The World Health Organization (WHO) Integrated Care for Older People (ICOPE) Framework: A Narrative Review on Its Adoption Worldwide and Lessons Learnt
Abstract
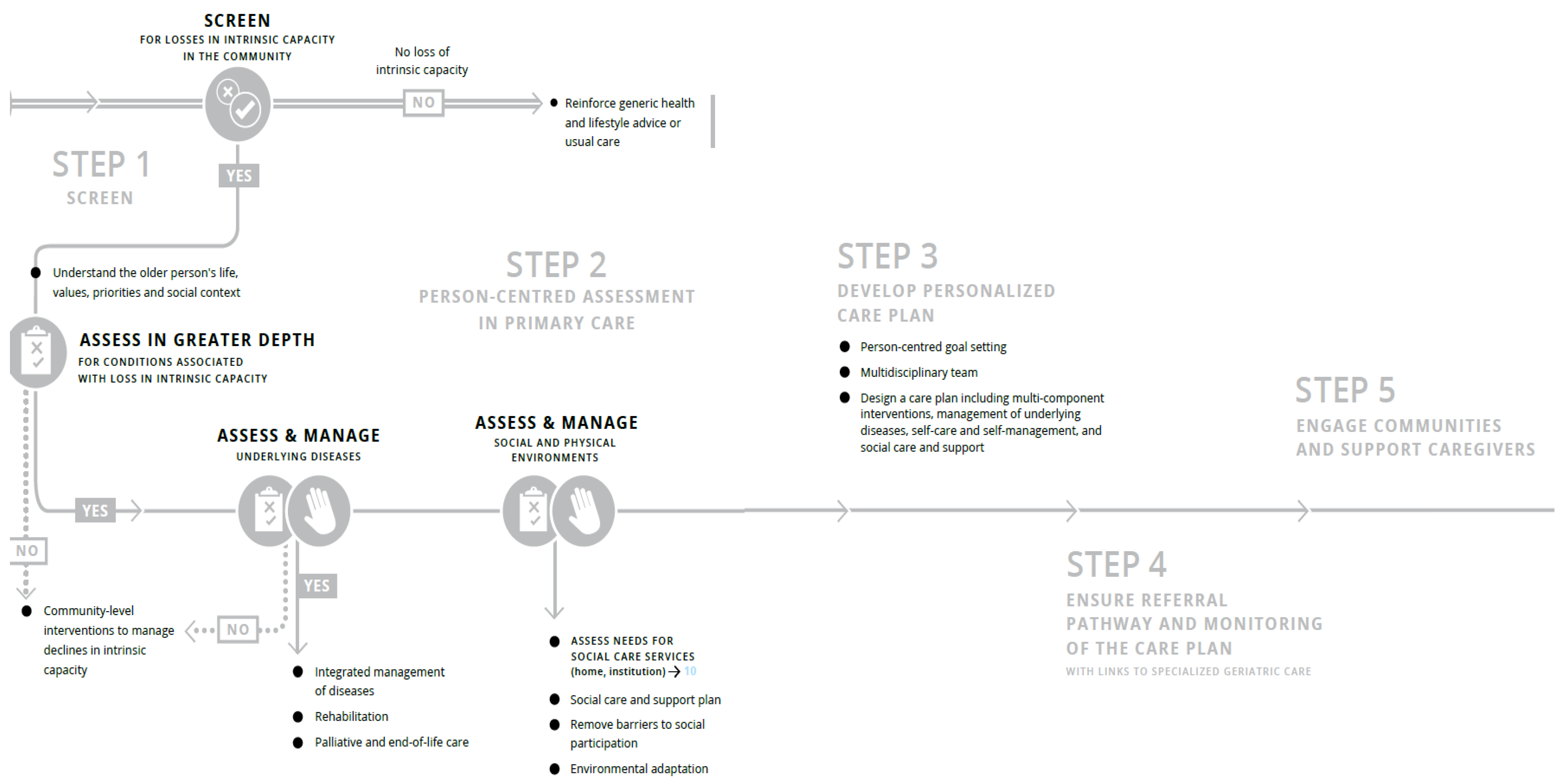
1. Introduction
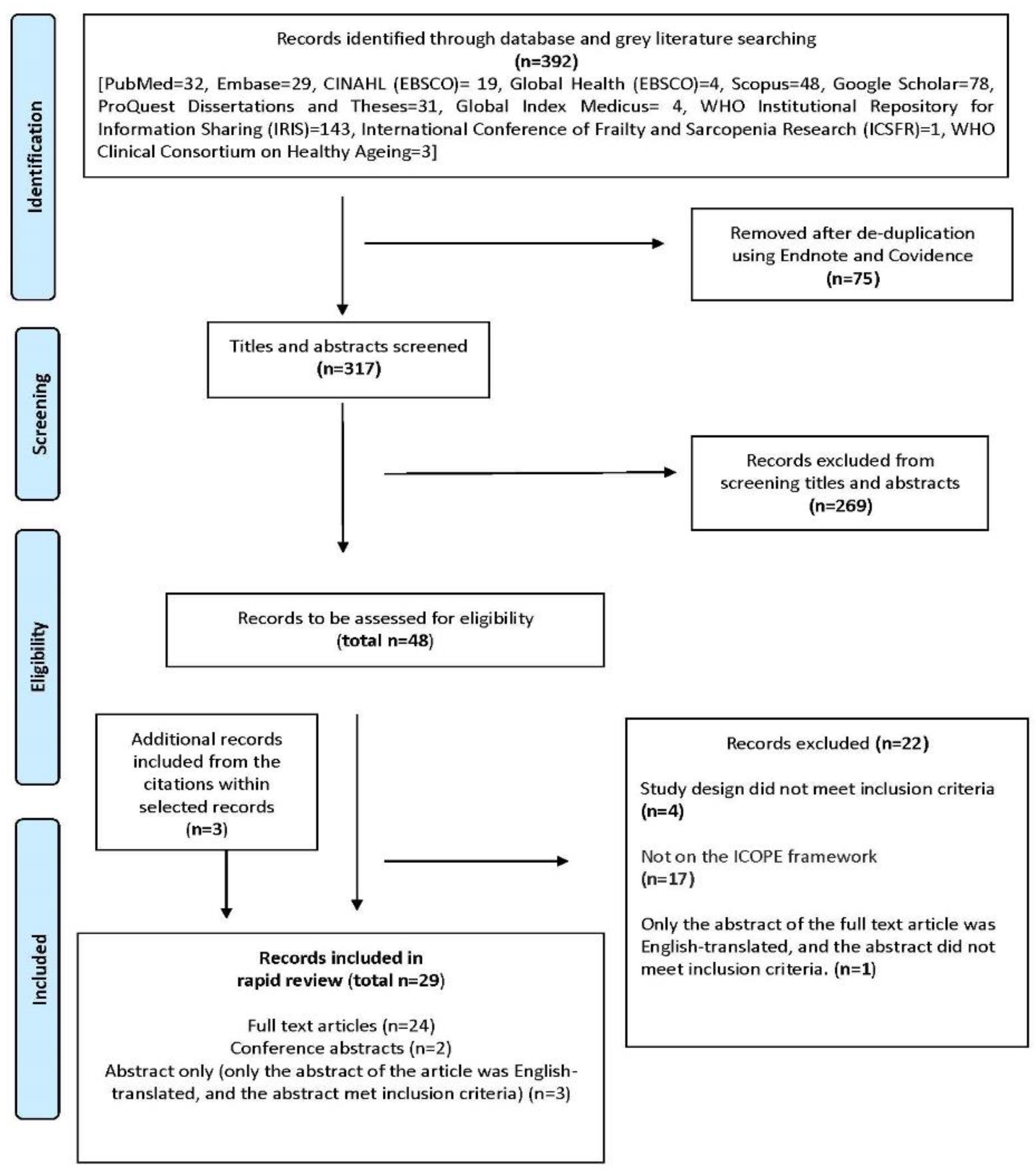
2. Methods
2.1. Systematic Search Strategy
2.2. Inclusion and Exclusion Criteria
2.3. Systematic Selection of Records
2.4. Data Extraction and Quality Evaluation
2.5. Data Synthesis
3. Results
3.1. Selection of Records
3.1.1. Identification and Development Phase (4 of 18 Study Teams)
3.1.2. Plans to Apply ICOPE Step 1 Only
3.1.3. Plans to Apply ICOPE Steps 1 to 5
3.1.4. Feasibility Phase (7 of 18 Study Teams)
3.1.5. Feasibility of Applying Only IC Domains Using Secondary Data Analysis
3.1.6. Feasibility of Implementing Step 1–3, with Modifications to the ICOPE Screening Tool
3.1.7. Feasibility of Implementing Step 1, without Modifications to the ICOPE Screening Tool
3.1.8. Implementation (7 of 18 Study Sites)
3.1.9. Implementation of Step 1 Only
3.1.10. Implementation of Steps 1–3 Only
3.1.11. Implementation of Steps 1–5
4. Discussion
4.1. Lessons Learnt and Implications for Practice and Policy
- 1
- Should the ICOPE programme target community-dwelling older adults in the general population or only older adults who attend primary care?
- 2
- Whether to adopt only Step 1 on IC screening or include other steps? What are the considerations for adopting ICOPE partially?
- 3
- Whether to modify the IC screening tool in Step 1?
- 4
- Whether to use digital tools
- 5
- At which phase of the intervention should ICOPE be adopted?
4.2. Implications for Future Research
4.3. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- The World Health Organisation (WHO). Decade of Healthy Ageing 2021–2030. Available online: https://www.euro.who.int/en/health-topics/Life-stages/healthy-ageing/news/news/2021/01/decade-of-healthy-ageing-2021-2030 (accessed on 30 September 2021).
- World Health Organisation. World Report on Ageing and Health; WHO: Geneva, Switzerland, 2015. [Google Scholar]
- Global Burden of Disease Study 2013 Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015, 386, 743–800. [Google Scholar] [CrossRef] [PubMed]
- Atun, R. Transitioning health systems for multimorbidity. Lancet 2015, 386, 721–722. [Google Scholar] [CrossRef] [PubMed]
- Briggs, A.M.; Valentijn, P.P.; Thiyagarajan, J.A.; Araujo de Carvalho, I. Elements of integrated care approaches for older people: A review of reviews. BMJ Open 2018, 8, e021194. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Framework on Integrated, People-Centred Health Services; World Health Organization: Geneva, Switzerland, 2016. [Google Scholar]
- de Carvalho, I.A.; Epping-Jordan, J.; Pot, A.M.; Kelley, E.; Toro, N.; Thiyagarajan, J.A.; Beard, J.R. Organizing integrated health-care services to meet older people’s needs. Bull. World Health Organ. 2017, 95, 756–763. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. WHO Global Strategy on Integrated People-Centred Health Services 2016–2026; WHO: Geneva, Switzerland, 2015. [Google Scholar]
- Integrated Care for Older People: Guidelines on Community-Level Interventions to Manage Declines in Intrinsic Capacity; Licence: CC BY-NC-SA 3.0 IGO; World Health Organization: Geneva, Switzerland, 2017.
- Global Consultation on Integrated Care for Older People (ICOPE)–The Path to Universal Health Coverage: Report of Consultation Meeting 23–25 October 2017 in Berlin, Germany; (WHO/FWC/ALC/18.3); Licence: CC BY-NC-SA 3.0 IGO; World Health Organization: Geneva, Switzerland, 2018.
- Integrated Care for Older People (ICOPE): Guidance for Person-Centred Assessment and Pathways in Primary Care; (WHO/FWC/ALC/19.1); Licence: CC BY-NC-SA 3.0 IGO; World Health Organization: Geneva, Switzerland, 2019.
- Integrated Care for Older People (ICOPE) Implementation Framework: Guidance for Systems and Services; Licence: CC BY-NC-SA 3.0 IGO; World Health Organization: Geneva, Switzerland, 2019.
- A Handbook on How to Implement mAgeing; Licence: CC BY-NC-SA 3.0 IGO; World Health Organization and International Telecommunication Union: Geneva, Switzerland, 2018.
- Integrated Care for Older People (ICOPE) Implementation Pilot Programme: Findings from the ‘Ready’ Phase; Licence: CC BY-NC-SA 3.0 IGO; World Health Organization: Geneva, Switzerland, 2022.
- Briggs, A.M.; Araujo de Carvalho, I. Actions required to implement integrated care for older people in the community using the World Health Organization’s ICOPE approach: A global Delphi consensus study. PLoS ONE 2018, 13, e0205533. [Google Scholar] [CrossRef] [PubMed]
- WHO Clinical Consortium on Healthy Ageing 2019: Report of Consortium Meeting Held 21–22 November 2019, Geneva, Switzerland; Licence: CC BY-NC-SA 3.0 IGO; World Health Organization: Geneva, Switzerland, 2020.
- WHO Clinical Consortium on Healthy Ageing 2020: Report of Consortium Meeting Held Virtually, 18–19 November 2020; Licence: CC BY-NC-SA 3.0 IGO; World Health Organization: Geneva, Switzerland, 2021.
- Covidence Systematic Review Software, Veritas Health Innovation, Melbourne, Australia. Available online: www.covidence.org (accessed on 1 June 2021).
- Garritty, C.; Gartlehner, G.; Nussbaumer-Streit, B.; King, V.J.; Hamel, C.; Kamel, C.; Affengruber, L.; Stevens, A. Cochrane Rapid Reviews Methods Group offers evidence-informed guidance to conduct rapid reviews. J. Clin. Epidemiol. 2021, 130, 13–22. [Google Scholar] [CrossRef]
- Sayers, A. Tips and tricks in performing a systematic review. Br. J. Gen. Pract. 2007, 57, 759. [Google Scholar] [CrossRef]
- Skivington, K.; Matthews, L.; Simpson, S.A.; Craig, P.; Baird, J.; Blazeby, J.M.; Boyd, K.A.; Craig, N.; French, D.P.; McIntosh, E.; et al. A new framework for developing and evaluating complex interventions: Update of Medical Research Council guidance. BMJ 2021, 374, n2061. [Google Scholar] [CrossRef]
- Sanchez-Rodriguez, D.; Piccard, S.; Dardenne, N.; Giet, D.; Annweiler, C.; Gillain, S. Implementation of the Integrated Care of Older People (ICOPE) App and ICOPE Monitor in Primary Care: A study protocol. J. Frailty Aging 2021, 10, 290–296. [Google Scholar] [CrossRef]
- Alekhina, A.V.; Silyutina, M.V.; Chernov, A.V.; Testova, S.G.; Romanova, M.M. Implementation of the WHO ICOPE Handbook App in the practice of primary care physicians. Vrach 2021, 32, 83–84. [Google Scholar] [CrossRef]
- Blancafort Alias, S.; Cuevas-Lara, C.; Martínez-Velilla, N.; Zambom-Ferraresi, F.; Soto, M.E.; Tavassoli, N.; Mathieu, C.; Heras Muxella, E.; Garibaldi, P.; Anglada, M.; et al. A Multi-Domain Group-Based Intervention to Promote Physical Activity, Healthy Nutrition, and Psychological Wellbeing in Older People with Losses in Intrinsic Capacity: AMICOPE Development Study. Int. J. Environ. Res. Public Health 2021, 18, 5979. [Google Scholar] [CrossRef] [PubMed]
- González-Bautista, E.; de Souto Barreto, P.; Virecoulon Giudici, K.; Andrieu, S.; Rolland, Y.; Vellas, B. Frequency of Conditions Associated with Declines in Intrinsic Capacity According to a Screening Tool in the Context of Integrated Care for Older People. J. Frailty Aging 2021, 10, 94–102. [Google Scholar] [CrossRef] [PubMed]
- González-Bautista, E.; de Souto Barreto, P.; Andrieu, S.; Rolland, Y.; Vellas, B. What day is today? Cognitive capacity and the risk of incident dementia in the context of integrated care for older people (ICOPE Step 1). Aging Clin. Exp. Res. 2021, 33, 3135–3139. [Google Scholar] [CrossRef] [PubMed]
- González-Bautista, E.; de Souto Barreto, P.; Andrieu, S.; Rolland, Y.; Vellas, B. Screening for intrinsic capacity impairments as markers of increased risk of frailty and disability in the context of integrated care for older people: Secondary analysis of MAPT. Maturitas 2021, 150, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Pagès, A.; Costa, N.; González-Bautista, E.; Mounié, M.; Juillard-Condat, B.; Molinier, L.; Cestac, P.; Rolland, Y.; Vellas, B.; Barreto, P.D.S. Screening for deficits on intrinsic capacity domains and associated healthcare costs. Arch. Gerontol. Geriatr. 2022, 100, 104654. [Google Scholar] [CrossRef] [PubMed]
- Gutiérrez-Robledo, L.M.; García-Chanes, R.E.; Pérez-Zepeda, M.U. Screening intrinsic capacity and its epidemiological characterization: A secondary analysis of the Mexican Health and Aging Study. Rev. Panam. Salud Pública 2021, 45, e121. [Google Scholar] [CrossRef]
- Prince, M.J.; Acosta, D.; Guerra, M.; Huang, Y.; Jacob, K.S.; Jimenez-Velazquez, I.Z.; Jotheeswaran, A.T.; Llibre Rodriguez, J.J.; Salas, A.; Sosa, A.L.; et al. Intrinsic capacity and its associations with incident dependence and mortality in 10/66 Dementia Research Group studies in Latin America, India, and China: A population-based cohort study. PLoS Med. 2021, 18, e1003097. [Google Scholar] [CrossRef]
- Won, C.W.; Ha, E.; Jeong, E.; Kim, M.; Park, J.; Baek, J.E.; Kim, S.; Kim, S.B.; Roh, J.; Choi, J.H.; et al. World Health Organization Integrated Care for Older People (ICOPE) and the Integrated Care of Older Patients with Frailty in Primary Care (ICOOP_Frail) Study in Korea. Ann. Geriatr. Med. Res. 2021, 25, 10–16. [Google Scholar] [CrossRef]
- Ma, L.; Chhetri, J.K.; Zhang, Y.; Liu, P.; Chen, Y.; Li, Y.; Chan, P. Integrated Care for Older People Screening Tool for Measuring Intrinsic Capacity: Preliminary Findings From ICOPE Pilot in China. Front. Med. 2020, 7, 576079. [Google Scholar] [CrossRef]
- Ma, L.; Zhang, Y.; Liu, P.; Li, S.; Li, Y.; Ji, T.; Zhang, L.; Chhetri, J.K. Plasma N-Terminal Pro-B-Type Natriuretic Peptide Is Associated with Intrinsic Capacity Decline in an Older Population. J. Nutr. Health Aging 2021, 25, 271–277. [Google Scholar] [CrossRef]
- Mathur, A.; Bhardwaj, P.; Joshi, N.K.; Jain, Y.K.; Singh, K. Intrinsic Capacity of Rural Elderly in Thar Desert using WHO ICOPE (Integrated Care for Older Persons) Screening Tool: A Pilot Study. medRxiv 2022. [Google Scholar] [CrossRef]
- Vaillant-Ciszewicz, A.; Cuni, A.; Girod, A. Abstracts of the 17th Congress of the European Geriatric Medicine Society. Eur. Geriatr. Med. 2021, 12, 1–387. [Google Scholar]
- Cheng, Y.C.; Kuo, Y.C.; Chang, P.C.; Li, Y.C.; Huang, W.T.; Chen, W.; Chou, C.Y. Geriatric Functional Impairment Using the Integrated Care for Older People (ICOPE) Approach in Community-Dwelling Elderly and Its Association with Dyslipidemia. Vasc. Health Risk Manag. 2021, 17, 389–394. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.; Kang, L.; Liu, X.; Zhao, S.; Wang, X.; Li, J.; Jiang, S. Trajectory and Correlation of Intrinsic Capacity and Frailty in a Beijing Elderly Community. Front. Med. 2021, 8, 751586. [Google Scholar] [CrossRef] [PubMed]
- Yu, R.; Leung, G.; Leung, J.; Cheng, C.; Kong, S.; Tam, L.Y.; Woo, J. Prevalence and Distribution of Intrinsic Capacity and Its Associations with Health Outcomes in Older People: The Jockey Club Community eHealth Care Project in Hong Kong. J. Frailty Aging 2022, 11, 302–308. [Google Scholar] [CrossRef] [PubMed]
- Smith, T. Paper Session. J. Am. Geriatr. Soc. 2018, 66, S443–S514. [Google Scholar]
- Guyonnet, S.; Rolland, Y.; Takeda, C.; Ousset, P.J.; Ader, I.; Davezac, N.; Dray, C.; Fazilleau, N.; Gourdy, P.; Liblau, R.; et al. The INSPIRE Bio-Resource Research Platform for Healthy Aging and Geroscience: Focus on the Human Translational Research Cohort (The INSPIRE-T Cohort). J. Frailty Aging 2021, 10, 110–120. [Google Scholar] [CrossRef]
- Piau, A.; Steinmeyer, Z.; Cesari, M.; Kornfeld, J.; Beattie, Z.; Kaye, J.; Vellas, B.; Nourhashemi, F. Intrinsic Capacitiy Monitoring by Digital Biomarkers in Integrated Care for Older People (ICOPE). J. Frailty Aging 2021, 10, 132–138. [Google Scholar] [CrossRef]
- Takeda, C.; Guyonnet, S.; Sumi, Y.; Vellas, B.; Araujo de Carvalho, I. Integrated Care for Older People and the Implementation in the INSPIRE Care Cohort. J. Prev. Alzheimer’s Dis. 2020, 7, 70–74. [Google Scholar] [CrossRef]
- de Souto Barreto, P.; Guyonnet, S.; Ader, I.; Andrieu, S.; Casteilla, L.; Davezac, N.; Dray, C.; Fazilleau, N.; Gourdy, P.; Liblau, R.; et al. The Inspire Research Initiative: A Program for Geroscience and Healthy Aging Research going from Animal Models to Humans and the Healthcare System. J. Frailty Aging 2021, 10, 86–93. [Google Scholar] [CrossRef]
- Lafont, C.; Tavassoli, N. Step 1 screening: Experimentation in Occitania with nurses and pharmacists. Soins Gerontol. 2021, 26, 12–15. [Google Scholar] [CrossRef] [PubMed]
- Mathieu, C.; McCambridge, C.; de Kerimel, J.; Jakovenko, D.; Lafont, C. Step 1 screening: Experimentation in Occitania with nurses and pharmacists. Soins Gerontol. 2021, 26, 16–19. [Google Scholar] [CrossRef] [PubMed]
- Tavassoli, N.; Piau, A.; Berbon, C.; De Kerimel, J.; Lafont, C.; De Souto Barreto, P.; Guyonnet, S.; Takeda, C.; Carrie, I.; Angioni, D.; et al. Framework Implementation of the INSPIRE ICOPE-CARE Program in Collaboration with the World Health Organization (WHO) in the Occitania Region. J. Frailty Aging 2021, 10, 103–109. [Google Scholar] [CrossRef]
- Zhao, J.; Chhetri, J.K.; Chang, Y.; Zheng, Z.; Ma, L.; Chan, P. Intrinsic Capacity vs. Multimorbidity: A Function-Centered Construct Predicts Disability Better Than a Disease-Based Approach in a Community-Dwelling Older Population Cohort. Front. Med. 2021, 8, 1656. [Google Scholar] [CrossRef]
- Cartier, Y.; Fichtenberg, C.; Gottlieb, L.M. Implementing Community Resource Referral Technology: Facilitators And Barriers Described By Early Adopters. Health Aff. 2020, 39, 662–669. [Google Scholar] [CrossRef] [PubMed]
- Ham, C.; Oldham, J. Integrating Health and Social Care in England: Lessons from Early Adopters and Implications for Policy. J. Integr. Care 2009, 17, 3–9. [Google Scholar] [CrossRef]
- Langarizadeh, M.; Moghbeli, F.; Aliabadi, A. Application of Ethics for Providing Telemedicine Services and Information Technology. Med. Arch. 2017, 71, 351–355. [Google Scholar]
- Nittari, G.; Khuman, R.; Baldoni, S.; Pallotta, G.; Battineni, G.; Sirignano, A.; Amenta, F.; Ricci, G. Telemedicine Practice: Review of the Current Ethical and Legal Challenges. Telemed. J. E Health 2020, 26, 1427–1437. [Google Scholar] [CrossRef]
- de la Torre-Díez, I.; López-Coronado, M.; Vaca, C.; Aguado, J.S.; de Castro, C. Cost-utility and cost-effectiveness studies of telemedicine, electronic, and mobile health systems in the literature: A systematic review. Telemed. J. E Health 2015, 21, 81–85. [Google Scholar] [CrossRef]
- Sukkriang, N.; Punsawad, C. Comparison of geriatric assessment tools for frailty among community elderly. Heliyon 2020, 6, e04797. [Google Scholar] [CrossRef]
- Thiam, C.N.; Ooi, C.Y.; Seah, Y.K.; Chuan, D.R.; Looi, I.; Ch’ng, A.S.H. Assessing Frailty in the General Medical Clinic of a Tertiary Hospital in Northern Malaysia: The FRAIL Scale or the Clinical Frailty Scale. Curr. Gerontol. Geriatr. Res. 2021, 2021, 7570592. [Google Scholar] [CrossRef] [PubMed]
- George, P.P.; Lun, P.; Ong, S.P.; Lim, W.S. A Rapid Review of the Measurement of Intrinsic Capacity in Older Adults. J. Nutr. Health Aging 2021, 25, 774–782. [Google Scholar] [CrossRef] [PubMed]
- Khangura, S.; Konnyu, K.; Cushman, R.; Grimshaw, J.; Moher, D. Evidence summaries: The evolution of a rapid review approach. Syst. Rev. 2012, 1, 10. [Google Scholar] [CrossRef] [PubMed]
| Inclusion | Exclusion | |
|---|---|---|
| Study design | ||
| 1. |
|
|
| 2. | Published from 31 October 2017 to 31 March 2022.The WHO introduced the WHO ICOPE framework by publishing a WHO report on the ICOPE guidelines for community interventions in October 2017. Hence, we searched for records published from 31 October 2017. The search was conducted in early April 2022, hence, we searched for published records up till 31 March 2022. | Published before 31 October 2017 or after 31 March 2022. |
| 3. | In English or with English translations.
| Not in English and had no English translations. |
| Population | ||
| 4. | Older adults | |
| Intervention | ||
| 5. | We aimed to find literature that answers the research questions:
| The record is not on the ICOPE framework. |
| Comparator | ||
| 6. | Records with and without controls can be included | |
| Outcome | ||
| 7. | There were no inclusion criteria on outcomes. This was supported by:
| |
| Phase of Intervention | Citation | Study Participants | Who Does IC Screening | Brief Description of Application of the ICOPE Framework | |
|---|---|---|---|---|---|
| Development phase (4 study teams) | Study teams that plan to adopt ICOPE Step 1 only (Methodology and protocol articles) (3 study teams) | Study team 1 | |||
| Methodology of a 1 year prospective cohort study in Leige, Belgium Setting: Community Mobile health technology: ICOPE app, ICOPE MONITOR app | |||||
| Sanchez-Rodriguez 2021 [22] | Community-dwelling adults aged 65 years and above who are living at home and able to use apps. | Self-assessment using two apps, the ICOPE app and ICOPE MONITOR. | The ICOPE app will assess five IC domains. Two results are possible: positive (probable decrease in intrinsic capacity) or negative (intrinsic capacity not decreased), as a total binary result of the five domains together. The app includes the possibility to record the summary of the screening, download it in PDF, or send it by mail. The ICOPE MONITOR app will be used for identification, obtaining informed consent of both healthcare workers and the participants, and monitoring five IC domains. The results obtained in the five domains will be provided as a checklist: two results are possible for each one of the five domains: Yes or No in each domain. Recommendations for each domain are provided. The app automatically schedules the date for the next IC screening every 4 months and sends the informed consent by mail to participants. | ||
| Study team 2 | |||||
| Development of a study in Voronezh, Russia Setting: Primary care Mobile health technology: ICOPE app | |||||
| Alekhina et al., 2021 [23] | Patients aged 65 years and above. | Primary care physicians. | Physicians screen for functional ability using a mobile app. | ||
| Study team 3 | |||||
| Plans to conduct secondary analysis of the CRELES (2005–2009) dataset Nationally representative sample in Costa Rica, Mexico | |||||
| WHO Report 2020 [11]; Mexico | CRELES dataset consists of a nationally representative sample. | Not specified. | Among the variables used in the study was the IC index, which is a summary index built from the five ICOPE domains using a scale of 0 (severe deterioration) to 10 (optimal). | ||
| Study team that plans to adopt ICOPE Steps 1–5 | Study team 1 | ||||
| Conceptualisation of the AMICOPE Study in Spain and France (11 territories in Occitanie, Andorra, Navarra, Catalonia) Setting: Community | |||||
| Blancafort Alias et al., 2021 [24] | Older people with losses in mobility, nutritional and/or psychological domains of intrinsic capacity; without cognitive decline, visual impairment, or hearing loss; living in the community; and recruited or referred from primary care and community settings. | Healthcare workers | Conceptual framework involved multimodal exercises, advice on cognitive stimulation, dietary advice, advice on managing depressive symptoms like reducing stress, tackling loneliness, strengthening social support, and accessing community facilities, medication review, supporting self-management, goal setting, and maintaining autonomy and preventing dependence on care. Older persons will be recruited from community facilities, such as senior leisure centres, civic centres, or primary care centres. Health and social care professionals would be from different backgrounds, including nurses, physiotherapists, occupational therapists, nutritionists, psychologists, and physical activity trainers. | ||
| Feasibility phase (7 study teams) | Feasibility of only applying ICOPE IC domains using secondary data analysis (3 study teams) | Study team 1 | |||
| Secondary analysis of the MAPT dataset Setting: Community (memory clinics in the community in France) (MAPT is a 3-year, multi-centre, randomised, placebo-controlled superiority trial) | |||||
| González-Bautista et al., 2021 [25] (J Frailty Aging, Frequency of conditions) | Community-dwelling older adults aged 70 years or older without dementia at baseline. | Secondary data analysis of the MAPT dataset. | Step 1 is called MAPT Step 1. The IC domains included cognitive decline, limited mobility, malnutrition, visual impairment, hearing loss, and depressive symptoms, and they refer to the conditions associated with declines in IC. Adapted operationalisation of: Visual impairment: Self-reported visual acuity items. Hearing loss: Item number 3 of the screening version of the hearing handicap inventory for the elderly (HHSE) Depressive symptoms: Defined according to items 2 and 7 of the Geriatric Depression Scale (GDS-15), which were judged by three experts (one geriatrician, one general practitioner, and one researcher in clinical gerontology) as being the most similar items compared to those recommended by WHO. After being screened with the adapted MAPT Step 1 tool, approximately 9 of 10 older adults had one or more conditions associated with declines in IC. | ||
| Gonzalez-Bautista et al., 2021 [26] (Ageing Clinical Experimental Research Journal) | Only the cognitive ICOPE IC domain was applied. People with impaired cognitive capacity according to the ICOPE Step 1 tool had higher dementia risk. | ||||
| Gonzalez-Bautista et al., 2021 [27] (Maturitas Journal) | Step 1 is called MAPT Step 1. The study appliedthe modified ICOPE Step 1 for 3 domains, including cognition (time and space orientation plus word recall), locomotion (perform five chair rises within 14 s), and vitality/nutrition (self-reported weight loss or appetite loss). Adapted operationalisation of: Vision: answering “yes” to any of: “Even if wearing glasses, do you have visual problems to (a) distinguish the faces of people in the same room? (b) move indoors/outdoors? (c) other activities (reading a paper, watching television)?” Hearing: answering “sometimes” or “yes” to the question “Do you have difficulty hearing when someone speaks in a whisper?” (HHSE-S); Psychological function: answering “yes” to the item 2 of Geriatric Depression Scale (GDS-15) “Have you dropped many of your activities and interests?”, or responding “no” to the item 7 of the GDS-15 “Do you feel happy most of the time?” Three experts (one geriatrician, one general practitioner, and one researcher in clinical gerontology) judged these GDS items as the closest ones to the ICOPE screening. Calculated total score by adding the number of intrinsic capacity impairments found by the MAPT Step 1 (score range 0–6, higher is worst). Decline in each additional IC domain was associated with a higher risk of incident frailty, IADL, and ADL disability. | ||||
| Pages et al., 2022 [28] | ICOPE Steps: Step 1 (modified, referred to as MAPT Step 1) Applied an adapted version of the ICOPE Step 1 to screen for 6 IC domains. | ||||
| Study team 2 | |||||
| Secondary analysis of the Mexico Health and Ageing Study (MHAS) Wave 2015 dataset; Nationally representative population | |||||
| Gutierrez-Robledo et al., 2021 [29] | Older adults aged 50 years and older in the Mexican population. | Secondary data analysis of an existing dataset. | The IC domains included cognition, psychological, senses (vision and hearing), vitality, and mobility. The exact ICOPE screening questions may not be used. The questions will be from the MHAS survey. Decreased levels of IC in the Mexican older people were associated with lower levels of education, poorer self-rated health, more chronic diseases, more visits to a physician, and increased dependencies in ADLs. | ||
| Study team 3 | |||||
| Secondary analysis of the Dementia Research Group (DRG) cohort study (2003-07, 2008-10) dataset on 8 LMICs across Latin America, China, and India Setting: Community | |||||
| Prince et al., 2021 [30] | Older people aged 65 years and over living in geographically defined catchment areas in eight countries. | Interviewer who visited participants’ homes. | The IC domains were evaluated at baseline, including neuromusculoskeletal capacity, vitality, nutrition, sensory capacity (visual impairment), cognitive capacity, psychological capacity, and continence. Declines in IC was associated with dependence for care and mortality. | ||
| Feasibility of implementing Step 1, with modifications to the ICOPE IC screening tool (1 study team) | Study team 1 | ||||
| 6-month feasibility study of ICOOP_FRAIL in South Korea (A RCT across 4 primary care clinics) Setting: Primary care Mobile health technology: IC screening (KPI_PC) on mobile devices | |||||
| Won et al., 2021 [31] | Not specified. | Nurses and doctors. | Nurses and doctors applied the Korean Frailty Index for Primary Care (KFI_PC) on mobile devices to evaluate the functional decline and frailty of older adult patients. The KFI_PC consists of 53 items in eight IC domains, including cognition, mobility, malnutrition, visual impairment, hearing loss, depressive symptoms, and geriatric syndromes including urinary incontinence and risk of falls. All items in the KFI_PC were on a mobile notepad used by nurses and doctors to evaluate the frailty index score and assessed risk factors for frailty. Primary care physicians talked to patients about functional declines and its risk factors, nutrition, exercise, medication, and disease management. Within 1 month, a health coach contacted the patient via telephone to monitor them and encouraged consuming a protein-rich balanced diet or/and exercise. The patient was linked to social welfare services managed by community administration centres or senior welfare centres for social support. However, none were available due to COVID-19. Health coaches involved in ICOOP_Frail were paramedical students. The phone call for health coaching was repeated monthly for a total of 6 months. The KFI_PC was re-evaluated at 3 and 6 months | ||
| Feasibility of implementing Step 1, without modifications to the ICOPE IC screening tool (3 study teams) | Study team 1 | ||||
| Cross-sectional study by a team in Beijing, China Setting: Hospital setting (Department of Geriatrics of a University Hospital) | |||||
| Ma et al., 2020 [32] | Healthy participants without acute illness and aged ≥50 years. | Not specified. | The authors examined the clinical utility of Step 1 on healthy older adults without acute illnesses in the department of geriatrics of a University Hospital. The ICOPE screening tool appeared useful to identify adults with poor physical and mental function in a Chinese sample. | ||
| Ma et al., 2021 [33] | |||||
| Study team 2 | |||||
| Cross-sectional feasibility study in the villages of Jodphur, Rajasthan, India Setting: Community | |||||
| Mathur et al., 2021 [34] (preprint) | Geriatric persons aged 60 years and above. | Community-based healthcare workers and trained interviewers, including trained public health students | The IC domains included cognition, mobility, visual and hearing, and depressive symptoms. The ICOPE screening tool provided the proportions of older persons with declines in each of the IC domains. | ||
| WHO Clinical Consortium on Healthy Ageing 2019 [16] | It will involve ICOPE screening, assessment and interventions. Follow-up period is planned to be 15 months. | ||||
| WHO Clinical Consortium on Healthy Ageing 2020 [17] | Step 1 will be by community-based health workers. Step 2 will be by mid-level health providers and doctors. Step 3 will be by the multidisciplinary team. Step 4 (Referrals) will be by hospital care navigators to the appropriate assessments and interventions, and Step 5 is on caregivers. Community health workers, case managers and navigators (trained to assist patients in seeking the right level of care in hospital settings) will help align health and social services and facilitate referral of rural older adults. | ||||
| ICOPE implementation pilot programme: findings from the ‘ready’ phase. Geneva, 2022 [14] | Step 1 was conducted at the homes and the community in Rajasthan by 15 public health students. Assessments were planned. Due to COVID-19, no further activity was possible following IC screening. The most significant declines were in hearing and mobility, with more than half of the older persons having declines in these domains. There were higher levels of decline in the mobility domain among female than male participants. | ||||
| Study team 3 | |||||
| 6-month feasibility study by a study team in Nice, France Setting: Hospital (University Hospital Centre of Nice) Mobile health technology: ICOPE MONITOR app | |||||
| Valliant-Ciszewicz et al., 2021 [35] (Conference proceeding) | Dementia patients and their caregivers (patient-carer dyads). | A nurse | Nurses carried out Step 1 at the first month and fourth month of care. Nurses carried out screening for frailty and prevention activities based on the ICOPE MONITOR app. For Step 2, the nurse referred older adults to hospital prescribers and/or attending physicians, if declines in IC were identified. Interventions by geronto-psychologists were given at home, including non-drug approaches for the patient and psychoeducation programme for the carer. | ||
| Implementation phase (7 study teams/sites) | Implementation of Step 1 only (3 study teams/sites) | Study team/study site 1 | |||
| Cross-sectional study by a study team in Chia-Yi, Taiwan Setting: Community | |||||
| Cheng et al., 2021 [36] | Community-dwelling persons aged at least 65 years with hypertension, diabetes or dyslipidemia; or persons aged at least 75 years. | Not specified | The team aimed to examine associations between IC with chronic conditions IC domains included cognitive decline, limited mobility, malnutrition, visual impairment, hearing loss, and depressive symptoms. Dyslipidemia was associated with greater declines in IC. | ||
| Study team/study site 2 | |||||
| 2-year cohort study in Taikang Yanyuan, Beiing, China Setting: Community (Taikang Yanyuan continuing care retirement community) | |||||
| Liu et al., 2021 [37] | Older adults aged 75 years and more who lived in the compound senior community. They were independent, as evaluated by community doctors. | Trained geriatricians from Peking Union Medical College Hospital (PUMCH). | The IC domains included cognition, locomotion, vitality, sensory capacity (vision and hearing) and psychosocial needs. Step 1 screening was adapted by using the Comprehensive Geriatric Assessment (CGA) Electronic Data Capture System. IC decline was more strongly associated with adverse outcomes than with frailty. | ||
| Study team/study site 3 | |||||
| Longitudinal observational study of 18 districts in Hong Kong Setting: Community (80 community elderly centres across 18 districts in Hong Kong.) | |||||
| Yu et al., 2022 [38] | Community-dwelling older adults | Older adults completed IC surveys with guidance from trained staff members of the elderly centres. | Six IC domains included cognition, locomotion, vitality, sensory capacity (vision), sensory capacity (hearing), psychological capacity. The team aimed to examine the prevalence and distribution of IC in older adults at 80 community-based elder centres across 18 districts in Hong Kong. IC decline was associated with increased risks of polypharmacy, incontinence, poorer self-rated health, and IADL dependencies. | ||
| Implementation of Steps 1–3 (2 study teams/sites) | Study team/study site 1 | ||||
| Longitudinal observational study in Ohio, United States Setting: Primary care (45 primary care group practices) | |||||
| Smith 2018 [39] | Older adults with nutritional conditions or at risk of nutritional conditions. | Primary care practitioners | Step 1 involved identification of nutritional conditions. During routine office visits, primary care practitioners used nutrition care pathways to identify the potential of being under- or overnourished. Practitioners recommended oral nutrition supplements appropriate for the patient’s condition and provided basic nutrition education through a variety of resources. Follow-up care was given during subsequent patient office visits. | ||
| Study team/study site 2 | |||||
| Observation study from July–Sept 2020 at Canillo, Andorra Setting: Community (Small urban site in a small town in a mountainous area) | |||||
| ICOPE implementation pilot programme: findings from the ‘ready’ phase. Geneva [14] | Older adults aged 65 years and above. | The study team comprised two geriatricians and a geriatric nurse. They engaged primary care doctors to ensure follow-up care. | The study teams reported that the screening sessions took between 5 and 20 mins per person. The setting for the screening was a social club for older people run by the city council in Canillo (two geriatricians and one geriatrics nurse). A rolling recruitment process was used that followed a public health media campaign. The participants were screened and assessed as they were identified. The team was small and already had awareness of ICOPE, so it needed minimal training. The team assessed declines in IC at the community health facility. The team met with all participants to discuss the results of their screening and assessment. Any person with declines in mobility or cognition received an appointment with the lead geriatrician to develop a personalized care plan, which was then shared with the participant’s primary care doctor. More than half of the older persons had declines in cognition and more than one in three had depressive symptoms. | ||
| Implementation of Steps 1–5 (2 study teams/sites) | Study team/study site 1 | ||||
| ICOPE-Care Programme in Toulouse City, Occitanie, France from October 2019 to September 2028. Setting: Community (primarily) and primary care Mobile health technology: ICOPE app, ICOPE MONITOR app, ICOPE BOT (conversational chat bot), FRAILTY-ICOPE database, telemedicine platform | |||||
| Guyonnet 2020 [40] (Methodology article) | Older persons aged more than 60 years (a group for those aged 40–60 years could be included) | Patients (with or without caregiver’s help), research or clinical nurse | Between two annual visits, IC domains will be monitored every 4 months by using the ICOPE MONITOR app. Six IC domains are monitored (with or without the help of a caregiver) in either the application developed in collaboration with WHO (ICOPE Monitor app) or a web platform, or through a phone call by a Gerontopole’s trained research nurse. When declines are detected in the ICOPE Step 1, a phone call is organized by the research nurse within one week to confirm this decline and to investigate the causes in collaboration with the medical research team. Participants will be trained to monitor their IC during the baseline visit by the Gerontopole’ research team. The remote monitoring of IC will last the whole length of the research study for up to ten years. Once an IC decline is confirmed, participants will have a thorough clinical assessment and blood sampling. The information will allow the examination of some markers of aging at the time declines are detected. There will be a personalized prevention care plan to maintain function according to the recommendations from the WHO ICOPE programme for usual care. | ||
| Piau et al., 2020 [41] (Narrative description of INSPIRE) | Self-assessment. | There is self-screening every 4 months. There could be app-guided and chat box-guided questions. A team of nurses will receive the results remotely on a dashboard. When a decline is detected between two self-assessments, the patient will be offered a face-to-face evaluation. There could also be clinical confirmation tests. | |||
| Takeda et al., 2020 [42] (Methodology article) | Self-assessment. | Self- assessment is every 4 months and monitored by the Toulouse regional team for ageing and prevention. Once IC decline is identified, the older adults will go through clinical assessment and blood sampling. | |||
| WHO Clinical Consortium on Healthy Ageing 2019 [16] | Self-assessment. | The programme will involve biological sampling and self-monitoring using the ICOPE screening tool after training with a health care worker. The follow-up period will be 4 months for self-monitoring, and annual and biannual visits by health care workers. | |||
| De Souto Barreto 2021 [43] (Methodology article) | Primary care providers (in particular, community nurses). | Primary care providers, in particular community nurses, will use the ICOPE app for tablets/smartphones to implement the ICOPE pathway for each older adult. ICOPE Step 1 (i.e., screening for low IC levels) will be performed in all individuals. The other steps of the model may be performed according to available resources in the local care services/facilities. A modified version of Step 1 (with discrete/continuous IC variables) in the ICOPE app will be used for the remote monitoring of IC levels over time. All the data will be automatically transferred to a secure database and will be used to investigate the evolution of IC domains over time. | |||
| Lafont et al., 2021 [44] (Abstract only (only the abstract was English translated)) | Nurses and pharmacists. | Digital tools were developed. | |||
| Mathieu et al., 2021 [45] (Abstract only (only the abstract was English translated)) | Nurses and pharmacists. | Nurses and pharmacists were invited to integrate Step 1 in their practices. They attended a free webinar training if they wanted to. | |||
| Tavassoli et al., 2021 [46] (Methodology article) | Self-assessment, assistance from caregivers, healthcare professionals. | Step 1 will use the mobile app for remote monitoring on a large-scale. Seniors would be invited to use the Step 1 every 4–6 months. If the senior could not carry out the self-assessment, a professional would intervene every 6 months to perform Step 1. Steps 2 and 3 will involve assessment by the nurse and/or general practitioner if Step 1 was abnormal, or if an alert was generated during follow-up. If the screening of IC was abnormal, Steps 2 and 3 were carried out by the GP or nurse trained in geriatrics. Step 4 will involve Digital medicine used in this programme to simultaneously monitor large populations regardless of where they lived and ensure the implementation and follow up of the personalised care plan that was proposed in Step 3. Step 5 will be engagement of the community. This step is part of the INSPIRE ICOPE-CARE programme and plays an important role in bringing together different actors and organisations. | |||
| WHO Clinical Consortium on Healthy Ageing 2020 [17] | Self-assessment by older adults and healthcare professionals (community nurses, general practitioners) | All domains of IC were systematically monitored through ICOPE tools, which has been adapted in digital form to make remote and large-scale monitoring possible. Two tools were developed, the ICOPE MONITOR and the ICOPE BOT, a conversational robot. Both are connected to the Gérontopôle frailty database. Step 1 was done every 4–6 months by healthcare professionals or older people themselves. If deterioration in one or more domains of IC is identified, an algorithm alerts health care professionals so they can quickly intervene. If abnormalities were determined in Step 1, nurses used a telemedicine platform to refer the older person to a primary care provider. There was teleconsultation by professionals with expertise in geriatric care. Measures included screening and full assessments, comprehensive battery of geriatric clinical assessments, body composition, maximal tests (VO² max, isokinetic strength) and biospecimens (fluids and cells/tissues). | |||
| ICOPE implementation pilot programme: findings from the ‘ready’ phase. Geneva, 2022 [14] | 1711 health and care workers (1053 nurses, 245 pharmacists, 104 doctors) and 20 post office workers) are trained for Step 1. | Older people having the opportunity to be involved in their own carewas a key message of the campaign in Occitanie to encourage participants to self-screen. This engagement and recruitment were achieved through a multimedia campaign using flyers, posters, a film promoting the ICOPE Monitor mobile app, webinars, conferences, and interviews. The assessments were organized and conducted by primary care workers (physicians, nurses, physiotherapist) with participants who had a positive screening result in IC at a health facility or the participant’s home, and used digital tools. Development of care plans and any necessary follow up were referred to the primary care workers. There was also community engagement. Ninety-four percent of participants had potential declines in at least one domain and there were also high numbers of participants that experienced declines in multiple domains. Approximately two-thirds of the older persons had loss of mobility and over 40% had issues with malnutrition. | |||
| Study team/study site 2 | |||||
| A healthy ageing programme in Chaoyang, Beijing, China (slogan: ICOPE will bring older people happiness) Setting: Community (Urban, suburban, and rural areas of the Chaoyang district) | |||||
| WHO Clinical Consortium on Healthy Ageing 2019 [16] | Community-dwelling persons aged 80 years and older with a risk of decline in IC, determined by ICOPE screening. | Not specified. | It involved ICOPE screening with examination of biomarkers. The next steps included validation of the screening tool including the app, a pilot study onintegrated interventions for specific IC abnormalities with different outcome measures, and the development of a project evaluation. | ||
| WHO Clinical Consortium on Healthy Ageing 2020 [17] | Integrated care managers (may include community health workers. They are being trained to understand the care plan and deliver the ICOPE guidance. | The intervention will involve a personalized care plan with health and social care services coordinated by integrated care managers. The follow up period is 6–12 months. A longer study will be considered if findings demonstrate efficacy. Lower age groups may be enrolled. | |||
| Zhao et al., 2021 [47] | Trained clinicians | IC domains included locomotion, vitality, sensory (vison and hearing impairments), cognition, and psychology. At the 1-year follow up, there was a stronger association between IC declines and dependency in ADL than the association between multimorbidity and ADL dependency. | |||
| ICOPE implementation pilot programme: findings from the ‘ready’ phase. Geneva. 2022 [14] | Healthcare workers. | Step 1 was at the homes of older people and health centres in Chaoyang. Step 2 was carried out by integrated care managers with all participants. After developing personalized care plans with older people, integrated care managers (trained health and care workers) provided follow up sessions mainly through video calls. These aimed to support rehabilitative exercises, medication adherence and assistive care, and to check for any new or additional needs for social and health services. About 14% of respondents showed potential cognitive decline at screening compared with 37% at the formal assessment. A lower proportion of older adults had depressive symptoms. | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sum, G.; Lau, L.K.; Jabbar, K.A.; Lun, P.; George, P.P.; Munro, Y.L.; Ding, Y.Y. The World Health Organization (WHO) Integrated Care for Older People (ICOPE) Framework: A Narrative Review on Its Adoption Worldwide and Lessons Learnt. Int. J. Environ. Res. Public Health 2023, 20, 154. https://doi.org/10.3390/ijerph20010154
Sum G, Lau LK, Jabbar KA, Lun P, George PP, Munro YL, Ding YY. The World Health Organization (WHO) Integrated Care for Older People (ICOPE) Framework: A Narrative Review on Its Adoption Worldwide and Lessons Learnt. International Journal of Environmental Research and Public Health. 2023; 20(1):154. https://doi.org/10.3390/ijerph20010154
Chicago/Turabian StyleSum, Grace, Lay Khoon Lau, Khalid Abdul Jabbar, Penny Lun, Pradeep Paul George, Yasmin Lynda Munro, and Yew Yoong Ding. 2023. "The World Health Organization (WHO) Integrated Care for Older People (ICOPE) Framework: A Narrative Review on Its Adoption Worldwide and Lessons Learnt" International Journal of Environmental Research and Public Health 20, no. 1: 154. https://doi.org/10.3390/ijerph20010154
APA StyleSum, G., Lau, L. K., Jabbar, K. A., Lun, P., George, P. P., Munro, Y. L., & Ding, Y. Y. (2023). The World Health Organization (WHO) Integrated Care for Older People (ICOPE) Framework: A Narrative Review on Its Adoption Worldwide and Lessons Learnt. International Journal of Environmental Research and Public Health, 20(1), 154. https://doi.org/10.3390/ijerph20010154






