Over Half of Falls Were Associated with Psychotropic Medication Use in Four Nursing Homes in Japan: A Retrospective Cohort Study
Abstract
:1. Introduction
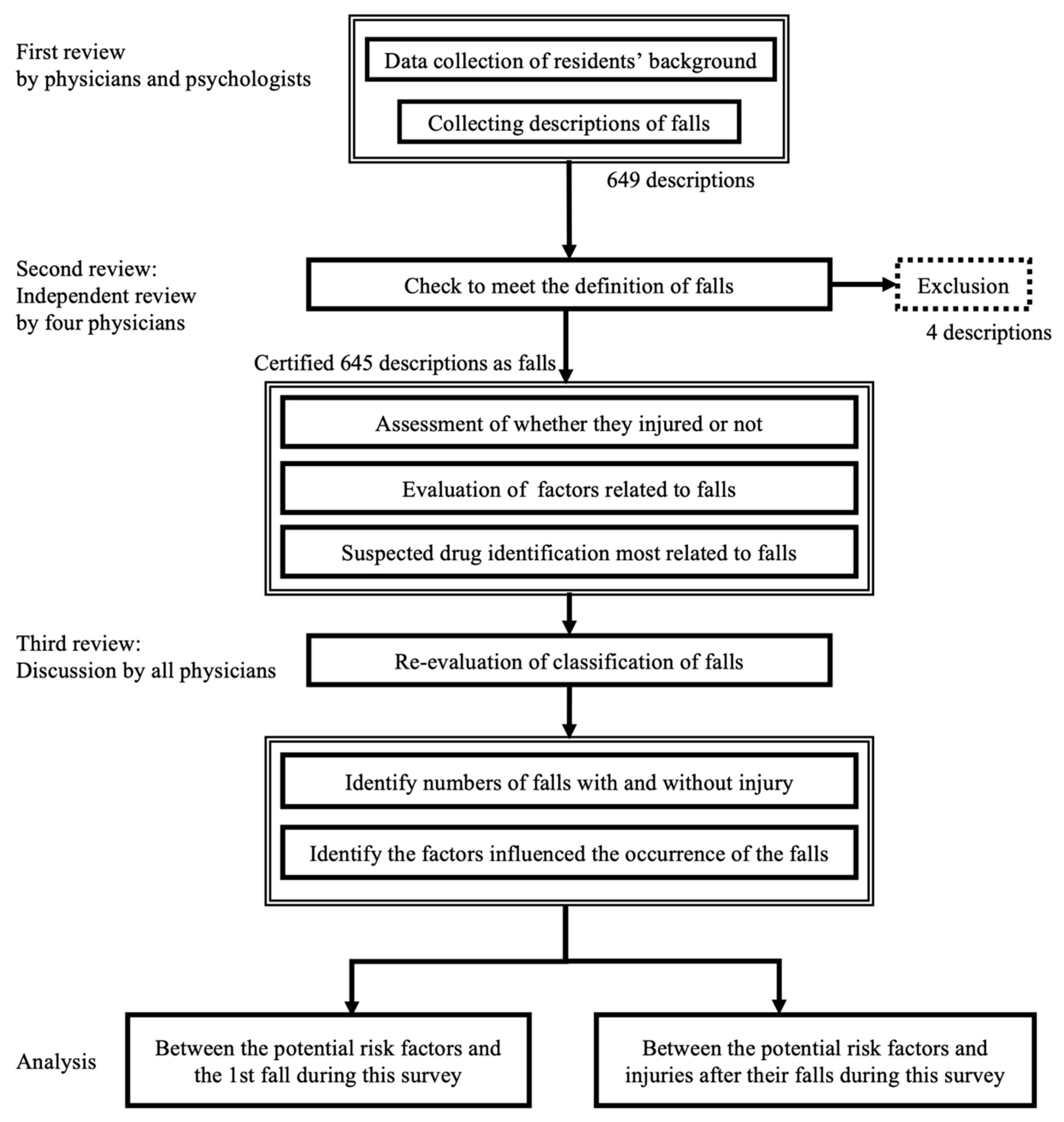
2. Materials and Methods
2.1. Study Design and Resident Population
2.2. Definition
2.3. Data Collection Process
2.4. Data Analysis
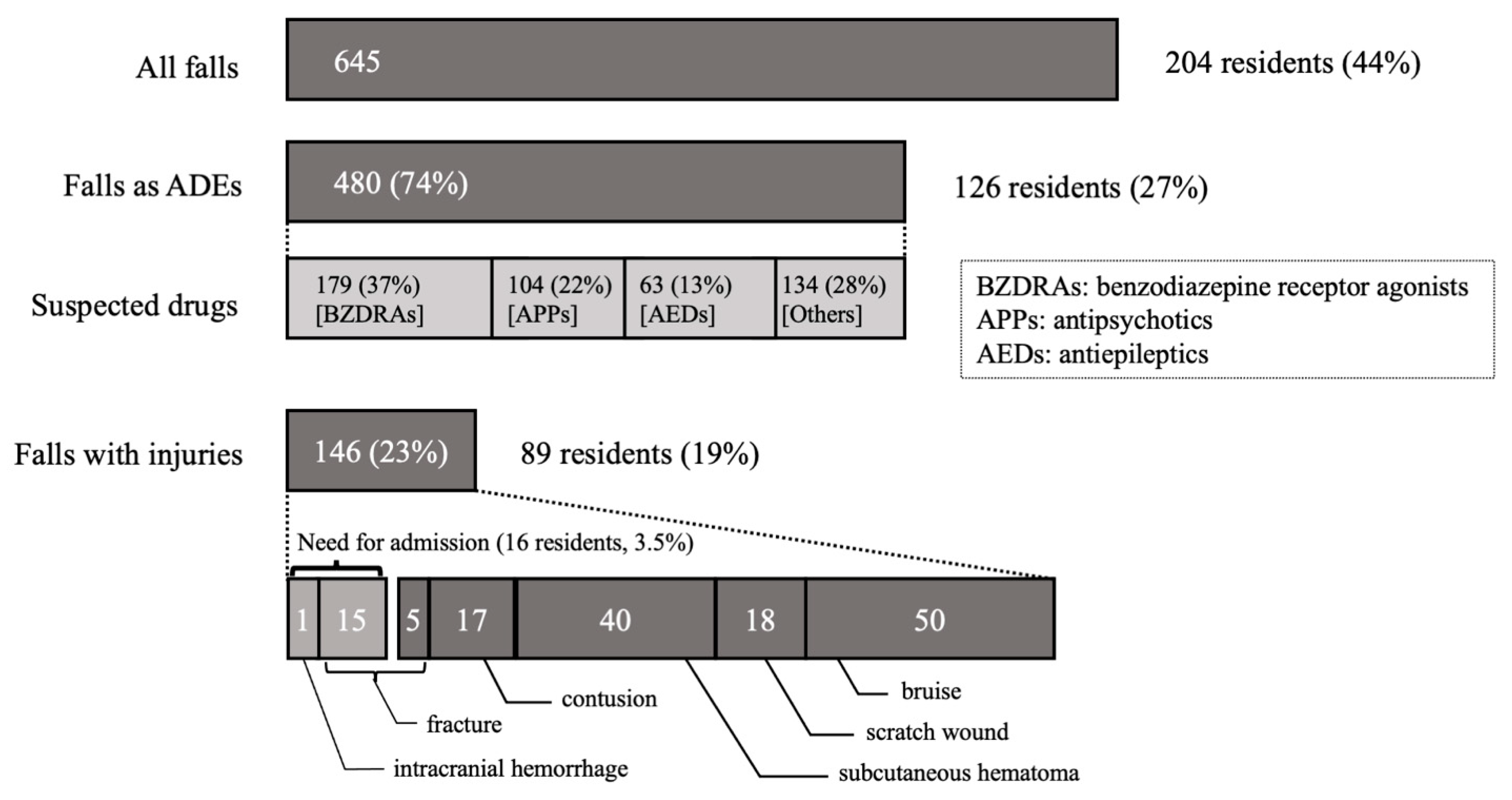
3. Results
3.1. Characteristics of the Study Residents and the Incidence of Falls
3.2. Comparison of the Characteristics and Risk Factors between Fallers and Non-Fallers among All Residents
3.3. Comparison of Characteristics and Risk Factors between Fallers with and without Injuries
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Population Prospects 2019, United Nations. Available online: https://population.un.org/wpp/Download/Standard/Population/ (accessed on 21 May 2021).
- Ministry of Health, Lablur and Welfare. Japan Long-Term Care Insurance Annual Report in 2018. Available online: https://www.mhlw.go.jp/topics/kaigo/osirase/jigyo/18/index.html (accessed on 21 May 2021).
- Ministry of Health, Lablur and Welfare. Japan the Situation Surrounding the Nursing Care Sector. Available online: https://www.mhlw.go.jp/content/12300000/000608284.pdf (accessed on 21 May 2021).
- National Center for Health. Long-Term Care Providers and Services Users in the United States, 2015–2016; Hyattsville, S., Ed.; 2019. Available online: https://stacks.cdc.gov/view/cdc/76253 (accessed on 1 August 2021).
- Thapa, P.B.; Brockman, K.G.; Gideon, P.; Fought, R.L.; Ray, W.A. Injurious Falls in Nonambulatory Nursing Home Residents: A Comparative Study of Circumstances, Incidence, and Risk Factors. J. Am. Geriatr. Soc. 1996, 44, 273–278. [Google Scholar] [CrossRef] [PubMed]
- Moreland, B.; Kakara, R.; Henry, A. Trends in Nonfatal Falls and Fall-Related Injuries among Adults Aged ≥ 65 Years—United States, 2012–2018. Morb. Mortal. Wkly. Rep. 2020, 69, 875–881. [Google Scholar] [CrossRef] [PubMed]
- Jiang, Y.; Xia, Q.; Wang, J.; Zhou, P.; Jiang, S.; Diwan, V.K.; Xu, B. Insomnia, Benzodiazepine Use, and Falls among Residents in Long-Term Care Facilities. Int. J. Environ. Res. Public Health 2019, 16, 4623. [Google Scholar] [CrossRef] [Green Version]
- Berry, S.D.; Placide, S.G.; Mostofsky, E.; Zhang, Y.; Lipsitz, L.A.; Mittleman, M.A.; Kiel, D.P. Antipsychotic and Benzodiazepine Drug Changes Affect Acute Falls Risk Differently in the Nursing Home. J. Gerontol. A Biol. Sci. Med. Sci. 2016, 71, 273–278. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vu, M.Q.; Weintraub, N.; Rubenstein, L.Z. Falls in the nursing home: Are they preventable? J. Am. Med. Dir. Assoc. 2004, 5, 401–406. [Google Scholar] [CrossRef] [PubMed]
- Becker, C.; Loy, S.; Nikolaus, T.; Rissmann, U.; Rapp, K.; Lindemann, B.; Kron, M. A follow-up study on fall and fracture incidence in long-term care including the role of formal caregiver time on fall incidence rates. Z. Gerontol. Und Geriatr. 2006, 39, 292–296. [Google Scholar] [CrossRef] [PubMed]
- Van Doorn, C.; Gruber-Baldini, A.L.; Zimmerman, S.; Hebel, J.R.; Port, C.L.; Baumgarten, M.; Quinn, C.C.; Taler, G.; May, C.; Magaziner, J. Dementia as a risk factor for falls and fall injuries among nursing home residents. J. Am. Geriatr. Soc. 2003, 51, 1213–1218. [Google Scholar] [CrossRef]
- Damián, J.; Pastor-Barriuso, R.; Valderrama-Gama, E.; de Pedro-Cuesta, J. Factors associated with falls among older adults living in institutions. BMC Geriatr. 2013, 13, 6. [Google Scholar] [CrossRef] [Green Version]
- Tanaka, B.; Sakuma, M.; Ohtani, M.; Toshiro, J.; Matsumura, T.; Morimoto, T. Incidence and risk factors of hospital falls on long-term care wards in Japan. J. Eval. Clin. Pract. 2012, 18, 572–577. [Google Scholar] [CrossRef]
- Rubenstein, L.Z.; Josephson, K.R.; Robbins, A.S. Falls in the nursing home. Ann. Intern. Med. 1994, 121, 442–451. [Google Scholar] [CrossRef]
- Seppala, L.J.; Wermelink, A.; de Vries, M.; Ploegmakers, K.J.; van de Glind, M.; Daams, J.G.; van der Velde, N. EUGMS Task and Finish Group on Fall-Risk-Increasing Drugs. Fall-Risk-Increasing Drugs: A Systematic Review and Meta-Analysis: II. Psychotropics. J. Am. Med. Dir. Assoc. 2018, 19, 371.e11–371.e17. [Google Scholar] [PubMed] [Green Version]
- Cox, C.A.; van Jaarsveld, H.J.; Houterman, S.; van der Stegen, J.C.; Wasylewicz, A.T.; Grouls, R.J.; van der Linden, C.M. Psychotropic Drug Prescription and the Risk of Falls in Nursing Home Residents. J. Am. Med. Dir. Assoc. 2016, 17, 1089–1093. [Google Scholar] [CrossRef] [PubMed]
- Baranzini, F.; Diurni, M.; Ceccon, F.; Poloni, N.; Cazzamalli, S.; Costantini, C.; Colli, C.; Greco, L.; Callegari, C. Fall-related injuries in a nursing home setting: Is polypharmacy a risk factor? BMC Health Serv. Res. 2009, 9, 228. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Masumoto, S.; Sato, M.; Maeno, T.; Ichinohe, Y.; Maeno, T. Potentially inappropriate medications with polypharmacy increase the risk of falls in older Japanese patients: 1-year prospective cohort study. Geriatr. Gerontol. Int. 2018, 18, 1064–1070. [Google Scholar] [CrossRef]
- Association, W.M. World Medical Association Declaration of Helsinki: Ethical Principles for Medical Research Involving Human Subjects. JAMA 2013, 310, 2191–2194. [Google Scholar]
- Gibson, M.J. The prevention of falls in later life. A report of the Kellogg International Work Group on the Prevention of Falls by the Elderly. Dan. Med. Bull. 1987, 34, 1–24. [Google Scholar]
- Bates, D.W.; Cullen, D.J.; Laird, N.; Petersen, L.A.; Small, S.D.; Servi, D.; Laffel, G.; Sweitzer, B.J.; Shea, B.F.; Hallisey, R.; et al. Incidence of adverse drug events and potential adverse drug events. Implications for prevention. ADE Prevention Study Group. JAMA 1995, 274, 29–34. [Google Scholar] [CrossRef]
- Baker, S.P.; Harvey, A.H. Fall injuries in the elderly. Clin. Geriatr. Med. 1985, 1, 501–512. [Google Scholar] [CrossRef]
- Masnoon, N.; Shakib, S.; Kalisch-Ellett, L.; Caughey, G.E. What is polypharmacy? A systematic review of definitions. BMC Geriatr. 2017, 17, 230. [Google Scholar] [CrossRef] [Green Version]
- Charlson, M.E.; Pompei, P.; Ales, K.L.; MacKenzie, C.R. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. J. Chron. Dis. 1987, 40, 373–383. [Google Scholar] [CrossRef]
- Mahoney, F.I.; Barthel, D.W. Functional Evaluation: The Barthel Index. MD State Med. J. 1965, 14, 61–65. [Google Scholar] [PubMed]
- Naranjo, C.A.; Busto, U.; Sellers, E.M.; Sandor, P.; Ruiz, I.; Roberts, E.A.; Janecek, E.; Domecq, C.; Greenblatt, D.J. A method for estimating the probability of adverse drug reactions. Clin. Pharmacol. Ther. 1981, 30, 239–245. [Google Scholar] [CrossRef] [PubMed]
- Morimoto, T. Adverse drug events and medication errors: Detection and classification methods. Qual. Saf. Health Care 2004, 13, 306–314. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nakanishi, M.; Hattori, K.; Nakashima, T.; Sawamura, K. Health care and personal care needs among residents in nursing homes, group homes, and congregate housing in Japan: Why does transition occur, and where can the frail elderly establish a permanent residence? J. Am. Med. Dir. Assoc. 2014, 15, 76.e1–76.e6. [Google Scholar] [CrossRef]
- Jester, D.J.; Molinari, V.; Zgibor, J.C.; Volicer, L. Prevalence of psychotropic polypharmacy in nursing home residents with dementia: A meta-analysis. Int. Psychogeriatr. 2021, 33, 1083–1098. [Google Scholar] [CrossRef]
- Towne, S.D.; Cho, J.; Smith, M.L.; Ory, M.G. Factors Associated with Injurious Falls in Residential Care Facilities. J. Aging Health 2016, 29, 669–687. [Google Scholar] [CrossRef]
- Gustafsson, M.; Karlsson, S.; Gustafson, Y.; Lövheim, H. Psychotropic drug use among people with dementia—A six-month follow-up study. BMC Pharmacol. Toxicol. 2013, 14, 56. [Google Scholar] [CrossRef] [Green Version]
- Park, T.W.; Saitz, R.; Ganoczy, D.; Ilgen, M.A.; Bohnert, A.S. Benzodiazepine prescribing patterns and deaths from drug overdose among US veterans receiving opioid analgesics: Case-cohort study. BMJ 2015, 350, h2698. [Google Scholar] [CrossRef] [Green Version]
- Ralph, S.J.; Espinet, A.J. Increased All-Cause Mortality by Antipsychotic Drugs: Updated Review and Meta-Analysis in Dementia and General Mental Health Care. J. Alzheimers Dis. Rep. 2018, 2, 1–26. [Google Scholar] [CrossRef] [Green Version]
- Baillon, S.F.; Narayana, U.; Luxenberg, J.S.; Clifton, A.V. Valproate preparations for agitation in dementia. Cochrane Database Syst. Rev. 2018, 10, CD003945. [Google Scholar] [CrossRef] [Green Version]
- Jordan, S.; Prout, H.; Carter, N.; Dicomidis, J.; Hayes, J.; Round, J.; Carson-Stevens, A. Nobody ever questions—Polypharmacy in care homes: A mixed methods evaluation of a multidisciplinary medicines optimisation initiative. PLoS ONE 2021, 16, e0244519. [Google Scholar] [CrossRef] [PubMed]
- Jordan, S.; Logan, V.; Turner, A.; Hughes, D. Using nurse-led patient monitoring to avoid medicines-related harm. Nurs. Stand. 2021, 36, 61–66. [Google Scholar] [PubMed]
- Rawle, M.J.; Cooper, R.; Kuh, D.; Richards, M. Associations Between Polypharmacy and Cognitive and Physical Capability: A British Birth Cohort Study. J. Am. Geriatri. Soc. 2018, 66, 916–923. [Google Scholar] [CrossRef] [Green Version]
- Vetrano, D.L.; Villani, E.R.; Grande, G.; Giovannini, S.; Cipriani, M.C.; Manes-Gravina, E.; Bernabei, R.; Onder, G. Association of Polypharmacy with 1-Year Trajectories of Cognitive and Physical Function in Nursing Home Residents: Results From a Multicenter European Study. J. Am. Med. Dir. Assoc. 2018, 19, 710–713. [Google Scholar] [CrossRef] [PubMed]
- Ayani, N.; Sakuma, M.; Morimoto, T.; Kikuchi, T.; Watanabe, K.; Narumoto, J.; Fukui, K. The epidemiology of adverse drug events and medication errors among psychiatric inpatients in Japan: The JADE study. BMC Psychiatry 2016, 16, 303. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Variables | ALL (n = 459) | Fallers † (n = 204) | Non-Fallers (n = 255) | Χ2 or t Value | p-Value |
|---|---|---|---|---|---|
| Female, n (%) | 344 (75) | 157 (77) | 187 (73) | 0.79 | 0.4 |
| Age, mean (SD) (years) | 87.0 (6.9) | 87.3 (6.5) | 86.9 (7.2) | 0.50 | 0.7 |
| Length of stay, median (IQR) (days) | 113 (0–760) | 148 (0–776) | 104 (0–738) | −0.48 | 0.6 |
| No. of all drugs §, median (IQR) | 4 (2–6) | 5 (3–7) | 4 (2–6) | 2.37 | 0.02 |
| Polypharmacy §,¶, n (%) | 210 (46) | 105 (51) | 105 (41) | 4.84 | 0.03 |
| No. of psychotropic drugs §, median (IQR) | 0 (0–1) | 1 (0–2) | 0 (0–1) | 3.55 | <0.001 |
| Psychotropic drugs §,#, n (%) | 228 (49.6) | 115 (56) | 113 (44) | 6.61 | 0.01 |
| BZDRAs §,$, n (%) | 115 (25) | 68 (33) | 47 (18) | 13.4 | <0.001 |
| Antipsychotic drugs §, n (%) | 332 (72) | 59 (29) | 68 (27) | 0.29 | 0.6 |
| Antiepileptic drugs §, n (%) | 65 (14) | 38 (19) | 27 (11) | 6.73 | 0.01 |
| Antidepressant drugs §, n (%) | 29 (6.3) | 16 (7.8) | 13 (5.1) | 1.43 | 0.2 |
| Antihypertensive drugs §, n (%) | 206 (45) | 95 (47) | 111 (44) | 0.42 | 0.5 |
| Dementia, n (%) | 406 (88) | 181 (89) | 225 (88) | 0.03 | 0.9 |
| Charlson Comorbidity Index, median (IQR) | 1 (1–3) | 1 (1–3) | 2 (1–3) | −2.47 | 0.006 |
| Body mass index, median (IQR) | 19.7 (17.5–21.9) | 20.3 (18.0–22.3) | 19.0 (17.1–21.8) | 1.92 | 0.06 |
| Barthel Index), median (IQR) | 50 (25–80) | 65 (45–80) | 45 (10–75) | 5.83 | <0.001 |
| Barthel Index ≥ 60 (independent, mildly dependent), n (%) | 213 (46) | 114 (56) | 99 (39) | 13.3 | <0.001 |
| Factors (Multiple Selections Were Possible) | |
|---|---|
| No. of falls, n | 645 |
| Medications (i.e., ADEs *1), n(%) | 480 (74) |
| Physical conditions *2, n(%) | 375 (58) |
| Psychiatric conditions, n(%) | 315 (49) |
| Operation errors of wheelchairs, n(%) | 25 (3.9) |
| Mistakes during caregiving, n(%) | 25 (3.9) |
| Slip of their feet, n(%) | 12 (1.9) |
| Trouble with clothes(trousers)/shoes, n(%) | 9 (1.4) |
| Obstacles at their feet, n(%) | 8 (1.2) |
| Operation errors of walking frames, n(%) | 7 (1.1) |
| Troubles with others *3, n(%) | 4 (0.6) |
| Unspecified, n(%) | 29 (4.5) |
| Risk Factor | Crude HR | 95% CI | Adjusted HR | 95% CI |
|---|---|---|---|---|
| No. of medication ¶ ≥ 5 | 1.37 | 1.04–1.80 | 1.33 | 1.00–1.77 |
| Female | 0.86 | 0.63–1.21 | 0.80 | 0.57–1.11 |
| Age ≥ 85 | 0.96 | 0.72–1.28 | 1.02 | 0.75–1.37 |
| Dementia | 0.97 | 0.64–1.53 | 1.03 | 0.65–1.63 |
| CCI ≥ 3 | 0.82 | 0.60–1.11 | 0.83 | 0.60–1.15 |
| BMI < 20 | 0.81 | 0.61–1.07 | 0.89 | 0.67–1.18 |
| Barthel Index ≥ 60 (independent, mildly dependent) | 1.48 | 1.12–1.95 | 1.44 | 1.08–1.92 |
| Variables | All Fallers (n = 204) | Fallers with Injuries (n = 89) | Fallers without Injuries (n = 115) | Χ2 or t Value | p-Value |
|---|---|---|---|---|---|
| Female, n (%) | 157 | 68 (76) | 89 (77) | 0.03 | 0.9 |
| Age, mean (SD) (years) | 87.3 | 87.1 (6.6) | 87.4 (6.4) | −0.39 | 0.7 |
| Length of stay, median (IQR) (days) | 148 (0–776) | 169 (0–872) | 120 (0–649) | 1.26 | 0.2 |
| No. of all drugs §, median (IQR) | 5 (3–7) | 5 (3–6.5) | 4 (2–7) | 0.61 | 0.3 |
| Polypharmacy §,¶, n (%) | 105 | 52 (58) | 53 (46) | 3.07 | 0.08 |
| No. of psychotropic drugs §, median (IQR) | 1 (0–2) | 1 (0–2) | 1 (0–2) | 0.12 | 0.8 |
| Psychotropic drugs §, n (%) | 115 | 53 (60) | 62 (54) | 0.65 | 0.4 |
| BZDRAs §, n (%) | 68 | 32 (36) | 36 (31) | 0.49 | 0.5 |
| Antipsychotic drugs §, n (%) | 59 | 25 (28) | 34 (30) | 0.05 | 0.8 |
| Antiepileptic drugs §, n (%) | 38 | 15 (17) | 23 (20) | 0.07 | 0.6 |
| Antidepressant drugs §, n (%) | 16 | 4 (4) | 12 (10) | 2.59 | 0.1 |
| Antihypertensive drugs §, n (%) | 95 | 43 (48) | 52 (45) | 0.19 | 0.7 |
| Dementia, n (%) | 181 | 82 (92) | 99 (86) | 1.89 | 0.2 |
| Charlson Comorbidity Index, median (IQR) | 1 (1–3) | 1 (1–3) | 1 (1–3) | 0.46 | 0.6 |
| Body mass index, median (IQR) | 20.3 (18.0–22.3) | 20.2 (18.1–22.0) | 20.3 (17.8–22.5) | −0.21 | 0.8 |
| Barthel Index, median (IQR) | 65 (45–80) | 70 (50–90) | 50 (40–75) | 4.30 | <0.0001 |
| Barthel Index ≥ 60 (independent, mildly dependent), n (%) | 114 | 64 (72) | 50 (43) | 16.8 | <0.0001 |
| Risk Factor | Crude OR | 95% CI | Adjusted OR | 95% CI |
|---|---|---|---|---|
| No. of medication ¶ ≥ 5 | 1.64 | 0.94–2.87 | 2.41 | 1.30–4.50 |
| Female | 0.95 | 0.49–1.82 | 0.91 | 0.44–1.87 |
| Age ≥ 85 y | 0.91 | 0.51–1.63 | 0.94 | 0.49–1.77 |
| Dementia | 1.89 | 0.74–4.82 | 2.52 | 0.87–7.30 |
| CCI ≥ 3 | 0.96 | 0.51–1.79 | 0.98 | 0.50–1.96 |
| BMI < 20 | 1.10 | 0.63–1.94 | 1.29 | 0.70–2.37 |
| Barthel Index ≥ 60 (independent, mildly dependent) | 3.33 | 1.84–6.01 | 3.46 | 1.84–6.54 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Oya, N.; Ayani, N.; Kuwahara, A.; Kitaoka, R.; Omichi, C.; Sakuma, M.; Morimoto, T.; Narumoto, J. Over Half of Falls Were Associated with Psychotropic Medication Use in Four Nursing Homes in Japan: A Retrospective Cohort Study. Int. J. Environ. Res. Public Health 2022, 19, 3123. https://doi.org/10.3390/ijerph19053123
Oya N, Ayani N, Kuwahara A, Kitaoka R, Omichi C, Sakuma M, Morimoto T, Narumoto J. Over Half of Falls Were Associated with Psychotropic Medication Use in Four Nursing Homes in Japan: A Retrospective Cohort Study. International Journal of Environmental Research and Public Health. 2022; 19(5):3123. https://doi.org/10.3390/ijerph19053123
Chicago/Turabian StyleOya, Nozomu, Nobutaka Ayani, Akiko Kuwahara, Riki Kitaoka, Chie Omichi, Mio Sakuma, Takeshi Morimoto, and Jin Narumoto. 2022. "Over Half of Falls Were Associated with Psychotropic Medication Use in Four Nursing Homes in Japan: A Retrospective Cohort Study" International Journal of Environmental Research and Public Health 19, no. 5: 3123. https://doi.org/10.3390/ijerph19053123
APA StyleOya, N., Ayani, N., Kuwahara, A., Kitaoka, R., Omichi, C., Sakuma, M., Morimoto, T., & Narumoto, J. (2022). Over Half of Falls Were Associated with Psychotropic Medication Use in Four Nursing Homes in Japan: A Retrospective Cohort Study. International Journal of Environmental Research and Public Health, 19(5), 3123. https://doi.org/10.3390/ijerph19053123






