Social Support Mediates the Relationship between Body Image Distress and Depressive Symptoms in Prostate Cancer Patients
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants and Procedures
2.2. Measures
2.2.1. Demographics and Clinical Characteristics
2.2.2. Body Image Distress
2.2.3. Depressive Symptoms
2.2.4. Social Support
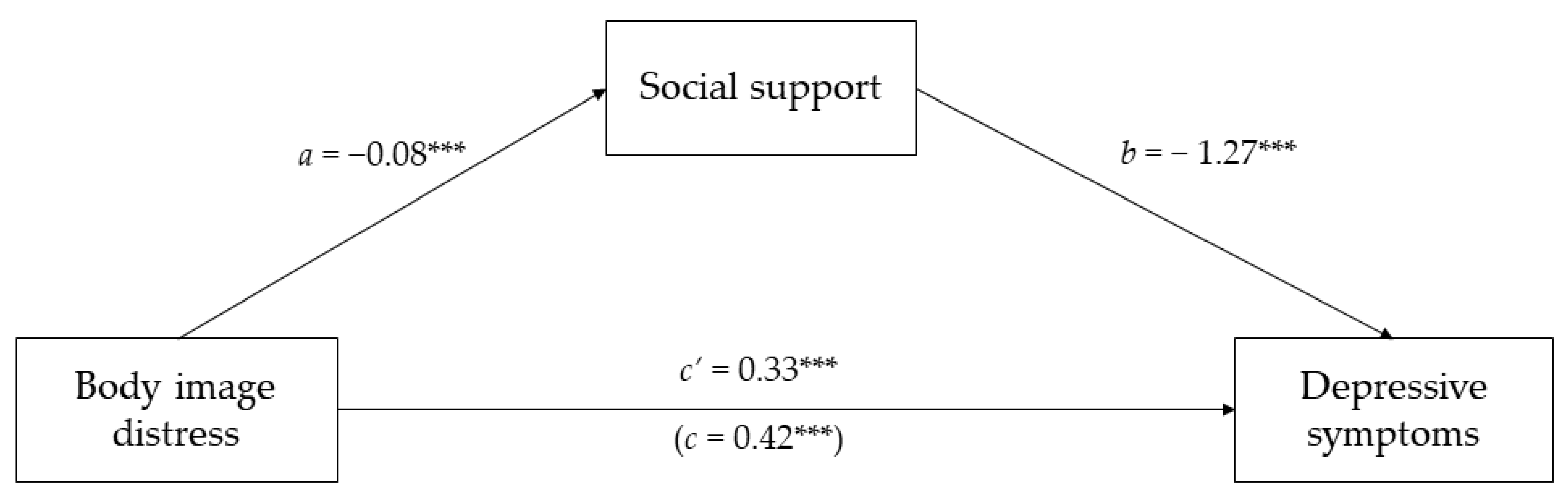
2.3. Statistical Analyses
3. Results
3.1. Participants’ Characteristics
3.2. Descriptive Statistics and Bivariate Correlations
3.3. Direct and Indirect Effects of Body Image Distress and Social Support on Depressive Symptoms
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer statistics, 2020. CA Cancer J. Clin. 2020, 70, 7–30. [Google Scholar] [CrossRef] [PubMed]
- Ilie, G.; Rutledge, R.; Sweeney, E. Post-Treatment Adverse Health Correlates among Prostate Cancer Survivors in a Sample of Men Residing in Atlantic Canada. Curr. Oncol. 2021, 28, 2812–2822. [Google Scholar] [CrossRef] [PubMed]
- Lin, P.H.; Liu, J.M.; Hsu, R.J.; Chuang, H.C.; Chang, S.W.; Pang, S.T.; Chang, Y.H.; Chuang, C.K.; Lin, S.K. Depression negatively impacts survival of patients with metastatic prostate cancer. Int. J. Environ. Res. Public Health 2018, 15, 2148. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brunckhorst, O.; Hashemi, S.; Martin, A.; George, G.; Van Hemelrijck, M.; Dasgupta, P.; Stewart, R.; Ahmed, K. Depression, anxiety, and suicidality in patients with prostate cancer: A systematic review and meta-analysis of observational studies. Prostate Cancer Prostatic Dis. 2021, 24, 281–289. [Google Scholar] [CrossRef] [PubMed]
- Grogan, S. Body Image: Understanding Body Dissatisfaction in Men, Women, and Children, 3rd ed.; Routledge: London, UK, 2021. [Google Scholar]
- Kadono, Y.; Machioka, K.; Nakashima, K.; Iijima, M.; Shigehara, K.; Nohara, T.; Narimoto, K.; Izumi, K.; Kitagawa, Y.; Konaka, H.; et al. Changes in penile length after radical prostatectomy: Investigation of the underlying anatomical mechanism. BJU Int. 2017, 120, 293–299. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bowie, J.; Brunckhorst, O.; Stewart, R.; Dasgupta, P.; Ahmed, K. Body image, self-esteem, and sense of masculinity in patients with prostate cancer: A qualitative meta-synthesis. J. Cancer Surviv. 2022, 16, 95–110. [Google Scholar] [CrossRef]
- Taylor-Ford, M.; Meyerowitz, B.E.; D’Orazio, L.M.; Christie, K.M.; Gross, M.E.; Agus, D.B. Body image predicts quality of life in men with prostate cancer. Psychooncology 2013, 22, 756–761. [Google Scholar] [CrossRef]
- Bullen, T.L.; Sharpe, L.; Lawsin, C.; Patel, D.C.; Clarke, S.; Bokey, L. Body image as a predictor of psychopathology in surgical patients with colorectal disease. J. Psychosom. Res. 2012, 73, 459–463. [Google Scholar] [CrossRef]
- Mainwaring, J.M.; Walker, L.M.; Robinson, J.W.; Wassersug, R.J.; Wibowo, E. The psychosocial consequences of prostate cancer treatments on body image, sexuality, and relationships. Front. Psychol. 2021, 12, 765315. [Google Scholar] [CrossRef]
- Saini, A.; Berruti, A.; Cracco, C.; Sguazzotti, E.; Porpiglia, F.; Russo, L.; Bertaglia, V.; Picci, R.L.; Negro, M.; Tosco, A.; et al. Psychological distress in men with prostate cancer receiving adjuvant androgen-deprivation therapy. Urol. Oncol. 2013, 31, 352–358. [Google Scholar] [CrossRef]
- Schwarzer, R.; Knoll, N.; Rieckmann, N. Social support. In Health Psychology; Kaptein, A., Weinman, J., Eds.; Blackwell Publishing: Hoboken, NJ, USA, 2004; pp. 158–181. [Google Scholar]
- Cohen, S. Psychosocial models of the role of social support in the etiology of physical disease. Health Psychol. 1988, 7, 269–297. [Google Scholar] [CrossRef]
- Cohen, S.; Underwood, L.G.; Gottlieb, B.H. Social Support Measurement and Intervention: A Guide for Health and Social Scientists; Oxford University Press: Oxford, UK, 2000. [Google Scholar]
- Helgeson, V.S. Social support and quality of life. Qual. Life Res. 2003, 12, 25–31. [Google Scholar] [CrossRef] [PubMed]
- Avalos, L.C.; Tylka, T.L. Exploring a model of intuitive eating with college women. J. Couns. Psychol. 2006, 53, 486–497. [Google Scholar] [CrossRef] [Green Version]
- Cohen, S.; Wills, T.A. Stress, social support, and the buffering hypothesis. Psychol. Bull. 1985, 98, 310–357. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S. Social relationships and health. Am. Psychol. 2004, 59, 676–684. [Google Scholar] [CrossRef] [PubMed]
- Pruneti, C.; Cosentino, C.; Merisio, C.; Berretta, R. Adapting to cancer with body, mind, and heart: Psychological, psychophysiological assessment and management in sample of ovarian cancer survivors. J. Clin. Exp. Oncol. 2020, 9, 1–6. [Google Scholar]
- Spatuzzi, R.; Vespa, A.; Lorenzi, P.; Miccinesi, G.; Ricciuti, M.; Cifarelli, W.; Susi, M.; Fabrizio, T.; Ferrari, M.G.; Ottaviani, M.; et al. Evaluation of social support, quality of life, and body image in women with breast cancer. Breast Care 2016, 11, 28–32. [Google Scholar] [CrossRef] [Green Version]
- Bennett, E.V.; Hurd, L.C.; Pritchard, E.M.; Colton, T.; Crocker, P. An examination of older men’s body image: How men 65 years and older perceive, experience, and cope with their aging bodies. Body Image 2020, 34, 27–37. [Google Scholar] [CrossRef]
- Chen, C.; Cao, J.; Wang, L.; Zhang, R.; Li, H.; Peng, J. Body image and its associated factors among Chinese head and neck cancer patients undergoing surgical treatment: A cross-sectional survey. Support Care Cancer 2020, 28, 1233–1239. [Google Scholar] [CrossRef]
- Tylka, T.L. Positive psychology perspectives on body image. In Body Image: A Handbook of Science, Practice, and Prevention, 2nd ed.; Cash, T.F., Smolak, L., Eds.; The Guilford Press: New York, NY, USA, 2011; pp. 56–64. [Google Scholar]
- Den Heijer, M.; Seynaeve, C.; Timman, R.; Duivenvoorden, H.J.; Vanheusden, K.; Tilanus-Linthorst, M.; Menke-Pluijmers, M.B.; Tibben, A. Body image and psychological distress after prophylactic mastectomy and breast reconstruction in genetically predisposed women: A prospective long-term follow-up study. Eur. J. Cancer 2012, 48, 1263–1268. [Google Scholar] [CrossRef]
- Huang, C.Y.; Chen, W.K.; Lu, C.Y.; Tsai, C.C.; Lai, H.L.; Lin, H.Y.; Guo, S.E.; Wu, L.M.; Chen, C.I. Mediating effects of social support and self-concept on depressive symptoms in adults with spinal cord injury. Spinal Cord 2015, 53, 413–416. [Google Scholar] [CrossRef] [PubMed]
- Tsai, W.; Lu, Q. Perceived social support mediates the longitudinal relations between ambivalence over emotional expression and quality of life among Chinese American breast cancer survivors. Int. J. Behav. Med. 2018, 25, 368–373. [Google Scholar] [CrossRef] [PubMed]
- Yang, C.; Xia, M.; Han, M.; Liang, Y. Social support and resilience as mediators between stress and life satisfaction among people with substance use disorder in China. Front. Psychiatry 2018, 9, 436. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Paterson, C.; Jones, M.; Rattray, J.; Lauder, W. Exploring the relationship between coping, social support and health-related quality of life for prostate cancer survivors: A review of the literature. Eur. J. Oncol. Nurs. 2013, 17, 750–759. [Google Scholar] [CrossRef]
- Geng, Z.; Ogbolu, Y.; Wang, J.; Hinds, P.S.; Qian, H.; Yuan, C. Gauging the effects of self-efficacy, social support, and coping style on self-management behaviors in Chinese cancer survivors. Cancer Nurs. 2018, 41, E1–E10. [Google Scholar] [CrossRef]
- Garner, M.J.; Mcgregor, B.A.; Murphy, K.M.; Koenig, A.L.; Dolan, E.D.; Albano, D. Optimism and depression: A new look at social support as a mediator among women at risk for breast cancer. Psychooncology 2015, 24, 1708–1713. [Google Scholar] [CrossRef]
- Dunkel Schetter, C. Psychological science on pregnancy: Stress processes, biopsychosocial models, and emerging research issues. Annu. Rev. Psychol. 2011, 62, 531–558. [Google Scholar] [CrossRef]
- Thoits, P.A. Mechanisms linking social ties and support to physical and mental health. J. Health Soc. Behav. 2011, 52, 145–161. [Google Scholar] [CrossRef] [Green Version]
- Ettridge, K.A.; Bowden, J.A.; Chambers, S.K.; Smith, D.P.; Murphy, M.; Evans, S.M.; Order, D.; Miller, C.L. “Prostate cancer is far more hidden…”: Perceptions of stigma, social isolation and help-seeking among men with prostate cancer. Eur. J. Cancer Care 2018, 27, e12790. [Google Scholar] [CrossRef]
- Zhao, X.; Sun, M.; Yang, Y. Effects of social support, hope and resilience on depressive symptoms within 18 months after diagnosis of prostate cancer. Health Qual. Life Outcomes 2021, 19, 15. [Google Scholar] [CrossRef]
- Pereira, M.G.; Ponte, M.; Ferreira, G.; Machado, J.C. Quality of life in patients with skin tumors: The mediator role of body image and social support. Psychooncology 2017, 26, 815–821. [Google Scholar] [CrossRef] [PubMed]
- Hsu, H.T.; Juan, C.H.; Chen, J.L.; Hsieh, H.F. Mediator roles of social support and hope in the relationship between body image distress and resilience in breast cancer patients undergoing treatment: A modeling analysis. Front. Psychol. 2021, 12, 695682. [Google Scholar] [CrossRef] [PubMed]
- Epstein, J.I.; Egevad, L.; Amin, M.B.; Delahunt, B.; Srigley, J.R.; Humphrey, P.A.; Grading Committee. The 2014 International Society of Urological Pathology (ISUP) Consensus Conference on Gleason Grading of Prostatic Carcinoma: Definition of grading patterns and proposal for a new grading system. Am. J. Surg. Pathol. 2016, 40, 244–252. [Google Scholar] [CrossRef]
- Hopwood, P.; Fletcher, I.; Lee, A.; Al Ghazal, S. A body image scale for use with cancer patients. Eur. J. Cancer 2001, 37, 189–197. [Google Scholar] [CrossRef]
- Langelier, D.M.; Cormie, P.; Bridel, W.; Grant, C.; Albinati, N.; Shank, J.; Daun, J.T.; Fung, T.S.; Davey, C.; Culos-Reed, S.N. Perceptions of masculinity and body image in men with prostate cancer: The role of exercise. Support Care Cancer 2018, 26, 3379–3388. [Google Scholar] [CrossRef] [PubMed]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B. Validation and utility of a self-report version of PRIME-MD: The PHQ primary care study. Primary care evaluation of mental disorders. Patient Health Questionnaire. JAMA 1999, 282, 1737–1744. [Google Scholar] [CrossRef] [Green Version]
- Zimet, G.D.; Dahlem, N.W.; Zimet, S.G.; Farley, G.K. Psychometric characteristics of the Multidimensional Scale of Perceived Social Support. J. Pers. Assess 1988, 52, 30–41. [Google Scholar] [CrossRef] [Green Version]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach, 1st ed.; Guilford Press: New York, NY, USA, 2013. [Google Scholar]
- Begovic-Juhant, A.; Chmielewski, A.; Iwuagwu, S.; Chapman, L.A. Impact of body image on depression and quality of life among women with breast cancer. J. Psychosoc. Oncol. 2012, 30, 446–460. [Google Scholar] [CrossRef]
- Esser, P.; Mehnert, A.; Johansen, C.; Hornemann, B.; Dietz, A.; Ernst, J. Body image mediates the effect of cancer-related stigmatization on depression: A new target for intervention. Psychooncology 2018, 27, 193–198. [Google Scholar] [CrossRef]
- Przezdziecki, A.; Sherman, K.A.; Baillie, A.; Taylor, A.; Foley, E.; Stalgis-Bilinski, K. My changed body: Breast cancer, body image, distress and self-compassion. Psychooncology 2013, 22, 1872–1879. [Google Scholar] [CrossRef]
- Sharpe, L.; Patel, D.; Clarke, S. The relationship between body image disturbance and distress in colorectal cancer patients with and without stomas. J. Psychosom. Res. 2011, 70, 395–402. [Google Scholar] [CrossRef] [PubMed]
- de Moraes Lopes, M.H.; Higa, R.; Cordeiro, S.N.; Rodrigues Estape, N.A.; Levi D’ancona, C.A.; Turato, E.R. Life experiences of Brazilian men with urinary incontinence and erectile dysfunction following radical prostatectomy. J. Wound Ostomy. Cont. Nurs. 2012, 39, 90–94. [Google Scholar] [CrossRef] [PubMed]
- Craike, M.J.; Livingston, P.M.; Botti, M. An exploratory study of the factors that influence physical activity for prostate cancer survivors. Support Care Cancer 2011, 19, 1019–1028. [Google Scholar] [CrossRef]
- Klaeson, K.; Sandell, K.; Bertero, C.M. Sexuality in the context of prostate cancer narratives. Qual. Health Res. 2012, 22, 1184–1194. [Google Scholar] [CrossRef]
- Appleton, L.; Wyatt, D.; Perkins, E.; Parker, C.; Crane, J.; Jones, A.; Moorhead, L.; Brown, V.; Wall, C.; Pagett, M. The impact of prostate cancer on men’s everyday life. Eur. J. Cancer Care 2015, 24, 71–84. [Google Scholar] [CrossRef] [PubMed]
- Oliffe, J.; Thorne, S. Men, masculinities, and prostate cancer: Australian and Canadian patient perspectives of communication with male physicians. Qual. Health Res. 2007, 17, 149–161. [Google Scholar] [CrossRef] [PubMed]
- Coco, M.; Buscemi, A.; Guerrera, C.S.; Licitra, C.; Pennisi, E.; Vettor, V.; Rizzi, L.; Bovo, P.; Fecarotta, P.; Dell’Orco, S.; et al. Touch and communication in the institutionalized elderly. In Proceedings of the 10th IEEE International Conference on Cognitive Infocommunications (CogInfoCom), Naples, Italy, 23–25 October 2019; pp. 451–458. [Google Scholar]
- Dieperink, K.B.; Wagner, L.; Hansen, S.; Hansen, O. Embracing life after prostate cancer. A male perspective on treatment and rehabilitation. Eur. J. Cancer Care 2013, 22, 549–558. [Google Scholar] [CrossRef]
- Siedlecki, K.L.; Salthouse, T.A.; Oishi, S.; Jeswani, S. The relationship between social support and subjective well-being across age. Soc. Indic. Res. 2014, 117, 561–576. [Google Scholar] [CrossRef] [Green Version]
- Uchino, B.N.; Bowen, K.; Carlisle, M.; Birmingham, W. Psychological pathways linking social support to health outcomes: A visit with the ghost of research past, present and future. Soc. Sci. Med. 2013, 74, 949–957. [Google Scholar] [CrossRef] [Green Version]
- Kim, J.; Han, J.Y.; Shaw, B.; McTavish, F.; Gustafson, D. The roles of social support and coping strategies in predicting breast cancer patients’ emotional well-being: Testing mediation and moderation models. J. Health Psychol. 2010, 15, 543–552. [Google Scholar] [CrossRef] [Green Version]
- Li, M.Y.; Yang, Y.L.; Liu, L.; Wang, L. Effects of social support, hope and resilience on quality of life among Chinese bladder cancer patients: A cross-sectional study. Health Qual. Life Outcomes 2016, 14, 73. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, L.; Yang, Y.L.; Wang, Z.Y.; Wu, H.; Wang, Y.; Wang, L. Prevalence and positive correlates of posttraumatic stress disorder symptoms among Chinese patients with hematological malignancies: A cross-sectional study. PLoS ONE 2015, 10, e0145103. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhou, E.S.; Penedo, F.J.; Lewis, J.E.; Rasheed, M.; Traeger, L.; Lechner, S.; Soloway, M.; Kava, B.R.; Antoni, M.H. Perceived stress mediates the effects of social support on health-related quality of life among men treated for localized prostate cancer. J. Psychosom. Res. 2010, 69, 587–590. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Evans, R.; Mallet, P.; Bazillier, C.; Amiel, P. Friendship and cancer. Rev. Health Care 2015, 6, 53–65. [Google Scholar] [CrossRef] [Green Version]
- Cicero, V.; Lo Coco, G.; Gullo, S.; Lo Verso, G. The role of attachment dimensions and perceived social support in predicting adjustment to cancer. Psychooncology 2009, 18, 1045–1052. [Google Scholar] [CrossRef]
- Chapple, A.; Ziebland, S. Prostate cancer: Embodied experience and perceptions of masculinity. Sociol. Health Illn. 2002, 24, 820–841. [Google Scholar] [CrossRef]
- McAteer, G.; Gillanders, D. Investigating the role of psychological flexibility, masculine self-esteem and stoicism as predictors of psychological distress and quality of life in men living with prostate cancer. Eur. J. Cancer Care 2019, 28, e13097. [Google Scholar] [CrossRef]
- Scandurra, C.; Monaco, S.; Dolce, P.; Nothdurfter, U. Heteronormativity in Italy: Psychometric characteristics of the Italian version of the Heteronormative Attitudes and Beliefs Scale. Sex Res. Soc. Policy 2021, 18, 637–652. [Google Scholar] [CrossRef]
- Amodeo, A.L.; Esposito, C.; Bochicchio, V.; Valerio, P.; Vitelli, R.; Bacchini, D.; Scandurra, C. Parenting desire and minority stress in lesbians and gay men: A mediation framework. Int. J. Environ. Res. Public Health 2018, 15, 2318. [Google Scholar] [CrossRef] [Green Version]
- Scandurra, C.; Pennasilico, A.; Esposito, C.; Mezza, F.; Vitelli, R.; Bochicchio, V.; Maldonato, N.M.; Amodeo, A.L. Minority stress and mental health in Italian bisexual people. Soc. Sci. 2020, 9, 46. [Google Scholar] [CrossRef] [Green Version]
- Scandurra, C.; Bochicchio, V.; Dolce, P.; Caravà, C.; Vitelli, R.; Testa, R.J.; Balsam, K.F. The Italian validation of the Gender Minority Stress and Resilience Measure. Psychol. Sex Orientat. Gend. Divers. 2020, 7, 208–221. [Google Scholar] [CrossRef]
| Variable | Patients n (%) or M ± SD |
|---|---|
| Age | 67.19 ± 6.83 |
| Range | 48–79 |
| Education | |
| ≤high school | 148 (75.1) |
| ≥university | 49 (24.9) |
| Ethnicity | |
| Caucasian | 193 (08) |
| Non-Caucasian | 4 (2) |
| Stable relationship | |
| Yes | 167 (84.8) |
| No | 30 (15.2) |
| Sexual orientation | |
| Heterosexual | 191 (96.9) |
| Non-heterosexual | 7 (3.1) |
| Time of treatment (in years) | 1.58 ± 1.47 |
| Type of intervention | |
| Surgery only | 188 (95.4) |
| Surgery in combination with ADT | 7 (3.6) |
| Radiation therapy only | 2 (1) |
| Radiation therapy in combination with surgery | 2 (1) |
| ISUP grade/Gleason score | |
| ISUP grade 1/Gleason score 6 | 22 (11.2) |
| ISUP grade 2/Gleason score 7 (3 + 4) | 33 (16.8) |
| ISUP grade 4/Gleason score 8 | 86 (43.6) |
| ISUP grade 5/Gleason score 9 | 21 (10.7) |
| ISUP grade 5/Gleason score 10 | 3 (1.5) |
| PSA (median and range) | 7.49 (1−103) |
| 1 | 2 | 3 | M ± SD | Ranges | |
|---|---|---|---|---|---|
| 1. Body image distress | - | 7.88 ± 6.32 | 0−27 | ||
| 2. Social support | −0.37 *** | - | 5.64 ± 1.08 | 1−7 | |
| 3. Depressive symptoms | 0.52 *** | −0.38 *** | - | 5.41 ± 5.01 | 0−24 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Scandurra, C.; Muzii, B.; La Rocca, R.; Di Bello, F.; Bottone, M.; Califano, G.; Longo, N.; Maldonato, N.M.; Mangiapia, F. Social Support Mediates the Relationship between Body Image Distress and Depressive Symptoms in Prostate Cancer Patients. Int. J. Environ. Res. Public Health 2022, 19, 4825. https://doi.org/10.3390/ijerph19084825
Scandurra C, Muzii B, La Rocca R, Di Bello F, Bottone M, Califano G, Longo N, Maldonato NM, Mangiapia F. Social Support Mediates the Relationship between Body Image Distress and Depressive Symptoms in Prostate Cancer Patients. International Journal of Environmental Research and Public Health. 2022; 19(8):4825. https://doi.org/10.3390/ijerph19084825
Chicago/Turabian StyleScandurra, Cristiano, Benedetta Muzii, Roberto La Rocca, Francesco Di Bello, Mario Bottone, Gianluigi Califano, Nicola Longo, Nelson Mauro Maldonato, and Francesco Mangiapia. 2022. "Social Support Mediates the Relationship between Body Image Distress and Depressive Symptoms in Prostate Cancer Patients" International Journal of Environmental Research and Public Health 19, no. 8: 4825. https://doi.org/10.3390/ijerph19084825
APA StyleScandurra, C., Muzii, B., La Rocca, R., Di Bello, F., Bottone, M., Califano, G., Longo, N., Maldonato, N. M., & Mangiapia, F. (2022). Social Support Mediates the Relationship between Body Image Distress and Depressive Symptoms in Prostate Cancer Patients. International Journal of Environmental Research and Public Health, 19(8), 4825. https://doi.org/10.3390/ijerph19084825










