Feasibility and Efficacy of a Virtual Reality Game-Based Upper Extremity Motor Function Rehabilitation Therapy in Patients with Chronic Stroke: A Pilot Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Pilot Study
2.1.1. Participants
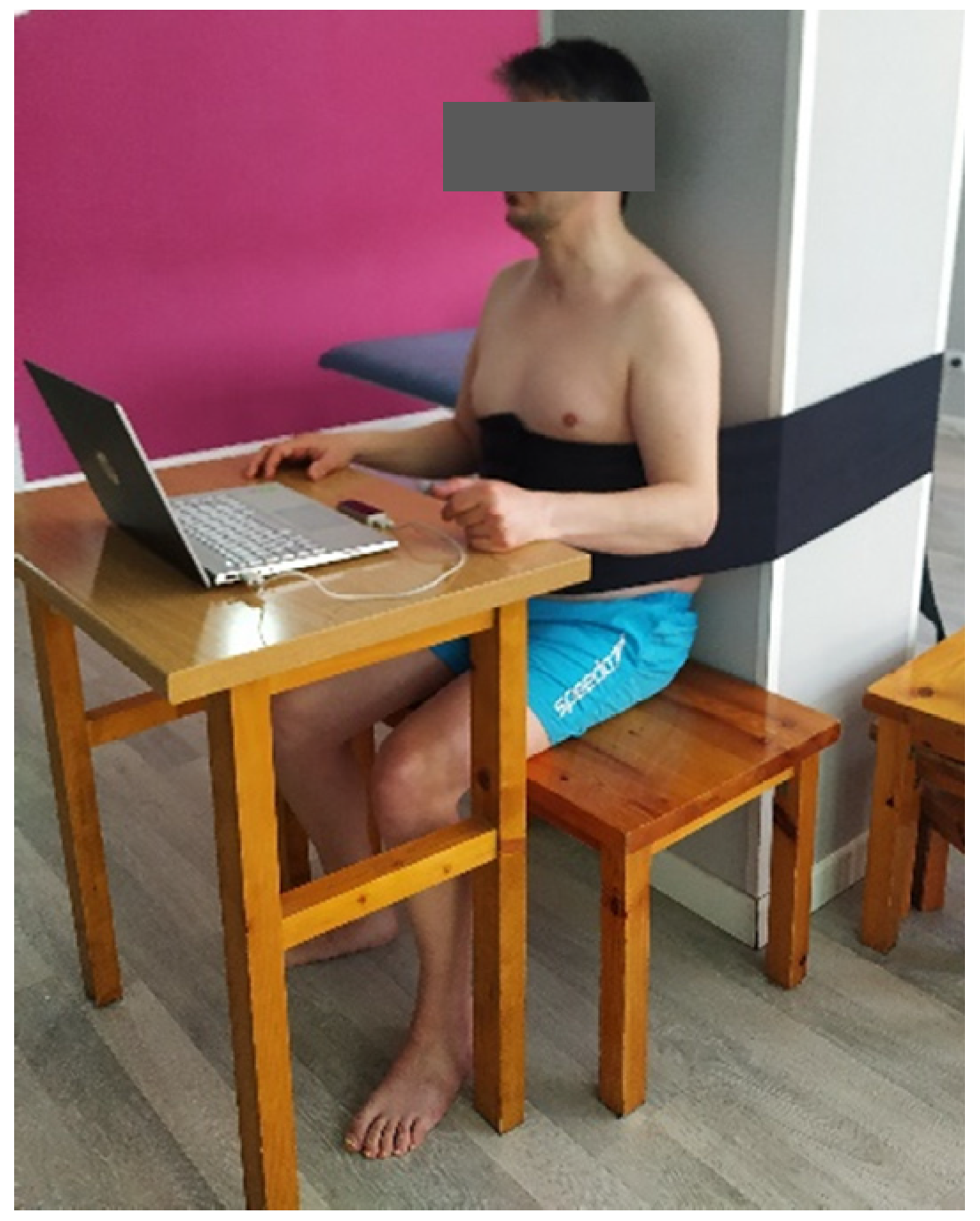
2.1.2. Procedure
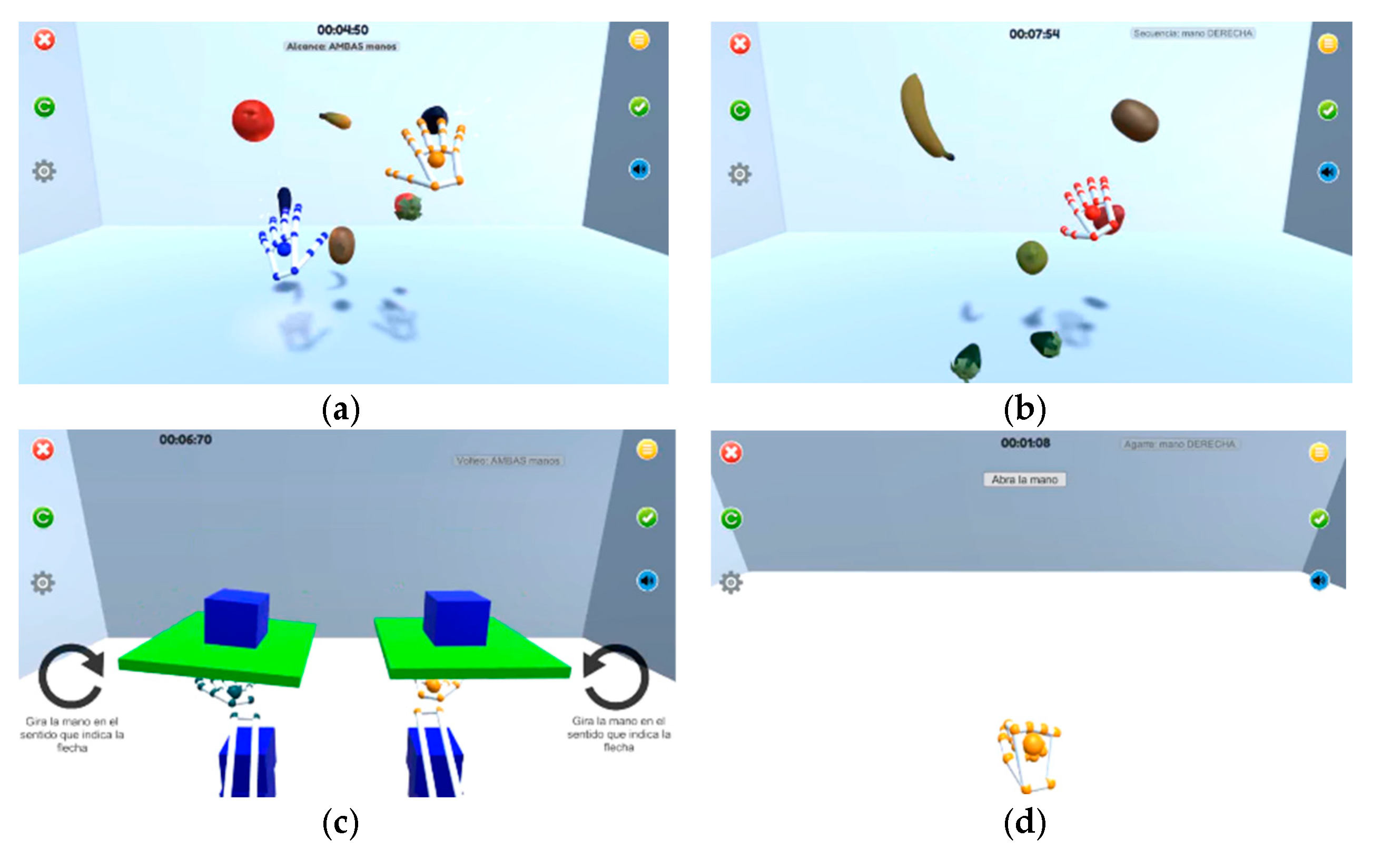
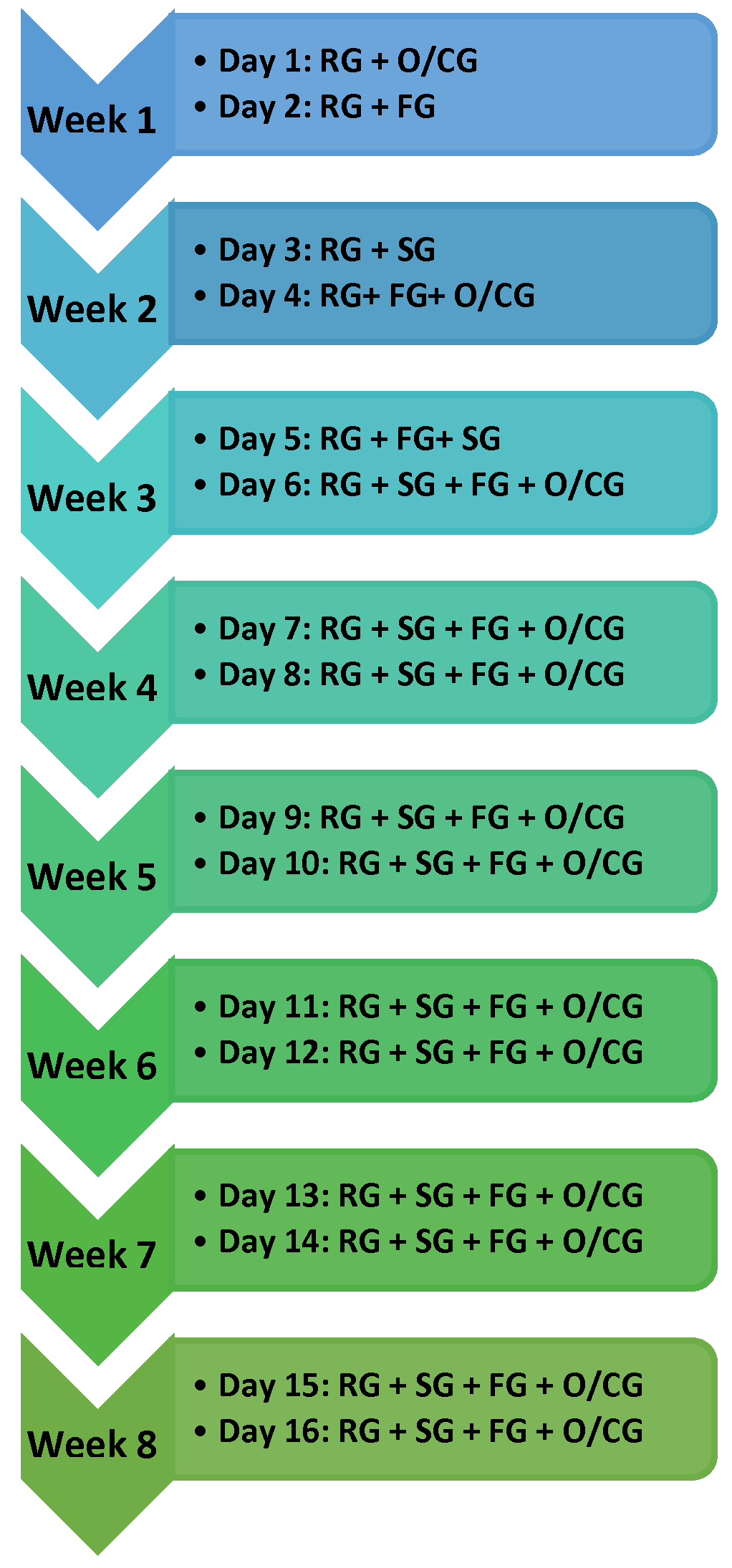
2.2. Design and Protocol
2.2.1. Outcome Measures
- Grip strength. A hydraulic Jamar hand dynamometer was used to measure the maximum grip strength. This was conducted according to the protocol of the American Hand Therapy Association [23]. In a seated position, participants had the arm in adduction, the elbow flexed to 90 degrees, the forearm in neutral position and the wrist between 0 and 30 degrees of extension. Three consecutive trials were carried out with the affected hand, and the mean of the three trials was used for statistical analysis. Clinically, grip strength is an important factor, as in the elderly population, it can inform future development as well as the most appropriate therapeutic approach [24]. Bertrand et al. [24] measured their test-retest reality, concluding that it was excellent (ICC 0.80 to 0.89).
- Action Research Arm Test (ARAT). It is a reliable tool for assessing UE motor deficits after stroke. It is a recommended test for stroke patients with an excellent test-retest reliability for this population (ICC = 0.965) [25]. It consists of 19 tests subdivided into 4 groups (grasp, grip, pinch and gross movement). The higher the score, the better the UE motor skills [26].
- The Box and Blocks Test (BBT). Through this test, gross manual dexterity was measured, both on the more affective and the less affective side. The BBT consists of moving, for one minute and one at a time, the maximum number of blocks from one side of a box to the other. It is an objective, easy to perform, reliable and standardized test and is validated for both acute and chronic stroke patients [27,28]. The minimum detectable change in stroke patients is 1.99 blocks in the most affected hand, and 2.84 blocks in the less affected hand. It has an excellent test-retest reliability for both the most affected hand (r = 0.98) and the least affected hand (r = 0.93) [28].
- Short Form Health Survey-36 Questionnaire (SF-36). The SF-36 is a generic scale on health status, valid both in the general population and in certain groups such as stroke. It consists of 36 questions subdivided into 8 scales: Physical Function, Physical Role, Body Pain, General Health, Vitality, Social Function, Emotional Role and Mental Health. It also adds an item comparing one’s health status with that of the previous year. It is used in descriptive studies as well as in therapeutic interventions [29,30]. In patients with chronic stroke, it has an excellent interrater/intra-rater reality with an ICC = 0.89 [31].
- Patient satisfaction was assessed by means of a questionnaire based on a Likert-type scale, designed by the research group. The questionnaire is made up of 9 items that assess the usefulness of the LMC in their rehabilitation, the degree of motivation, possible technical problems during the intervention, usability, whether they reported pain, the importance of therapist support, experience, frequency of use of electronic devices and the use of new technologies in the rehabilitation process. The range of the questionnaire was from 1 to 4, and the maximum possible score was 36. All questions were directly proportional, i.e., the higher the score, the better the patient’s perception [32,33].
- Attendance rate. Additionally, we recorded the attendance rate (%) for therapy sessions (compliance).
2.2.2. Data Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- De Neurologia, S.E.; Grupo de Estudio de Enfermedades Cerebrovasculares. Sociedad Española de Neurología. El Atlas del Ictus España. 2019. Available online: https://www.sen.es/images/2020/atlas/Atlas_del_Ictus_de_Espana_version_web.pdf (accessed on 10 February 2021).
- Tran, J.E.; Fowler, C.A.; Delikat, J.; Kaplan, H.; Merzier, M.M.; Schlesinger, M.R.; Litzenberger, S.; Marszalek, J.M.; Scott, S.L. Immersive Virtual Reality to Improve Outcomes in Veterans with Stroke: Protocol for a Single-Arm Pilot Study. JMIR Res. Protoc. 2021, 10, e26133. [Google Scholar] [CrossRef] [PubMed]
- Bui, J.; Luauté, J.; Farnè, A. Enhancing Upper Limb Rehabilitation of Stroke Patients with Virtual Reality: A Mini Review. Front. Virtual Real. 2021, 2, 146. [Google Scholar] [CrossRef]
- Cabeza, Á.S. Terapia Ocupacional Para la Rehabilitación del Control Motor; EAE Editorial Academia Espanola: Chisinau, Moldova, 2012. [Google Scholar]
- Cheong, M.J.; Jeon, B.; Noh, S. A protocol for systematic review and meta- analysis on psychosocial factors related to rehabilitation motivation of stroke patients. Medicine 2020, 99, e23727. [Google Scholar] [CrossRef] [PubMed]
- Schuster-Amft, C.; Eng, K.; Suica, Z.; Thaler, I.; Signer, S.; Lehmann, I.; Schmid, L.; McCaskey, M.A.; Hawkins, M.; Verra, M.; et al. Effect of a four-week virtual reality-based training versus conventional therapy on upper limb motor function after stroke: A multicenter parallel group randomized trial. PLoS ONE 2018, 13, e0204455. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Laver, K.E.; Lange, B.; George, S.; Deutsch, J.E.; Saposnik, G.; Crotty, M. Virtual reality for stroke rehabilitation. Cochrane Database Syst. Rev. 2017, 11, 57–62. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Choi, Y.; Paik, N. Mobile Game-based Virtual Reality Program for Upper Extremity Stroke Rehabilitation. J. Vis. Exp. 2018, 133, e56241. [Google Scholar] [CrossRef]
- Szczepańska-Gieracha, J.; Cieślik, B.; Rutkowski, S.; Kiper, P.; Turolla, A. What can virtual reality offer to stroke patients? A narrative review of the literature. NeuroRehabilitation 2020, 47, 109–120. [Google Scholar] [CrossRef]
- Cuesta-Gómez, A.; Sánchez-Herrera-Baeza, P.; Oña-Simbaña, E.D.; Martínez-Medina, A.; Ortiz-Comino, C.; Balaguer-Bernaldo-de-Quirós, C.; Cano-de-la-Cuerda, R. Effects of virtual reality associated with serious games for upper limb rehabilitation inpatients with multiple sclerosis: Randomized controlled trial. J. Neuroeng. Rehabil. 2020, 17, 90. [Google Scholar] [CrossRef]
- Fernández-González, P.; Tejada, M.C.; Monge-Pereira, E.; Collado-Vázquez, S.; Baeza, P.S.-H.; Cuesta-Gómez, A.; Simbaña, E.D.O.; Huete, A.J.; Molina-Rueda, F.; De Quirós, C.B.-B.; et al. Leap motion controlled video game-based therapy for upper limb rehabilitation in patients with Parkinson’s disease: A feasibility study. J. Neuroeng. Rehabil. 2019, 16, 133. [Google Scholar] [CrossRef]
- Niechwiej-Szwedo, E.; Gonzalez, D.; Nouredanesh, M.; Tung, J. Evaluation of the leap motion controller during the performance of visually-guided upper limb movements. PLoS ONE 2018, 13, e0193639. [Google Scholar] [CrossRef] [Green Version]
- Aguilera-Rubio, Á.; Alguacil-Diego, I.M.; Cuesta-Gómez, A. Uso del dispositivo Leap Motion Controller® en pacientes con ictus crónico. In XII Simposio CEA de Bioingeniería; Escuela Superior de Ciencias Experimentales y Tecnología URJC: Madrid, Spain, 2021; pp. 26–31. [Google Scholar]
- Wee, S.K.; Hughes, A.M.; Warner, M.; Burridge, J.H. Trunk restraint to promote upper extremity recovery in stroke patients: A systematic review and meta-analysis. Neurorehabil. Neural Repair 2014, 28, 660–677. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rueda, F.M.; Montero, F.M.R.; Torres, M.P.D.H.; Diego, I.M.A.; Sánchez, A.M.; Miangolarra, J.C. Análisis del movimiento de la extremidad superior hemiparética en pacientes con accidente cerebrovascular: Estudio piloto. Neurología 2012, 27, 343–347. [Google Scholar] [CrossRef] [PubMed]
- Cirstea, M.C.; Levin, M.F. Compensatory strategies for reaching in stroke. Brain 2000, 123, 940–953. [Google Scholar] [CrossRef] [PubMed]
- Pain, L.M.; Baker, R.; Richardson, D.; Agur, A.M.R. Effect of trunk-restraint training on function and compensatory trunk, shoulder and elbow patterns during post-stroke reach: A systematic review. Disabil. Rehabil. 2015, 37, 553–562. [Google Scholar] [CrossRef] [PubMed]
- De Oliveira Cacho, R.; Cacho, E.W.A.; Ortolan, R.L.; Cliquet, A.; Borges, G. Trunk restraint therapy: The continuous use of the harness could promote feedback dependence in poststroke patients. Medicine 2015, 94, e641. [Google Scholar] [CrossRef]
- Lima, R.C.; Teixeira-Salmela, L.; Michaelsen, S.M. Effects of trunk restraint in addition to home-based modified constraint-induced movement therapy after stroke: A randomized controlled trial. Int. J. Stroke 2012, 7, 258–264. [Google Scholar] [CrossRef]
- Greisberger, A.; Aviv, H.; Garbade, S.F.; Diermayr, G. Clinical relevance of the effects of reach-to-grasp training using trunk restraint in individuals with hemiparesis poststroke: A systematic review. J. Rehabil. Med. 2016, 48, 405–416. [Google Scholar] [CrossRef] [Green Version]
- Michaelsen, S.M.; Levin, M.F. Short-term effects of practice with trunk restraint on reaching movements in patients with chronic stroke: A controlled trial. Stroke 2004, 35, 1914–1919. [Google Scholar] [CrossRef] [Green Version]
- Thielman, G.; Kaminski, T.; Gentile, A.M. Rehabilitation of reaching after stroke: Comparing 2 training protocols utilizing trunk restraint. Neurorehabil. Neural Repair 2008, 22, 697–705. [Google Scholar] [CrossRef]
- Fess, E.M.C. Clinical Assessment Recommendations, 1st ed.; Garner, N.C., Ed.; American Society of Hand Therapists: Chicago, IL, USA, 1981. [Google Scholar]
- Bertrand, A.M.; Mercier, C.; Bourbonnais, D.; Desrosiers, J.; Grave, D. Reliability of maximal static strength measurements of the arms in subjects with hemiparesis. Clin. Rehabil. 2007, 21, 248–257. [Google Scholar] [CrossRef]
- Platz, T.; Pinkowski, C.; Berlin, K.; Rehabilitation, N.; Universitatsmedizin, C. Reliability and validity of arm function assessment with standardized guidelines for the FugI-Meyer Test, Action Research Arm Test and Box and Block Test: A multicentre study. Clin. Rehabil. 2005, 19, 404–411. [Google Scholar] [CrossRef] [PubMed]
- Yozbatiran, N.; Der-yeghiaian, L.; Cramer, S.C. A standardized approach to performing the action research arm test. Neurorehabil. Neural Repair 2008, 22, 78–90. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mathiowetz, V.; Volland, G.; Kashman, N.; Weber, K. Adult norms for the Box and Block Test of manual dexterity. Am. J. Occup. Ther. 1985, 39, 386–391. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, H.; Chen, C.C.; Hsueh, I.; Huang, S.; Hsieh, C. Test-Retest Reproducibility and Smallest Difference of 5 Hand Function Tests in Patients with Stroke. Neurorehabil. Neural Repair 2009, 23, 435–440. [Google Scholar] [CrossRef]
- Ware, J.E., Jr.; Snow, K.K.; Kosinski, M.G.B. SF-36 Health Survey: Manual and Interpretation Guide; New England Medical Center: Boston, MA, USA, 1993.
- Alonso, J.; Prieto, L.; Anto, J.M. The Spanish version of the SF-36 Health Survey (the SF-36 health questionnaire): An instrument for measuring clinical results. Med. Clin. 1995, 104, 771–776. [Google Scholar]
- Cabral, D.L.; Damascena, C.G.; Faria, C.D.C.M.; Melo, P.G. Comparisons of the Nottingham Health Profile and the SF-36 health survey for the assessment of quality of life in individuals with chronic stroke. Braz. J. Phys. Ther. 2012, 16, 301–308. [Google Scholar] [CrossRef] [Green Version]
- Guti, R.O.; Gal, F.; Carlos, J.; Page, M. A telerehabilitation program by virtual reality-video games improves balance and postural control in multiple sclerosis patients. NeuroRehabilitation 2013, 33, 545–554. [Google Scholar]
- Ortiz-Gutiérrez, R.; Cano-de-la-Cuerda, R.; Galán-del-Río, F. A Telerehabilitation Program Improves Postural Control in Multiple Sclerosis Patients: A Spanish Preliminary Study. Int. J. Environ. Res. Public Health 2013, 10, 5697–5710. [Google Scholar] [CrossRef] [Green Version]
- Iosa, M.; Morone, G.; Fusco, A.; Castagnoli, M.; Fusco, F.R.; Pratesi, L.; Paolucci, S. Leap motion controlled videogame-based therapy for rehabilitation of elderly patients with subacute stroke: A feasibility pilot study. Top. Stroke Rehabil. 2015, 22, 306–316. [Google Scholar] [CrossRef]
- Vanbellingen, T.; Filius, S.J.; Nyffeler, T.; van Wegen, E.E.H. Usability of videogame-based dexterity training in the early rehabilitation phase of stroke patients: A pilot study. Front. Neurol. 2017, 8, 654. [Google Scholar] [CrossRef] [Green Version]
- Ögün, M.N.; Kurul, R.; Yaşar, M.F.; Turkoglu, S.A.; Avci, Ş.; Yildiz, N. Effect of leap motion-based 3D immersive virtual reality usage on upper extremity function in ischemic stroke patients. Arq. Neuro-Psiquiatr. 2019, 77, 681–688. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, Z.; Wang, P.; Xing, L.; Mei, L.; Zhao, J.; Zhang, T. Leap Motion-based virtual reality training for improving motor functional recovery of upper limbs and neural reorganization in subacute stroke patients. Neural Regen. Res. 2017, 12, 1823. [Google Scholar] [PubMed]
- Colombo, R.; Raglio, A.; Panigazzi, M.; Mazzone, A.; Bazzini, G.; Imarisio, C.; Molteni, D.; Caltagirone, C.; Imbriani, M. The SonicHand Protocol for Rehabilitation of Hand Motor Function: A Validation and Feasibility Study. IEEE Trans. Neural Syst. Rehabil. Eng. 2019, 27, 664–672. [Google Scholar] [CrossRef]
- Fluet, G.G.; Qiu, Q.; Patel, J.; Cronce, A.; Merians, A.S.; Adamovich, S.V. Autonomous Use of the Home Virtual Rehabilitation System: A Feasibility and Pilot Study. Games Health J. 2019, 8, 432–438. [Google Scholar] [CrossRef] [PubMed]
- Hatem, S.M.; Saussez, G.; Faille, M.; Prist, V.; Dan, B. Rehabilitation of Motor Function after Stroke: A Multiple Systematic Review Focused on Techniques to Stimulate Upper Extremity Recovery. Front. Hum. Neurosci. 2016, 10, 442. [Google Scholar] [CrossRef] [Green Version]
- Intercollegiate Stroke Working Party. National Clinical Guideline for Stroke, 3rd ed.; Royal College of Physicians: London, UK, 2008. [Google Scholar]
- Teasell, R.W.; Murie Fernandez, M.; McIntyre, A.; Mehta, S. Rethinking the continuum of stroke rehabilitation. Arch. Phys. Med. Rehabil. 2014, 95, 595–596. [Google Scholar] [CrossRef] [PubMed]
- Aziz, N.A.; Leonardi-Bee, J.; Phillips, M.; Gladman, J.R.F.; Legg, L.; Walker, M.F. Therapy-based rehabilitation services for patients living at home more than one year after stroke. Cochrane Database of Systematic Reviews. Cochrane Database Syst. Rev. 2008, 2008, CD005952. [Google Scholar]
- Aguilera-Rubio, Á.; Alguacil-Diego, I.M.; Mallo-López, A.; Cuesta-Gómez, A. Use of the Leap Motion Controller System in the Rehabilitation of the Upper Limb in Stroke. A Systematic Review. J. Stroke Cerebrovasc. Dis. 2022, 31, 106174. [Google Scholar] [CrossRef]
- Aramaki, A.L.; Sampaio, R.F.; Reis, A.C.S.; Cavalcanti, A.; Dutra, F.C.M.S.E. Virtual reality in the rehabilitation of patients with stroke: An integrative review. Arq. Neuro-Psiquiatr. 2019, 77, 268–278. [Google Scholar] [CrossRef] [Green Version]
- Rutkowski, S.; Kiper, P.; Cacciante, L.; Cieślik, B.; Mazurek, J.; Turolla, A.; Szczepańska-Gieracha, J. Use of virtual reality-based training in different fields of rehabilitation: A systematic review and meta-analysis. J. Rehabil. Med. 2020, 52, jrm00121. [Google Scholar] [CrossRef]
- Knippenberg, E.; Verbrugghe, J.; Lamers, I.; Palmaers, S.; Timmermans, A.; Spooren, A. Markerless motion capture systems as training device in neurological rehabilitation: A systematic review of their use, application, target population and efficacy. J. Neuroeng. Rehabil. 2017, 14, 61. [Google Scholar] [CrossRef] [PubMed]
- Dabholkar, A.; Mehta, D.; Yardi, S.; Dabholkar, T. Assessment of scapular behavior in stroke patients. Int. J. Health Rehabil. Sci. 2015, 4, 95. [Google Scholar] [CrossRef]
- Adams, R.J.; Ellington, A.L.; Armstead, K.; Sheffield, K.; Patrie, J.T.; Diamond, P.T. Upper Extremity Function Assessment Using a Glove Orthosis and Virtual Reality System. OTJR 2019, 39, 81–89. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stevens, E.; McKevitt, C.; Emmett, E.; Wolfe, C.D. El Impacto del Ictus en Europa [Internet]. ISBN 978-1-5272-0858-2. 2014, pp. 1–42. Available online: https://ictusfederacion.es/wp-content/uploads/2018/11/Informe-completo-compressed.pdf (accessed on 22 June 2021).
- Lee, H.S.; Park, Y.J.; Park, S.W. The Effects of Virtual Reality Training on Function in Chronic Stroke Patients: A Systematic Review and Meta-Analysis. Biomed. Res. Int. 2019, 2019, 7595639. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Variable | Pre | Post | p Value |
|---|---|---|---|
| Grip strength | 16.30 (13.20) | 17.80 (14.90) | 0.005 * |
| ARAT total | 48 (30) | 50 (31) | 0.028 * |
| ARAT A | 14 (8) | 16 (9) | 0.139 |
| ARAT B | 12 (5) | 12 (5) | 0.157 |
| ARAT C | 12 (15) | 13 (13) | 0.168 |
| ARAT D | 9 (2) | 9 (1) | 0.157 |
| BBT | 27 (24) | 20.50 (23) | 0.011 * |
| SF-36. Physical function | 45 (37.50) | 50 (40) | 0.655 |
| SF36. Physical role | 62.50 (100) | 62.50 (100) | 0.317 |
| SF-36. Body ache | 35 (30) | 30 (27.50) | 0.059 |
| SF-36. General health | 60 (13.80) | 60 (13.80) | 0.317 |
| SF-36. Vitality | 55 (13.80) | 57.50 (13.80) | 0.317 |
| SF-36. Social function | 50 (12.50) | 50 (24.90) | 0.083 |
| SF-36. Emotional role | 100 (91.80) | 100 (66.90) | 0.317 |
| SF-36. Mental health | 62 (11) | 62 (12) | 0.197 |
| Item | Media (Standard Deviation) |
|---|---|
| Motivation | 3.50 (0.527) |
| Usability | 3.00 (0.816) |
| Use of electronic devices | 2.70 (0.949) |
| Pain | 3.80 (0.422) |
| Therapist support | 3.70 (0.483) |
| Technical problems | 2.60 (0.966) |
| Utility | 3.50 (0.527) |
| Experience | 3.40 (0.516) |
| New technologies | 3.80 (0.422) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aguilera-Rubio, Á.; Cuesta-Gómez, A.; Mallo-López, A.; Jardón-Huete, A.; Oña-Simbaña, E.D.; Alguacil-Diego, I.M. Feasibility and Efficacy of a Virtual Reality Game-Based Upper Extremity Motor Function Rehabilitation Therapy in Patients with Chronic Stroke: A Pilot Study. Int. J. Environ. Res. Public Health 2022, 19, 3381. https://doi.org/10.3390/ijerph19063381
Aguilera-Rubio Á, Cuesta-Gómez A, Mallo-López A, Jardón-Huete A, Oña-Simbaña ED, Alguacil-Diego IM. Feasibility and Efficacy of a Virtual Reality Game-Based Upper Extremity Motor Function Rehabilitation Therapy in Patients with Chronic Stroke: A Pilot Study. International Journal of Environmental Research and Public Health. 2022; 19(6):3381. https://doi.org/10.3390/ijerph19063381
Chicago/Turabian StyleAguilera-Rubio, Ángela, Alicia Cuesta-Gómez, Ana Mallo-López, Alberto Jardón-Huete, Edwin Daniel Oña-Simbaña, and Isabel Mª Alguacil-Diego. 2022. "Feasibility and Efficacy of a Virtual Reality Game-Based Upper Extremity Motor Function Rehabilitation Therapy in Patients with Chronic Stroke: A Pilot Study" International Journal of Environmental Research and Public Health 19, no. 6: 3381. https://doi.org/10.3390/ijerph19063381
APA StyleAguilera-Rubio, Á., Cuesta-Gómez, A., Mallo-López, A., Jardón-Huete, A., Oña-Simbaña, E. D., & Alguacil-Diego, I. M. (2022). Feasibility and Efficacy of a Virtual Reality Game-Based Upper Extremity Motor Function Rehabilitation Therapy in Patients with Chronic Stroke: A Pilot Study. International Journal of Environmental Research and Public Health, 19(6), 3381. https://doi.org/10.3390/ijerph19063381









