“I’ll leave that to the case managers.” Healthcare Service Providers‘ Perceptions of Organizational Readiness for Change in a Randomized Controlled Trial—A Qualitative Analysis Exploring Implementation Success
Abstract
1. Introduction
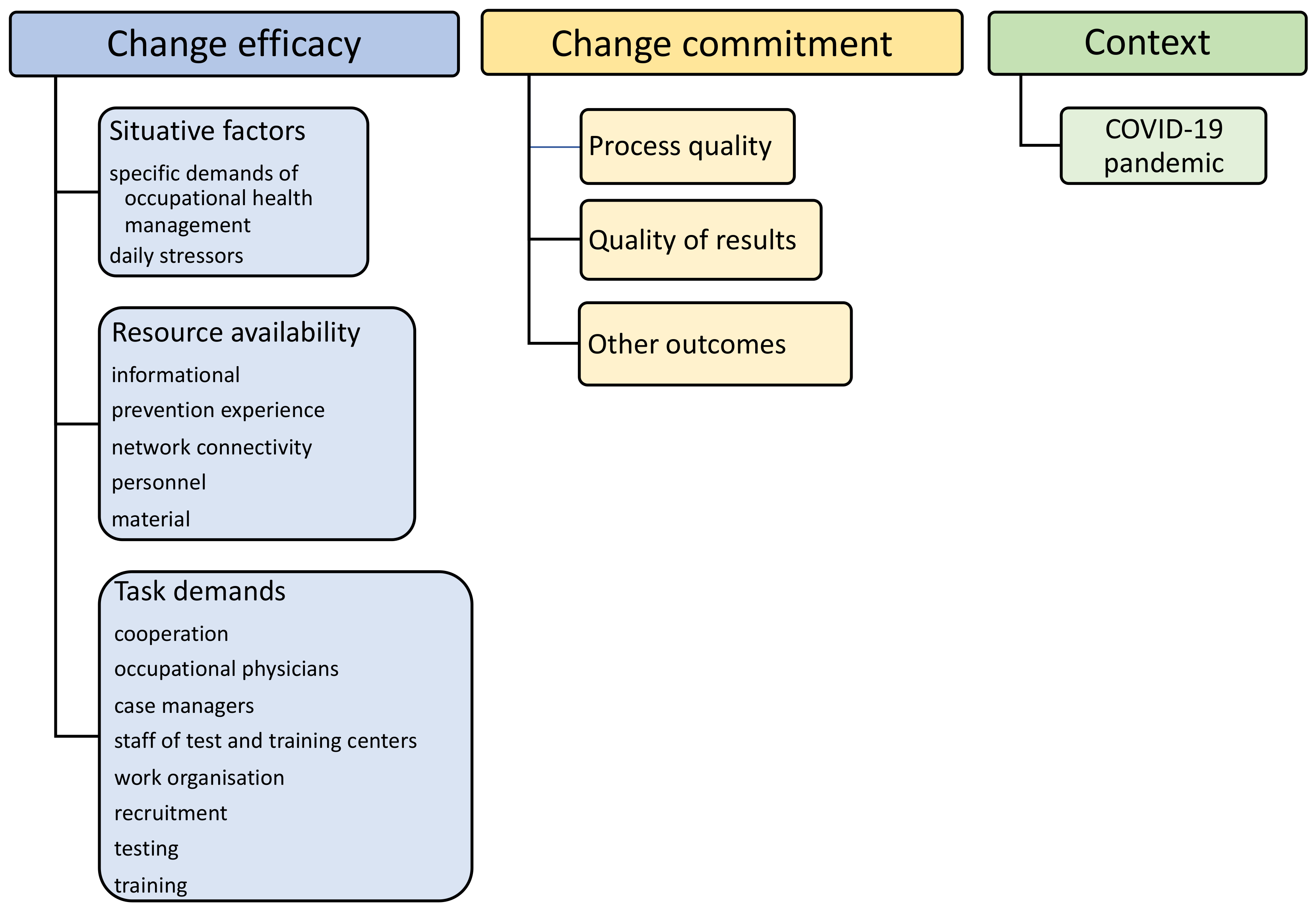
1.1. Organizational Readiness for Change
1.2. Creating New Networks
2. Materials and Methods
2.1. Accessing the Sample
2.2. Setting Procedure and Data Collection
2.3. Data Analysis
3. Results
3.1. Change Efficacy
3.1.1. Situative Factors
“So, it’s like, I’m very, very overwhelmed with administrative tasks at the moment and my... number of patient contacts I have is very poor. (…) Well, the situation for my colleagues is a bit different. They have very few administrative tasks, but very many patient contacts.”(BA5 32)
“Well, I see a number on the tablet that says ‘massage’. I finish that quickly and hand over the tablet and patient afterwards. Not very personal...”(MA6 16)
“Because there’s no time for more. Motivation maybe…, but no time indeed.”(BA5 64)
“There’s definitely no time to explain the study arms. In fact, I do not want to go into detail. I’ll leave that to the case managers.”(BA2 68)
3.1.2. Resource Availability
“Well, I mean, there are a lot of interfaces, right? Well, there are interfaces with the human resources department, of course, there are interfaces with our health studios here, there are interfaces with the psychologists we have in-house, there are interfaces with the insurances. So, sure, it’s a network.”(BA5 44)
“Exactly, that’s documented. We use digital solutions, but also old-school paper. The training follows standardization. Therefore, each trainer knows exactly what exercise at what device with what arrangements. If colleague A has designed the plan, colleague B can supervise the trainee without any problems. (…) The same is true for the general diagnostics and test. That makes collaboration easy.”(MA2 42)
“There were critical times at some point when people said: Now it’s already very crowded here and the filing and work is overflowing and then I have to do another test. But basically, it’s such a personal feeling. You can never avoid that. But in terms of the time required, as we have also discussed, over the three years, I think it was almost, … So you can say that it was very bearable.”(MA3 2102)
3.1.3. Task Demands
“We’re a rehab center, so it’s on prescription. It’s not a gym, it’s a real rehabilitation center via medical prescriptions and approvals, applications for rehabilitation, which are then carried out at our center. We have doctors in the center, we have psychologists, therapists, physiotherapists, masseurs. What else do we have? Nutritionists. So… the complete program of medical primary care providers… in principle.”(MA3 20)
“We know our person in charge that we can contact, if we have any questions. The collaboration is smooth.”(MA5 74)
“Let’s say it’s contacts via contacts. [...] So that means that if there are any sporting activities that can be offered, whether they are courses, whether they are lectures, etc., we are a bit in the same boat with the insurance company. That means we have larger companies around here [...]. At some point, inquiries were made as to whether we could offer any fitness courses from our premises, and then the talks came about bit by bit. That is, either it was the companies’ own initiative, or we got involved in the companies via the insurance company, which, let’s say, also got involved.”(MA7 28)
3.2. Change Commitment
3.2.1. Process Quality
“It is so often lost in the everyday life. No possibility to think about the study.”(BA5 72)
“We had a very optimistic start, because that’s a nice project. (…) But well, our employees are the kind of people that say ‘someone else should fix that’—even in dealing with their own diseases.”(BA1 90)
“It’s the good work of the case manager! She really cares for their customers and leads them through the whole process—that’s a huge plus!”(MA4 96)
“See, if there’s finally someone willing to participate, and then he only receives a … let’s say it offhand: a thera-band—he won’t like that. Enthusiasms looks different. I know that randomization is necessary for the quality of the study, but it’s not very helpful for the atmosphere.”(BA9 68)
3.2.2. Quality of Results
“We saw reliable results, also from the testing, and patients that the positive effects were highly motivated and diligent with the exercises. They even had fun, I think, it was a personal success for them.”(MA1 54)
“This was of course very positive for the members or for the people who took part in the study, they were of course very strongly motivated by it and also had the corresponding success after this study. So you could clearly see that they were also improving from time to time.”(MA5 48)
“But for the project itself, I really wouldn’t know. So, we have here, yeah, like I said, we’re out of the one control by now because it was just pointless. We didn’t have anything... was a lot of effort and didn’t come out of it.”(BA1 80)
3.2.3. Other Outcomes
3.3. Context
COVID-19 Pandemic
“We closed the center for some time. Some of the study participants could not train for this period and it was hard for them to catch up with the training afterwards.”(MA2 48)
“I would say that it still has a bit of an effect today that there are still people who have not been there since the reopening. They have simply said that it is too much for them with masks and here and there. So you can still see that, but the majority, I would say, of those who were always there, who also liked to come, they are also there again now. So in the meantime, we are back in the spheres where we were before.”(MA7 92)
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Trial Registration
Abbreviations
| BA | interview with occupational physician |
| ETTC(s) | employees of test and training centers |
| MA | interview with employee of test and training centers |
| MSD | musculoskeletal disorder(s) |
| OP(s) | occupational physician(s) |
| ORC | organizational readiness for change |
| ORIC | organizational readiness for implementation change |
| RCT | randomized controlled trial |
| TCU-ORC-D | Texas Christian University—organizational readiness for change—Director version |
References
- Bazzoli, G.J.; Dynan, L.; Burns, L.R.; Yap, C. Two decades of organizational change in health care: What have we learned? Med. Care Res. Rev. 2004, 61, 247–331. [Google Scholar] [CrossRef] [PubMed]
- Grol, R.; Grimshaw, J. From best evidence to best practice: Effective implementation of change in patients’ care. Lancet 2003, 362, 1225–1230. [Google Scholar] [CrossRef]
- Weiner, B.J. A theory of organizational readiness for change. Implement. Sci. 2009, 4, 67. [Google Scholar] [CrossRef] [PubMed]
- Holt, D.T.; Helfrich, C.D.; Hall, C.G.; Weiner, B.J. Are you ready? How health professionals can comprehensively conceptualize readiness for change. J. Gen. Intern. Med. 2010, 25 (Suppl. 1), 50–55. [Google Scholar] [CrossRef]
- Attieh, R.; Gagnon, M.P.; Estabrooks, C.A.; Legare, F.; Ouimet, M.; Roch, G.; Ghandour, E.K.; Grimshaw, J. Organizational readiness for knowledge translation in chronic care: A review of theoretical components. Implement. Sci. 2013, 8, 138. [Google Scholar] [CrossRef]
- Willis, C.D.; Saul, J.; Bevan, H.; Scheirer, M.A.; Best, A.; Greenhalgh, T.; Mannion, R.; Cornelissen, E.; Howland, D.; Jenkins, E.; et al. Sustaining organizational culture change in health systems. J. Health Organ. Manag. 2016, 30, 2–30. [Google Scholar] [CrossRef]
- Montague, T.J.; Gogovor, A.; Krelenbaum, M. Time for chronic disease care and management. Can. J. Cardiol. 2007, 23, 971–975. [Google Scholar] [CrossRef][Green Version]
- Wensing, M.; Wollersheim, H.; Grol, R. Organizational interventions to implement improvements in patient care: A structured review of reviews. Implement. Sci. 2006, 1, 2. [Google Scholar] [CrossRef]
- Kent, T.; Johnson, J.A.; Graber, D.R. Leadership in the formation of new health care environments. Health Care Superv. 1996, 15, 27–34. [Google Scholar]
- Choi, K.A.; Lindert, L.; Schlomann, L.; Samel, C.; Hellmich, M.; Pfaff, H. A Cross-Provider Healthcare Management Program for Musculoskeletal Disorders: Results of a Randomized Controlled Trial in 22 German Companies. Int. J. Environ. Res. Public Health 2021, 18, 11844. [Google Scholar] [CrossRef]
- Lehmann, B.A.; Lindert, L.; Ohlmeier, S.; Schlomann, L.; Pfaff, H.; Choi, K.E. “And Then He Got into the Wrong Group”: A Qualitative Study Exploring the Effects of Randomization in Recruitment to a Randomized Controlled Trial. Int. J. Environ. Res. Public Health 2020, 17, 1886. [Google Scholar] [CrossRef] [PubMed]
- Schubin, K.; Schlomann, L.; Lindert, L.; Pfaff, H.; Choi, K.E. Occupational Physicians’ Perspectives on Determinants of Employee Participation in a Randomized Controlled Musculoskeletal Health Promotion Measure: A Qualitative Study. Int J. Environ. Res. Public Health 2020, 17, 7445. [Google Scholar] [CrossRef] [PubMed]
- Tong, A.; Sainsbury, P.; Craig, J. Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int. J. Qual. Health Care 2007, 19, 349–357. [Google Scholar] [CrossRef] [PubMed]
- Damschroder, L.J.; Aron, D.C.; Keith, R.E.; Kirsh, S.R.; Alexander, J.A.; Lowery, J.C. Fostering implementation of health services research findings into practice: A consolidated framework for advancing implementation science. Implement. Sci. 2009, 4, 50. [Google Scholar] [CrossRef]
- Frese, E.; Graumann, M.; Theuvse, L. Organisation, Organisationstheorien und Organisationsgestaltung. In Grundlagen der Organisation; Gabler Verlag Springer Fachmedien GmbH: Wiesbaden, Germany, 2012. [Google Scholar] [CrossRef]
- Gläser, J.L.G. Experteninterviews und Qualitative Inhaltsanalyse als Instrumente rekonstruierender Untersuchungen; VS Verlag: Wiesbaden, Germany, 2010. [Google Scholar]
- Geerligs, L.; Rankin, N.M.; Shepherd, H.L.; Butow, P. Hospital-based interventions: A systematic review of staff-reported barriers and facilitators to implementation processes. Implement. Sci. 2018, 13, 36. [Google Scholar] [CrossRef]
- Miake-Lye, I.M.; Delevan, D.M.; Ganz, D.A.; Mittman, B.S.; Finley, E.P. Unpacking organizational readiness for change: An updated systematic review and content analysis of assessments. BMC Health Serv. Res. 2020, 20, 106. [Google Scholar] [CrossRef]
- Rankin, N.M.; Butow, P.N.; Thein, T.; Robinson, T.; Shaw, J.M.; Price, M.A.; Clover, K.; Shaw, T.; Grimison, P. Everybody wants it done but nobody wants to do it: An exploration of the barrier and enablers of critical components towards creating a clinical pathway for anxiety and depression in cancer. BMC Health Serv. Res. 2015, 15, 28. [Google Scholar] [CrossRef]
- Geerligs, L.; Shepherd, H.L.; Butow, P.; Shaw, J.; Masya, L.; Cuddy, J.; Group, A.P.; Rankin, N.M. What factors influence organisational readiness for change? Implementation of the Australian clinical pathway for the screening, assessment and management of anxiety and depression in adult cancer patients (ADAPT CP). Support. Care Cancer 2021, 29, 3235–3244. [Google Scholar] [CrossRef]
- Pace, K.B.; Sakulkoo, S.; Hoffart, N.; Cobb, A.K. Barriers to successful implementation of a clinical pathway for CHF. J. Healthc Qual. 2002, 24, 32–38. [Google Scholar] [CrossRef]
- Austin, T.; Chreim, S.; Grudniewicz, A. Examining health care providers’ and middle-level managers’ readiness for change: A qualitative study. BMC Health Serv. Res. 2020, 20, 47. [Google Scholar] [CrossRef]
- McCormack, B.; Rycroft-Malone, J.; Decorby, K.; Hutchinson, A.M.; Bucknall, T.; Kent, B.; Schultz, A.; Snelgrove-Clarke, E.; Stetler, C.; Titler, M.; et al. A realist review of interventions and strategies to promote evidence-informed healthcare: A focus on change agency. Implement. Sci. 2013, 8, 107. [Google Scholar] [CrossRef] [PubMed]
- Arends, I.; Bultmann, U.; Shaw, W.S.; van Rhenen, W.; Roelen, C.; Nielsen, K.; van der Klink, J.J. How to engage occupational physicians in recruitment of research participants: A mixed-methods study of challenges and opportunities. J. Occup. Rehabil. 2014, 24, 68–78. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Braithwaite, J.; Churruca, K.; Ellis, L.A.; Long, J.; Clay-Williams, R.; Damen, N.; Herkes, J.; Pomare, C.; Ludlow, K. Complexity Science in Healthcare—Aspirations, Approaches, Applications and Accomplishments: A White Paper; Australian Institute of Health Innovations, Marquarie University: Sydney, Australia, 2017. [Google Scholar]
- Boaz, A.; Hanney, S.; Borst, R.; O’Shea, A.; Kok, M. How to engage stakeholders in research: Design principles to support improvement. Health Res. Policy Syst. 2018, 16, 60. [Google Scholar] [CrossRef] [PubMed]
- de Wit, M.; Kleijnen, M.; Lissenberg-Witte, B.; van Uden-Kraan, C.; Millet, K.; Frambach, R.; Verdonck-de Leeuw, I. Understanding Drivers of Resistance Toward Implementation of Web-Based Self-Management Tools in Routine Cancer Care Among Oncology Nurses: Cross-Sectional Survey Study. J. Med. Internet Res. 2019, 21, e14985. [Google Scholar] [CrossRef] [PubMed]
- Liverani, M.; Hawkins, B.; Parkhurst, J.O. Political and institutional influences on the use of evidence in public health policy. A systematic review. PLoS ONE 2013, 8, e77404. [Google Scholar] [CrossRef] [PubMed]
- Shea, C.M.; Jacobs, S.R.; Esserman, D.A.; Bruce, K.; Weiner, B.J. Organizational readiness for implementing change: A psychometric assessment of a new measure. Implement. Sci. 2014, 9, 7. [Google Scholar] [CrossRef]
- Gagnon, M.P.; Attieh, R.; Ghandour, E.K.; Legare, F.; Ouimet, M.; Estabrooks, C.A.; Grimshaw, J. A systematic review of instruments to assess organizational readiness for knowledge translation in health care. PLoS ONE 2014, 9, e114338. [Google Scholar] [CrossRef]
| Questions | Answers | |
|---|---|---|
| 1st round OPs | How old are you? | min: 41 years, max: 62 years, mean: 53 years |
| What is your gender? | female: 7, male: 3 | |
| Do you work in full or parttime? | full time: 7, part time: 2, other: 1 | |
| For how many years have you been working as OP? | min: 4 years, max: 40 years, mean: 17 years | |
| For how many years have you been working for this company? | min: 4 years, max: 30 years, mean: 11 years | |
| Have you been involved in the study from its start? | yes: 8, no: 2 | |
| How many companies do you support? | min: 1, max: 44, mean: 10 | |
| Do you have experience with studies? | yes: 7, no: 3 | |
| How many hours per week do you work for the study? | min: <1, max: 3, mean: 1 | |
| Is there a substitute physician for you? | yes: 9, no: 1 | |
| 2nd round OPs | How old are you? | min: 40 years, max: 67 years, mean: 56 years |
| What is your gender? | female: 8, male: 5 | |
| Do you work in full or parttime? | full time: 8, part time: 2, other: 1, no comment: 2 | |
| For how many years have you been working as OP? | min: 5 years, max: 31 years, mean: 17 years | |
| For how many years have you been working for this company? | min: 1.5 years, max: 31 years, mean: 11 years | |
| Have you been involved in the study from its start? | yes: 10, no: 0, no comment: 2 | |
| How many companies do you support? | min: 1, max: 60, mean: 18 | |
| Do you have experience with studies? | yes: 7, no: 4, no comment: 2 | |
| How many hours per week do you work for the study? | min: <1, max: 2, mean: 1 | |
| Is there a substitute physician for you? | yes: 9, no: 2, no comment: 2 | |
| ETTCs | In the study, our center is… | exclusively test center: 3, exclusively training center: 4, both: 2 |
| If applicable, if which part of the center do you work? | test center only: 4, training center only: 4, both centers: 1 | |
| How many employees do work in your center? | min: 10 employees, max: 48 employees, mean: 28 employees | |
| How many of these are involved in the study? | min: 1 employee, max: 5 employees, mean: 3 | |
| How old are you? | min: 25 years, max: 53 years, mean: 41 years | |
| What is your gender? | female: 2, male: 7 | |
| What is your job description? | sports scientist/teacher, practice manager, trainer, physiotherapist | |
| Do you work in full or parttime? | full time: 9 | |
| Do you have a leadership role? | yes: 6, no: 3 | |
| For how many years have you been working for the center? | min: 2.5 years, max: 25 years, mean: 12 years | |
| Have you been involved in the study from its start? | yes: 9, no: 0 | |
| How many companies do you support? | min: 1, max: 3, mean: 1 | |
| How many hours per week do you work for the study? | min: 0.5, max: 10, mean: 3 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Choi, K.-E.; Lindert, L.; Schlomann, L.; Pfaff, H. “I’ll leave that to the case managers.” Healthcare Service Providers‘ Perceptions of Organizational Readiness for Change in a Randomized Controlled Trial—A Qualitative Analysis Exploring Implementation Success. Int. J. Environ. Res. Public Health 2022, 19, 5782. https://doi.org/10.3390/ijerph19095782
Choi K-E, Lindert L, Schlomann L, Pfaff H. “I’ll leave that to the case managers.” Healthcare Service Providers‘ Perceptions of Organizational Readiness for Change in a Randomized Controlled Trial—A Qualitative Analysis Exploring Implementation Success. International Journal of Environmental Research and Public Health. 2022; 19(9):5782. https://doi.org/10.3390/ijerph19095782
Chicago/Turabian StyleChoi, Kyung-Eun (Anna), Lara Lindert, Lara Schlomann, and Holger Pfaff. 2022. "“I’ll leave that to the case managers.” Healthcare Service Providers‘ Perceptions of Organizational Readiness for Change in a Randomized Controlled Trial—A Qualitative Analysis Exploring Implementation Success" International Journal of Environmental Research and Public Health 19, no. 9: 5782. https://doi.org/10.3390/ijerph19095782
APA StyleChoi, K.-E., Lindert, L., Schlomann, L., & Pfaff, H. (2022). “I’ll leave that to the case managers.” Healthcare Service Providers‘ Perceptions of Organizational Readiness for Change in a Randomized Controlled Trial—A Qualitative Analysis Exploring Implementation Success. International Journal of Environmental Research and Public Health, 19(9), 5782. https://doi.org/10.3390/ijerph19095782



_Choi.png)




