Water, Sanitation and Hygiene in Schools in Low- and Middle-Income Countries: A Systematic Review and Implications for the COVID-19 Pandemic
Abstract
1. Introduction
- (i)
- What is the situation of water, sanitation and hygiene conditions in schools in LMICs?
- (ii)
- What are the implications of the current WASH conditions in schools in LMICs for the safe reopening of schools during the ongoing COVID-19 pandemic and for future water-related pandemics?
2. Materials and Methods
2.1. Search Strategy
2.2. Selection Criteria
2.3. Data Extraction
- (i)
- Availability: water supply must be sufficient and continuous, and sanitation facilities should be available for use at all times of day and night in sufficient numbers.
- (ii)
- Accessibility: water and sanitation facilities should be physically accessible within or in the immediate vicinity of the environment to all at all times. The design of the facilities should also take into account elderly people, young children, and persons with disabilities.
- (iii)
- Affordability: water and sanitation services must be affordable for all. The costs must not affect peoples’ capacity to secure other essential necessities guaranteed by human rights.
- (iv)
- Quality and safety: The water must be safe, therefore free from micro-organisms, chemical substances, and radiological hazards that constitute a threat to health (i.e., it should follow the national, local, or international guidelines for drinking water quality). As for sanitation, the facilities must be situated where physical security can be safeguarded and must be hygienic. Wastewater and excreta must be safely disposed to effectively prevent human, animal, and insect contact with human feces, and the infrastructure should be constructed to prevent collapse.
- (v)
- Acceptability, privacy, and dignity: All water and sanitation facilities and services must be culturally appropriate and sensitive to gender, lifecycle, and privacy requirements. Water organoleptic properties such as odor, taste, and color should be acceptable, and sanitation facilities must have their design, positioning, and conditions of use sensitive to people’s cultures and priorities. That includes gender-separated facilities, infrastructure that ensures privacy, and appropriate resources for menstrual.
2.4. Quality Assessment
3. Results
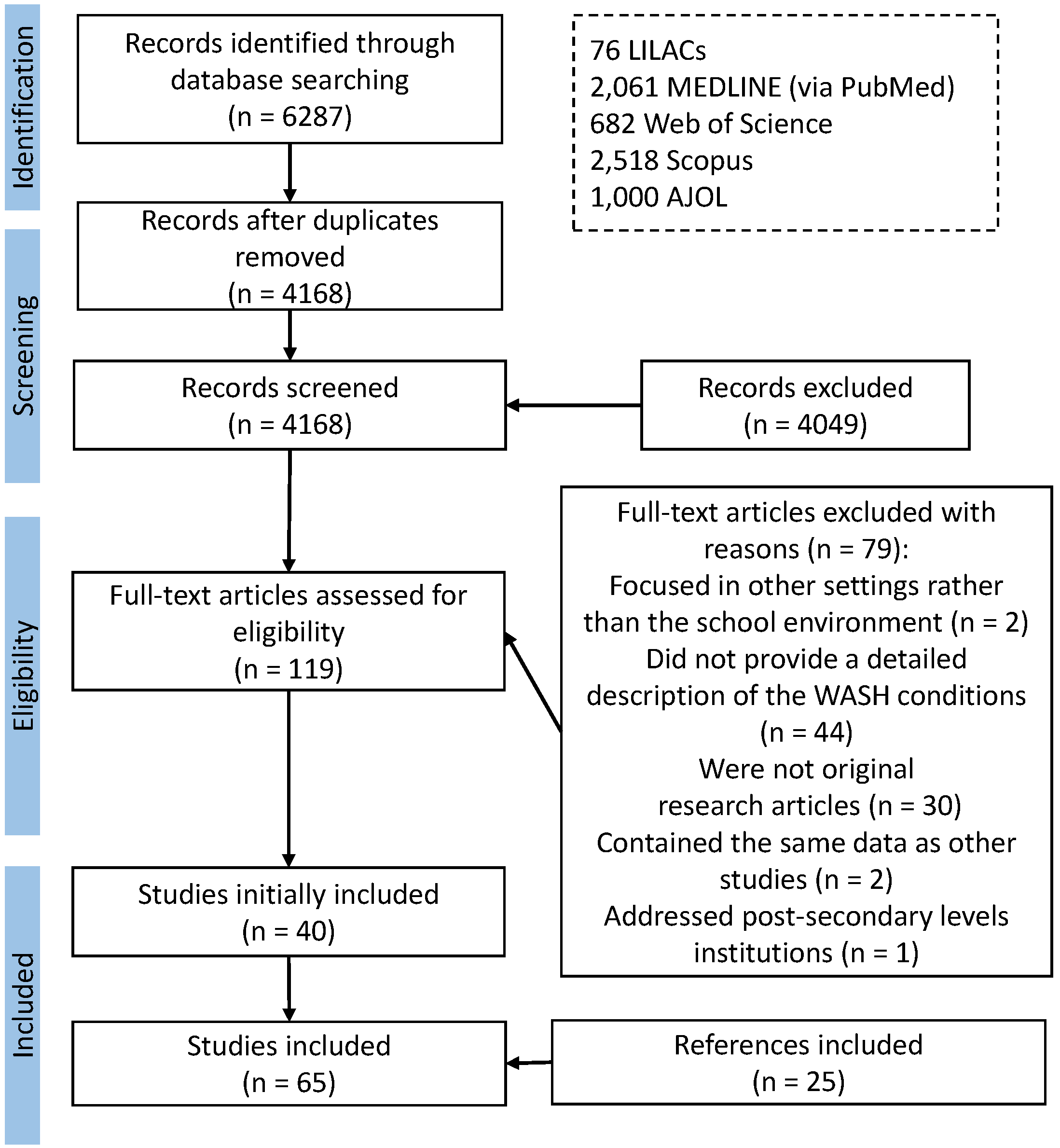
3.1. Search Results
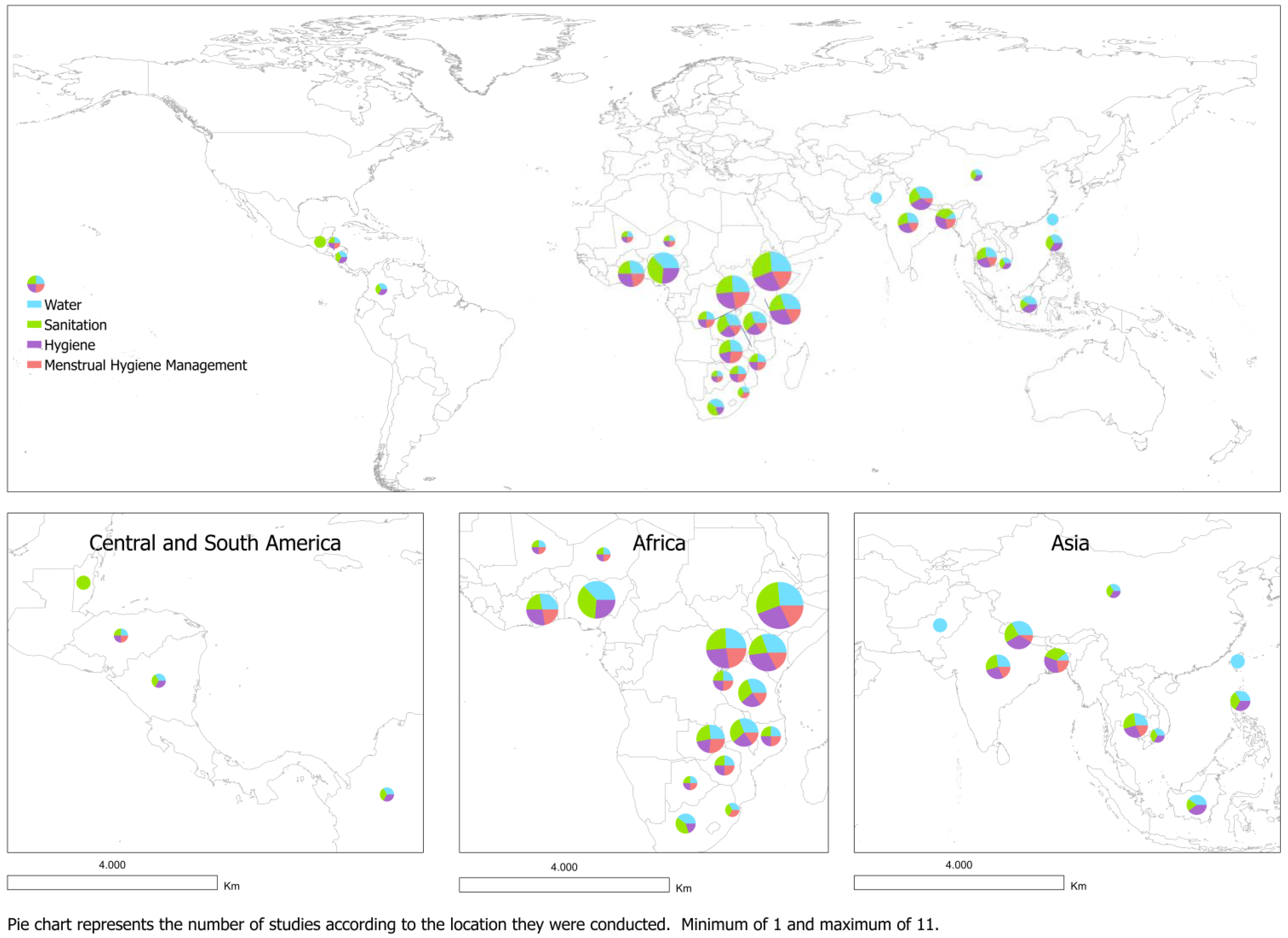
3.2. Study Characteristics
3.3. Quality Assessment Results
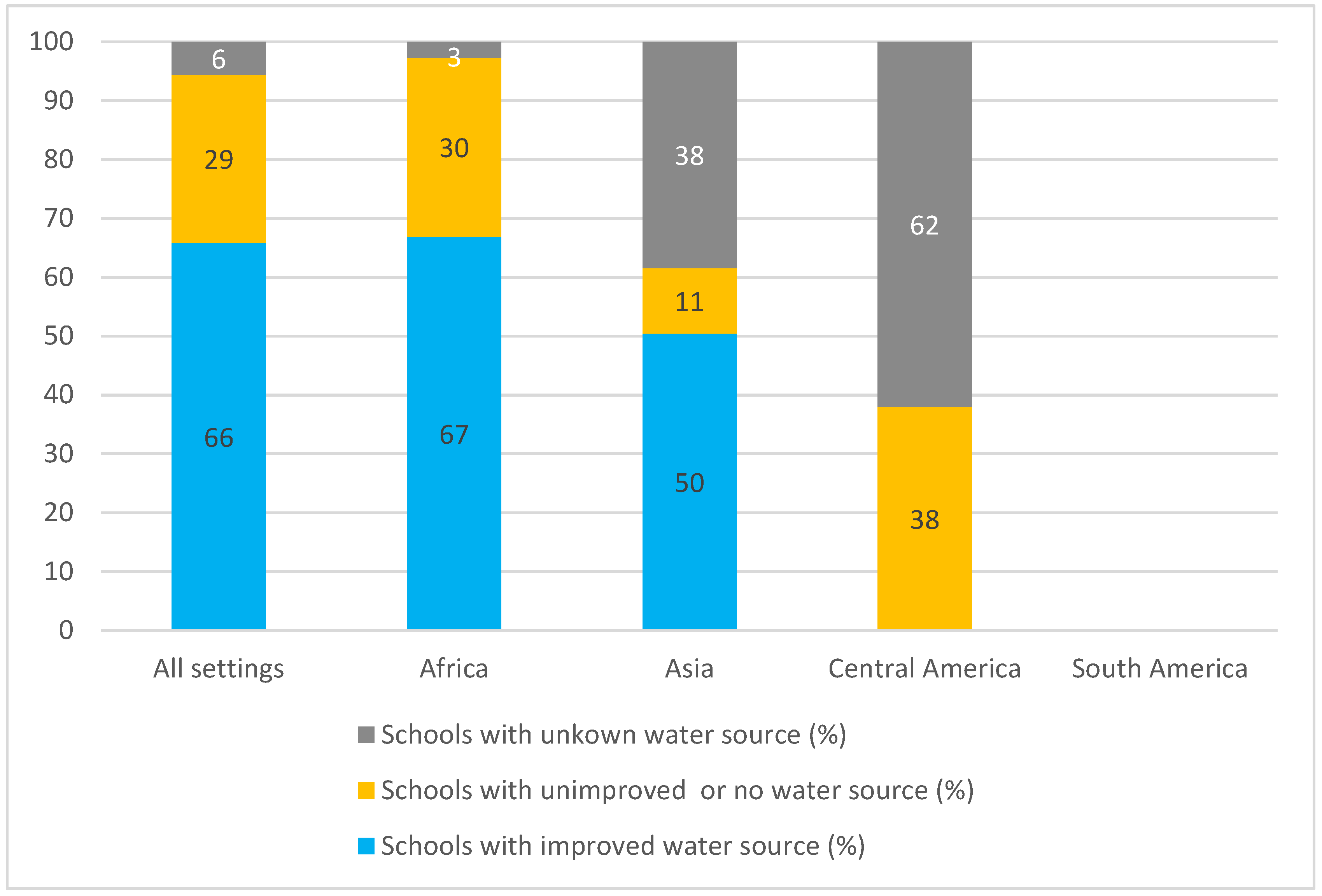
3.4. Water
3.4.1. Availability
3.4.2. Accessibility
3.4.3. Affordability
3.4.4. Quality and Safety
3.4.5. Acceptability, Dignity and Privacy
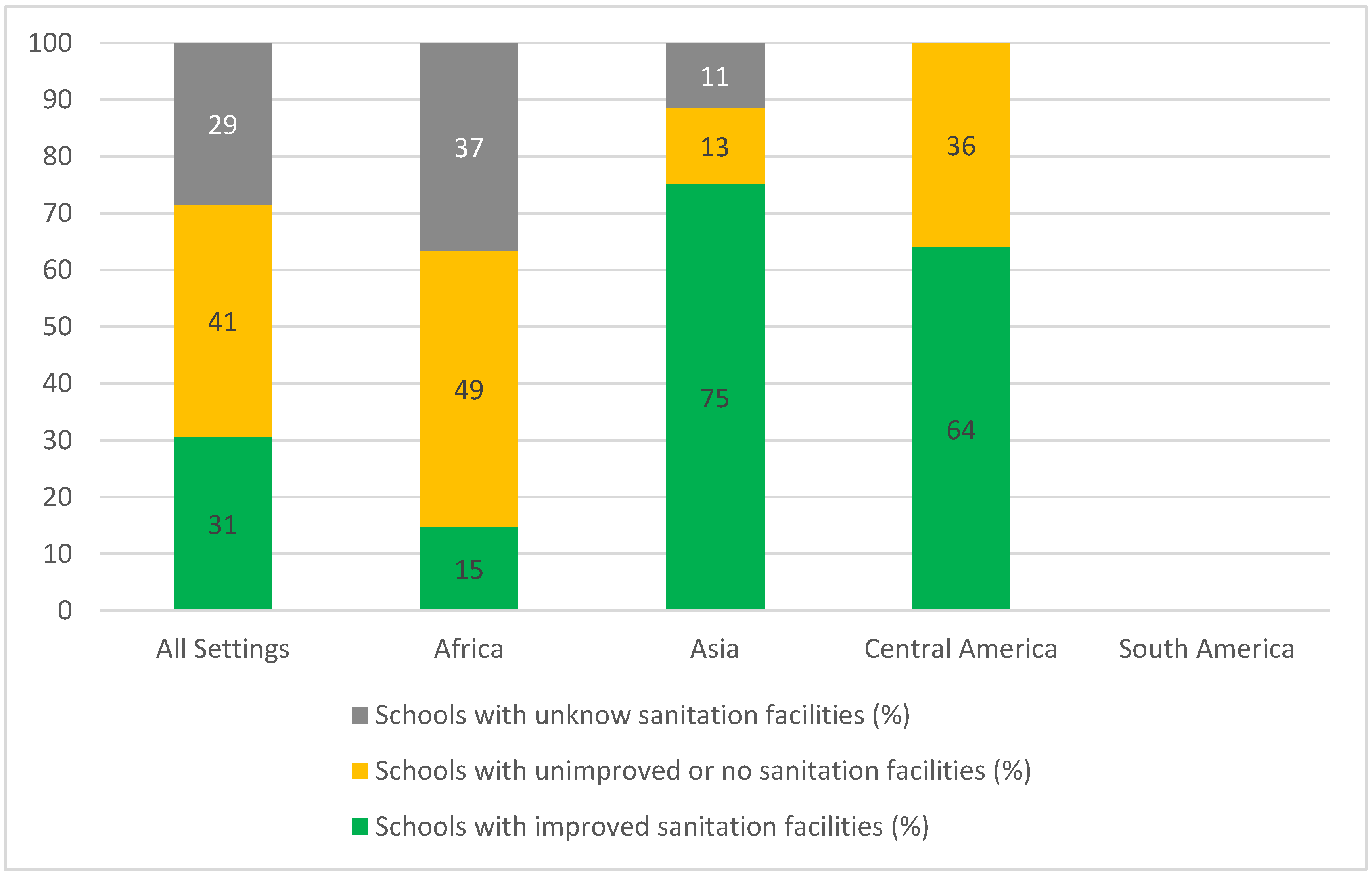
3.5. Sanitation
3.5.1. Availability
3.5.2. Accessibility
3.5.3. Affordability
3.5.4. Quality and Safety
3.5.5. Acceptability, Dignity and Privacy
3.6. Hygiene
3.6.1. Availability
3.6.2. Accessibility
3.6.3. Affordability
3.6.4. Quality and Safety
3.6.5. Acceptability, Dignity and Privacy
3.7. Menstrual Hygiene Management–MHM
4. Discussion
4.1. The Current State of WASH Conditions in Schools in LMICs
4.2. The Implications for COVID-19 Pandemic on WASH in Schools
5. Limitations of the Review
6. Conclusions and Future Research
- Assess what is the situation of WASH conditions in schools in Latin America;
- Describe the differences of WASH conditions in schools in LMICs according to the locality (rural vs. urban) and model of management (public vs. private);
- Identify what WASH interventions have been implemented in schools during the ongoing COVID-19 pandemic in order to provide safe reopening and how they satisfy the normative contents of HRTWS;
- Explore emergent themes in the school environment, such as MHM, gender discrimination and inequalities, and disability-friendly WASH services;
- Discuss how to improve standardization across studies (e.g., enhance the use of the JMP service ladders and definitions) in order to allow the comparison of WASH services in different locations;
- Investigate how to integrate the normative contents of the HRTWS to the JMP service ladders and definitions.
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO-World Health Organization. Timeline: WHO’s COVID-19 Response. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/interactive-timeline (accessed on 30 March 2021).
- WHO-World Health Organization. WHO Coronavirus (COVID-19) Dashboard. Available online: https://covid19.who.int (accessed on 30 March 2021).
- Mansourian, M.; Ghandi, Y.; Habibi, D.; Mehrabi, S. COVID-19 infection in children: A systematic review and meta-analysis of clinical features and laboratory findings. Arch. Pédiatrie 2021, 28, 242–248. [Google Scholar] [CrossRef] [PubMed]
- Mania, A.; Mazur-Melewska, K.; Lubarski, K.; Kuczma-Napierała, J.; Mazurek, J.; Jończyk-Potoczna, K.; Służewski, W.; Figlerowicz, M. Wide spectrum of clinical picture of COVID-19 in children-from mild to severe disease. J. Infect. Public Health 2020, 14, 374–379. [Google Scholar] [CrossRef] [PubMed]
- Brookman, S.; Cook, J.; Zucherman, M.; Broughton, S.; Harman, K.; Gupta, A. Effect of the new SARS-CoV-2 variant B.1.1.7 on children and young people. Lancet Child Adolesc. Health 2021, 5, e9–e10. [Google Scholar] [CrossRef]
- Bhopal, S.S.; Bagaria, J.; Olabi, B.; Bhopal, R. Children and young people remain at low risk of COVID-19 mortality. Lancet Child Adolesc. Health 2021, 5, e12–e13. [Google Scholar] [CrossRef]
- Verdoni, L.; Mazza, A.; Gervasoni, A.; Martelli, L.; Ruggeri, M.; Ciuffreda, M.; Bonanomi, E.; D’Antiga, L. An outbreak of severe Kawasaki-like disease at the Italian epicentre of the SARS-CoV-2 epidemic: An observational cohort study. Lancet 2020, 395, 1771–1778. [Google Scholar] [CrossRef]
- Godfred-cato, S.; Bryant, B.; Leung, J.; Oster, M.E.; Conklin, L.; Abrams, J.; Roguski, K.; Wallace, B.; Prezzato, E.; Koumans, E. COVID-19–Related Multisystem Inflammatory Syndrome in Children. AAP Grand Rounds 2020, 44, 30. [Google Scholar] [CrossRef]
- Okarska-Napierała, M.; Ludwikowska, K.; Szenborn, L.; Dudek, N.; Mania, A.; Buda, P.; Książyk, J.; Mazur-Malewska, K.; Figlerowicz, M.; Szczukocki, M.; et al. Pediatric Inflammatory Multisystem Syndrome (PIMS) Did Occur in Poland during Months with Low COVID-19 Prevalence, Preliminary Results of a Nationwide Register. J. Clin. Med. 2020, 9, 3386. [Google Scholar] [CrossRef]
- Dufort, E.M.; Koumans, E.H.; Chow, E.J.; Rosenthal, E.M.; Muse, A.; Rowlands, J.; Barranco, M.A.; Maxted, A.M.; Rosenberg, E.S.; Easton, D.; et al. Multisystem Inflammatory Syndrome in Children in New York State. N. Engl. J. Med. 2020, 383, 347–358. [Google Scholar] [CrossRef]
- Bhuiyan, M.U.; Stiboy, E.; Hassan, M.Z.; Chan, M.; Islam, M.S.; Haider, N.; Jaffe, A.; Homaira, N. Epidemiology of COVID-19 infection in young children under five years: A systematic review and meta-analysis. Vaccine 2021, 39, 667–677. [Google Scholar] [CrossRef]
- Fantini, M.P.; Reno, C.; Biserni, G.B.; Savoia, E.; Lanari, M. COVID-19 and the re-opening of schools: A policy maker’ s dilemma. Ital. J. Pediatr. 2020, 46, 1–3. [Google Scholar] [CrossRef]
- Viner, R.M.; Russell, S.J.; Croker, H.; Packer, J.; Ward, J.; Stansfield, C.; Mytton, O.; Bonell, C.; Booy, R. School closure and management practices during coronavirus outbreaks including COVID-19: A rapid systematic review. Lancet Child Adolesc. Health 2020, 4, 397–404. [Google Scholar] [CrossRef]
- United Nations Children’s Fund (UNICEF). COVID-19 and Children. UNICEF Data Hub. Available online: https://data.unicef.org/covid-19-and-children/ (accessed on 30 March 2021).
- United Nations Educational; Scientific and Cultural Organization (UNESCO). Adverse Consequences of School Closures. Available online: https://en.unesco.org/covid19/educationresponse/consequences (accessed on 30 March 2021).
- Esposito, S.; Principi, N. School Closure During the Coronavirus Disease 2019 (COVID-19) Pandemic an Effective Intervention at the Global Level? Clin. Infect. Dis. 2020, 71, 2027–2034. [Google Scholar] [CrossRef]
- Benzian, H.; Buijs, G.; Kolbe, L.; McCall, D. Checklist to Support Schools Re-Opening and Preparation for COVID-19 Resurgences or Similar public Health Crises; WHO: Geneva, Switzerland, 2020; pp. 1–20. [Google Scholar]
- Wu, Y.; Guo, C.; Tang, L.; Hong, Z.; Zhou, J.; Dong, X.; Yin, H.; Xiao, Q.; Tang, Y.; Qu, X.; et al. Prolonged presence of SARS-CoV-2 viral RNA in faecal samples. Lancet Gastroenterol. Hepatol 2020, 5, 434–435. [Google Scholar] [CrossRef]
- Chen, Y.; Chen, L.; Deng, Q.; Zhang, G.; Wu, K.; Ni, L.; Yang, Y.; Liu, B.; Wang, W.; Wei, C.; et al. The presence of SARS-CoV-2 RNA in the feces of COVID-19 patients. J. Med. Virol. 2020, 92, 833–840. [Google Scholar] [CrossRef]
- Medema, G.; Heijnen, L.; Elsinga, G.; Italiaander, R.; Brouwer, A. Presence of SARS-Coronavirus-2 in sewage. Environ. Sci. Technol. Lett. 2020, 7, 511–516. [Google Scholar] [CrossRef]
- Chavarria-Miró, G.; Anfruns-Estrada, E.; Guix, S.; Paraira, M.; Galofré, B.; Sánchez, G.; Pintó, R.M.; Bosch, A. Sentinel surveillance of SARS-CoV-2 in wastewater anticipates the occurrence of COVID-19 cases. MedRxiv 2020. [Google Scholar] [CrossRef]
- Fongaro, G.; Stoco, P.H.; Souza, D.S.M.; Grisard, E.C.; Magri, M.E.; Rogovski, P.; Schörner, M.A.; Barazzetti, F.H.; Christoff, A.P.; de Oliveira, L.F.V.; et al. SARS-CoV-2 in human sewage in Santa Catalina, Brazil, November 2019. Sci. Total Environ. 2021, 778, 146198. [Google Scholar] [CrossRef]
- Camilo, L.; Oliveira, D.; Torres-franco, A.F.; Coelho, B.; Senra, B.; Santos, S.; Azevedo, E.; Costa, M.S.; Tulius, M.; Reis, P.; et al. Viability of SARS-CoV-2 in river water and wastewater at different temperatures and solids content. Water Res. 2021, 195, 117002. [Google Scholar]
- Jasper, C.; Le, T.-T.; Bartram, J. Water and Sanitation in Schools: A Systematic Review of the Health and Educational Outcomes. Int. J. Environ. Res. Public Health 2012, 9, 2772–2787. [Google Scholar] [CrossRef]
- Freeman, M.C.; Greene, L.E.; Dreibelbis, R.; Saboori, S.; Muga, R.; Brumback, B.; Rheingans, R. Assessing the impact of a school-based water treatment, hygiene and sanitation programme on pupil absence in Nyanza Province, Kenya: A cluster-randomized trial. Trop. Med. Int. Health 2012, 17, 380–391. [Google Scholar] [CrossRef]
- Bar-David, Y.; Urkin, J.; Kozminsky, E. The effect of voluntary dehydration on cognitive functions of elementary school children. Acta Paediatr. Int. J. Paediatr. 2005, 94, 1667–1673. [Google Scholar] [CrossRef] [PubMed]
- Agol, D.; Harvey, P. Gender differences related to WASH in schools and educational efficiency. Water Altern. 2018, 11, 284–296. [Google Scholar]
- Connolly, S.; Sommer, M. Cambodian girls’ recommendations for facilitating menstrual hygiene management in school. J. Water Sanit. Hyg. Dev. 2013, 3, 612–622. [Google Scholar] [CrossRef]
- Sommer, M.; Ackatia-Armah, N.; Connolly, S.; Smiles, D. A comparison of the menstruation and education experiences of girls in Tanzania, Ghana, Cambodia and Ethiopia. Comp. J. Comp. Int. Educ. 2015, 45, 589–609. [Google Scholar] [CrossRef]
- Anthonj, C.; Githinji, S.; Höser, C.; Stein, A.; Blanford, J.; Grossi, V. Kenyan school book knowledge for water, sanitation, hygiene and health education interventions: Disconnect, integration or opportunities? Int. J. Hyg. Environ. Health 2021, 235, 113756. [Google Scholar] [CrossRef]
- McMichael, C. Water, sanitation and hygiene (WASH) in schools in low-income countries: A review of evidence of impact. Int. J. Environ. Res. Public Health 2019, 16, 359. [Google Scholar] [CrossRef]
- United Nations (UN). General Assembly Resolution 64/292, the Human Right to Water and Sanitation, A/RES/64/292; United Nations General Assembly: Geneva, Switzerland, 2010. [Google Scholar]
- United Nations (UN). Realizing the Human Rights to Water and Sanitation: A Handbook by the UN Special Rapporteur Catarina de Albuquerque; United Nations: Lisbon, Portugal, 2014. [Google Scholar]
- United Nations Children’s Fund (UNICEF); World Health Organization (WHO). Progress on Drinking Water, Sanitation and Hygiene in Schools: Special Focus on COVID-19. Available online: https://www.unicef.org/media/74011/file/Progress-on-drinking-water-sanitation-and-hygiene-in-schools-focus-on%20covid-19.pdf (accessed on 30 March 2021).
- Kshnaratne, S.; Lm, P.; Coenen, M.; Ge, K.; Klinger, C.; Kratzer, S.; Littlecott, H.; Movsisyan, A.; Je, R.; Rehfuess, E.; et al. Measures implemented in the school setting to contain the COVID-19 pandemic: A rapid scoping review. Cochrane Database Syst. Rev. 2020. Available online: http://www.cochranelibrary.com (accessed on 22 July 2021). [CrossRef]
- Ezeonu, C.; Uneke, C.; Ezeonu, P. A rapid review of the reopening of schools in this COVID-19 pandemic? How ready are we in Nigeria? Niger. J. Med. 2021, 30, 8. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Int. J. Surg. 2021, 88, 105906. [Google Scholar] [CrossRef]
- Rayyan. Intelligent Systematic Review. Available online: https://www.rayyan.ai/ (accessed on 27 May 2021).
- United Nations Children’s Fund (UNICEF) and World Health Organization (WHO). Consultation on Draft Long List of Goal, Target and Indicator Options for Future Global Monitoring of Water, Sanitation and Hygiene. Available online: https://washdata.org/sites/default/files/documents/reports/2017-06/JMP-2012-post2015-consultation.pdf (accessed on 30 March 2021).
- Hong, Q.N.; Pluye, P.; Fabregues, S.; Bartlett, G.; Boardman, F.; Cargo, M.; Dagenais, P.; Gagnon, M.-P.; Griffiths, F.; Nicolau, B.; et al. Mixed Methods Apprisal Tool (MMAT) Version 2018. Available online: http://mixedmethodsappraisaltoolpublic.pbworks.com/w/file/fetch/127916259/MMAT_2018_criteria-manual_2018-08-01_ENG.pdf (accessed on 31 July 2021).
- Ahmed, J.; Wong, L.P.; Chua, Y.P.; Channa, N.; Mahar, R.B.; Yasmin, A.; VanDerslice, J.A.; Garn, J.V. Quantitative Microbial Risk Assessment of Drinking Water Quality to Predict the Risk of Waterborne Diseases in Primary-School Children. Int. J. Environ. Res. Public Health 2020, 17, 2774. [Google Scholar] [CrossRef]
- Alam, M.-U.; Luby, S.P.; Halder, A.K.; Islam, K.; Opel, A.; Shoab, A.K.; Ghosh, P.K.; Rahman, M.; Mahon, T.; Unicomb, L. Menstrual hygiene management among Bangladeshi adolescent schoolgirls and risk factors affecting school absence: Results from a cross-sectional survey. BMJ Open 2017, 7, e015508. [Google Scholar] [CrossRef] [PubMed]
- Alexander, K.T.; Oduor, C.; Nyothach, E.; Laserson, K.F.; Amek, N.; Eleveld, A.; Mason, L.; Rheingans, R.; Beynon, C.; Mohammed, A.; et al. Water, sanitation and hygiene conditions in kenyan rural schools: Are schools meeting the needs of menstruating girls? Water 2014, 6, 1453–1466. [Google Scholar] [CrossRef]
- Antwi-Agyei, P.; Mwakitalima, A.; Seleman, A.; Tenu, F.; Kuiwite, T.; Kiberiti, S.; Roma, E. Water, sanitation and hygiene (WASH) in schools: Results from a process evaluation of the national sanitation campaign in Tanzania. J. Water Sanit. Hyg. Dev. 2017, 7, 140–150. [Google Scholar] [CrossRef]
- Aschale, A.; Adane, M.; Getachew, M.; Faris, K.; Gebretsadik, D.; Sisay, T.; Dewau, R.; Chanie, M.G.; Muche, A.; Zerga, A.A.; et al. Water, sanitation, and hygiene conditions and prevalence of intestinal parasitosis among primary school children in Dessie City, Ethiopia. PLoS ONE 2021, 16, e0245463. [Google Scholar] [CrossRef] [PubMed]
- Assefa, M.; Kumie, A. Assessment of factors influencing hygiene behaviour among school children in Mereb-Leke District, Northern Ethiopia: A cross-sectional study. BMC Public Health 2014, 14, 1000. [Google Scholar] [CrossRef] [PubMed]
- Babalobi, B. Water, sanitation and hygiene practices among primary-school children in Lagos: A case study of the Makoko slum community. Water Int. 2013, 38, 921–929. [Google Scholar] [CrossRef]
- Bergenfeld, I.; Jackson, E.C.; Yount, K.M. Creation of the gender-equitable school index for secondary schools using principal components analysis. Int. Health 2021, 13, 205–207. [Google Scholar] [CrossRef]
- Boosey, R.; Prestwich, G.; Deave, T. Menstrual hygiene management amongst schoolgirls in the Rukungiri district of Uganda and the impact on their education: A cross-sectional study. Pan Afr. Med. 2014, 19, 1–13. [Google Scholar] [CrossRef]
- Bowen, A.; Ma, H.; Ou, J.; Billhimer, W.; Long, T.; Mintz, E.; Hoekstra, R.M.; Luby, S. A cluster-randomized controlled trial evaluating the effect of a handwashing-promotion program in Chinese primary schools. Am. J. Trop. Med. Hyg. 2007, 76, 1166–1173. [Google Scholar] [CrossRef]
- Bulto, G.A. Knowledge on menstruation and practice of menstrual hygiene management among school adolescent girls in central ethiopia: A cross-sectional study. Risk Manag. Healthc. Policy 2021, 14, 911–923. [Google Scholar] [CrossRef]
- Chatterley, C.; Linden, K.G.; Javernick-Will, A. Identifying pathways to continued maintenance of school sanitation in Belize. J. Water Sanit. Hyg. Dev. 2013, 3, 411–422. [Google Scholar] [CrossRef]
- Chatterley, C.; Javernick-Will, A.; Linden, K.G.; Alam, K.; Bottinelli, L.; Venkatesh, M. A qualitative comparative analysis of well-managed school sanitation in Bangladesh. BMC Public Health 2014, 14, 6. [Google Scholar] [CrossRef] [PubMed]
- Chinyama, J.; Chipungu, J.; Rudd, C.; Mwale, M.; Verstraete, L.; Sikamo, C.; Mutale, W.; Chilengi, R.; Sharma, A. Menstrual hygiene management in rural schools of Zambia: A descriptive study of knowledge, experiences and challenges faced by schoolgirls. BMC Public Health 2019, 19, 16. [Google Scholar] [CrossRef]
- Chung, P.L.; Chung, C.Y.; Liao, S.W.; Miaw, C.L. Assessment of the school drinking water supply and the water quality in Pingtung County, Taiwan. Environ. Monit. Assess. 2009, 159, 207–216. [Google Scholar] [CrossRef] [PubMed]
- Crofts, T.; Fisher, J. Menstrual hygiene in Ugandan schools: An investigation of low-cost sanitary pads. J. Water Sanit. Hyg. Dev. 2012, 2, 50–58. [Google Scholar] [CrossRef]
- Cronk, R.; Guo, A.; Fleming, L.; Bartram, J. Factors associated with water quality, sanitation, and hygiene in rural schools in 14 low- and middle-income countries. Sci. Total Environ. 2021, 761, 144226. [Google Scholar] [CrossRef] [PubMed]
- Degefu Birhane, A.; Kaba Serbessa, M.; Tilahun Degfie, T. Menstrual hygiene management: A study of adolescent schoolgirls in sebeta town, oromia region, Ethiopia. Glob. Drugs Ther. 2019, 4, 1–8. [Google Scholar] [CrossRef][Green Version]
- Devkota, G.P.; Bastien, S.; Jenssen, P.D.; Pandey, M.K.; Devkota, B.; Maharjan, S.K. Immediate influences of hygiene education sessions on handwashing behaviors of selected nepali students. J. Water Sanit. Hyg. Dev. 2020, 10, 979–985. [Google Scholar] [CrossRef]
- Dube, B.; January, J. Factors leading to poor water sanitation hygiene among primary school going children in Chitungwiza. J. Public Health Afr. 2012, 3, 25–28. [Google Scholar] [CrossRef]
- Ebong, R.D. Environmental health knowledge and practice survey among secondary schoolchildren in Zaria, Nigeria. Environ. Health Perspect. 1994, 102, 310–312. [Google Scholar] [CrossRef]
- Egbinola, C.N.; Amanambu, A.C. Water supply, sanitation and hygiene education in secondary schools in Ibadan, Nigeria. Bull. Geogr. Socio Econ. 2015, 29, 31–46. [Google Scholar] [CrossRef]
- Ekpo, U.F.; Odoemene, S.N.; Mafiana, C.F.; Sam-Wobo, S.O. Helminthiasis and hygiene conditions of schools in Ikenne, Ogun State, Nigeria. PLoS Negl. Trop. Dis. 2008, 2, e146. [Google Scholar] [CrossRef] [PubMed]
- Erhard, L.; Degabriele, J.; Naughton, D.; Freeman, M.C. Policy and provision of WASH in schools for children with disabilities: A case study in Malawi and Uganda. Glob. Public Health 2013, 8, 1000–1013. [Google Scholar] [CrossRef] [PubMed]
- Ezeonu, C.T.; Anyansi, M.N. Environmental health assessment of primary schools in southeastern Nigeria: Implication for a healthy school environment in developing countries. World Health Popul. 2010, 12, 18–22. [Google Scholar] [CrossRef]
- Freeman, M.C.; Clasen, T.; Dreibelbis, R.; Saboori, S.; Greene, L.E.; Brumback, B.; Muga, R.; Rheingans, R. The impact of a school-based water supply and treatment, hygiene, and sanitation programme on pupil diarrhoea: A cluster-randomized trial. Epidemiol. Infect. 2014, 142, 340–351. [Google Scholar] [CrossRef]
- Grant, M.; Lloyd, C.; Mensch, B. Menstruation and school absenteeism: Evidence from rural Malawi. Comp. Educ. Rev. 2013, 57, 260–284. [Google Scholar] [CrossRef]
- Grimes, J.E.T.; Tadesse, G.; Gardiner, I.A.; Yard, E.; Wuletaw, Y.; Templeton, M.R.; Harrison, W.E.; Drake, L.J. Sanitation, hookworm, anemia, stunting, and wasting in primary school children in southern Ethiopia: Baseline results from a study in 30 schools. PLoS Negl. Trop. Dis. 2017, 11, e0005948. [Google Scholar] [CrossRef]
- Hassen, S.; Abera, K. The status of school sanitation facilities in some selected primary and secondary schools in Dessie City Administration, South Wello Zone, Amhara Region. Ethiop. J. Health Dev. 2015, 27, 80–84. [Google Scholar]
- Jahan, F.; Nuruzzaman, M.; Sultana, F.; Mahfuz, M.T.; Rahman, M.; Akhand, F.; Luby, S.P.; Unicomb, L.; Winch, P.J. Piloting an acceptable and feasible menstrual hygiene products disposal system in urban and rural schools in Bangladesh. BMC Public Health 2020, 20, 1366. [Google Scholar] [CrossRef]
- Jordanova, T.; Cronk, R.; Obando, W.; Medina, O.Z.; Kinoshita, R.; Bartram, J. Water, sanitation, and hygiene in schools in low socio-economic regions in Nicaragua: A cross-sectional survey. Int. J. Environ. Res. Public Health 2015, 12, 6197–6217. [Google Scholar] [CrossRef]
- Karon, A.J.; Cronin, A.A.; Cronk, R.; Hendrawan, R. Improving water, sanitation, and hygiene in schools in Indonesia: A cross-sectional assessment on sustaining infrastructural and behavioral interventions. Int. J. Hyg. Environ. Health 2017, 220, 539–550. [Google Scholar] [CrossRef] [PubMed]
- Korir, E.; Okwara, F.N.; Okumbe, G. Menstrual hygiene management practices among primary school girls from a pastoralist community in Kenya: A cross sectional survey. Pan Afr. Med. J. 2018, 31, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Lang, M.C. Implementation of an evidence-based hand hygiene program in elementary schools in Ghana, as part of a city-to-city partnership between ottawa public health and KEEA health directorate. Fam. Community Health Fam. 2012, 35, 203–211. [Google Scholar] [CrossRef]
- Lopez-Quintero, C.; Freeman, P.; Neumark, Y. Hand washing among school children in Bogotá, Colombia. Am. J. Public Health 2009, 99, 94–101. [Google Scholar] [CrossRef] [PubMed]
- Majra, J.; Gur, A. School environment and sanitation in rural India. J. Glob. Infect. Dis. 2010, 2, 109. [Google Scholar] [CrossRef]
- Mathew, K.; Zachariah, S.; Shordt, K.; Snel, M.; Cairncross, S.; Biran, A.; Schmidt, W.P. The sustainability and impact of school sanitation, water and hygiene education in southern India. Waterlines 2009, 28, 275–292. [Google Scholar] [CrossRef]
- Mbatha, T. Addressing girls’ challenges of water and sanitation in a rural schooling context in Swaziland. Agenda 2011, 25, 35–42. [Google Scholar] [CrossRef]
- Miiro, G.; Rutakumwa, R.; Nakiyingi-Miiro, J.; Nakuya, K.; Musoke, S.; Namakula, J.; Francis, S.; Torondel, B.; Gibson, L.J.; Ross, D.A.; et al. Menstrual health and school absenteeism among adolescent girls in Uganda (MENISCUS): A feasibility study. BMC Women’s Health 2018, 18, 4. [Google Scholar] [CrossRef]
- Mirassou-Wolf, T.; Chanthou, V.; Grossman, K.G.; DeCoursey, M.; Ryan, P.E. Baseline Assessment of Water, Sanitation, and Hygiene (Wash) Infrastructure and Practices in Government Schools of the Trapeang Chour Commune, Cambodia. J. Environ. Health Sci. 2017, 3, 1–8. [Google Scholar] [CrossRef]
- Mogaji, H.O.; Adeaga, D.O.; Yusuff, Q.A.; Johnson, M.E.; Ekpo, U.F. Preliminary evaluation of UNICEF’s assisted water, sanitation and hygiene (WASH) programme using interview guides and spot checks in Ogun State, Nigeria. Annu. Res. Rev. Biol. 2016, 9, 1–7. [Google Scholar] [CrossRef]
- Mohammed, S.; Larsen-Reindorf, R.E. Menstrual knowledge, sociocultural restrictions, and barriers to menstrual hygiene management in Ghana: Evidence from a multi-method survey among adolescent schoolgirls and schoolboys. PLoS ONE 2020, 15, e0241106. [Google Scholar] [CrossRef] [PubMed]
- Montgomery, P.; Hennegan, J.; Dolan, C.; Wu, M.; Steinfield, L.; Scott, L. Menstruation and the Cycle of Poverty: A Cluster Quasi-Randomised Control Trial of Sanitary Pad and Puberty Education Provision in Uganda. PLoS ONE 2016, 11, e0166122. [Google Scholar] [CrossRef] [PubMed]
- Morgan, C.; Bowling, M.; Bartram, J.; Lyn Kayser, G. Water, sanitation, and hygiene in schools: Status and implications of low coverage in Ethiopia, Kenya, Mozambique, Rwanda, Uganda, and Zambia. Int. J. Hyg. Environ. Health 2017, 220, 950–959. [Google Scholar] [CrossRef] [PubMed]
- Mwanri, L.; Worsley, A.; Masika, J. School and anaemia prevention: Current reality and opportunities—A Tanzanian case study. Health Promot. Int. 2001, 16, 321–331. [Google Scholar] [CrossRef] [PubMed]
- Nazliansyah, N.; Wichaikull, S.; Wetasin, K. Factors Affecting Hand Washing Practice Among Elementary Schools Students in Indonesia. Belitung Nurs. J. 2016, 2, 58–64. [Google Scholar] [CrossRef]
- Ngwenya, B.N.; Thakadu, O.T.; Phaladze, N.A.; Bolaane, B. Access to water and sanitation facilities in primary schools: A neglected educational crisis in Ngamiland district in Botswana. Phys. Chem. Earth 2018, 105, 231–238. [Google Scholar] [CrossRef]
- Ofovwe, G.; Ofili, A. Knowledge, attitude and practice of school health programme among head teachers of primary schools in Egor local government area of Edo state, Nigeria. Ann. Afr. Med. 2007, 6, 99. [Google Scholar] [CrossRef]
- Parker, A.H.; Smith, J.A.; Verdemato, T.; Cooke, J.; Webster, J.; Carter, R.C. Menstrual management: A neglected aspect of hygiene interventions. Disaster Prev. Manag. 2014, 23, 437–454. [Google Scholar] [CrossRef]
- Rai, P.; Sah, R.B.; Rijal, R.; Pokharel, P. Neglected scenario of sanitation in schools of Sunsari district of Nepal: Critical sphere for public health consideration. Health Renaiss. 2017, 13, 114–124. [Google Scholar] [CrossRef]
- Saboori, S.; Mwaki, A.; Porter, S.E.; Okech, B.; Freeman, M.C.; Rheingans, R.D. Sustaining school hand washing and water treatment programmes: Lessons learned and to be learned. Waterlines 2011, 30, 298–310. [Google Scholar] [CrossRef]
- Sangalang, S.O.; Prado, N.O.; Lemence, A.L.G.; Cayetano, M.G.; Lu, J.L.D.; Valencia, J.C.; Kistemann, T.; Borgemeister, C. Diarrhea, Helminth Infection, Dehydration, and Malnutrition Associated with Water, Sanitation, and Hygiene Facilities and Poor Handwashing in Schools in Metro Manila, Philippines: A Cross-Sectional Study. MedRxiv 2020. [Google Scholar] [CrossRef]
- Shallo, S.A.; Willi, W.; Abubeker, A. Factors affecting menstrual hygiene management practice among school adolescents in Ambo, western Ethiopia, 2018: A cross-sectional mixed-method study. Risk Manag. Healthc. Policy 2020, 13, 1579–1587. [Google Scholar] [CrossRef] [PubMed]
- Shehmolo, M.; Gari, T.; Jember Tesfaye, D.; Boti, N.; Oumer, B. Magnitude and Factors Associated with Hygiene Practice Among Primary School Children in Mareko District, Southern Ethiopia: A Cross-Sectional Study. J. Multidiscip. Healthc. 2021, 14, 311–320. [Google Scholar] [CrossRef]
- Shrestha, A.; Sharma, S.; Gerold, J.; Erismann, S.; Sagar, S.; Koju, R.; Schindler, C.; Odermatt, P.; Utzinger, J.; Cissé, G. Water quality, sanitation, and hygiene conditions in schools and households in dolakha and ramechhap districts, Nepal: Results from a cross-sectional survey. Int. J. Environ. Res. Public Health 2017, 14, 89. [Google Scholar] [CrossRef] [PubMed]
- Sibiya, J.E.; Gumbo, J.R. Knowledge, attitude and practices (KAP) survey on water, sanitation and hygiene in selected schools in Vhembe district, Limpopo, South Africa. Int. J. Environ. Res. Public Health 2013, 10, 2282. [Google Scholar] [CrossRef] [PubMed]
- Sommer, M. Structural factors influencing menstruating school girls’ health and well-being in Tanzania. Comp. J. Comp. Int. Educ. 2013, 43, 323–345. [Google Scholar] [CrossRef]
- Uduku, O. Designing schools for quality: An international, case study-based review. Int. J. Educ. Dev. 2015, 44, 56–64. [Google Scholar] [CrossRef]
- Vally, H.; McMichael, C.; Doherty, C.; Li, X.; Guevarra, G.; Tobias, P. The impact of a school-based water, sanitation and hygiene intervention on knowledge, practices, and diarrhoea rates in the Philippines. Int. J. Environ. Res. Public Health 2019, 16, 4056. [Google Scholar] [CrossRef]
- Wichaidit, W.; Steinacher, R.; Okal, J.A.; Whinnery, J.; Null, C.; Kordas, K.; Yu, J.; Pickering, A.J.; Ram, P.K. Effect of an equipment-behavior change intervention on handwashing behavior among primary school children in Kenya: The Povu Poa school pilot study. BMC Public Health 2019, 19, 647. [Google Scholar] [CrossRef]
- Xuan, L.T.T.; Hoat, L.; Rheinländer, T.; Dalsgaard, A.; Konradsen, F. Sanitation behavior among schoolchildren in a multi-ethnic area of Northern rural Vietnam. BMC Public Health 2012, 12, 140. [Google Scholar] [CrossRef]
- Zaunda, H.; Holm, R.H.; Itimu-Phiri, A.; Malota, M.; White, S. A qualitative assessment of disability friendly water and sanitation facilities in primary schools, Rumphi, Malawi. Dev. South. Afr. 2018, 35, 760–773. [Google Scholar] [CrossRef]
- Byford, T. Water, sanitation and hygiene standards for schools in low-cost settings. Int. J. Environ. Stud. 2014, 71, 409–410. [Google Scholar] [CrossRef]
- Cronk, R.; Slaymaker, T.; Bartram, J. Monitoring drinking water, sanitation, and hygiene in non-household settings: Priorities for policy and practice. Int. J. Hyg. Environ. Health 2015, 218, 694–703. [Google Scholar] [CrossRef] [PubMed]
- Wright, J.; Gundry, S.; Conroy, R. Household drinking water in developing countries: A systematic review of microbiological contamination between source and point-of-use. Trop. Med. Int. Health 2004, 9, 106–117. [Google Scholar] [CrossRef] [PubMed]
- Dada, N.; Vannavong, N.; Seidu, R.; Lenhart, A.; Stenström, T.A.; Chareonviriyaphap, T.; Overgaard, H.J. Relationship between Aedes aegypti production and occurrence of Escherichia coli in domestic water storage containers in rural and sub-urban villages in Thailand and Laos. Acta Trop. 2013, 126, 177–185. [Google Scholar] [CrossRef] [PubMed]
- Morgan, C.E.; Bowling, J.M.; Bartram, J.; Kayser, G.L. Attributes of drinking water, sanitation, and hygiene associated with microbiological water quality of stored drinking water in rural schools in Mozambique and Uganda. Int. J. Hyg. Environ. Health 2021, 236, 113804. [Google Scholar] [CrossRef] [PubMed]
- Fadda, R.; Rapinett, G.; Grathwohl, D.; Parisi, M.; Fanari, R.; Calò, C.M.; Schmitt, J. Effects of drinking supplementary water at school on cognitive performance in children. Appetite 2012, 59, 730–737. [Google Scholar] [CrossRef]
- Adan, A. Cognitive performance and dehydration. J. Am. Coll. Nutr. 2012, 31, 71–78. [Google Scholar] [CrossRef]
- Geere, J.A.; Bartram, J.; Bates, L.; Danquah, L.; Evans, B.; Fisher, M.B.; Groce, N.; Majuru, B.; Mokoena, M.M.; Mukhola, M.S.; et al. Carrying water may be a major contributor to disability from musculoskeletal disorders in low income countries: A cross-sectional survey in South Africa, Ghana and Vietnam. J. Glob. Health 2018, 8, 1–14. [Google Scholar] [CrossRef]
- Geere, J.A.L.; Hunter, P.R.; Jagals, P. Domestic water carrying and its implications for health: A review and mixed methods pilot study in Limpopo Province, South Africa. Environ. Health A Glob. Access Sci. Source 2010, 9, 1–13. [Google Scholar] [CrossRef]
- Freeman, M.C.; Snel, M.; Yousif, M.E.F.; Gitahi, S.; Khan, F.; Wachira, S.; Krukkert, I. The usage of urinals in Kenyan schools. Waterlines 2012, 31, 226–239. [Google Scholar] [CrossRef]
- Berger, S.; Kunerl, A.; Wasmuth, S.; Tierno, P.; Wagner, K.; Brügger, J. Menstrual toxic shock syndrome: Case report and systematic review of the literature. Lancet Infect. Dis. 2019, 19, e313–e321. [Google Scholar] [CrossRef]
- Ademas, A.; Adane, M.; Sisay, T.; Kloos, H.; Eneyew, B.; Keleb, A.; Lingerew, M.; Derso, A.; Alemu, K. Does menstrual hygiene management and water, sanitation, and hygiene predict reproductive tract infections among reproductive women in urban areas in Ethiopia? PLoS ONE 2020, 15, e0237696. [Google Scholar] [CrossRef] [PubMed]
- Coswosk, É.D.; Neves-Silva, P.; Modena, C.M.; Heller, L. Having a toilet is not enough: The limitations in fulfilling the human rights to water and sanitation in a municipal school in Bahia, Brazil. BMC Public Health 2019, 19, 137. [Google Scholar] [CrossRef] [PubMed]
- Wada, O.Z.; Oloruntoba, E.O. Safe Reopening of Schools during COVID-19: An Evaluation of Handwash Facilities and Students’ Hand Hygiene Knowledge and Practices. Eur. J. Environ. Public Health 2021, 5, em0072. [Google Scholar]
- Mbakaya, B.C.; Kalembo, F.W.; Zgambo, M. Use, adoption, and effectiveness of tippy-tap handwashing station in promoting hand hygiene practices in resource-limited settings: A systematic review. BMC Public Health 2020, 20, 1005. [Google Scholar] [CrossRef]
- World Health Organisation. WHO Saves Lives: Clean Your Hands in the Context of COVID-19; World Health Organization: Geneva, Switzerland, 2020; pp. 19–20. [Google Scholar]
- Luby, S.P.; Halder, A.K.; Huda, T.; Unicomb, L.; Johnston, R.B. The effect of handwashing at recommended times with water alone and with soap on child diarrhea in rural Bangladesh: An observational study. PLoS Med. 2011, 8, e1001052. [Google Scholar] [CrossRef]
- Burton, M.; Cobb, E.; Donachie, P.; Judah, G.; Curtis, V.; Schmidt, W.P. The effect of handwashing with water or soap on bacterial contamination of hands. Int. J. Environ. Res. Public Health 2011, 8, 97–104. [Google Scholar] [CrossRef]
- Chaudhary, N.K.; Chaudhary, N.; Dahal, M.; Guragain, B.; Rai, S.; Chaudhary, R.; Sachin, K.M.; Lamichhane-Khadka, R.; Bhattarai, A. Fighting the SARS CoV-2 (COVID-19) Pandemic with Soap. Preprints 2020, 60, 1–19. [Google Scholar] [CrossRef]
- Lin, Q.; Lim, J.Y.C.; Xue, K.; Yew, P.Y.M.; Owh, C.; Chee, P.L.; Loh, X.J. Sanitizing agents for virus inactivation and disinfection. View 2020, 1, e16. [Google Scholar] [CrossRef]
- Lee, J.; Jing, J.; Yi, T.P.; Bose, R.J.C.; Mccarthy, J.R.; Tharmalingam, N.; Madheswaran, T. Hand sanitizers: A review on formulation aspects, adverse effects, and regulations. Int. J. Environ. Res. Public Health 2020, 17, 3326. [Google Scholar]
- Santos, C.; Kieszak, S.; Wang, A.; Law, R.; Schier, J.; Wolkin, A. Reported Adverse Health Effects in Children from Ingestion of Alcohol-Based Hand Sanitizers—United States, 2011–2014. MMWR. Morb. Mortal. Wkly. Rep. 2017, 66, 223–226. [Google Scholar] [CrossRef] [PubMed]
- Hanna, S.; Zwi, K.; Tzioumi, D. Morbidity in the COVID-19 era: Ethanol intoxication secondary to hand sanitiser ingestion. J. Paediatr. Child Health 2021, 57, 741–742. [Google Scholar] [CrossRef] [PubMed]
- Roy, A.; Parida, S.P.; Bhatia, V. Role of disinfection and hand hygiene: A COVID-19 perspective. Int. J. Community Med. Public Health 2020, 7, 2845. [Google Scholar] [CrossRef]
- World Health Organization. Water, Sanitation, Hygiene, and Waste Management for SARS-CoV-2, the Virus that Causes COVID-19: Interim Guidance-2; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- Bloomfield, S.F.; Nath, K.J. Use of Ash and Mud for Handwashing in Low Income Communities International Scientific Forum on Home Hygiene (IFH); 2009. Available online: http://www.ehproject.org/PDF/ehkm/ifh-mudash2009.pdf (accessed on 16 February 2022).
- Paludan-Müller, A.S.; Boesen, K.; Klerings, I.; Jørgensen, K.J.; Munkholm, K. Hand cleaning with ash for reducing the spread of viral and bacterial infections: A rapid review. Cochrane Database Syst. Rev. 2020, 4, 1–56. [Google Scholar] [CrossRef]
- Aronson, S.S.; Shope, T.R. Managing Infectious Diseases in Child Care and Schools: A Quick Reference Guide; American Academy of Pediatrics: Itasca, IL, USA, 2008; ISBN 9781610023481. [Google Scholar]
- Curtis, V.A.; Danquah, L.O.; Aunger, R.V. Planned, motivated and habitual hygiene behaviour: An eleven country review. Health Educ. Res. 2009, 24, 655–673. [Google Scholar] [CrossRef]
- Xuan, L.T.T.; Rheinländer, T.; Hoat, L.N.; Dalsgaard, A.; Konradsen, F. Teaching handwashing with soap for schoolchildren in a multi-ethnic population in northern rural Vietnam. Glob. Health Action 2013, 6, 20288. [Google Scholar] [CrossRef][Green Version]
- Asadi-Pooya, A.A.; Nemati, H.; Shahisavandi, M.; Akbari, A.; Emami, A.; Lotfi, M.; Rostamihosseinkhani, M.; Barzegar, Z.; Kabiri, M.; Zeraatpisheh, Z.; et al. Long COVID in children and adolescents. World J. Pediatr. 2021, 17, 495–499. [Google Scholar] [CrossRef]
- Borch, L.; Holm, M.; Knudsen, M.; Ellermann-Eriksen, S.; Hagstroem, S. Long COVID symptoms and duration in SARS-CoV-2 positive children—A nationwide cohort study. Eur. J. Pediatr. 2022, 1–11. [Google Scholar] [CrossRef]
- Mushi, V.; Shao, M. Tailoring of the ongoing water, sanitation and hygiene interventions for prevention and control of COVID-19. Trop. Med. Health 2020, 48, 1–3. [Google Scholar] [CrossRef]
- Bhowmick, G.D.; Dhar, D.; Nath, D.; Ghangrekar, M.M.; Banerjee, R.; Das, S.; Chatterjee, J. Coronavirus disease 2019 (COVID-19) outbreak: Some serious consequences with urban and rural water cycle. Npj Clean Water 2020, 3, 1–8. [Google Scholar] [CrossRef]
- United Nations Children’s Fund (UNICEF); World Health Organization (WHO). JMP. Sanitation. Available online: https://washdata.org/monitoring/sanitation (accessed on 16 February 2022).
- Heller, L.; Mota, C.R.; Greco, D.B. COVID-19 faecal-oral transmission: Are we asking the right questions? Sci. Total Environ. 2020, 729, 138919. [Google Scholar] [CrossRef] [PubMed]
- El Baz, S.; Imziln, B. Can Aerosols and Wastewater be Considered as Potential Transmissional Sources of COVID-19 to Humans? Eur. J. Environ. Public Health 2020, 4, em0047. [Google Scholar] [CrossRef]
- Tian, Y.; Rong, L.; Nian, W.; He, Y. Review article: Gastrointestinal features in COVID-19 and the possibility of faecal transmission. Aliment. Pharmacol. Ther. 2020, 51, 843–851. [Google Scholar] [CrossRef]

| Exclusion Criteria | Sub-Criteria |
|---|---|
| Lack of detailed description of WASH conditions | The theme of the study was right, however, the study did not present a detailed description of the WASH conditions |
| Wrong location | Not in low- and middle-income countries |
| Wrong educational level | Addressed universities, faculties and colleges |
| Wrong setting | Focused on other settings rather than the school environment (e.g., household, healthcare facilities, etc.) |
| Wrong study type | Did not present original research (e.g., systematic reviews, study protocol, short communication, etc.) |
| Grey literature | - |
| Duplication of information | Paper partially contained the same information included in other publications (in case of publications from the same research group) |
| Topics | Description of Extracted Data |
|---|---|
| Publication | Reference (authors and year of publication), year of data collection and location where the study was conducted |
| School | Type of educational institution, number of schools, locality (urban vs. rural) and management model (private vs. public) |
| Thematic addressed | Components of WASH and MHM that were addressed in the studies, and with specific regards to water and sanitation the normative contents of the HRTWS that were mentioned |
| Water | Drinking water-related specifics according to the normative contents of the HMRTWS, schools with improved water source, schools with unimproved or no water source, schools with “unknown” water source, ratio of water tap to school population, reported water shortage, and reported maintenance problems with water supply in the schools |
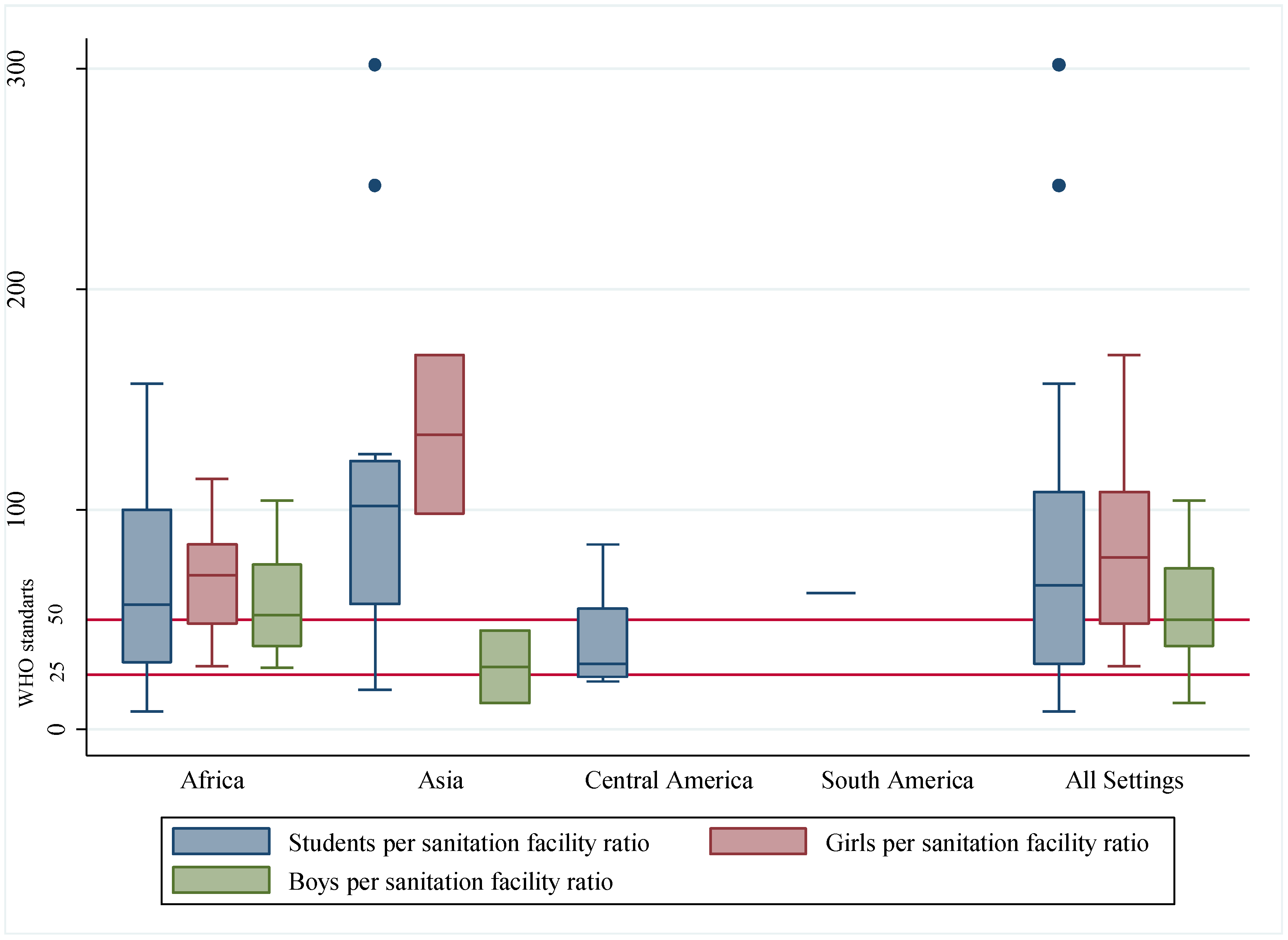
| Sanitation | Sanitation facility-related specifics according to the normative contents of the HMRTWS, schools with improved sanitation facilities, schools with unimproved or no sanitation facilities, schools with “unknown” sanitation facilities, students per sanitation facility ratio, girls per sanitation facility ratio, boys per sanitation facility ratio, reported lack of cleanliness, reported shared facilities between boys and girls, reported shared facilities between students and teachers, reported lack of doors, reported lack of locks and reported lack of roofs |
| Hygiene | Schools with the presence of handwashing facilities, type, number and location of handwashing stations, student-to-handwashing basin ratio, schools with water available for handwashing, schools with the presence of soap, schools with water available in the sanitation facilities, reported lack of handwashing facilities, reported lack of soap, reported lack of water in the sanitation facilities, reported lack of anal cleaning materials/self-cleaning, reported lack of cleaning materials |
| MHM | Reported lack of access to menstrual hygiene materials to absorb or collect menstrual blood, reported lack of disposal facilities for used menstrual materials such as bins and trash cans for sanitary materials disposal, reported lack of room for changing, bathing, or washing sanitary materials |
| Study | Country | Type of School | Number of Schools | Water | Sanitation | Hygiene | MHM | JMP Definitions | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 1 | 2 | 3 | 4 | 5 | |||||||
| Agol and Harvey, 2018 [27] | Zambia | - | 10,000 | X | X | X | X | X | ||||||||
| Ahmed et al., 2020 [41] | Pakistan | Primary | 425 | X | X | X | ||||||||||
| Alam et al., 2017 [42] | Bangladesh | Primary and Secondary | 700 | X | X | X | X | |||||||||
| Alexander et al., 2014 [43] | Kenya | Primary | 62 | X | X | X | X | X | X | X | ||||||
| Antwi-Agyei et al., 2017 [44] | Tanzania | Primary | 70 | X | X | X | X | X | X | X | ||||||
| Aschale et al., 2021 [45] | Ethiopia | Primary | 5 | X | X | X | X | X | X | |||||||
| Assefa and Kumie, 2014 [46] | Ethiopia | Primary | 5 | X | X | X | X | X | X | |||||||
| Babalobi, 2013 [47] | Nigeria | Primary | 4 | X | X | X | X | |||||||||
| Bergenfeld, Jackson and Yount, 2021 [48] | Nepal | Secondary | 159 | X | X | X | X | |||||||||
| Boosey, Prestwich and Deave, 2014 [49] | Uganda | Primary | 6 | X | X | X | X | X | X | X | ||||||
| Bowen et al., 2007 [50] | China | Primary | 87 | X | X | X | ||||||||||
| Bulto, 2021 [51] | Ethiopia | Preparatory and High | 3 | X | ||||||||||||
| Chatterley, Liden and Javernick-Will, 2013 [52] | Belize | Primary School | 15 | X | X | |||||||||||
| Chatterley et al., 2014 [53] | Bangladesh | Primary School | 16 | X | X | X | X | |||||||||
| Chinyama et al., 2019 [54] | Zambia | Primary and Secondary | 6 | X | X | X | X | X | X | |||||||
| Chung et al., 2009 [55] | Taiwan | Above senior high school level and schools under junior high school level | 42 | X | X | |||||||||||
| Connolly and Sommer, 2013 [28] | Cambodia | Secondary | 2 | X | X | X | X | X | X | X | ||||||
| Crofts and Fisher, 2012 [56] | Uganda | Secondary | 18 | X | X | X | X | X | X | |||||||
| Cronk et al., 2021 [57] | Ethiopia, Ghana, Honduras, India, Kenya, Malawi, Mali, Mozambique, Niger, Rwanda, Tanzania, Uganda, Zambia, and Zimbabwe | Primary and Secondary | 2690 | X | X | X | X | X | X | X | X | |||||
| Degefu Birhane, Serbessa and Degfie, 2019 [58] | Ethiopia | Junior | 5 | X | X | X | ||||||||||
| Devkota et al., 2020 [59] | Nepal | - | 1 | X | X | |||||||||||
| Dube and January, 2012 [60] | Zimbabwe | Primary | 4 | X | X | X | X | X | ||||||||
| Ebong, 1994 [61] | Nigeria | Secondary | 1 | X | X | X | X | |||||||||
| Egbinola and Amanambu, 2015 [62] | Nigeria | Secondary | 44 | X | X | X | X | X | X | X | ||||||
| Ekpo et al., 2008 [63] | Nigeria | Primary | 3 | X | X | X | X | X | ||||||||
| Erhard et al., 2013 [64] | Uganda and Malawi | Primary | 41 | X | X | X | X | X | X | X | ||||||
| Ezeonu and Anyansi, 2010 [65] | Nigeria | Primary | 31 | X | X | X | X | X | ||||||||
| Freeman et al., 2014 [66] | Kenya | Primary | 185 | X | X | X | X | X | ||||||||
| Grant, Lloyd and Mensch, 2013 [67] | Malawi | Primary | 59 | X | X | X | X | X | ||||||||
| Grimes et al., 2017 [68] | Ethiopia | Primary | 30 | X | X | X | ||||||||||
| Hassen and Abera, 2015 [69] | Ethiopia | Primary and Secondary | 10 | X | X | X | X | X | ||||||||
| Jahan et al., 2020 [70] | Bangladesh | - | 8 | X | X | X | X | X | X | |||||||
| Jordanova et al., 2015 [71] | Nicaragua | Pre-school, Primary, Secondary, with all levels and unspecific schools | 526 | X | X | X | X | X | X | X | X | |||||
| Karon et al., 2017 [72] | Indonesia | Primary and combined Primary and Junior high | 75 | X | X | X | X | X | X | X | X | X | X | |||
| Korir, Okwara and Okumbe, 2018 [73] | Kenya | Primary | 10 | X | X | X | X | X | X | |||||||
| Lang, 2012 [74] | Ghana | Elementary | 4 | X | X | |||||||||||
| Lopez-Quintero, Freeman and Neumark, 2009 [75] | Colombia | - | 25 | X | X | X | ||||||||||
| Majra and Gur, 2010 [76] | India | Primary, Upper Primary and from Primary to High school level | 20 | X | X | X | X | X | ||||||||
| Mathew et al., 2009 [77] | India | Upper Primary | 300 | X | X | X | X | X | X | X | ||||||
| Mbatha, 2011 [78] | Eswatini | Primary | 2 | X | X | X | X | X | X | |||||||
| Miiro et al., 2018 [79] | Uganda | Secondary | 4 | X | X | X | X | |||||||||
| Mirassou-Wolf et al., 2017 [80] | Cambodia | Primary and Secondary | 8 | X | X | X | X | X | X | |||||||
| Mogaji et al., 2016 [81] | Nigeria | Primary School | 3 | X | X | X | X | X | ||||||||
| Mohammed and Larsen-Reindor, 2020 [82] | Ghana | Junior High | 5 | X | X | X | X | X | X | |||||||
| Montgomery et al., 2016 [83] | Uganda | Primary | 8 | X | X | X | X | X | ||||||||
| Morgan et al., 2017 [84] | Ethiopia, Kenya, Mozambique, Rwanda, Uganda, and Zambia | Primary, Secondary and combined schools | 2270 | X | X | X | X | X | X | X | ||||||
| Mwanri, Worsley and Masika., 2000 [85] | Tanzania | - | 76 | X | X | X | X | |||||||||
| Nazliansyah, Wichaikull and Wetasin, 2016 [86] | Indonesia | Elementary | 11 | X | X | |||||||||||
| Ngwenya et al., 2018 [87] | Botswana | Primary | 3 | X | X | X | X | X | X | |||||||
| Ofovwe and Ofili, 2009 [88] | Nigeria | Primary | 133 | X | X | X | ||||||||||
| Parker et al., 2014 [89] | Uganda | Primary and Secondary | 14 | X | X | X | X | X | X | X | ||||||
| Rai et al., 2017 [90] | Nepal | - | 40 | X | X | X | X | X | ||||||||
| Saboori et al., 2011 [91] | Kenya | Primary | 55 | X | X | X | X | X | ||||||||
| Sangalang et al., 2020 [92] | Philippines | Primary and Secondary | 15 | X | X | X | X | X | X | |||||||
| Shallo, Willi and Abubeker, 2020 [93] | Ethiopia | High | 5 | X | X | X | X | |||||||||
| Shehmolo et al., 2021 [94] | Ethiopia | Primary | 8 | X | X | X | X | X | ||||||||
| Shrestha et al., 2017 [95] | Nepal | Secondary or above | 16 | X | X | X | X | X | X | X | ||||||
| Sibiya and Gumbo, 2013 [96] | South Africa | Secondary | 8 | X | X | X | ||||||||||
| Sommer et al., 2015 [29] | Ghana, Cambodia and Ethiopia | Secondary | 6 | X | X | X | X | X | X | |||||||
| Sommer, 2013 [97] | Tanzania | Primary, Secondary and Boarding schools | 12 | X | X | X | X | X | ||||||||
| Uduku, 2015 [98] | Ghana and South Africa | Primary | 2 | X | X | X | ||||||||||
| Vally et al., 2019 [99] | Philippines | Elementary | 8 | X | X | X | X | X | X | |||||||
| Wichaidit et al., 2019 [100] | Kenya | Primary | 30 | X | X | |||||||||||
| Xuan et al., 2012 [101] | Vietnam | Primary and Secondary | 6 | X | X | X | X | X | X | X | ||||||
| Zaunda et al., 2018 [102] | Malawi | Primary | 10 | X | X | X | X | X | X | X | X | |||||
| Study | Country | |
|---|---|---|
| Chung et al., 2009 [55] | Taiwan | 26% of schools (11 out of 42) had the water samples in non-conformity with the national standards for water quality |
| Sangalang et al., 2020 [92] | Philippines | 20% of schools (3 out of 15) had water that was contaminated by E. coli |
| Shrestha et al., 2017 [95] | Nepal | 75% of school drinking water source samples and 76.9% point-of-use samples (water bottles) collected in 16 schools were contaminated with thermo-tolerant coliforms |
| Ahmed et al., 2020 [41] | Pakistan | Drinking-water samples collected in 425 schools were contaminated with E. coli (49%), Salmonella spp. (54%), V. cholerae (49%) and Shigella (63%), respectively |
| Morgan et al., 2017 [84] | Ethiopia, Kenya, Mozambique, Rwanda, Uganda, and Zambia | No rural schools in Mozambique (n = 198), Zambia (n = 576) and Uganda (n = 251) had very high-risk water quality. Most of the rural schools in all the countries assessed had samples with E. coli counts in the lowest risk category (79% considering only water samples taken from the source and 77% considering water samples taken from stored water). |
| Cronk et al., 2021 [57] | Ethiopia, Ghana, Honduras, India, Kenya, Malawi, Mali, Mozambique, Niger, Rwanda, Tanzania, Uganda, Zambia, and Zimbabwe | Zambia had the highest proportion (80%) of schools with water that conformed with the WHO guideline value for E. coli, while Honduras (22%) and Tanzania (16%) had the lowest compliance |
| Girls per Sanitation Facility | Boys per Sanitation Facility | Students per Sanitation Facility | |
|---|---|---|---|
| Kenya [43,73] | 25:1 | 30:1 | - |
| Philippines [92] | Two toilets for 30–100 female students with an increment of one toilet for each additional 100 female students | 50:2 for 50 or more male students with an increment of one toilet for each additional 100 male students | - |
| Tanzania [97] | 20:1 | - | - |
| Tanzania [44] | 40:1 | 50:1 | - |
| Zambia [27] | - | - | 20:1 |
| Colombia [75] | - | - | 25:1 |
| WHO [44,85,103] | 25:1 | 50:1 | - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Poague, K.I.H.M.; Blanford, J.I.; Anthonj, C. Water, Sanitation and Hygiene in Schools in Low- and Middle-Income Countries: A Systematic Review and Implications for the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2022, 19, 3124. https://doi.org/10.3390/ijerph19053124
Poague KIHM, Blanford JI, Anthonj C. Water, Sanitation and Hygiene in Schools in Low- and Middle-Income Countries: A Systematic Review and Implications for the COVID-19 Pandemic. International Journal of Environmental Research and Public Health. 2022; 19(5):3124. https://doi.org/10.3390/ijerph19053124
Chicago/Turabian StylePoague, Kasandra I. H. M., Justine I. Blanford, and Carmen Anthonj. 2022. "Water, Sanitation and Hygiene in Schools in Low- and Middle-Income Countries: A Systematic Review and Implications for the COVID-19 Pandemic" International Journal of Environmental Research and Public Health 19, no. 5: 3124. https://doi.org/10.3390/ijerph19053124
APA StylePoague, K. I. H. M., Blanford, J. I., & Anthonj, C. (2022). Water, Sanitation and Hygiene in Schools in Low- and Middle-Income Countries: A Systematic Review and Implications for the COVID-19 Pandemic. International Journal of Environmental Research and Public Health, 19(5), 3124. https://doi.org/10.3390/ijerph19053124







