Morphological Characteristics and Prevention of Tooth Enamel Demineralization during Orthodontic Treatment with Non-Removable Appliances
Abstract
1. Introduction
2. Materials and Methods
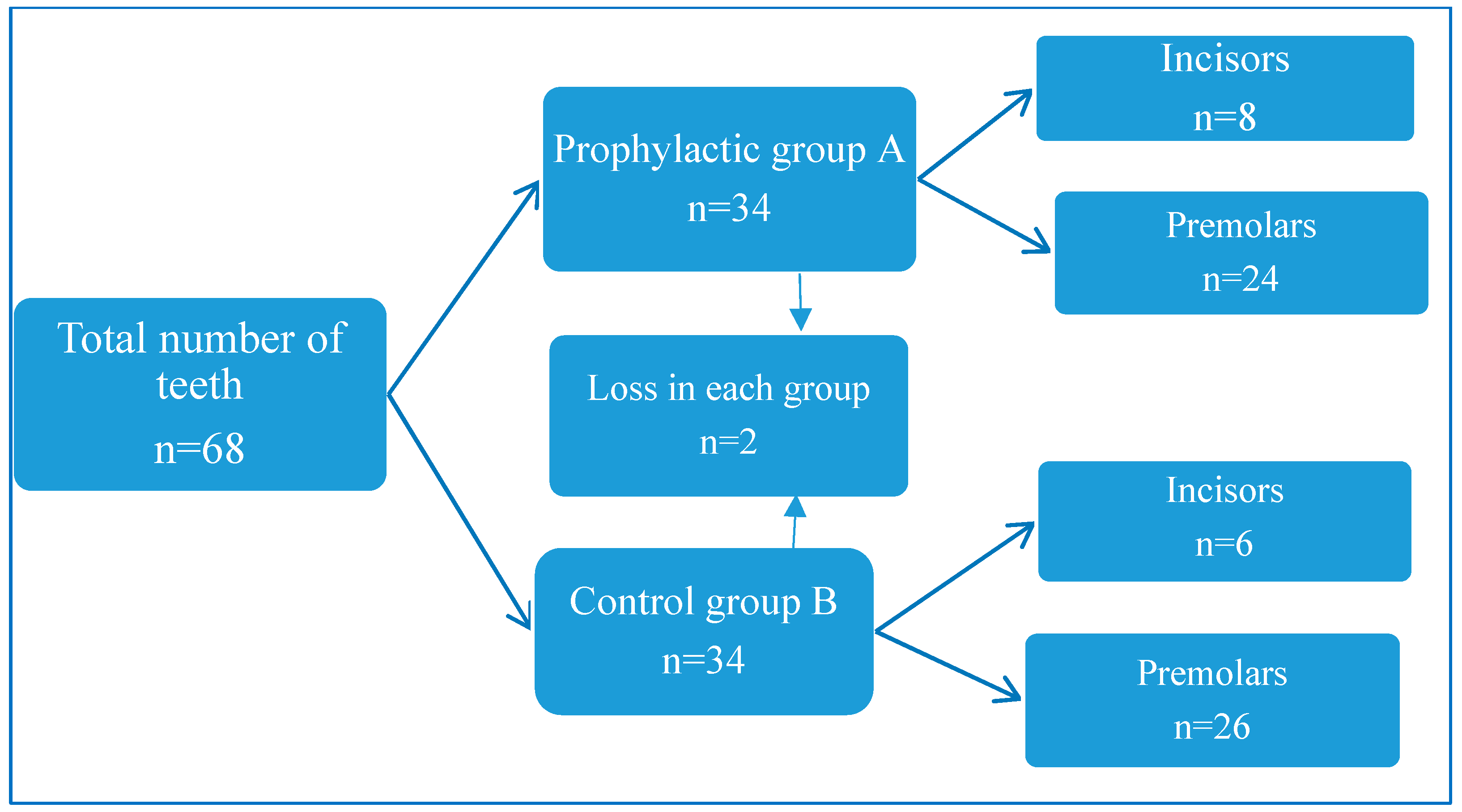
2.1. Study Design
2.2. In Vitro Study
2.3. Artificial Caries Induction
2.4. Morphological Study
- Decalcification for 3 days in 5% nitric acid solution.
- Washing with running tap water during the day 5–6 times to remove the acid solution.
- Washed tissues were transferred to alcohol solutions of increasing concentrations for the dehydration procedure.
- After dehydration, a cleaning procedure was carried out by soaking in a xylol solution.
- The cleaned tissues were transferred into soft paraffin (melting point 46–48 °C).
- Then they were blocked by pouring into hard paraffin (melting point 56–58 °C).
- Preparation of 5 µm, 7 µm, and 10 µm thick sagittal sections taken from blocked tissues by means of a rotary microtome (Leitz, Wetzlar, Germany).
- Staining with Ehrlich’s hematoxylin for 5–10 min.
- After staining, the sections were dehydrated and covered with a coverslip [26].
2.5. Exclusion Criteria of Clinical Study
- The presence of white spots on the teeth before fixing the braces.
- Refusal of the patient or parents to participate in the study.
- Ineligibility for the studied age groups.
2.6. In Vivo Study
2.7. Statistical Analysis
3. Results
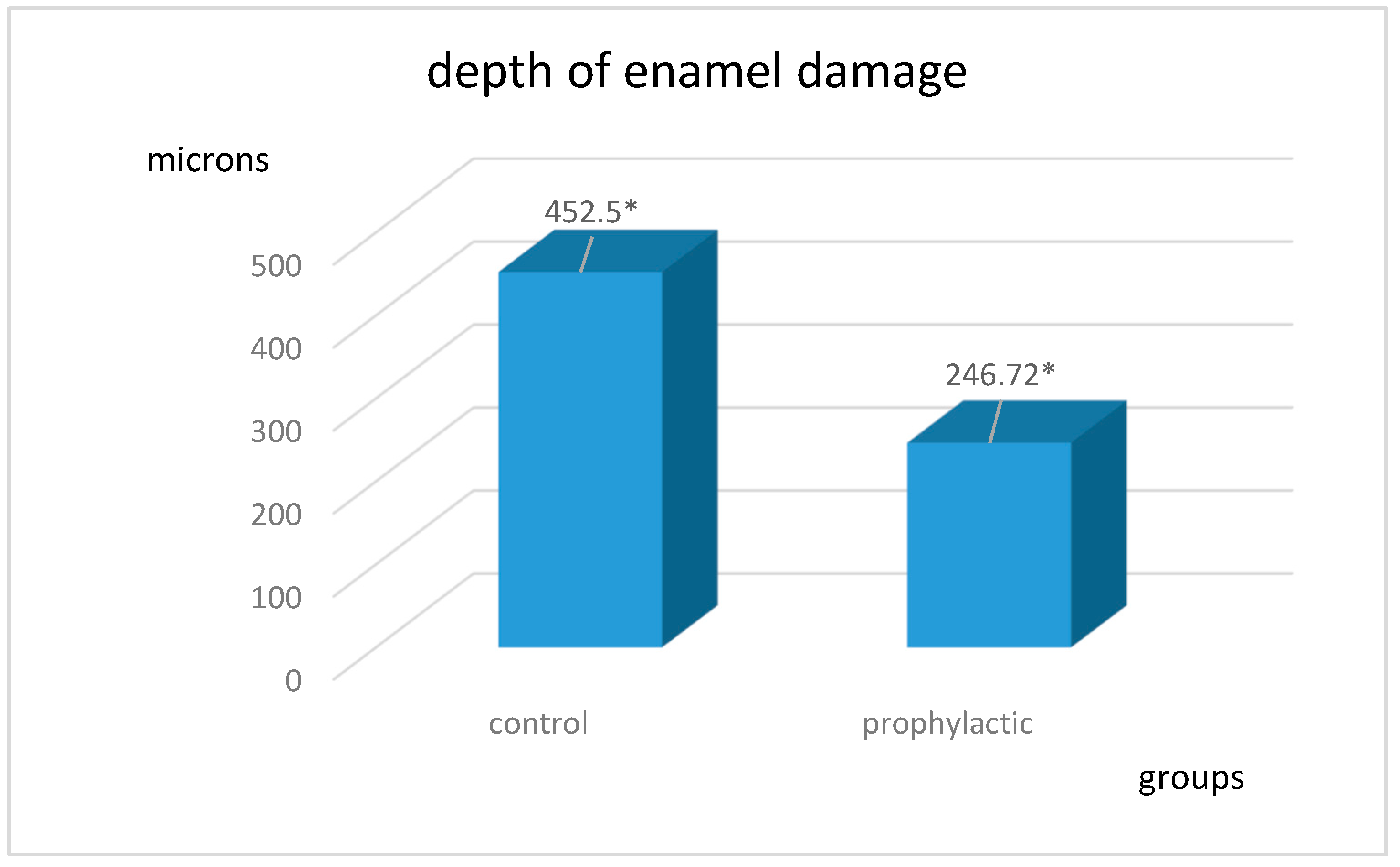
3.1. Results of Studies In Vitro
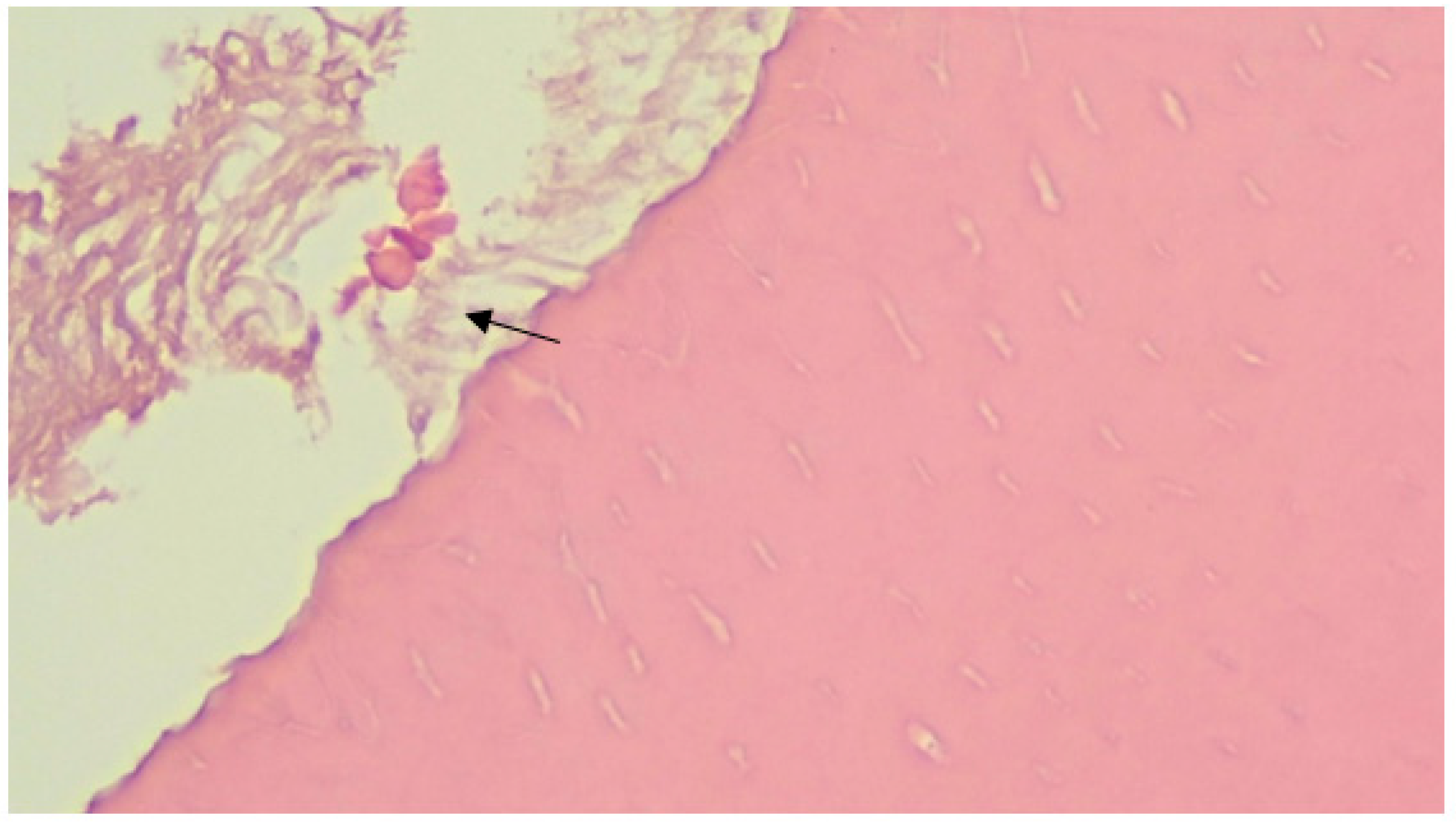
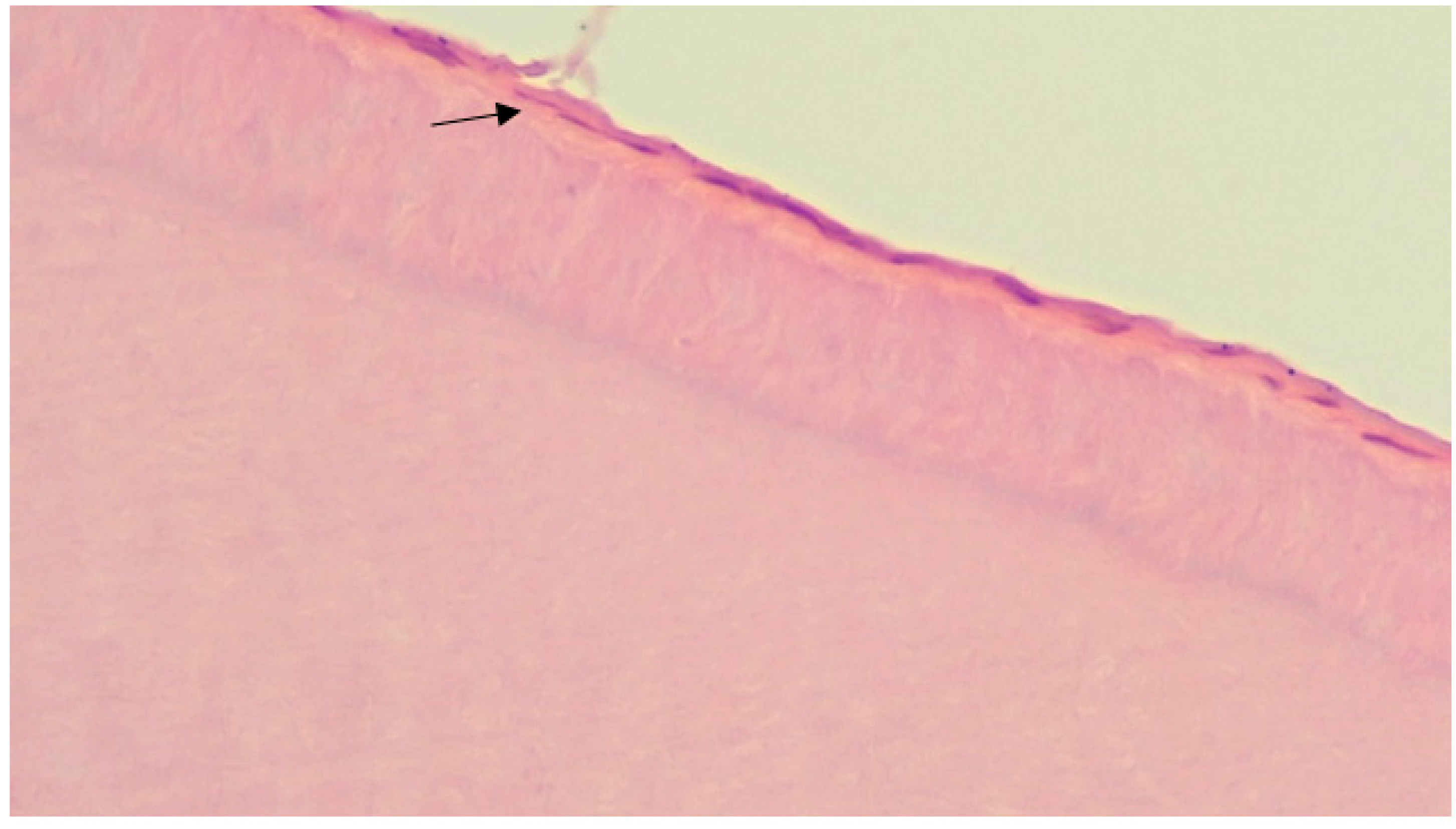
3.2. Results of Morphological Study
3.3. Clinical Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bonetti, A.G.; Zanarini, M.; Incerti Parenti, S.; Lattuca, M.; Marchionni, S.; Gatto, M.R. Evaluation of enamel surfaces after bracket debonding: An in-vivo study with scanning electron microscopy. Am. J. Orthod. Dentofac. Orthop. 2011, 140, 696–702. [Google Scholar] [CrossRef] [PubMed]
- Bora, N.; Mahanta, P.; Kalita, D.; Deka, S.; Konwar, R.; Phukan, C. Enamel Surface Damage following Debonding of Ceramic Brackets: A Hospital-Based Study. Sci. World J. 2021, 2021, 5561040. [Google Scholar] [CrossRef]
- Kozak, U.; Sękowska, A.; Chałas, R. The Effect of Regime Oral-Hygiene Intervention on the Incidence of New White Spot Lesions in Teenagers Treated with Fixed Orthodontic Appliances. Int. J. Environ. Res. Public Health 2020, 17, 9460. [Google Scholar] [CrossRef] [PubMed]
- Akay, E.N. Preventive Methods and Treatments of White Spot Lesions in Orthodontics. In Oral Health Care—An Important Issue of the Modern Society; Ardelean, L., Rusu, L.C., Eds.; Intech Open: London, UK, 2022. [Google Scholar] [CrossRef]
- Pont, H.B.; Özcan, M.; Bagis, B.; Ren, Y. Loss of surface enamel after bracket debonding: An in-vivo and ex-vivo evaluation. Am. J. Orthod. Dentofac. Orthop. 2010, 138, 387.E1–387.E9. [Google Scholar] [CrossRef]
- Sarafopoulou, S.; Zafeiriadis, A.A.; Tsolakis, A.I. Enamel Defects During Orthodontic Treatment. Balk. J. Dent. Med. 2018, 22, 64–73. [Google Scholar] [CrossRef]
- Gittner, R.; Müller-Hartwich, R.; Engel, S.; Jost-Brinkmann, P.G. Shear bond strength and enamel fracture behavior of ceramic brackets fascination® and fascination®2. J. Orofac. Orthop. 2012, 73, 49–57. [Google Scholar] [CrossRef]
- Khoroushi, M.; Kachuie, M. Prevention and Treatment of White Spot Lesions in Orthodontic Patients. Contemp. Clin. Dent. 2017, 8, 11–19. [Google Scholar] [CrossRef]
- Metin-Gürsoy, G.; Uzuner, F.D. The Relationship between Orthodontic Treatment and Dental Caries. In Dental Caries—Diagnosis, Prevention and Management; Intech Open: London, UK, 2018. [Google Scholar] [CrossRef]
- Zou, J.; Meng, M.; Law, C.S.; Rao, Y.; Zhou, X. Common dental diseases in children and malocclusion. Int. J. Oral Sci. 2018, 10, 7. [Google Scholar] [CrossRef]
- Heymann, G.C.; Grauer, D. A contemporary review of white spot lesions in orthodontics. J. Esthet. Restor. Dent. 2013, 25, 85–95. [Google Scholar] [CrossRef]
- Carvalho, F.B.; Barbosa, A.F.; Zanin, F.A.; Brugnera Júnior, A.; Silveira Júnior, L.; Pinheiro, A. Use of laser fluorescence in dental caries diagnosis: A fluorescence x biomolecular vibrational spectroscopic comparative study. Braz. Dent. J. 2013, 24, 59–63. [Google Scholar] [CrossRef]
- Kavvadia, K.; Seremidi, K.; Reppa, C.; Makou, M.; Lagouvardos, P. Validation of fluorescence devices for evaluation of white spot lesions in orthodontic patients. Eur. Arch. Paediatr. Dent. 2018, 19, 83–89. [Google Scholar] [CrossRef] [PubMed]
- Nascimento, P.L.; Fernandes, M.T.; Figueiredo, F.E.; Faria-E-Silva, A.L. Fluoride-Releasing Materials to Prevent White Spot Lesions around Orthodontic Brackets: A Systematic Review. Braz. Dent. J. 2016, 27, 101–107. [Google Scholar] [CrossRef] [PubMed]
- Mazur, M.; Jedliński, M.; Ndokaj, A.; Ardan, R.; Janiszewska-Olszowska, J.; Nardi, G.M.; Ottolenghi, L.; Guerra, F. Long-Term Effectiveness of Treating Dentin Hypersensitivity with Bifuorid 10 and Futurabond U: A Split-Mouth Randomized Double-Blind Clinical Trial. J. Clin. Med. 2021, 10, 2085. [Google Scholar] [CrossRef] [PubMed]
- Greenwall, L. White lesion eradication using resin infiltration. Int. Dent. Afr. Ed. 2013, 3, 54–62. [Google Scholar]
- Devji, T. Silver diamine fluoride is probably more effective than atraumatic restorative treatment, fluoride varnish, or no treatment for controlling caries progression in children. J. Am. Dent. Assoc. 2018, 149, e65. [Google Scholar] [CrossRef]
- Kooshki, F.; Pajoohan, S.; Kamareh, S. Effects of treatment with three types of varnish remineralizing agents on the microhardness of demineralized enamel surface. J. Clin. Exp. Dent. 2019, 11, e630–e635. [Google Scholar] [CrossRef]
- Meto, A.; Meto, A.; Tragaj, E.; Lipo, M.; Bauermann, C. The Use of Tiefenfluorid for Desensitization of Dentinal Hyperesthesia. Balk. J. Dent. Med. 2014, 18, 85–88. [Google Scholar] [CrossRef][Green Version]
- Kozaczuk, S. Deep Penetration Fluoridation for Caries Prevention and Treatment: The Use of Tiefenfluorid® Junior in Children. Case Reports; Nowa Stomatologia: Kraków, Poland, 2020; pp. 15–25. [Google Scholar] [CrossRef]
- Knappvost, A. Indications for Use and Mechanisms of Cares Prophylactic Action of Preparations of Deep Fluoridation—Enamel-Sealing and Dentin-Sealing Liquids; Dentistry for All: West New York, NJ, USA, 2001; pp. 38–42. [Google Scholar]
- Femiano, F.; Femiano, R.; Femiano, L.; Nucci, L.; Minervini, G.; Antonelli, A.; Bennardo, F.; Barone, S.; Scotti, N.; Sorice, V.; et al. A New Combined Protocol to Treat the Dentin Hypersensitivity Associated with Non-Carious Cervical Lesions: A Randomized Controlled Trial. Appl. Sci. 2021, 11, 187. [Google Scholar] [CrossRef]
- Zhu, H.; Zhang, S.; Ahn, C. Sample size considerations for split-mouth design. Stat. Methods Med. Res. 2017, 26, 2543–2551, Erratum in Stat. Methods Med. Res. 2019, 28, 3487. [Google Scholar] [CrossRef]
- Smaïl-Faugeron, V.; Fron-Chabouis, H.; Courson, F.; Durieux, P. Comparison of intervention effects in split-mouth and parallel-arm randomized controlled trials: A meta-epidemiological study. BMC Med. Res Methodol. 2014, 14, 64. [Google Scholar] [CrossRef]
- Pozos-Guillén, A.; Chavarría-Bolaños, D.; Garrocho-Rangel, A. Split-mouth design in Paediatric Dentistry clinical trials. Eur. J. Paediatr. Dent. 2017, 18, 61–65. [Google Scholar] [PubMed]
- Lee, J.J.; Nettey-Marbell, A.; Cook, A., Jr.; Pimenta, L.A.; Leonard, R.; Ritter, A.V. Using extracted teeth for research: The effect of storage medium and sterilization on dentin bond strengths. J. Am. Dent. Assoc. 2007, 138, 1599–1603. [Google Scholar] [CrossRef] [PubMed]
- Nawrocka, A.; Łukomska-Szymańska, M. Extracted human teeth and their utility in dental research. Recommendations on proper preservation: A literature review. Dent. Med. Probl. 2019, 56, 185–190. [Google Scholar] [CrossRef] [PubMed]
- Qeli, E.; Toti, Ç.; Odorici, A.; Blasi, E.; Tragaj, E.; Tepedino, M.; Masedu, F.; Kaçani, G.; Hysi, D.; Meto, A.; et al. Effectiveness of Two Different Fluoride-Based Agents in the Treatment of Dentin Hypersensitivity: A Prospective Clinical Trial. Materials 2022, 15, 1266. [Google Scholar] [CrossRef]
- Rogers, S.; Chadwick, B.; Treasure, E. Fluoride-containing orthodontic adhesives and decalcification in patients with fixed appliances: A systematic review. Am. J. Orthod. Dentofac. Orthop. 2010, 138, 390.E1–390.E8. [Google Scholar] [CrossRef]
- Salmerón-Valdés, E.; Lara-Carrillo, E.; Medina-Solís, C.; Robles-Bermeo, N.L.; Scougall-Vilchis, R.J.; Casanova-Rosado, J.F.; Pontigo-Loyola, A.P.; Fernández Barrera, M.Á. Tooth demineralization and associated factors in patients on fixed orthodontic treatment. Sci. Rep. 2016, 6, 36383. [Google Scholar] [CrossRef]
- Choi, Y.Y. Relationship between orthodontic treatment and dental caries: Results from a national survey. Int. Dent. J. 2020, 70, 38–44. [Google Scholar] [CrossRef]
- Srivastava, K.; Tikku, T.; Khanna, R.; Sachan, K. Risk factors and management of white spot lesions in orthodontics. J. Orthod. Sci. 2013, 2, 43–49. [Google Scholar] [CrossRef]
- Zarzycka-Kogut, K.; Pucek, M.; Jolanta, S. Orthodontic Treatment—Complications and Preventive Measures. Pol. J. Public Health 2014, 124, 103–106. [Google Scholar] [CrossRef]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Khachatryan, G.; Markaryan, M.; Vardanyan, I.; Manrikyan, M.; Manrikyan, G. Morphological Characteristics and Prevention of Tooth Enamel Demineralization during Orthodontic Treatment with Non-Removable Appliances. Int. J. Environ. Res. Public Health 2023, 20, 540. https://doi.org/10.3390/ijerph20010540
Khachatryan G, Markaryan M, Vardanyan I, Manrikyan M, Manrikyan G. Morphological Characteristics and Prevention of Tooth Enamel Demineralization during Orthodontic Treatment with Non-Removable Appliances. International Journal of Environmental Research and Public Health. 2023; 20(1):540. https://doi.org/10.3390/ijerph20010540
Chicago/Turabian StyleKhachatryan, Gagik, Marina Markaryan, Izabella Vardanyan, Mikayel Manrikyan, and Gayane Manrikyan. 2023. "Morphological Characteristics and Prevention of Tooth Enamel Demineralization during Orthodontic Treatment with Non-Removable Appliances" International Journal of Environmental Research and Public Health 20, no. 1: 540. https://doi.org/10.3390/ijerph20010540
APA StyleKhachatryan, G., Markaryan, M., Vardanyan, I., Manrikyan, M., & Manrikyan, G. (2023). Morphological Characteristics and Prevention of Tooth Enamel Demineralization during Orthodontic Treatment with Non-Removable Appliances. International Journal of Environmental Research and Public Health, 20(1), 540. https://doi.org/10.3390/ijerph20010540





