.; Korfage, I.J.; Ritchie, C.S.; et al. Defining Advance Care Planning for adults: A consensus definition from a multidisciplinary delphi panel. J. Pain Symptom Manag. 2017, 53, 821–832.e1. [Google Scholar] [CrossRef]
- Payne, C.; Brown, M.J.; Guerin, S.; Kernohan, W.G. EMTReK: An Evidence-based Model for the Transfer & Exchange of Research Knowledge-five case studies in palliative care. SAGE Open Nurs. 2019, 5, 2377960819861854. [Google Scholar]
| Tool(s) | Assessor | Construct | Author |
|---|---|---|---|
| Followers’ satisfaction in their role | HCPs | Relationship with the leadership | Gatti, Hall & Schyns, 2014 [44] |
| Interpersonal closeness | HCPs | Relationship with colleagues | Aron, 1992 [41] |
| Leader Identity granted by followers to the leader | HCPs | Relationship with the leadership | Lord and Gatti [personal communication 2018] |
| Liking—The Leader Affect Questionnaires | HCPs | Relationship with the leadership | Martinko, Mackey, Moss, Harvey, McAllister, Brees, 2018 [43] |
| Group cohesiveness | HCPs | Relationship with colleagues | Dobbins & Zaccaro, 1986 [42] |
| Semi-structured ad hoc questionnaire | NH manager | Structure and process variables of the NH | - |
| Tool(s) | Assessor | Construct | Author | Italian Version | Timing |
|---|---|---|---|---|---|
| 2-item QOC questionnaire | HCPs | Quality of communication | Engelberg et al., 2006 [36] | Solari et al. [in validation] | T0/T1/T2 |
| 5-point Likert scale | Family carers | Quality of care | - | - | T0/T1/T2 |
| 5-point Likert scale | Family carers | Satisfaction with the care received | - | - | T0/T1/T2 |
| 5-point Likert scale | HCPs | Confidence in communication | - | - | T0/T1/T2 |
| NRS 0–10 | Family carers | Quality of communication | - | - | T0/T1/T2 |
| 13-item QOC questionnaire | Family carers | Quality of communication | Engelberg et al., 2006 [36] | - | T0/T1/T2 * |
| Semi-structured ad hoc questionnaire | Reference person | Hospital services used, advance care planning documents | - | - | T0/T1/T2 |
| Semi-structured interview | Family carers | Intervention quality, implementation barriers, and suggestions for improvement | - | - | T3 |
| Semi-structured interview | HCPs | Intervention quality, implementation barriers, and suggestions for improvement | - | - | T3 |
| SWC-EOLD | Family carers | Satisfaction with the care received | Volicer et al., 2001 [37] | - | T0/T1/T2 |
| ZBI | Family carers | Family carers burden | Hebert et al., 2000 [45] | Chattat et al., 2011 [46] | T0/T1/T2 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gonella, S.; Di Giulio, P.; Berchialla, P.; Bo, M.; Cotogni, P.; Macchi, G.; Campagna, S.; Dimonte, V. The Impact of Health and Social Care Professionals’ Education on the Quality of Serious Illness Conversations in Nursing Homes: Study Protocol of a Quality Improvement Project. Int. J. Environ. Res. Public Health 2023, 20, 725. https://doi.org/10.3390/ijerph20010725
Gonella S, Di Giulio P, Berchialla P, Bo M, Cotogni P, Macchi G, Campagna S, Dimonte V. The Impact of Health and Social Care Professionals’ Education on the Quality of Serious Illness Conversations in Nursing Homes: Study Protocol of a Quality Improvement Project. International Journal of Environmental Research and Public Health. 2023; 20(1):725. https://doi.org/10.3390/ijerph20010725
Chicago/Turabian StyleGonella, Silvia, Paola Di Giulio, Paola Berchialla, Mario Bo, Paolo Cotogni, Giorgia Macchi, Sara Campagna, and Valerio Dimonte. 2023. "The Impact of Health and Social Care Professionals’ Education on the Quality of Serious Illness Conversations in Nursing Homes: Study Protocol of a Quality Improvement Project" International Journal of Environmental Research and Public Health 20, no. 1: 725. https://doi.org/10.3390/ijerph20010725
APA StyleGonella, S., Di Giulio, P., Berchialla, P., Bo, M., Cotogni, P., Macchi, G., Campagna, S., & Dimonte, V. (2023). The Impact of Health and Social Care Professionals’ Education on the Quality of Serious Illness Conversations in Nursing Homes: Study Protocol of a Quality Improvement Project. International Journal of Environmental Research and Public Health, 20(1), 725. https://doi.org/10.3390/ijerph20010725











