The Effect of Human Settlement Pedestrian Environment on Gait of Older People: An Umbrella Review
Abstract
1. Introduction
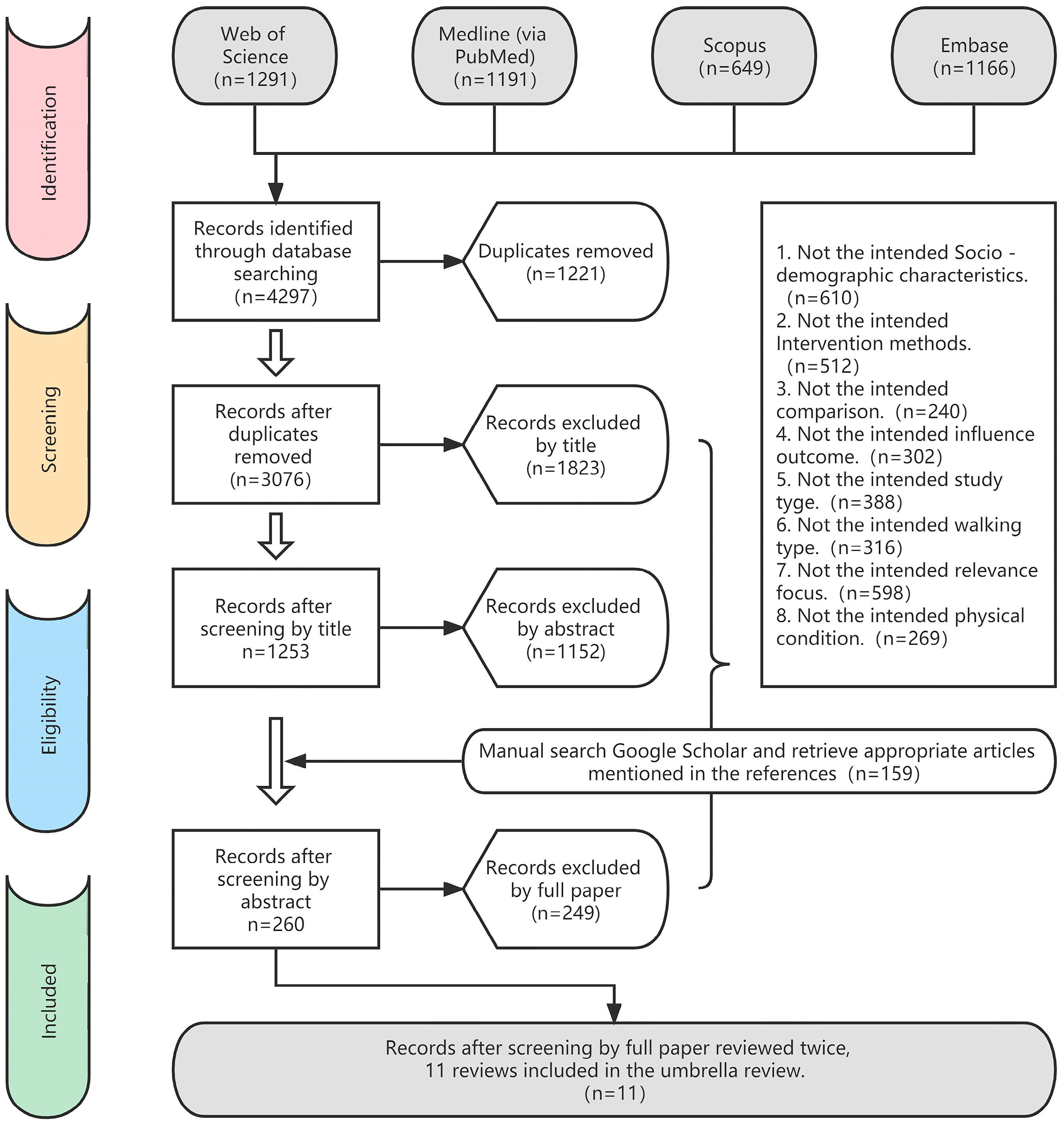
2. Methods
2.1. Design and Registration
2.2. Data Sources and Search Strategy
2.3. Inclusion and Exclusion Criteria
2.4. Methodological Quality
2.5. Data Extraction
- First author, year of publication, search date, number of primary studies meeting the requirements of this umbrella review, the total number of primary studies included in the included systematic reviews, characteristics of the population included (e.g., number of participants, healthy condition, the gender proportion, and age range/mean age).
- Aim of the review, type of intervention, interventions, and diagnostic criteria.
- Effect size results for intervention controls, metric of effect size.
- Overall results and main findings, overall recommendations, and limitations as provided by the review itself.
2.6. Data Synthesis and Analysis
2.7. Evidence Map
- Number of studies (figure size): the size of each figure is directly proportional to the number of original studies included in each of the meta-analyses.
- Study quality and type of action relationship (symbol): The methodological quality evaluated in each study is represented by color. The action relationship type determines each symbol inside the bubble (X: contested effect relationship; −: negative correlation; +: positive correlation).
- X-axis: in the descriptive mapping, the environmental variables of each study are on the X-axis.
- Y-axis: descriptive mapping representing the gait characteristics variables of the older people for each study.
| References, Author(s) (year) | Search Date | Included in the Umbrella Review/ Included in the Review | Aim of the Review | Number of Participants | Health Condition | Age | Intervention | + * | − | Gait Effect |
|---|---|---|---|---|---|---|---|---|---|---|
| Mehdizadeh et al. (2021) [37] | 20 February | 4/34 | Investigate the association between measures of gait center of pressure (COP) and aging and falls. | 65 | Healthy older people | Over 65 | During obstacle crossing | √ | Average anterior-posterior and medio-lateral center of pressure displacements | |
| √ | Average anterior-posterior and medio-lateral center of pressure velocity | |||||||||
| Valipoor et al. (2020) [38] | 2018 | 4/45 | To determine the current state of knowledge of the effects of internal scale elements of the human settlements’ environment on falls in older people, the extent to which the effects are studied, and the extent to which these effects are measured. | 95 | Older people | / | Carpet | / | Postural sway | |
| Flooring type | / | Dynamic balance | ||||||||
| Ghai et al. (2017) [39] | 17 May | 18/34 | To analyze the effects of rhythmic auditory cues on spatiotemporal gait parameters among healthy young and older people participants. | 355 | Healthy older people | 68 ± 5.6 years | Rhythmic auditory cues | √ | Gait velocity | |
| √ | Stride length | |||||||||
| √ | Cadence | |||||||||
| √ | Coefficient of variability stride time | |||||||||
| √ | Coefficient of variability stride length | |||||||||
| Non-modulated rhythmic auditory cues | √ | Gait velocity | ||||||||
| √ | Stride length | |||||||||
| √ | Cadence | |||||||||
| Aboutorabi et al. (2017) [40] | 2002 to July 2015 | 12/15 | To summarize the current evidence for subthreshold vibration interventions on postural control and gait in older people. | 250 | Health older people and other | Over 55 | Vibration interventions | √ | Postural sway | |
| √ | Postural stability | |||||||||
| √ | COP velocity | |||||||||
| √ | Balance | |||||||||
| √ | Gait speed | |||||||||
| √ | Cadence | |||||||||
| Noise stimulation | / | Stride length | ||||||||
| / | Gait variability | |||||||||
| Uiga et al. (2015) [41] | July 2014 | 11/25 | To synthesize the available evidence on the role of gaze behavior during locomotion (i.e., walking, turning,) to explore the role of gaze behavior among older people during different forms of locomotion. | 437 | Health older people and other | Over 60 | Stepping over an obstacle | √ | Stride length | |
| √ | Gait velocity | |||||||||
| √ | Saccade/step latency | |||||||||
| Walking up and down stairs | √ | Saccade/step interactions time | ||||||||
| √ | Stride length | |||||||||
| √ | Single stance phase | |||||||||
| Turning around a corner | √ | Gait velocity | ||||||||
| Nightingale et al. (2014) [42] | February 2012 | 24/88 | Summarize the literature related to timed stair tests. We aimed to determine whether stairs would be able to differentiate between participant groups by age or impairment. | 3365 | Healthy older people | Over 65 | Stair ascent | √ | Gait velocity | |
| Stair descent | √ | Gait velocity | ||||||||
| Stair ascent/stair descent | √ | Gait velocity | ||||||||
| Orth et al. (2013) [43] | August 2012 | 7/23 | This study was to evaluate the efficacy of textured materials for enhancing perceptual motor functionality. | / | Healthy older people | Over 65 | Textured materials | / | Gait performance | |
| Alfuth et al. (2012) [44] | 2000 to 2011 | 7/23 | This paper was to provide a review of studies reporting the effects of changes in plantar feedback on human gait characteristics. | 307 | Health older people and other | Over 55 | Walking on uneven surface and irregular surface | √ | Gait velocity | |
| √ | Step length | |||||||||
| √ | Step width | |||||||||
| √ | Cadence | |||||||||
| √ | Gait variability | |||||||||
| Galna et al. (2009) [45] | August 2008 | 11/15 | The primary aim was to investigate whether older people are more likely to contact ground-based obstacles when walking under time-constrained and unconstrained conditions. The second aim examined whether older people approach and step over obstacles using different spatiotemporal, kinematic, and kinetic strategies than younger adults. | / | Healthy older people | 68–76 | During obstacle crossing | √ | Stride length | |
| √ | Gait velocity | |||||||||
| √ | Measure maximum range of motion (rom) | |||||||||
| / | Hip, knee, and ankle range of motion | |||||||||
| √ | Eccentric contraction of the stance limb hip abductors | |||||||||
| √ | Vertical hip power (defined as the power used to raise the stance hip) at toe-off | |||||||||
| √ | Pelvic drop during stance, the height of the crossing limb. | |||||||||
| Lachance et al. (2017) [46] | October 2015 | 14/84 | What evidence exists from experiments conducted in a controlled, laboratory environment about balance, gait and mobility performance, and/or assistive device use on compliant flooring systems. | / | Older people | Over 65 | Compliant flooring systems | / | Gait speed | |
| / | Step length | |||||||||
| / | Toe clearance | |||||||||
| / | Timed up-and-go time | |||||||||
| Taylor et al. (2022) [10] | 2015 to 30 May 2022 | 12/33 | This systematic review aimed to assess current perturbation methods and outcome variables used to report participant biomechanical responses during walking. | 294/779 | Healthy older people | Over 65 | Perturbations during gait | √ | In base of support | |
| √ | Muscle activation | |||||||||
| √ | Dynamic stability | |||||||||
| √ | Margin of stability | |||||||||
| √ | Centre of mass sway | |||||||||
| √ | Cadence | |||||||||
| √ | Single support time and swing time | |||||||||
| / | Joint angle range of motion, | |||||||||
| / | Step width | |||||||||
| / | Step length | |||||||||
3. Results
3.1. Search Results
3.2. Characteristics of Included Studies
3.3. Methodological Quality of Included Studies
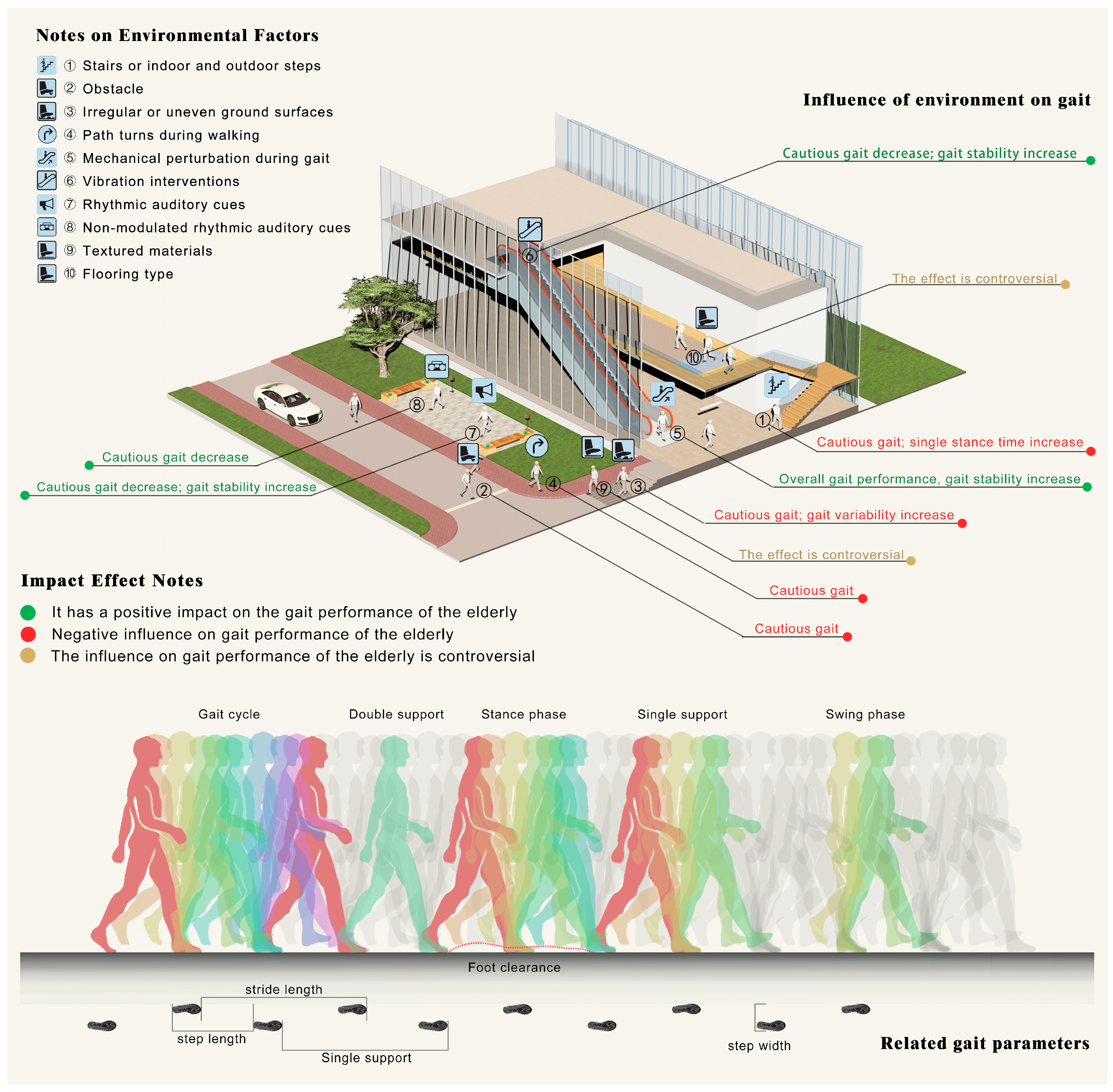
3.4. Findings: Associations between Gait Outcomes and Environment Features
3.4.1. Stairs or Indoor and Outdoor Steps
3.4.2. Obstacle
3.4.3. Irregular or Uneven Ground Surfaces
3.4.4. Path Turns during Walking
3.4.5. Mechanical Perturbation during Gait
3.4.6. Vibration Interventions
3.4.7. Auditory Cues
3.4.8. Textured Materials
3.4.9. Flooring Type
4. Discussion
4.1. Affected by the Pedestrian Environment: The Cautious Degree of Active Control Gait
4.2. Affected by the Pedestrian Environment: Gait Stability Changes Caused by Gait Adaptation
4.3. Pedestrian Environment Factors Influencing Other Physical Performance and Control
4.4. Disputed Pedestrian Environment Factors Affecting the Gait of the Older People
4.5. Limitations and Future Research Directions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| 1. Web of Science | |
| 1 | “elder*” or “aged” or “old* people*” or “old* adult*” “aged” |
| 2 | “walk*” or “pedestrian*” or “perambulat*” or “foot” or “gait” |
| 3 | #1 AND #2 |
| 4 | “environment*” or “circumstance” or “surround*” or “settlement*” or “residence” |
| 5 | #3 AND #4 |
| 6 | “health” or “physical” or “biomechani*” or “physiolog*” or “risk factors” |
| 7 | #5 AND #6 |
| 8 | influence* or “effact*” or “impact*” or “relation*” or “factor*” or “status” or “outcomes” or “aspects” or “responses” |
| 9 | #7 AND #8 = (((((TS = (“elder*” or “aged” or “old* people*” or “old* adult*” “aged”)) AND TS = (“environment*” or “circumstance” or “surround*” or “settlement*” or “residence”)) AND TS = (“walk*” or “pedestrian*” or “perambulat*” or “foot” or “gait”)) AND TS = (“health” or “physical” or “biomechani*” or “physiolog*” or “risk factors”)) AND TS = (influence* or “effact*” or “impact*” or “relation*” or “factor*” or “status” or “outcomes” or “aspects” or “responses”)) |
| 2. Medline (via PubMed) | |
| 1 | (“Aged”[Mesh] OR “Frail Elderly”[Mesh] OR “Geriatric Assessment”[Mesh] OR “Geroscience”[Mesh]) |
| 2 | (“Environment”[Mesh] OR “Social Environment”[Mesh] OR “Environment Design”[Mesh] OR “Environment and Public Health”[Mesh] OR “Home Environment”[Mesh] OR “Built Environment”[Mesh]) |
| 3 | #1 AND #2 |
| 4 | (“Walking”[Mesh] OR “Gait”[Mesh]) OR “Gait Analysis”[Mesh] OR “Walking Speed”[Mesh]) |
| 5 | #3 AND #4 |
| 6 | (“Geriatric Assessment”[Mesh] OR “Geroscience”[Mesh] OR “Physical Functional Performance”[Mesh] OR “Athletic Performance”[Mesh] OR “Physiology”[Mesh] OR “Physical Stimulation”[Mesh]) |
| 7 | #5 AND #6 |
| 8 | (“Influence*” or “Effact*” or “Impact*” or “Relation*” or “Factor*” or “Status” or “Outcomes” or “Aspects” or “Responses”) |
| 9 | #7 OR #8 = ((“Aged”[Mesh] OR “Frail Elderly”[Mesh] OR “Geriatric Assessment”[Mesh] OR “Geroscience”[Mesh])) AND ((“Environment”[Mesh] OR “Social Environment”[Mesh] OR “Environment Design”[Mesh] OR “Environment and Public Health”[Mesh] OR “Home Environment”[Mesh] OR “Built Environment”[Mesh])) AND ((“Walking”[Mesh] OR “Gait”[Mesh]) OR “Gait Analysis”[Mesh] OR “Walking Speed”[Mesh])) AND ((“Physical Functional Performance”[Mesh] OR “Athletic Performance”[Mesh]) OR (“Physiology”[Mesh] OR “Physical Stimulation”[Mesh])) AND ((“Influence*” or “Effact*” or “Impact*” or “Relation*” or “Factor*” or “Status” or “Outcomes” or “Aspects” or “Responses”)) AND (review) |
| 3. Scopus | |
| 1 | “elder*” or “aged” or “old* people*” or “old* adult*” “aged” |
| 2 | “walk*” or “pedestrian*” or “perambulat*” or “foot” or “gait” |
| 3 | “environment*” or “circumstance” or “surround*” or “settlement*” or “residence” |
| 4 | “health” or “physical” or “biomechani*” or “physiolog*” or “risk factors” |
| 5 | influence* or “effact*” or “impact*” or “relation*” or “factor*” or “status” or “outcomes” or “aspects” or “responses” |
| 6 | (“elder*” or “aged” or “old* people*” or “old* adult*” “aged”) AND (“environment*” or “circumstance” or “surround*” or “settlement*” or “residence”) AND (“walk*” or “pedestrian*” or “perambulat*” or “foot” or “gait”) AND (“health” or “physical” or “biomechani*” or “physiolog*” or “risk factors”) AND (influence* or “effact*” or “impact*” or “relation*” or “factor*” or “status” or “outcomes” or “aspects” or “responses”) |
| 4. Embase | |
| 1 | “elder*” or “aged” or “old* people*” or “old* adult*” “aged” |
| 2 | “walk*” or “pedestrian*” or “perambulat*” or “foot” or “gait” |
| 3 | “environment*” or “circumstance” or “surround*” or “settlement*” or “residence” |
| 4 | “health” or “physical” or “biomechani*” or “physiolog*” or “risk factors” |
| 5 | influence* or “effact*” or “impact*” or “relation*” or “factor*” or “status” or “outcomes” or “aspects” or “responses” |
| 6 | (“elder*” or “aged” or “old* people*” or “old* adult*” “aged”) AND (“environment*” or “circumstance” or “surround*” or “settlement*” or “residence”) AND (“walk*” or “pedestrian*” or “perambulat*” or “foot” or “gait”) AND (“health” or “physical” or “biomechani*” or “physiolog*” or “risk factors”) AND (influence* or “effact*” or “impact*” or “relation*” or “factor*” or “status” or “outcomes” or “aspects” or “responses”) |
References
- United Nations. 2019 Revision of World Population Prospects; United Nations: New York, NY, USA, 2019. [Google Scholar]
- Aged & Community Services Australia, National Rural Health Alliance. Older People and Aged Care in Rural, Regional and Remote Australia: A Discussion Paper; National Rural Health Alliance: Deakin West, Australia, 2004; pp. 1–25. [Google Scholar]
- Britt, H. It’s Different in the Bush: A Comparison of General Practice Activity in Metropolitan and Rural Areas of Australia 1998–2000; Australian Institute of Health and Welfare: Canberra, Australia, 2001.
- World Health Organization. World Report on Ageing and Health 2015. Available online: https://www.who.int/ageing/healthy-ageing/en/ (accessed on 28 June 2022).
- Van Cauwenberg, J.; De Bourdeaudhuij, I.; De Meester, F.; Van Dyck, D.; Salmon, J.; Clarys, P.; Deforche, B. Relationship between the physical environment and physical activity in older adults: A systematic review. Health Place 2011, 17, 458–469. [Google Scholar] [CrossRef]
- Haselwandter, E.M.; Corcoran, M.P.; Folta, S.C.; Hyatt, R.; Fenton, M.; Nelson, M.E. The Built Environment, Physical Activity, and Aging in the United States: A State of the Science Review. J. Aging Phys. Act. 2015, 23, 323–329. [Google Scholar] [CrossRef]
- The Huffington Post, B.C. Walk Score Names Vancouver as Canada’s “Most Walkable City”; HuffPost: Toronto, ON, Canada, 2013. [Google Scholar]
- Thaler-Kall, K.; Peters, A.; Thorand, B.; Grill, E.; Autenrieth, C.S.; Horsch, A.; Meisinger, C. Description of spatio-temporal gait parameters in elderly people and their association with history of falls: Results of the population-based cross-sectional KORA-Age study. BMC Geriatr. 2015, 15, 8. [Google Scholar] [CrossRef]
- Hamacher, D.; Singh, N.B.; Van Dieen, J.H.; Heller, M.O.; Taylor, W.R. Kinematic measures for assessing gait stability in elderly individuals: A systematic review. J. R. Soc. Interface 2011, 8, 1682–1698. [Google Scholar] [CrossRef] [PubMed]
- Taylor, Z.; Walsh, G.S.; Hawkins, H.; Inacio, M.; Esser, P. Perturbations during Gait: A Systematic Review of Methodologies and Outcomes. Sensors 2022, 22, 5927. [Google Scholar] [CrossRef] [PubMed]
- Levine, D.; Richards, J.; Whittle, M.W. Whittle’s Gait Analysis; Elsevier: London, UK, 2012. [Google Scholar]
- Belbasis, L.; Bellou, V.; Evangelou, E.; Ioannidis, J.P.A.; Tzoulaki, L. Environmental risk factors and multiple sclerosis: An umbrella review of systematic reviews and meta-analyses. Lancet Neurol. 2015, 14, 263–273. [Google Scholar] [CrossRef] [PubMed]
- Bertucco, M.; Cesari, P. Dimensional analysis and ground reaction forces for stair climbing: Effects of age and task difficulty. Gait Posture 2009, 29, 326–331. [Google Scholar] [CrossRef]
- Cesari, P. An invariant guiding stair descent by young and old adults. Exp. Aging Res. 2005, 31, 441–455. [Google Scholar] [CrossRef] [PubMed]
- Ogilvie, D.; Egan, M.; Hamilton, V.; Petticrew, M. Promoting walking and cycling as an alternative to using cars: Systematic review. BMJ 2004, 329, 763–766. [Google Scholar] [CrossRef]
- Lee, C.; Moudon, A.V. Physical Activity and Environment Research in the Health Field: Implications for Urban and Transportation Planning Practice and Research. J. Plan. Lit. 2004, 19, 147–181. [Google Scholar] [CrossRef]
- Gadais, T.; Boulanger, M.; Trudeau, F.; Rivard, M.-C. Environments favorable to healthy lifestyles: A systematic review of initiatives in Canada. J. Sport. Health Sci. 2018, 7, 7–18. [Google Scholar] [CrossRef] [PubMed]
- Tuckett, A.G.; Banchoff, A.W.; Winter, S.J.; King, A.C. The built environment and older adults: A literature review and an applied approach to engaging older adults in built environment improvements for health. Int. J. Older People Nurs. 2018, 13, e12171. [Google Scholar] [CrossRef] [PubMed]
- Won, J.; Lee, C.; Forjuoh, S.N.; Ory, M.G. Neighborhood safety factors associated with older adults’ health-related outcomes: A systematic literature review. Soc. Sci. Med. 2016, 165, 177–186. [Google Scholar] [CrossRef] [PubMed]
- Cerin, E.; Nathan, A.; van Cauwenberg, J.; Barnett, D.W.; Barnett, A.; Council Environm Phys, A. The neighbourhood physical environment and active travel in older adults: A systematic review and Meta-analysis. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 23. [Google Scholar] [CrossRef]
- Portegijs, E.; Keskinen, K.E.; Tsai, L.T.; Rantanen, T.; Rantakokko, M. Physical Limitations, Walkability, Perceived Environmental Facilitators and Physical Activity of Older Adults in Finland. Int. J. Environ. Res. Public Health 2017, 14, 333. [Google Scholar] [CrossRef] [PubMed]
- Reid, S.M.; Novak, A.C.; Brouwer, B.; Costigan, P.A. Relationship between stair ambulation with and without a handrail and centre of pressure velocities during stair ascent and descent. Gait Posture 2011, 34, 529–532. [Google Scholar] [CrossRef] [PubMed]
- Jacobs, J.V. A review of stairway falls and stair negotiation: Lessons learned and future needs to reduce injury. Gait Posture 2016, 49, 159–167. [Google Scholar] [CrossRef]
- Komisar, V.; Nirmalanathan, K.; Novak, A.C. Influence of handrail height and fall direction on center of mass control and the physical demands of reach-to-grasp balance recovery reactions. Gait Posture 2018, 60, 209–216. [Google Scholar] [CrossRef]
- Novak, A.C.; Komisar, V.; Maki, B.E.; Fernie, G.R. Age-related differences in dynamic balance control during stair descent and effect of varying step geometry. Appl. Ergon. 2016, 52, 275–284. [Google Scholar] [CrossRef]
- Hunt, H.; Pollock, A.; Campbell, P.; Estcourt, L.; Brunton, G. An introduction to overviews of reviews: Planning a relevant research question and objective for an overview. Syst Rev. 2018, 7, 39. [Google Scholar] [CrossRef] [PubMed]
- Ioannidis, J.P.A. Integration of evidence from multiple meta-analyses: A primer on umbrella reviews, treatment networks and multiple treatments meta-analyses. Can. Med. Assoc. J. 2009, 181, 488–493. [Google Scholar] [CrossRef] [PubMed]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gotzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: Explanation and elaboration. BMJ-Br. Med. J. 2009, 339, 37. [Google Scholar] [CrossRef] [PubMed]
- Stone, P.W. Popping the (PICO) question in research and evidence-based practice. Appl. Nurs. Res. 2002, 15, 197–198. [Google Scholar] [CrossRef] [PubMed]
- Shea, B.J.; Reeves, B.C.; Wells, G.; Thuku, M.; Hamel, C.; Moran, J.; Moher, D.; Tugwell, P.; Welch, V.; Kristjansson, E.; et al. AMSTAR 2: A critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ-Br. Med. J. 2017, 358, 8. [Google Scholar] [CrossRef] [PubMed]
- Shea, B.J.; Grimshaw, J.M.; Wells, G.A.; Boers, M.; Andersson, N.; Hamel, C.; Porter, A.C.; Tugwell, P.; Moher, D.; Bouter, L.M. Development of AMSTAR: A measurement tool to assess the methodological quality of systematic reviews. BMC Med. Res. Methodol. 2007, 7, 7. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. Cochrane Handbook for Systematic Reviews of Interventions, 2nd ed.; John Wiley & Sons, Incorporated: Newark, NJ, USA, 2019. [Google Scholar]
- Aromataris, E.; Fernandez, R.; Godfrey, C.M.; Holly, C.; Khalil, H.; Tungpunkom, P. Summarizing systematic reviews: Methodological development, conduct and reporting of an umbrella review approach. Int. J. Evid.-Based Healthc. 2015, 13, 132–140. [Google Scholar] [CrossRef]
- Egger, M.; Smith, G.D.; Schneider, M.; Minder, C. Bias in Meta-analysis detected by a simple, graphical test. BMJ-Br. Med. J. 1997, 315, 629–634. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. Br. Med. J. 2003, 327, 557–560. [Google Scholar] [CrossRef]
- Sterne, J.A.C.; Sutton, A.J.; Ioannidis, J.P.A.; Terrin, N.; Jones, D.R.; Lau, J.; Carpenter, J.; Rucker, G.; Harbord, R.M.; Schmid, C.H.; et al. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ-Br. Med. J. 2011, 343, 8. [Google Scholar] [CrossRef] [PubMed]
- Mehdizadeh, S.; Van Ooteghem, K.; Gulka, H.; Nabavi, H.; Faieghi, M.; Taati, B.; Iaboni, A. A systematic review of center of pressure measures to quantify gait changes in older adults. Exp. Gerontol. 2021, 143, 16. [Google Scholar] [CrossRef] [PubMed]
- Valipoor, S.; Pati, D.; Kazem-Zadeh, M.; Mihandoust, S.; Mohammadigorji, S. Falls in Older Adults: A Systematic Review of Literature on Interior-Scale Elements of the Built Environment. J. Aging Environ. 2020, 34, 351–374. [Google Scholar] [CrossRef]
- Ghai, S.; Ghai, I.; Effenberg, A.O. Effect of Rhythmic Auditory Cueing on Aging Gait: A Systematic Review and Meta-Analysis. Aging Dis. 2018, 9, 901–923. [Google Scholar] [CrossRef] [PubMed]
- Aboutorabi, A.; Arazpour, M.; Bahramizadeh, M.; Farahmand, F.; Fadayevatan, R. Effect of vibration on postural control and gait of elderly subjects: A systematic review. Aging Clin. Exp. Res. 2018, 30, 713–726. [Google Scholar] [CrossRef]
- Uiga, L.; Cheng, K.C.; Wilson, M.R.; Masters, R.S.W.; Capio, C.M. Acquiring visual information for locomotion by older adults: A systematic review. Ageing Res. Rev. 2015, 20, 24–34. [Google Scholar] [CrossRef]
- Nightingale, E.J.; Pourkazemi, F.; Hiller, C.E. Systematic review of timed stair tests. J. Rehabil. Res. Dev. 2014, 51, 335–350. [Google Scholar] [CrossRef] [PubMed]
- Orth, D.; Davids, K.; Wheat, J.; Seifert, L.; Liukkonen, J.; Jaakkola, T.; Ashford, D.; Kerr, G. The Role of Textured Material in Supporting Perceptual-Motor Functions. PLoS ONE 2013, 8, 14. [Google Scholar] [CrossRef] [PubMed]
- Alfuth, M.; Rosenbaum, D. Effects of changes in plantar sensory feedback on human gait characteristics: A systematic review. Footwear Sci. 2012, 4, 1–22. [Google Scholar] [CrossRef]
- Galna, B.; Peters, A.; Murphy, A.T.; Morris, M.E. Obstacle crossing deficits in older adults: A systematic review. Gait Posture 2009, 30, 270–275. [Google Scholar] [CrossRef]
- Lachance, C.C.; Jurkowski, M.P.; Dymarz, A.C.; Robinovitch, S.N.; Feldman, F.; Laing, A.C.; Mackey, D.C. Compliant flooring to prevent fall-related injuries in older adults: A scoping review of biomechanical efficacy, clinical effectiveness, cost-effectiveness, and workplace safety. PLoS ONE 2017, 12, 23. [Google Scholar] [CrossRef]
- Di Fabio, R.P.; Zampieri, C.; Henke, J.; Olson, K.; Rickheim, D.; Russell, M. Influence of Elderly Executive Cognitive Function on Attention in the Lower Visual Field during Step Initiation. Gerontology 2005, 51, 94–107. [Google Scholar] [CrossRef] [PubMed]
- Young, W.R.; Hollands, M.A. Evidence for age-related decline in visuomotor function and reactive stepping adjustments. Gait Posture 2012, 36, 477–481. [Google Scholar] [CrossRef] [PubMed]
- Di Fabio, R.P.; Greany, J.F.; Zampieri, C. Saccade-stepping interactions revise the motor plan for obstacle avoidance. J. Mot. Behav. 2003, 35, 383–397. [Google Scholar] [CrossRef] [PubMed]
- McFayden, B.J.; Prince, F. Avoidance and accommodation of surface height changes by healthy, community-dwelling, young, and elderly men. J. Gerontol. Ser. A-Biol. Sci. Med. Sci. 2002, 57, B166–B174. [Google Scholar] [CrossRef] [PubMed]
- Chapman, G.J.; Hollands, M.A. Evidence that older adult fallers prioritise the planning of future stepping actions over the accurate execution of ongoing steps during complex locomotor tasks. Gait Posture 2007, 26, 59–67. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.C.; Ashtonmiller, J.A.; Alexander, N.B.; Schultz, A.B. Stepping over obstacles: Gait patterns of healthy young and old adults. J. Gerontol. 1991, 46, M196–M203. [Google Scholar] [CrossRef]
- Lowrey, C.R.; Watson, A.; Vallis, L.A. Age-related changes in avoidance strategies when negotiating single and multiple obstacles. Exp. Brain Res. 2007, 182, 289–299. [Google Scholar] [CrossRef] [PubMed]
- McKenzie, N.C.; Brown, L.A. Obstacle negotiation kinematics: Age-dependent effects of postural threat. Gait Posture 2004, 19, 226–234. [Google Scholar] [CrossRef]
- Chen, H.C.; Ashtonmiller, J.A.; Alexander, N.B.; Schultz, A.B. Age effects on strategies used to avoid obstacles. Gait Posture 1994, 2, 139–146. [Google Scholar] [CrossRef]
- Menant, J.C.; Steele, J.R.; Menz, H.B.; Munro, B.J.; Lord, S.R. Rapid gait termination: Effects of age, walking surfaces and footwear characteristics. Gait Posture 2009, 30, 65–70. [Google Scholar] [CrossRef]
- Thies, S.B.; Richardson, J.K.; Ashton-Miller, J.A. Effects of surface irregularity and lighting on step variability during gait: A study in healthy young and older women. Gait Posture 2005, 22, 26–31. [Google Scholar] [CrossRef]
- Paquette, M.R.; Vallis, L.A. Age-related kinematic changes in late visual-cueing during obstacle circumvention. Exp. Brain Res. 2010, 203, 563–574. [Google Scholar] [CrossRef] [PubMed]
- Petrofsky, J.S.; Bweir, S.; Andal, A.; Chavez, J.; Crane, A.; Saunders, J.; Laymon, M. Joint acceleration during gait in relation to age. Eur. J. Appl. Physiol. 2004, 92, 254–262. [Google Scholar] [CrossRef] [PubMed]
- Aprigliano, F.; Monaco, V.; Tropea, P.; Martelli, D.; Vitiello, N.; Micera, S. Effectiveness of a Robot-Mediated Strategy While Counteracting Multidirectional Slippages. Robotica 2019, 37, 2119–2131. [Google Scholar] [CrossRef]
- Arvin, M.; Hoozemans, M.J.M.; Pijnappels, M.; Duysens, J.; Verschueren, S.M.P.; Dieen, J.H.V. Where to Step? Contributions of Stance Leg Muscle Spindle Afference to Planning of Mediolateral Foot Placement for Balance Control in Young and Old Adults. Front. Physiol. 2018, 9, 1134. [Google Scholar] [CrossRef] [PubMed]
- Vervoort, D.; Buurke, T.J.W.; Vuillerme, N.; Hortobagyi, T.; den Otter, R.; Lamoth, C. Adaptive Control of Dynamic Balance across the Adult Lifespan. Med. Sci. Sport. Exerc. 2020, 52, 2270–2277. [Google Scholar] [CrossRef] [PubMed]
- Madehkhaksar, F.; Klenk, J.; Sczuka, K.; Gordt, K.; Melzer, I.; Schwenk, M. The effects of unexpected mechanical perturbations during treadmill walking on spatiotemporal gait parameters, and the dynamic stability measures by which to quantify postural response. PLoS ONE 2018, 13, e0195902. [Google Scholar] [CrossRef] [PubMed]
- Onushko, T.; Boerger, T.; Van Dehy, J.; Schmit, B.D. Dynamic stability and stepping strategies of young healthy adults walking on an oscillating treadmill. PLoS ONE 2019, 14, e0212207. [Google Scholar] [CrossRef]
- Nestico, J.; Novak, A.; Perry, S.D.; Mansfield, A. Does increased gait variability improve stability when faced with an expected balance perturbation during treadmill walking? Gait Posture 2021, 86, 94–100. [Google Scholar] [CrossRef]
- Golyski, P.R.; Vazquez, E.; Leestma, J.K.; Sawicki, G.S. Onset timing of treadmill belt perturbations influences stability during walking. J. Biomech. 2022, 130, 110800. [Google Scholar] [CrossRef]
- Rieger, M.M.; Papegaaij, S.; Pijnappels, M.; Steenbrink, F.; van Dieën, J.H. Transfer and retention effects of gait training with anterior-posterior perturbations to postural responses after medio-lateral gait perturbations in older adults. Clin. Biomech. 2020, 75, 104988. [Google Scholar] [CrossRef]
- Kao, P.-C.; Pierro, M.A. Motor adaptation to cognitive challenges and walking perturbations in healthy young adults. Gait Posture 2022, 92, 167–175. [Google Scholar] [CrossRef] [PubMed]
- Roeles, S.; Rowe, P.J.; Bruijn, S.M.; Childs, C.R.; Tarfali, G.D.; Steenbrink, F.; Pijnappels, M. Gait stability in response to platform, belt, and sensory perturbations in young and older adults. Med. Biol. Eng. Comput. 2018, 56, 2325–2335. [Google Scholar] [CrossRef] [PubMed]
- Martelli, D.; Jiyeon, K.; Agrawal, S.K. A Single Session of Perturbation-Based Gait Training with the A-TPAD Improves Dynamic Stability in Healthy Young Subjects. In Proceedings of the 2017 International Conference on Rehabilitation Robotics, London, UK, 17–20 July 2017; IEEE: Piscataway, NJ, USA; pp. 479–484. [Google Scholar]
- Francis, C.A.; Franz, J.R.; O‘Connor, S.M.; Thelen, D.G. Gait variability in healthy old adults is more affected by a visual perturbation than by a cognitive or narrow step placement demand. Gait Posture 2015, 42, 380–385. [Google Scholar] [CrossRef] [PubMed]
- Kurz, I.; Gimmon, Y.; Shapiro, A.; Debi, R.; Snir, Y.; Melzer, I. Unexpected perturbations training improves balance control and voluntary stepping times in older adults—A double blind randomized control trial. BMC Geriatr. 2016, 16, 58. [Google Scholar] [CrossRef] [PubMed]
- Martelli, D.; Vashista, V.; Micera, S.; Agrawal, S.K. Direction-Dependent Adaptation of Dynamic Gait Stability Following Waist-Pull Perturbations. IEEE Trans. Neural. Syst. Rehabil. Eng. 2016, 24, 1304–1313. [Google Scholar] [CrossRef] [PubMed]
- Aprigliano, F.; Martelli, D.; Tropea, P.; Micera, S.; Monaco, V. Effects of Slipping-Like Perturbation Intensity on the Dynamical Stability. In Proceedings of the IEEE Engineering in Medicine and Biology Society, Milan, Italy, 25–29 August 2015; IEEE: Piscataway, NJ, USA; pp. 5295–5298. [Google Scholar]
- Punt, M.M.; Bruijn, S.M.P.; Roeles, S.M.; van de Port, I.G.P.; Wittink, H.P.; van Dieën, J.H.P. Responses to gait perturbations in stroke survivors who prospectively experienced falls or no falls. J. Biomech. 2017, 55, 56–63. [Google Scholar] [CrossRef] [PubMed]
- Rosenblum, U.; Melzer, I.; Zeilig, G.; Plotnik, M. Muscle activation profile is modulated by unexpected balance loss in walking. Gait Posture 2022, 93, 64–72. [Google Scholar] [CrossRef] [PubMed]
- Best, A.N.; Martin, J.-P.; Li, Q.; Wu, A.R. Stepping behaviour contributes little to balance control against continuous mediolateral trunk perturbations. J. Exp. Biol. 2019, 222, jeb212787. [Google Scholar] [CrossRef]
- Shulman, D.; Spencer, A.; Vallis, L.A. Age-related alterations in reactive stepping following unexpected mediolateral perturbations during gait initiation. Gait Posture 2018, 64, 130–134. [Google Scholar] [CrossRef]
- Haarman, J.A.M.; Vlutters, M.; Olde Keizer, R.A.C.M.; Van Asseldonk, E.H.F.; Buurke, J.H.; Reenalda, J.; Rietman, J.S.; Van Der Kooij, H. Paretic versus non-paretic stepping responses following pelvis perturbations in walking chronic-stage stroke survivors. J. Neuroeng. Rehabil. 2017, 14, 106. [Google Scholar] [CrossRef]
- Hof, A.L.; Duysens, J. Responses of human ankle muscles to mediolateral balance perturbations during walking. Hum. Mov. Sci. 2018, 57, 69–82. [Google Scholar] [CrossRef] [PubMed]
- Rutherford, D.; Baker, M.; Urquhart, N.; Stanish, W. The effect of a frontal plane gait perturbation bout on knee biomechanics and muscle activation in older adults and individuals with knee osteoarthritis. Clin. Biomech. 2022, 92, 105574. [Google Scholar] [CrossRef] [PubMed]
- Galica, A.M.; Kang, H.G.; Priplata, A.A.; D‘Andrea, S.E.; Starobinets, O.V.; Sorond, F.A.; Cupples, L.A.; Lipsitz, L.A. Subsensory vibrations to the feet reduce gait variability in elderly fallers. Gait Posture 2009, 30, 383–387. [Google Scholar] [CrossRef] [PubMed]
- Stephen, D.G.; Wilcox, B.J.; Niemi, J.B.; Franz, J.R.; Kerrigan, C.; D‘Andrea, S.E. Corrigendum to “Baseline-dependent effect of noise-enhanced insoles on gait variability in healthy elderly walkers” [GAIPOS 36 (3) (2012) 537–540]. Gait Posture 2012, 38, 361. [Google Scholar] [CrossRef]
- Lee, S.-W.; Cho, K.-H.; Lee, W.-H. Effect of a local vibration stimulus training programme on postural sway and gait in chronic stroke patients: A randomized controlled trial. Clin. Rehabil. 2013, 27, 921–931. [Google Scholar] [CrossRef] [PubMed]
- Lipsitz, L.A.M.D.; Lough, M.B.S.; Niemi, J.M.S.; Travison, T.P.; Howlett, H.M.E.M.; Manor, B.P. A Shoe Insole Delivering Subsensory Vibratory Noise Improves Balance and Gait in Healthy Elderly People. Arch. Phys. Med. Rehabil. 2015, 96, 432–439. [Google Scholar] [CrossRef]
- Novak, P.; Novak, V. Effect of step-synchronized vibration stimulation of soles on gait in Parkinson’s disease: A pilot study. J. Neuroeng. Rehabil. 2006, 3, 9. [Google Scholar] [CrossRef] [PubMed]
- Wanderley, F.S.P.T.; Alburquerque-Sendín, F.P.; Parizotto, N.A.P.T.P.; Rebelatto, J.R.P.T.P. Effect of Plantar Vibration Stimuli on the Balance of Older Women: A Randomized Controlled Trial. Arch. Phys. Med. Rehabil. 2011, 92, 199–206. [Google Scholar] [CrossRef] [PubMed]
- Priplata, A.A.; Niemi, J.B.; Harry, J.D.; Lipsitz, L.A.; Collins, J.J. Vibrating insoles and balance control in elderly people. Lancet 2003, 362, 1123–1124. [Google Scholar] [CrossRef] [PubMed]
- Dettmer, M.; Pourmoghaddam, A.; Lee, B.-C.; Layne, C.S. Effects of aging and tactile stochastic resonance on postural performance and postural control in a sensory conflict task. Somatosens. Mot. Res. 2015, 32, 128–135. [Google Scholar] [CrossRef] [PubMed]
- Wei, Q.; Liu, D.-H.; Wang, K.-H.; Liu, Q.; Abbod, M.F.; Jiang, B.C.; Chen, K.-P.; Wu, C.; Shieh, J.-S. Multivariate multiscale entropy applied to center of pressure signals analysis: An effect of vibration stimulation of shoes. Entropy 2012, 14, 2157–2172. [Google Scholar] [CrossRef]
- Yu, M.; Piao, Y.-J.; Kim, S.-H.; Kim, D.-W.; Kim, N.-G. Effects of tendon vibration during one-legged and two-legged stance in elderly individuals. Int. J. Precis. Eng. Manuf. 2010, 11, 969–977. [Google Scholar] [CrossRef]
- Priplata, A.; Niemi, J.; Salen, M.; Harry, J.; Lipsitz, L.A.; Collins, J.J. Noise-enhanced human balance control. Phys. Rev. Lett. 2002, 89, 238101. [Google Scholar] [CrossRef] [PubMed]
- Priplata, A.A.; Patritti, B.L.; Niemi, J.B.; Hughes, R.; Gravelle, D.C.; Lipsitz, L.A.; Veves, A.; Stein, J.; Bonato, P.; Collins, J.J. Noise-enhanced balance control in patients with diabetes and patients with stroke. Ann. Neurol. 2006, 59, 4–12. [Google Scholar] [CrossRef] [PubMed]
- Rochester, L.; Hetherington, V.; Jones, D.; Nieuwboer, A.; Willems, A.-M.; Kwakkel, G.; Van Wegen, E. The Effect of External Rhythmic Cues (Auditory and Visual) on Walking During a Functional Task in Homes of People With Parkinson ‘s Disease. Arch. Phys. Med. Rehabil. 2005, 86, 999–1006. [Google Scholar] [CrossRef] [PubMed]
- Baram, Y.; Aharon-Peretz, J.; Badarny, S.; Susel, Z.; Schlesinger, I. Closed-loop auditory feedback for the improvement of gait in patients with Parkinson’s disease. J. Neurol. Sci. 2015, 363, 104–106. [Google Scholar] [CrossRef]
- Schreiber, C.; Remacle, A.; Chantraine, F.; Kolanowski, E.; Moissenet, F. Influence of a rhythmic auditory stimulation on asymptomatic gait. Gait Posture 2016, 50, 17–22. [Google Scholar] [CrossRef] [PubMed]
- Hartmann, A.; Murer, K.; de Bie, R.A.; de Bruin, E.D. The effect of a training program combined with augmented afferent feedback from the feet using shoe insoles on gait performance and muscle power in older adults: A randomised controlled trial. Disabil. Rehabil. 2010, 32, 755–764. [Google Scholar] [CrossRef] [PubMed]
- Hatton, A.L.; Dixon, J.; Rome, K.; Newton, J.L.; Martin, D.J. Altering gait by way of stimulation of the plantar surface of the foot: The immediate effect of wearing textured insoles in older fallers. J. Foot Ankle Res. 2012, 5, 11. [Google Scholar] [CrossRef] [PubMed]
- Jenkins, M.E.; Almeida, Q.J.; Spaulding, S.J.; van Oostveen, R.B.; Holmes, J.D.; Johnson, A.M.; Perry, S.D. Plantar cutaneous sensory stimulation improves single-limb support time, and EMG activation patterns among individuals with Parkinson’s disease. Park. Relat. Disord. 2009, 15, 697–702. [Google Scholar] [CrossRef] [PubMed]
- Dixon, J.; Gamesby, H.; Robinson, J.; Hodgson, D.; Hatton, A.L.; Warnett, R.; Rome, K.; Martin, D. The Effect of Textured Insoles on Gait in People with Multiple Sclerosis: An Exploratory Study: Effect of Textured Insoles on Gait in MS. Physiother. Res. Int. J. Res. Clin. Phys. Ther. 2012, 17, 121–122. [Google Scholar] [CrossRef]
- Kelleher, K.J.; Spence, W.D.; Solomonidis, S.; Apatsidis, D. The effect of textured insoles on gait patterns of people with multiple sclerosis. Gait Posture 2010, 32, 67–71. [Google Scholar] [CrossRef] [PubMed]
- Nurse, M.A.; Hulliger, M.; Wakeling, J.M.; Nigg, B.M.; Stefanyshyn, D.J. Changing the texture of footwear can alter gait patterns. J. Electromyogr. Kinesiol. 2005, 15, 496–506. [Google Scholar] [CrossRef] [PubMed]
- Ritchie, C.; Paterson, K.; Bryant, A.L.; Bartold, S.; Clark, R.A. The effects of enhanced plantar sensory feedback and foot orthoses on midfoot kinematics and lower leg neuromuscular activation. Gait Posture 2011, 33, 576–581. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.; Nigg, B.M.; Hulliger, M.; de Koning, J. Influence of sensory input on plantar pressure distribution. Clin. Biomech. 1995, 10, 271–274. [Google Scholar] [CrossRef] [PubMed]
- Casalena, J.A.; Ovaert, T.C.; Cavanagh, P.R.; Streit, D.A. The Penn State safety floor: Part I—Design parameters associated with walking deflections. J. Biomech. Eng. 1998, 120, 518–526. [Google Scholar] [CrossRef]
- Adrian, M.; Deustch, H.; Riccio, G.E. Walking Patterns and Falling in the Elderly; Department of Kinesiology, University of Illinois at Urbana-Champaign: Urbana, IL, USA, 1990. [Google Scholar]
- Glaser, R.M.; Sawka, M.N.; Wilde, S.W.; Woodrow, B.K.; Suryaprasad, A.G. Energy cost and cardiopulmonary responses for wheelchair locomotion and walking on tile and on carpet. Paraplegia 1981, 19, 220–226. [Google Scholar] [CrossRef]
- Knoefel, F.D.; Mousseau, M.; Berry, M. Pilot study to assess mobility safety on a dual-stiffness floor. Can. J. Geriatr. 2008, 11, 110–112. [Google Scholar]
- Okan, J. Development of a Fall-Injury Reducing Flooring System in Geriatric Care with Focus on Improving the Models Used in the Biomechanical Simulations and Evaluating the First Test Area. Master‘s Thesis, KTH Royal Institute of Technology, Stockholm, Sweden, 2015. [Google Scholar]
- Shimura, Y.; Okada, H.; Sakai, T.; Hayashi, Y.; Ohkawara, K.; Numao, S.; Katayama, Y.; Tanaka, K. Gait characteristics during walking on known tripping floor surfaces in older Japanese stroke patients. J. Aging Phys. Act. 2008, 16, S46–S47. [Google Scholar]
- Laing, A.C.; Robinovitch, S.N. Low stiffness floors can attenuate fall-related femoral impact forces by up to 50% without substantially impairing balance in older women. Accid. Anal. Prev. 2009, 41, 642–650. [Google Scholar] [CrossRef]
- Finlay, O.; Beringer, T. Effects of floor coverings on measurement of gait and plantar pressure. Physiotherapy 2007, 93, 144–150. [Google Scholar] [CrossRef]
- Heijnen, M.; Rietdyk, S. Failure to clear stationary, visible obstacles is affected by surface characteristics. In Proceedings of the 22nd International Society of Posture and Gait Research World Congress, Vancouver, BC, Canada, 29 June–3 July 2014. [Google Scholar]
- Soangra, R.; Jones, B.; Lockhart, T.E. Effects of Anti-Fatigue Flooring on Gait Parameters; SAGE Publications: Los Angeles, CA, USA, 2010; Volume 54, pp. 2019–2022. [Google Scholar]
- Willmott, M. The effect of a vinyl floor surface and a carpeted floor surface upon walking in elderly hospital in-patients. Age Ageing 1986, 15, 119–120. [Google Scholar] [CrossRef]
- Hernandez, M.E.; Ashton-Miller, J. Effect of surface compliance on stepping responses to trunk perturbations. In Proceedings of the 31st Annual Conference of the American Society of Biomechanics, Palo Alto, CA, USA, 22–25 August 2007. [Google Scholar]
- Stephens, J.M.; Goldie, P.A. Walking speed on parquetry and carpet after stroke: Effect of surface and retest reliability. Clin. Rehabil. 1999, 13, 171–181. [Google Scholar] [CrossRef]
- Hanger, H.C.; Hurley, K.; Hurring, S.; White, A. Low Impact flooring—Is it practical in a hospital? In Proceedings of the 6th Biennial Australia and New Zealand Falls Prevention Conference, Sydney, Australia, 16–18 November 2014; p. 66. [Google Scholar]
- Jahn, K.; Zwergal, A.; Schniepp, R. Gait Disturbances in Old Age Classification, Diagnosis, and Treatment From a Neurological Perspective. Dtsch. Arztebl. Int. 2010, 107, 306-U39. [Google Scholar] [PubMed]
- Menz, H.B.; Lord, S.R.; Fitzpatrick, R.C. Age-related differences in walking stability. Age Ageing 2003, 32, 137–142. [Google Scholar] [CrossRef]
- Callisaya, M.L.; Blizzard, L.; McGinley, J.L.; Srikanth, V.K. Risk of falls in older people during fast-walking—The TASCOG study. Gait Posture 2012, 36, 510–515. [Google Scholar] [CrossRef] [PubMed]
- Reelick, M.F.; van Iersel, M.B.; Kessels, R.P.C.; Rikkert, M. The influence of fear of falling on gait and balance in older people. Age Ageing 2009, 38, 435–440. [Google Scholar] [CrossRef] [PubMed]
- Startzell, J.K.; Owens, D.A.; Mulfinger, L.M.; Cavanagh, P.R. Stair Negotiation in Older People: A Review. J. Am. Geriatr. Soc. 2000, 48, 567–580. [Google Scholar] [CrossRef] [PubMed]
- Overstall, P.W.; Exton-Smith, A.N.; Imms, F.J.; Johnson, A.L. Falls in the elderly related to postural imbalance. Br. Med. J. 1977, 1, 261–264. [Google Scholar] [CrossRef] [PubMed]
- Brach, J.S.; Berthold, R.; Craik, R.; VanSwearingen, J.M.; Newman, A.B. Gait variability in community-dwelling older adults. J. Am. Geriatr. Soc. 2001, 49, 1646–1650. [Google Scholar] [CrossRef] [PubMed]
- Marigold, D.S.; Patla, A.E. Gaze fixation patterns for negotiating complex ground terrain. Neuroscience 2006, 144, 302–313. [Google Scholar] [CrossRef] [PubMed]
- Patla, A.E. Strategies for dynamic stability during adaptive human locomotion. IEEE Eng. Med. Biol. Mag. 2003, 22, 48–52. [Google Scholar] [CrossRef]
- Hijmans, J.M.; Geertzen, J.H.B.; Zijlstra, W.; Hof, A.L.; Postema, K. Effects of vibrating insoles on standing balance in diabetic neuropathy. J. Rehabil. Res. Dev. 2008, 45, 1441–1449. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, R.A. Frequent Augmented Feedback Can Degrade Learning: Evidence and Interpretations; Springer: Dordrecht, The Netherlands, 1991; pp. 59–75. [Google Scholar]
- Winstein, C.J.; Pohl, P.S.; Lewthwaite, R. Effects of Physical Guidance and Knowledge of Results on Motor Learning: Support for the Guidance Hypothesis. Res. Q. Exerc. Sport. 1994, 65, 316–323. [Google Scholar] [CrossRef] [PubMed]
- Young, W.R.; Rodger, M.W.M.; Craig, C.M. Auditory observation of stepping actions can cue both spatial and temporal components of gait in Parkinson׳s disease patients. Neuropsychologia 2014, 57, 140–153. [Google Scholar] [CrossRef] [PubMed]
- Dotov, D.G.; Bayard, S.; Cock, V.C.d.; Geny, C.; Driss, V.; Garrigue, G.; Bardy, B.; Bella, S.D. Biologically-variable rhythmic auditory cues are superior to isochronous cues in fostering natural gait variability in Parkinson ‘s disease. Gait Posture 2016, 51, 64–69. [Google Scholar] [CrossRef] [PubMed]
- Gaver, W.W. How Do We Hear in the World? Explorations in Ecological Acoustics. Ecol. Psychol. 1993, 5, 285–313. [Google Scholar] [CrossRef]
- Young, W.; Rodger, M.; Craig, C.M. Perceiving and Reenacting Spatiotemporal Characteristics of Walking Sounds. J. Exp. Psychol. Hum. Percept Perform 2013, 39, 464–476. [Google Scholar] [CrossRef]
- Maculewicz, J.; Erkut, C.; Serafin, S. An investigation on the impact of auditory and haptic feedback on rhythmic walking interactions. Int. J. Hum.-Comput. Stud. 2016, 85, 40–46. [Google Scholar] [CrossRef]
- Robinovitch, S.N.; Feldman, F.; Yang, Y.J.; Schonnop, R.; Leung, P.M.; Sarraf, T.; Sims-Gould, J.; Loughin, M. Video capture of the circumstances of falls in elderly people residing in long-term care: An observational study. Lancet 2013, 381, 47–54. [Google Scholar] [CrossRef]
- Allet, L.; Armand, S.; de Bie, R.A.; Pataky, Z.; Aminian, K.; Herrmann, F.R.; de Bruin, E.D. Gait alterations of diabetic patients while walking on different surfaces. Gait Posture 2008, 29, 488–493. [Google Scholar] [CrossRef] [PubMed]
- Medell, J.L.; Alexander, N.B. A clinical measure of maximal and rapid stepping in older women. J. Gerontol. A Biol. Sci. Med. Sci. 2000, 55, M429–M433. [Google Scholar] [CrossRef] [PubMed]
- Woollacott, M.H.; Tang, P.-F. Balance Control During Walking in the Older Adult: Research and Its Implications. Phys. Ther. 1997, 77, 646–660. [Google Scholar] [CrossRef] [PubMed]
- Costa, M.; Priplata, A.A.; Lipsitz, L.A.; Wu, Z.; Huang, N.E.; Goldberger, A.L.; Peng, C.K. Noise and poise: Enhancement of postural complexity in the elderly with a stochastic-resonance–based therapy. Europhys. Lett. 2007, 77, 68008. [Google Scholar] [CrossRef]
- Tinetti, M.E.; Baker, D.I.; McAvay, G.; Claus, E.B.; Garrett, P.; Gottschalk, M.; Koch, M.L.; Trainor, K.; Horwitz, R.I. A Multifactorial Intervention to Reduce the Risk of Falling among Elderly People Living in the Community. N. Engl. J. Med. 1994, 331, 821–827. [Google Scholar] [CrossRef] [PubMed]
- Cromwell, R.L.; Newton, R.A. Relationship between Balance and Gait Stability in Healthy Older Adults. J. Aging Phys. Act. 2004, 12, 90–100. [Google Scholar] [CrossRef] [PubMed]
- Cromwell, R.L.; Newton, R.A.; Forrest, G. Influence of vision on head stabilization strategies in older adults during walking. J. Gerontol. A Biol. Sci. Med. Sci. 2002, 57, M442–M448. [Google Scholar] [CrossRef] [PubMed]
- Giladi, N.; Herman, T.; Reider-Groswasser, I.I.; Gurevich, T.; Hausdorff, J. Clinical characteristics of elderly patients with a cautious gait of unknown origin. J. Neurol. 2005, 252, 300–306. [Google Scholar] [CrossRef] [PubMed]
- Young, W.R.; Mark Williams, A. How fear of falling can increase fall-risk in older adults: Applying psychological theory to practical observations. Gait Posture 2014, 41, 7–12. [Google Scholar] [CrossRef]
- van Emmerik, R.E.A.; van Wegen, E.E.H. On the functional aspects of variability in postural control. Exerc. Sport Sci. Rev. 2002, 30, 177–183. [Google Scholar] [CrossRef] [PubMed]
- Lu, T.-W.; Chen, H.-L.; Chen, S.-C. Comparisons of the lower limb kinematics between young and older adults when crossing obstacles of different heights. Gait Posture 2006, 23, 471–479. [Google Scholar] [CrossRef] [PubMed]
- Moran, M.; Van Cauwenberg, J.; Hercky-Linnewiel, R.; Cerin, E.; Deforche, B.; Plaut, P. Understanding the relationships between the physical environment and physical activity in older adults: A systematic review of qualitative studies. Int. J. Behav. Nutr. Phys. Act 2014, 11, 79. [Google Scholar] [CrossRef]
- Van Cauwenberg, J.; Nathan, A.; Barnett, A.; Barnett, D.W.; Cerin, E. Council on E. Physical Activity—Older Adults Working, G., Relationships Between Neighbourhood Physical Environmental Attributes and Older Adults’ Leisure-Time Physical Activity: A Systematic Review and Meta-Analysis. Sport. Med. 2018, 48, 1635–1660. [Google Scholar] [CrossRef]
- Barnett, D.W.; Barnett, A.; Nathan, A.; Van Cauwenberg, J.; Cerin, E. Built environmental correlates of older adults’ total physical activity and walking: A systematic review and meta-analysis. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 103. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, P.M.; Inglis, J.T. Distribution and behaviour of glabrous cutaneous receptors in the human foot sole. J. Physiol. 2002, 538, 995–1002. [Google Scholar] [CrossRef]
- Maki, B.E.; Cheng, K.C.C.; Mansfield, A.; Scovil, C.Y.; Perry, S.D.; Peters, A.L.; McKay, S.; Lee, T.; Marquis, A.; Corbeil, P.; et al. Preventing falls in older adults: New interventions to promote more effective change-in-support balance reactions. J. Electromyogr. Kinesiol. 2007, 18, 243–254. [Google Scholar] [CrossRef]
- Watanabe, I.; Okubo, J. The role of the plantar mechanoreceptor in equilibrium control. Ann. NY Acad. Sci. 1981, 374, 855–864. [Google Scholar] [CrossRef] [PubMed]
- Qiu, F.; Cole, M.H.; Davids, K.W.; Hennig, E.M.; Silburn, P.A.; Netscher, H.; Kerr, G.K. Enhanced somatosensory information decreases postural sway in older people. Gait Posture 2012, 35, 630–635. [Google Scholar] [CrossRef] [PubMed]
- Hatton, A.L.; Dixon, J.; Rome, K.; Martin, D. Standing on textured surfaces: Effects on standing balance in healthy older adults. Age Ageing 2011, 40, 363–368. [Google Scholar] [CrossRef] [PubMed]
- Waddington, G.; Adams, R. Football boot insoles and sensitivity to extent of ankle inversion movement. Br. J. Sport. Med. 2003, 37, 170–174. [Google Scholar] [CrossRef] [PubMed]
- Maki, B.E.; Perry, S.D.; Norrie, R.G.; McIlroy, W.E. Effect of Facilitation of Sensation From Plantar Foot-Surface Boundaries on Postural Stabilization in Young and Older Adults. J. Gerontol. Ser. A Biomed. Sci. Med. Sci. 1999, 54, M281–M287. [Google Scholar] [CrossRef] [PubMed]


| Parameter | Description | |
|---|---|---|
| Inclusion | Exclusion | |
| Population 1 | Contains at least some subgroups of study subjects who are older people, non-institutional self-sufficient citizens, older people without definite physical illness with no reported disease, mean age > 60 years, or authors claiming that the study subjects are older people. | Older people with significant physical health problems, children, adolescents, young adults, institutionalized/hospitalized. |
| Intervention | Short-term interventions for walking in the environment, characteristics of the built environment: physical environment, visual environment, auditory environment, gait barriers, accessibility, sidewalk barriers, balance barriers, etc. | Long-term training of walking, intervention with walking aids, exercise, drug intervention, walking without environmental intervention. |
| Comparison | Walking state in natural state (gait and physiological indicators) of older people, baseline physiological state without other intervention in natural state of older people. | Comparison with young people, compare with the gait indexes of older people with various diseases. |
| Outcome | The influence of human settlements’ pedestrian environment on gait and physiological characteristics of older people. | Studies investigating training, exercise, therapy, and drugs to predict disease risk. |
| Study design | Systematic/narrative review and/or meta-analysis design. | Narrative review without systematic review |
| Stairs or Indoor and Outdoor Steps | Obstacle | Uneven Surface and Irregular Surface | Turning around a Corner | Mechanical Perturbation during Gait | Vibration Interventions | Rhythmic Auditory Cues | Non-Modulated Rhythmic Auditory Cues | Textured Materials | Flooring Type | ||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Gait parameters related to gait prudence | Stride length | −[41] | −[41,45] | −[44] | /[10] | /[40] | +[39] | +[39] | /[46] | ||
| Step width | −[44] | /[10] | |||||||||
| Single support time | +[41] | −[10] | |||||||||
| Gait velocity | −[42] | −[41,45] | −[44] | −[41] | +[40] | +[39] | +[39] | /[43] | /[46] | ||
| Cadence | −[44] | +[10] | +[40] | +[39] | +[39] | ||||||
| Saccade/step interactions time | +[41] | ||||||||||
| Saccade/step latency | +[41] | ||||||||||
| Gait parameters related to gait stability | Centre of mass sway | −[10] | |||||||||
| Displacement of pressure center | −[37] | +[40] | |||||||||
| Coefficient of variability stride time | −[39] | ||||||||||
| Coefficient of variability stride length | −[39] | ||||||||||
| Postural sway | −[40] | /[38] | |||||||||
| Gait variability | +[44] | /[40] | |||||||||
| Postural stability | +[40] | ||||||||||
| Dynamic stability | +[10] | ||||||||||
| Dynamic balance | +[40] | /[43] | /[38] | ||||||||
| Margin of stability | +[10] | ||||||||||
| Parameters related to attitude expression and control | Vertical hip power at toe-off | −[45] | |||||||||
| The height of the crossing limb | −[45] | ||||||||||
| Muscle activation | +[45] | +[10] | |||||||||
| Measure maximum range of motion | −[45] | ||||||||||
| Joint angle range of motion | /[10] | ||||||||||
| Hip, knee, and ankle range of motion | /[45] | ||||||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Xuan, C.; Zhang, B.; Jia, X. The Effect of Human Settlement Pedestrian Environment on Gait of Older People: An Umbrella Review. Int. J. Environ. Res. Public Health 2023, 20, 1567. https://doi.org/10.3390/ijerph20021567
Xuan C, Zhang B, Jia X. The Effect of Human Settlement Pedestrian Environment on Gait of Older People: An Umbrella Review. International Journal of Environmental Research and Public Health. 2023; 20(2):1567. https://doi.org/10.3390/ijerph20021567
Chicago/Turabian StyleXuan, Changzheng, Bo Zhang, and Xiaohu Jia. 2023. "The Effect of Human Settlement Pedestrian Environment on Gait of Older People: An Umbrella Review" International Journal of Environmental Research and Public Health 20, no. 2: 1567. https://doi.org/10.3390/ijerph20021567
APA StyleXuan, C., Zhang, B., & Jia, X. (2023). The Effect of Human Settlement Pedestrian Environment on Gait of Older People: An Umbrella Review. International Journal of Environmental Research and Public Health, 20(2), 1567. https://doi.org/10.3390/ijerph20021567








