Robotic Systems for the Physiotherapy Treatment of Children with Cerebral Palsy: A Systematic Review
Abstract
:1. Introduction
2. Materials and Methods
2.1. Systematic Literature Research
2.2. Selection Criteria
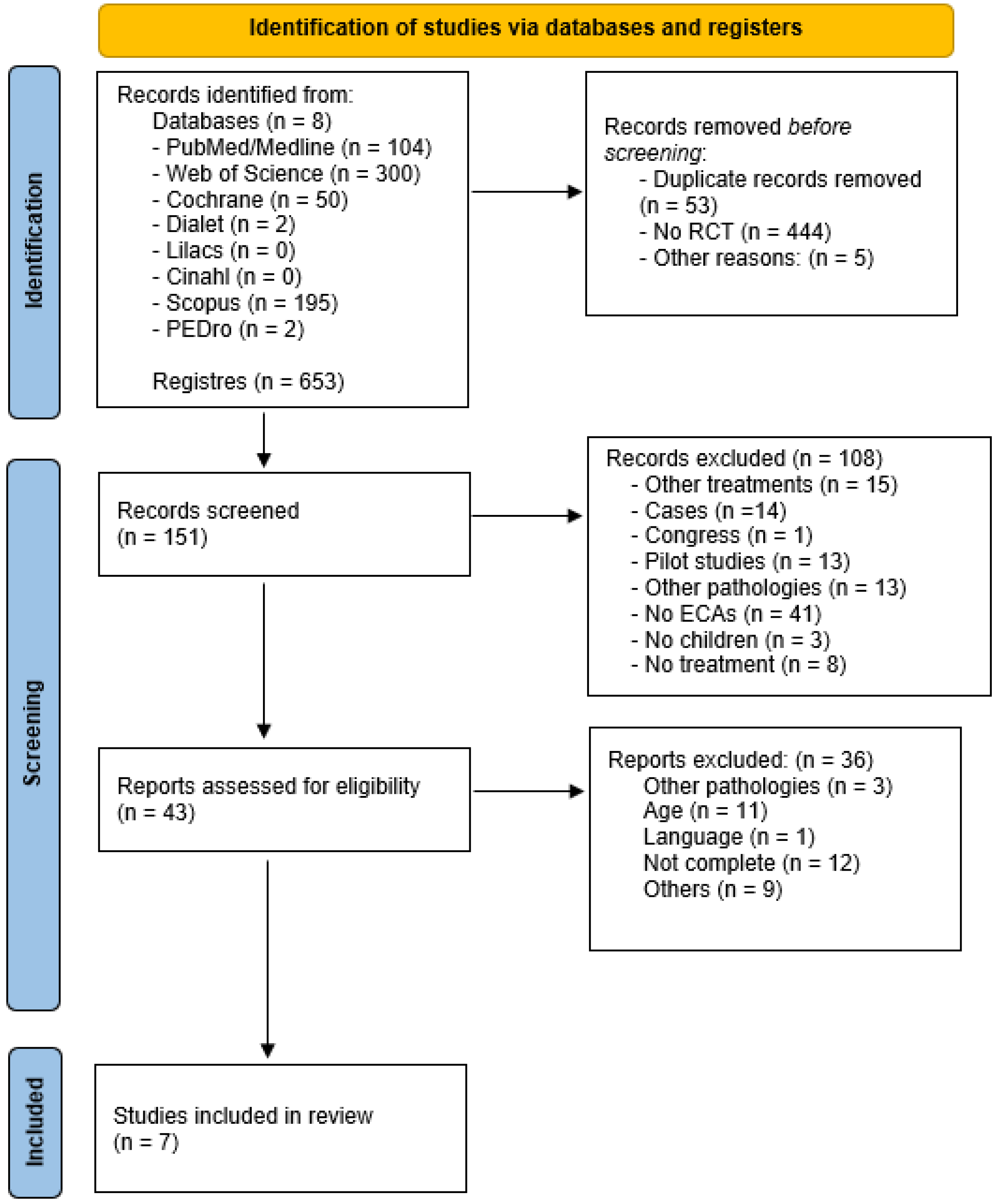
2.3. Screening, Selection and Data Extraction
2.4. Assessment of Methodological Quality and Risk of Bias
3. Results
3.1. Study Selection
3.2. Study Characteristics
3.3. Methodological Quality and Risk of Bias
3.4. Robotic Systems
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rosenbaum, P.; Paneth, N.; Leviton, A.; Goldstein, M.; Bax, M.; Damiano, D.; Dan, B.; Jacobsson, B. A report: The definition and classification of cerebral palsy April 2006. Dev. Med. Child Neurol. Suppl. 2007, 49, 8–14. [Google Scholar]
- Novak, I.; Morgan, C.; Adde, L.; Blackman, J.; Boyd, R.N.; Brunstrom-Hernandez, J.; Cioni, G.; Damiano, D.; Darrah, J.; Eliasson, A.C.; et al. Early, accurate diagnosis and early intervention in cerebral palsy: Advances in diagnosis and treatment. JAMA Pediatr. 2017, 171, 897–907. [Google Scholar] [CrossRef] [PubMed]
- Oskoui, M.; Coutinho, F.; Dykeman, J.; Jetté, N.; Pringsheim, T. An update on the prevalence of cerebral palsy: A systematic review and meta-analysis. Dev. Med. Child Neurol. 2013, 55, 509–519. [Google Scholar] [CrossRef] [PubMed]
- Sadowska, M.; Sarecka-Hujar, B.; Kopyta, I. Cerebral Palsy: Current Opinions on Definition, Epidemiology, Risk Factors, Classification and Treatment Options. Neuropsychiatr. Dis. Treat. 2020, 16, 1505–1518. [Google Scholar] [CrossRef] [PubMed]
- Balf, C.L.; Ingram, T.T.S. Problems in the Classification of Cerebral Palsy in Childhood. Br. Med. J. 1955, 2, 163–166. [Google Scholar] [CrossRef] [Green Version]
- Hagberg, G.; Hagberg, B.; Olow, I. The changing panorama of cerebral palsy in Sweden 1954—1970 III. The Importance of Foetal Deprivation of Supply. Acta Paediatr. 1976, 65, 403–408. [Google Scholar] [CrossRef] [PubMed]
- Simon-Martinez, C.; Jaspers, E.; Mailleux, L.; Desloovere, K.; Vanrenterghem, J.; Ortibus, E.; Molenaers, G.; Feys, H.; Klingels, K. Negative Influence of Motor Impairments on Upper Limb Movement Patterns in Children with Unilateral Cerebral Palsy. A Statistical Parametric Mapping Study. Front. Hum. Neurosci. 2017, 11, 482. [Google Scholar] [CrossRef]
- Hutton, J.L.; Pharoah, P.O.D.; Rosenbloom, L. Effects of cognitive, motor, and sensory disabilities on survival in cerebral palsy. Arch. Dis. Child. 2002, 86, 84–89. [Google Scholar] [CrossRef] [Green Version]
- Pharoah, P.O.D.; Cooke, T.; Johnson, M.A.; King, R.; Mutch, L. Epidemiology of cerebral palsy in England and Scotland, 1984–1989. Arch. Dis. Child. Fetal Neonatal Ed. 1998, 79, F21–F25. [Google Scholar] [CrossRef] [Green Version]
- Bjornson, K.F.; Zhou, C.; Stevenson, R.; Christakis, D.; Song, K. Walking activity patterns in youth with cerebral palsy and youth developing typically. Disabil. Rehabil. 2014, 36, 1279–1284. [Google Scholar] [CrossRef] [Green Version]
- Gorter, H.; Holty, L.; Rameckers, E.E.; Elvers, H.J.; Oostendorp, R.A. Changes in Endurance and Walking Ability Through Functional Physical Training in Children with Cerebral Palsy. Pediatr. Phys. Ther. 2009, 21, 31–37. [Google Scholar] [CrossRef] [PubMed]
- Wu, M.; Kim, J.; Gaebler-Spira, D.J.; Schmit, B.D.; Arora, P. Robotic Resistance Treadmill Training Improves Locomotor Function in Children with Cerebral Palsy: A Randomized Controlled Pilot Study. Arch. Phys. Med. Rehabil. 2017, 98, 2126–2133. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kolobe, A.; Fagg, T.H.A. Robot Reinforcement and Error-Based Movement Learning in Infants with and Without Cerebral Palsy. Phys. Ther. 2019, 99, 677–688. [Google Scholar] [CrossRef] [PubMed]
- Dusing, S.C.; Harbourne, R.T.; Lobo, M.A.; Westcott-McCoy, S.; Bovaird, J.A.; Kane, A.E.; Syed, G.; Marcinowski, E.C.; Koziol, N.A.; Brown, S.E. A Physical Therapy Intervention to Advance Cognitive and Motor Skills: A Single Subject Study of a Young Child with Cerebral Palsy. Pediatr. Phys. Ther. 2019, 31, 347–352. [Google Scholar] [CrossRef]
- Kolb, B.; Harker, A.; Gibb, R. Principles of plasticity in the developing brain. Dev. Med. Child Neurol. 2017, 59, 1218–1223. [Google Scholar] [CrossRef] [Green Version]
- Nithianantharajah, J.; Hannan, A. Enriched environments, experience-dependent plasticity and disorders of the nervous system. Nat. Rev. Neurosci. 2006, 7, 697–709. [Google Scholar] [CrossRef]
- Roberts, H.; Shierk, A.; Clegg, N.J.; Baldwin, D.; Smith, L.; Yeatts, P.; Delgado, M.R. Constraint Induced Movement Therapy Camp for Children with Hemiplegic Cerebral Palsy Augmented by Use of an Exoskeleton to Play Games in Virtual Reality. Phys. Occup. Ther. Pediatr. 2020, 41, 150–165. [Google Scholar] [CrossRef]
- Balgayeva, M.; Bulekbayeva, S. Effectiveness of the combined use of robotic kinesiotherapy and botulinum therapy in the complex rehabilitation of children with cerebral palsy. Asian J. Pharm. Clin. Res. 2018, 11, 360–364. [Google Scholar]
- Ren, K.; Gong, X.; Zhang, R.; Chen, X. Effects of virtual reality training on limb movement in children with spastic diplegia cerebral palsy. Zhongguo Dang Dai Er Ke Za Zhi 2016, 18, 975–979. [Google Scholar]
- Ivanova, E.; Krause, A.; Schalicke, M.; Schellhardt, F.; Jankowski, N.; Achner, J.; Schmidt, H.; Joebges, M.; Kruger, J. Let’s do this together: Bi-Manu-Interact, a novel device for studying human haptic interactive behavior. IEEE Int. Conf. Rehabil. Robot. 2017, 2017, 708–713. [Google Scholar] [CrossRef]
- Marchal-Crespo, L.; Reinkensmeyer, D.J. Review of control strategies for robotic movement training after neurologic injury. J. Neuroeng. Rehabil. 2009, 6, 20. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cherni, Y.; Girardin-Vignola, G.; Ballaz, L.; Begon, M. Reliability of maximum isometric hip and knee torque measurements in children with cerebral palsy using a paediatric exoskeleton—Lokomat. Neurophysiol. Clin. Neurophysiol. 2019, 49, 335–342. [Google Scholar] [CrossRef] [PubMed]
- Tornberg, A.B.; Lauruschkus, K. Non-ambulatory children with cerebral palsy: Effects of four months of static and dynamic standing exercise on passive range of motion and spasticity in the hip. PeerJ 2020, 8, e8561. [Google Scholar] [CrossRef] [PubMed]
- Van Hedel, H.J.; Severini, G.; Scarton, A.; O’Brien, A.; Reed, T.; Gaebler-Spira, D.; Egan, T.; Meyer-Heim, A.; Graser, J.; Chua, K.; et al. Correction to: Advanced Robotic Therapy Integrated Centers (ARTIC): An international collaboration facilitating the application of rehabilitation technologies. J. Neuroeng. Rehabil. 2018, 15, 36. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Maher, C.G.; Sherrington, C.; Herbert, R.D.; Moseley, A.M.; Elkins, M. Reliability of the PEDro Scale for Rating Quality of Randomized Controlled Trials. Phys. Ther. 2003, 83, 713–721. [Google Scholar] [CrossRef] [Green Version]
- Drużbicki, M.; Rusek, W.; Snela, S.; Dudek, J.; Szczepanik, M.; Zak, E.; Durmala, J.; Czernuszenko, A.; Bonikowski, M.; Sobota, G. Functional effects of robotic-assisted locomotor treadmill thearapy in children with cerebral palsy. J. Rehabil. Med. 2013, 45, 358–363. [Google Scholar] [CrossRef] [Green Version]
- Wallard, L.; Dietrich, G.; Kerlirzin, Y.; Bredin, J. Robotic-assisted gait training improves walking abilities in diplegic children with cerebral palsy. Eur. J. Paediatr. Neurol. 2017, 21, 557–564. [Google Scholar] [CrossRef]
- Wallard, L.; Dietrich, G.; Kerlirzin, Y.; Bredin, J. Effect of robotic-assisted gait rehabilitation on dynamic equilibrium control in the gait of children with cerebral palsy. Gait Posture 2018, 60, 55–60. [Google Scholar] [CrossRef]
- Yazıcı, M.; Livanelioğlu, A.; Gücüyener, K.; Tekin, L.; Sümer, E.; Yakut, Y. Effects of robotic rehabilitation on walking and balance in pediatric patients with hemiparetic cerebral palsy. Gait Posture 2019, 70, 397–402. [Google Scholar] [CrossRef]
- Jin, L.H.; Yang, S.; Choi, J.Y.; Sohn, M.K. The Effect of Robot-Assisted Gait Training on Locomotor Function and Functional Capability for Daily Activities in Children with Cerebral Palsy: A Single-Blinded, Randomized Cross-Over Trial. Brain Sci. 2020, 10, 801. [Google Scholar] [CrossRef] [PubMed]
- Petrarca, M.; Frascarelli, F.; Carniel, S.; Colazza, A.; Minosse, S.; Tavernese, E.; Castelli, E. Robotic-assisted locomotor treadmill therapy does not change gait pattern in children with cerebral palsy. Int. J. Rehabil. Res. 2021, 44, 69–76. [Google Scholar] [CrossRef] [PubMed]
- Yaşar, B.; Atıcı, E.; Razaei, D.A.; Saldıran, T. Effectiveness of Robot-Assisted Gait Training on Functional Skills in Children with Cerebral Palsy. J. Pediatr. Neurol. 2021. [Google Scholar] [CrossRef]
- Fang, Y.; Lerner, Z.F. Feasibility of Augmenting Ankle Exoskeleton Walking Performance with Step Length Biofeedback in Individuals with Cerebral Palsy. IEEE Trans. Neural Syst. Rehabil. Eng. 2021, 29, 442–449. [Google Scholar] [CrossRef]
- Gerber, C.N.; Kunz, B.; Van Hedel, H.J.A. Preparing a neuropediatric upper limb exergame rehabilitation system for home-use: A feasibility study. J. Neuroeng. Rehabil. 2016, 13, 33. [Google Scholar] [CrossRef] [Green Version]
- Mehrholz, J.; Hädrich, A.; Platz, T.; Kugler, J.; Pohl, M. Electromechanical and robot-assisted arm training for improving gene. Phys. Rev. Lett. 2012, 80, 2967. [Google Scholar]
- Lo, A.C.; Guarino, P.D.; Richards, L.G.; Haselkorn, J.K.; Wittenberg, G.F.; Federman, D.G.; Ringer, R.J.; Wagner, T.; Krebs, H.I.; Volpe, B.; et al. Robot-Assisted Therapy for Long-Term Upper-Limb Impairment after Stroke. N. Engl. J. Med. 2010, 362, 1772–1783. [Google Scholar] [CrossRef] [Green Version]
- Timmermans, A.A.; Seelen, H.A.; Willmann, R.D.; Kingma, H. Technology-assisted training of arm-hand skills in stroke: Concepts on reacquisition of motor control and therapist guidelines for rehabilitation technology design. J. Neuroeng. Rehabil. 2009, 6, 1. [Google Scholar] [CrossRef] [Green Version]
- Oujamaa, L.; Relave, I.; Froger, J.; Mottet, D.; Pelissier, J.-Y. Rehabilitation of arm function after stroke. Literature review. Ann. Phys. Rehabil. Med. 2009, 52, 269–293. [Google Scholar] [CrossRef]
- Biffi, E.; Maghini, C.; Cairo, B.; Beretta, E.; Peri, E.; Altomonte, D.; Mazzoli, D.; Giacobbi, M.; Prati, P.; Merlo, A.; et al. Movement Velocity and Fluidity Improve after Armeo® Spring Rehabilitation in Children Affected by Acquired and Congenital Brain Diseases: An Observational Study. BioMed Res. Int. 2018, 2018, 1537170. [Google Scholar] [CrossRef] [Green Version]
- Dobson, F.; Morris, M.E.; Baker, R.; Wolfe, R.; Graham, H.K. Clinician agreement on gait pattern ratings in children with spastic hemiplegia. Dev. Med. Child Neurol. 2006, 48, 429–435. [Google Scholar] [CrossRef] [PubMed]
- Aycardi, L.F.; Cifuentes, C.A.; Múnera, M.; Bayón, C.; Ramírez, O.; Lerma, S.; Frizera, A.; Rocon, E. Evaluation of biomechanical gait parameters of patients with Cerebral Palsy at three different levels of gait assistance using the CPWalker. J. Neuroeng. Rehabil. 2019, 16, 15. [Google Scholar] [CrossRef] [PubMed]
- Pool, D.; Elliott, C.; Bear, N.; Taylor, N.; Valentine, J. Locomotor training in children with cerebral palsy: Is Functional Electrical Stimulation integrated robotic training effective? A randomized controlled trial. Dev. Med. Child Neurol. 2020, 62, 53–60. [Google Scholar]
- Myrhaug, H.T.; Østensjø, S.; Larun, L.; Odgaard-Jensen, J.; Jahnsen, R. Intensive training of motor function and functional skills among young children with cerebral palsy: A systematic review and meta-analysis. BMC Pediatr. 2014, 14, 292. [Google Scholar] [CrossRef] [Green Version]
- Bleyenheuft, Y.; Ebner-Karestinos, D.; Surana, B.; Paradis, J.; Sidiropoulos, A.; Renders, A.; Friel, K.M.; Brandao, M.; Rameckers, E.; Gordon, A. Intensive upper- and lower-extremity training for children with bilateral cerebral palsy: A quasi-randomized trial. Dev. Med. Child Neurol. 2017, 59, 625–633. [Google Scholar] [CrossRef] [Green Version]
- Shin, J.; Yang, S.; Park, C.; Lee, Y.; You, S.H. Comparative effects of passive and active mode robot-assisted gait training on brain and muscular activities in sub-acute and chronic stroke. NeuroRehabilitation 2022. [Google Scholar] [CrossRef]
- Emken, J.L.; Bobrow, J.E.; Reinkensmeyer, D.J. Robotic movement training as an optimization problem: Designing a controller that assists only as needed. In Proceedings of the 9th International Conference on Rehabilitation Robotics, Chicago, IL, USA, 28 June–1 July 2005; pp. 307–312. [Google Scholar]
- Wegner, N.; Zeaman, D. Team and Individual Performances on a Motor Learning Task. J. Gen. Psychol. 1956, 55, 127–142. [Google Scholar] [CrossRef]
- Reed, K.; Peshkin, M.A. Physical Collaboration of Human-Human and Human-Robot Teams. IEEE Trans. Haptics 2008, 1, 108–120. [Google Scholar] [CrossRef] [Green Version]
- Reed, K.; Peshkin, M.; Hartmann, M.J.; Grabowecky, M.; Patton, J.; Yishton, P.M. Haptically linked dyads are two motor-control systems better than one? Psychol. Sci. 2006, 17, 365–366. [Google Scholar] [CrossRef]
- Ganesh, G.; Takagi, A.; Osu, R.; Yoshioka, T.; Kawato, M.; Burdet, E. Two is better than one: Physical interactions improve motor performance in humans. Sci. Rep. 2014, 4, 3824. [Google Scholar] [CrossRef] [Green Version]
- Jarrassé, N.; Charalambous, T.; Burdet, E. A Framework to Describe, Analyze and Generate Interactive Motor Behaviors. PLoS ONE 2012, 7, e49945. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hesse, S.; Schulte-Tigges, G.; Konrad, M.; Bardeleben, A.; Werner, C. Robot-assisted arm trainer for the passive and active practice of bilateral forearm and wrist movements in hemiparetic subjects. Arch. Phys. Med. Rehabil. 2003, 84, 915–920. [Google Scholar] [CrossRef]
- Ikoeva, G.A.; Nikityuk, I.E.; Kivoenko, O.I.; Moshonkina, T.R.; Solopova, I.A.; Sukhotina, I.A.; Vissarionov, S.V.; Umnov, V.V.; Gerasimenko, Y.P. Clinical, neurological, and neurophysiological evaluation of the efficiency of motor rehabilitation in children with cerebral palsy using robotic mechanotherapy and transcutaneous electrical stimulation of the spinal cord. Pediatr. Traumatol. Orthop. Reconstr. Surg. 2016, 4, 47–55. [Google Scholar] [CrossRef]
- Lin, Y.; Wang, G.; Wang, B. Rehabilitation treatment of spastic cerebral palsy with radial extracorporeal shock wave therapy and rehabilitation therapy. Medicine 2018, 97, e13828. [Google Scholar] [CrossRef]
- Ramírez, J.O.; de la Cruz, S.P. Therapeutic effects of kinesio taping in children with cerebral palsy: A systematic review. Arch. Argent. Pediatr. 2017, 115, E356–E361. [Google Scholar]
- Marrades-Caballero, E.; Santonja-Medina, C.S.; Sanz-Mengibar, J.M.; Santonja-Medina, F. Neurologic music therapy in upper-limb rehabilitation in children with severe bilateral cerebral palsy: A randomized controlled trial. Eur. J. Phys. Rehabil. Med. 2018, 54, 866–872. [Google Scholar] [CrossRef]
- Ammann-Reiffer, C.; Bastiaenen, C.H.; Meyer-Heim, A.D.; van Hedel, H.J. Lessons learned from conducting a pragmatic, randomized, crossover trial on robot-assisted gait training in children with cerebral palsy (PeLoGAIT). J. Pediatr. Rehabil. Med. 2020, 13, 137–148. [Google Scholar] [CrossRef]
| Author (Year) | Population | Robotic System | Intervention | Results and Conclusions |
|---|---|---|---|---|
| MARIUSZ DRUZBICKI (2013) [27] | 52 children with spastic diplegic cerebral palsy (6–13 years) | Lokomat active orthosis | Individual exercise program (motor control, sitting stability and walking skills) with Lokomat or individual exercise program; 20 sessions of 45 min | Walking speed showed a low level of improvement in both groups (r = −0.53, p = 0.0011). No statistically significant changes in gait parameters after 4 weeks. Lokomat: no significative improvement (p > 0.05). |
| LAURA WALLARD (2017) [28] | 30 children with bilateral spastic cerebral palsy (8–10 years) | Lokomat Pediatric | Lokomat Pediatric or physical/occupational therapy treatment (passive–active mobilizations, balance, grasping and displacements); 20 sessions: 5 times perweek (40 min) for 4 weeks | Lokomat improved walking ability, upper body control and lower limb kinematics. Standing activity: 60.58% ± 14.71 for experimental group versus 55.74% ± 15.02 for control group. 50.87% ± 15.82 for experimental group versus 43.61% ± 12.59 for control group for walking, running and climbing activities. |
| LAURA WALLARD (2018) [29] | 30 children with bilateral spastic cerebral palsy (8–10 years) | Lokomat Pediatric | Lokomat Pediatric or physical/occupational therapy treatment for walking on level ground or a mat and balance (unipodal or bipodal) up and down stairs; 20 sessions: 5 times per week (40 min) for 4 weeks | Lokomat system favored new gait organization to improve postural and locomotor functions and gait patterns: p = 0.073 (experimental group) versus p = 0.048 (control group). Lokomat system did not replace other therapies, it was a complement. |
| MELTEN YAZICI (2019) [30] | 24 children with congenital spastic hemiparetic cerebral palsy (5–12 years) | Innowalk Pro: robotic gait training program | Conventional treatment (stretching and strengthening exercises, squats, stair climbing and descending, functional reaching, balance and standing on a single leg) with RGTP or conventional treatment; 3 times per week (30 min) for 12 weeks | Muscle strength, balance (52.08 (2.68) points for experimental group versus 51.00 (3.30) for control group), walking speed (22 m for experimental group), functionality (93.00 (10.11) for experimental group versus 92.71 (8.88) for control group), endurance and peripheral O2 saturation improved. Experimental group: effects were preserved after three months. Robotic system rehabilitation: supportive tool, but not a therapeutic method alone. |
| LI HUA JIN (2020) [31] | 20 children with cerebral palsy (4–9 years) | Walkbot-K system (exoskeletal robot-assisted gait training) | Conventional physical therapy (2–4 times per week) or robotic system-assisted gait training (3 times per week, 30 min); 18 sessions over 6 weeks | Gross motor function and functional capability in daily activities improved after 6 weeks of treatment with the Walkbot-K system (p = 0.018 for standing activities and p = 0.021 for dynamic activities). |
| MAURIZIO PETRARCA (2020) [32] | 24 children with diplegic cerebral palsy (4–13 years) | Lokomat | Robotic system-assisted gait training and physiotherapy (functional gait exercises); 20 sessions: 5 times per week for 4 weeks | Robotic system-assisted gait training with Lokomat and physiotherapy produced no conclusive results in the search for new adaptative solutions for these children. |
| BURAK YASAR (2021) [33] | 26 children with diplegic cerebral palsy (7–14) | Robogait | Conventional physical therapy (40 min) and RoboGait (25 min) 2 times per week or conventional therapy alone (65 min) 2 times per week; 16 sessions over 8 weeks | No significant differences were observed between groups, although both groups showed improvement in functional independence, balance and performance at the end of the therapy (29.08 points (10.28) in robotic system group versus 26.69 points (10.82) in control group). Robogait alone was not superior to conventional physical therapy (p > 0.05). |
| M. DRUZBICKI (2013) | L. WALLARD (2017) | L. WALLARD (2018) | M. YACIZI (2019) | LH. JIN (2020) | M. PETRARCA (2020) | B. YASAR (2021) | |
|---|---|---|---|---|---|---|---|
| RANDOM PARTICIPANT ALLOCATION | Y | Y | Y | N | Y | N | Y |
| CONCEALED ALLOCATION | Y | Y | Y | N | Y | N | Y |
| GROUPS SIMILAR AT BASELINE | Y | Y | Y | Y | Y | NA | Y |
| SUBJECT BLINDING | N | N | N | N | N | N | N |
| THERAPIST BLINDING | N | N | N | N | N | N | Y |
| ASSESSOR BLINDING | Y | Y | N | N | Y | N | Y |
| LESS THAN 15% DROPOUT | N | Y | N | Y | Y | Y | Y |
| INTENTION TO TREAT ANALYSIS | N | N | N | N | N | N | N |
| STATISTICAL COMPARISONS BETWEEN GROUPS | Y | Y | Y | Y | Y | Y | Y |
| POINT MEASURES AND VARIABILITY DATA | Y | Y | Y | Y | Y | Y | Y |
| TOTAL SCORE | 6/10 | 7/10 | 5/10 | 4/10 | 7/10 | 3/10 | 8/10 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Llamas-Ramos, R.; Sánchez-González, J.L.; Llamas-Ramos, I. Robotic Systems for the Physiotherapy Treatment of Children with Cerebral Palsy: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 5116. https://doi.org/10.3390/ijerph19095116
Llamas-Ramos R, Sánchez-González JL, Llamas-Ramos I. Robotic Systems for the Physiotherapy Treatment of Children with Cerebral Palsy: A Systematic Review. International Journal of Environmental Research and Public Health. 2022; 19(9):5116. https://doi.org/10.3390/ijerph19095116
Chicago/Turabian StyleLlamas-Ramos, Rocío, Juan Luis Sánchez-González, and Inés Llamas-Ramos. 2022. "Robotic Systems for the Physiotherapy Treatment of Children with Cerebral Palsy: A Systematic Review" International Journal of Environmental Research and Public Health 19, no. 9: 5116. https://doi.org/10.3390/ijerph19095116
APA StyleLlamas-Ramos, R., Sánchez-González, J. L., & Llamas-Ramos, I. (2022). Robotic Systems for the Physiotherapy Treatment of Children with Cerebral Palsy: A Systematic Review. International Journal of Environmental Research and Public Health, 19(9), 5116. https://doi.org/10.3390/ijerph19095116







