Effectiveness of Interventions Based on Pain Neuroscience Education on Pain and Psychosocial Variables for Osteoarthritis: A Systematic Review
Abstract
:1. Introduction
2. Materials and Methods
2.1. Eligibility Criteria
2.2. Information Source and Search Strategy
2.3. Selection of Studies
2.4. Information Gathering Process
2.5. Quality Rating, Risk of Bias and Certainty of the Included Articles
3. Results
3.1. Description of the Intervention
3.2. Assessing the Quality of the Evidence
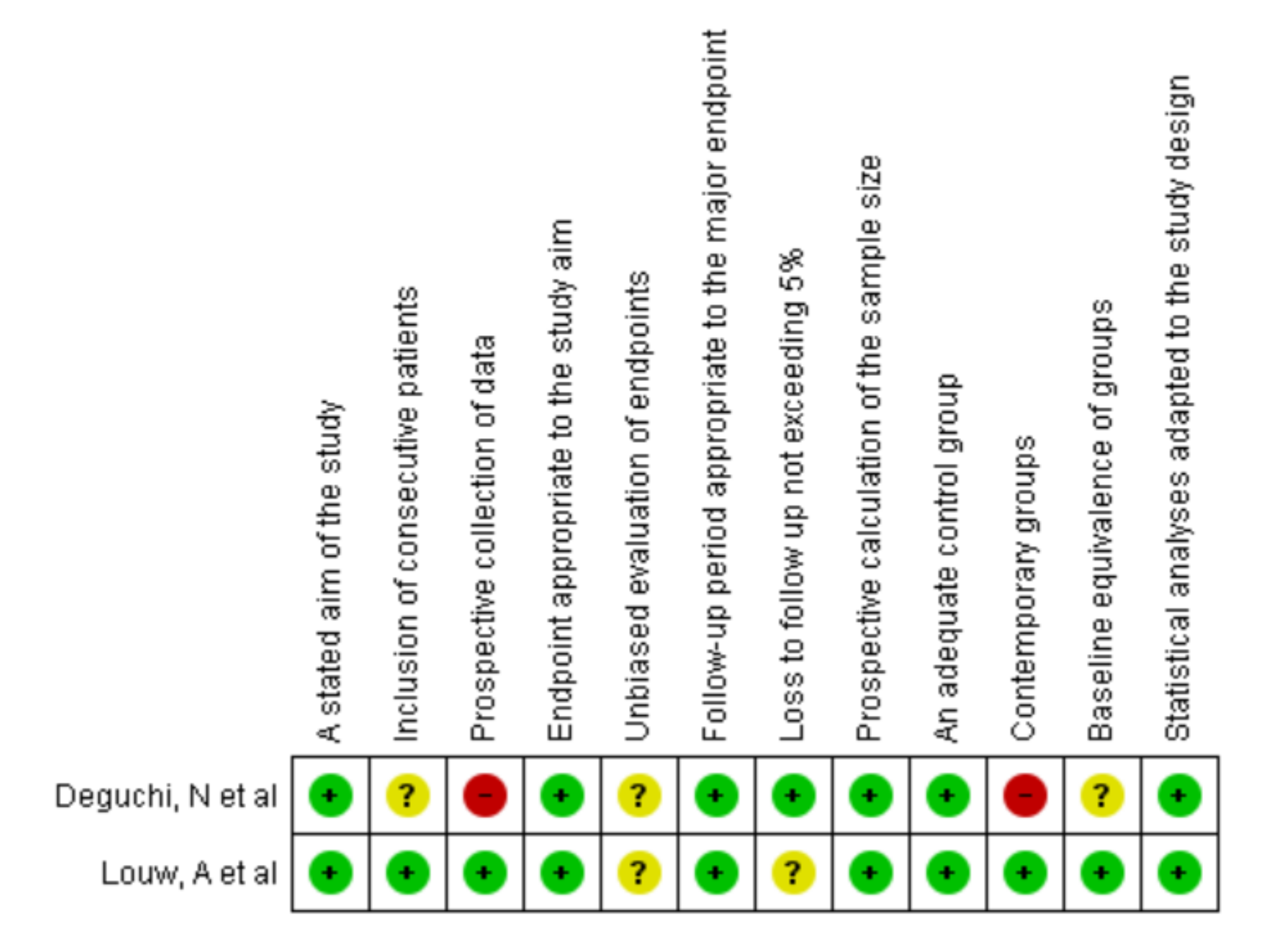
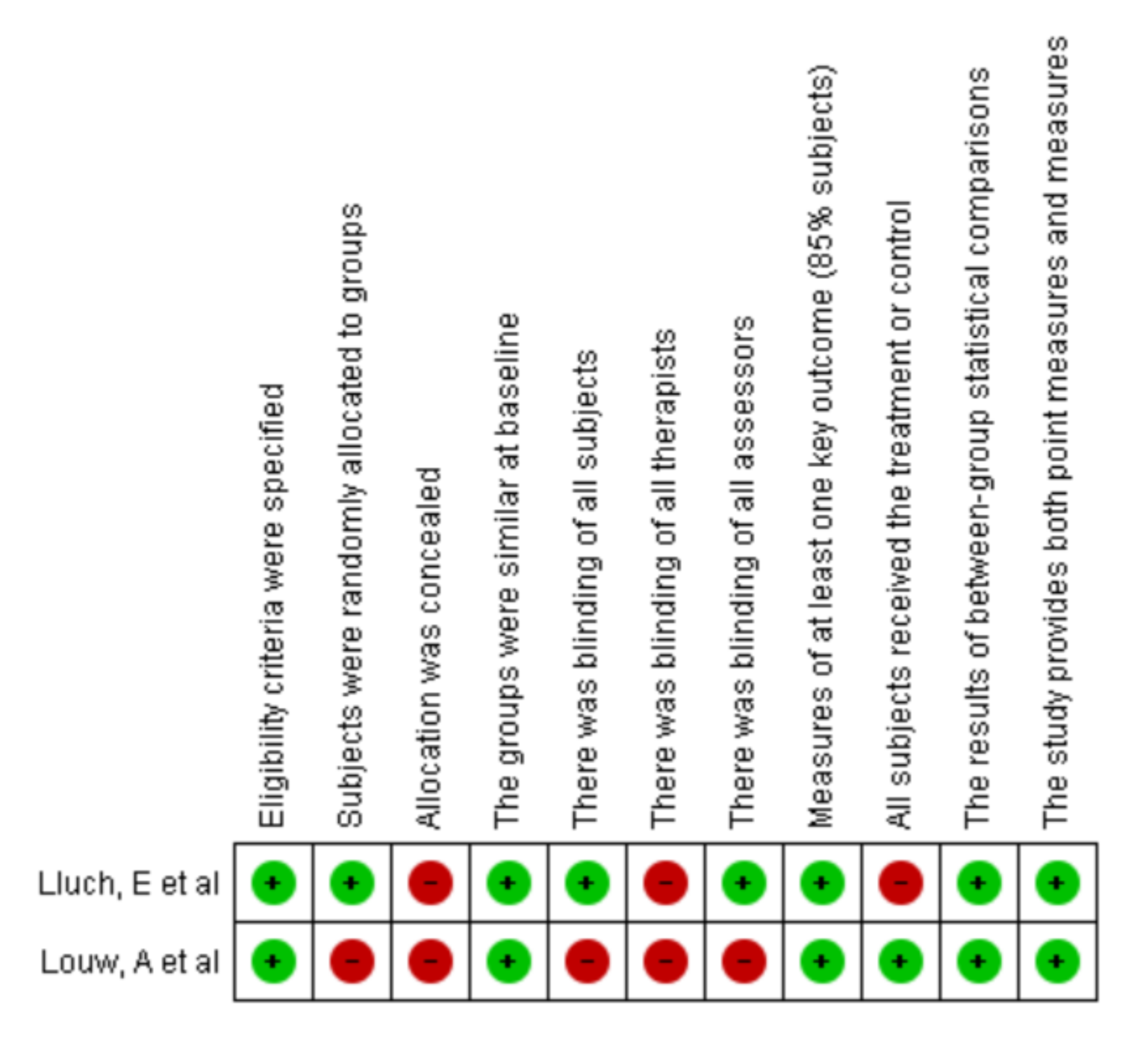
3.2.1. MINORS Scale
3.2.2. Pedro Scale
3.3. Pain Results
3.3.1. PNE Compared with Another Intervention
3.3.2. PNE Compared with Other Educational Processes
3.3.3. PNE with No Comparison
3.4. Catastrophizing Results
3.4.1. PNE Compared with Another Intervention
3.4.2. PNE Compared with Other Educational Processes
3.4.3. PNE with No Comparison
3.5. Kinesiophobia Results
3.5.1. PNE Compared with Other Educational Processes
3.5.2. PNE with No Comparison
3.6. Disability Results
PNE Compared with Other Educational Processes
3.7. Quality of Life Results
PNE Compared with Another Intervention
3.8. Certainty Analysis
3.9. Characteristics of the Excluded Studies
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
- Pain Education
- Pain Neuroscience
- Pain Neuroscience education
- Neurophysiology education
- Therapeutics Neuroscience Education
- Chronic Pain
- Osteoarthritis
- MH Chronic Pain
- MH Osteoarthritis
- 1 AND 6 AND 7
- 1 AND 6 OR 8 AND 7
- 2 AND 7
- 3 AND 7 OR 9
- 4 AND 7
- 5 AND 7
References
- Safiri, S.; Kolahi, A.A.; Smith, E.; Hill, C.; Bettampadi, D.; Mansournia, M.A.; Almasi-Hashiani, A.; Ashrafi-Asgarabad, A.; Moradi-Lakeh, M.; Qorbani, M.; et al. Global, regional and national burden of osteoarthritis 1990–2017: A systematic analysis of the Global Burden of Disease Study 2017. Ann. Rheum. Dis. 2020, 79, 819–828. [Google Scholar] [CrossRef] [PubMed]
- Organizacioón Mundial de la Salud. Aplicaciones de la Epidemiologiía al Estudio de Los Ancianos. Informe Teécnico. Available online: http://apps.who.int/iris/handle/10665/39141?locale=e (accessed on 8 November 2021).
- Michael, J.; Schlüter-Brust, K.; Eysel, P. The epidemiology, etiology, diagnosis, and treatment of osteoarthritis of the knee. Dtsch. Arztebl. Int. 2010, 107, 152–162. [Google Scholar] [CrossRef] [PubMed]
- Kolasinski, S.L.; Kolasinski, S.L.; Neogi, T.; Neogi, T.; Hochberg, M.C.; Hochberg, M.C.; Oatis, C.; Oatis, C.; Guyatt, G.; Guyatt, G.; et al. Guideline for the Management of Osteoarthritis of the Hand, Hip, and Knee. Arthritis Care Res. 2020, 72, 149–162. [Google Scholar] [CrossRef]
- O’Neill, T.; McCabe, P.; McBeth, J. Update on the epidemiology, risk factors and disease outcomes of osteoarthritis. Best Pract. Res. Clin. Rheumatol. 2018, 32, 312–326. [Google Scholar] [CrossRef]
- Malemud, C.J. Biologic basis of osteoarthritis: State of the evidence. Curr. Opin. Rheumatol. 2015, 27, 289–294. [Google Scholar] [CrossRef] [PubMed]
- Montero, A.; Mulero, J.; Tornero, C.; Guitart, J.; Serrano, M. Pain, disability and health-related quality of life in osteoarthritis-joint matters: An observational, multi-specialty trans-national follow-up study. Clin. Rheumatol. 2016, 35, 2293–2305. [Google Scholar] [CrossRef]
- Oliveira, P.; Monteiro, P.; Coutinho, M.; Salvador, M.; Costa, M.; Malcata, A. Health-related quality of life and chronic pain experience in rheumatic diseases. Acta Reumatol. Port. 2009, 34, 511–519. [Google Scholar] [PubMed]
- Mandl, L. Osteoarthritis year in review 2018: Clinical. Osteoarthr. Cartil. 2019, 27, 359–364. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nelson, A. Osteoarthritis year in review 2017 clinical. Osteoarthr. Cartil. 2018, 26, 319–325. [Google Scholar] [CrossRef] [Green Version]
- Robson, E.K.; Hodder, R.K.; Kamper, S.J.; O’Brien, K.M.; Williams, A.; Lee, H.; Wolfenden, L.; Yoong, S.; Wiggers, J.; Barnett, C.; et al. Effectiveness of Weight-Loss Interventions for Reducing Pain and Disability in People with Common Musculoskeletal Disorders: A Systematic Review with Meta-Analysis. J. Orthop. Sports Phys. Ther. 2020, 50, 319–333. [Google Scholar] [CrossRef] [PubMed]
- Teirlinck, C.H.; Verhagen, A.P.; Reijneveld, E.A.E.; Runhaar, J.; van Middelkoop, M.; van Ravesteyn, L.M.; Hermsen, L.; de Groot, I.B.; Bierma-Zeinstra, S.M.A. Responders to Exercise Therapy in Patients with Osteoarthritis of the Hip: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2020, 17, 7380. [Google Scholar] [CrossRef] [PubMed]
- Goh, S.-L.; Persson, M.S.M.; Stocks, J.; Hou, Y.; Welton, N.; Lin, J.; Hall, M.C.; Doherty, M.; Zhang, W. Relative Efficacy of Different Exercises for Pain, Function, Performance and Quality of Life in Knee and Hip Osteoarthritis: Systematic Review and Network Meta-Analysis. Sports Med. 2019, 49, 743–761. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gay, C.; Chabaud, A.; Guilley, E.; Coudeyre, E. Educating patients about the benefits of physical activity and exercise for their hip and knee osteoarthritis. Systematic literature review. Ann. Phys. Rehabil. Med. 2016, 59, 174–183. [Google Scholar] [CrossRef]
- Anwer, S.; Alghadir, A.; Zafar, H.; Brismée, J.M. Effects of orthopaedic manual therapy in knee osteoarthritis: A systematic review and meta-analysis. Physiotherapy 2018, 104, 264–276. [Google Scholar] [CrossRef]
- Marotta, N.; Demeco, A.; Marinaro, C.; Moggio, L.; Pino, I.; Barletta, M.; Petraroli, A.; Ammendolia, A. Comparative Effectiveness of Orthoses for Thumb Osteoarthritis: A Systematic Review and Network Meta-analysis. Arch. Phys. Med. Rehabil. 2021, 102, 502–509. [Google Scholar] [CrossRef]
- Letizia Mauro, G.; Scaturro, D.; Gimigliano, F.; Paoletta, M.; Liguori, S.; Toro, G.; Iolascon, G.; Moretti, A. Physical Agent Modalities in Early Osteoarthritis: A Scoping Review. Medicina 2021, 57, 1165. [Google Scholar] [CrossRef] [PubMed]
- Ritschl, V.; A Stamm, T.; Aletaha, D.; Bijlsma, J.W.J.; Böhm, P.; Dragoi, R.; Dures, E.; Estévez-López, F.; Gossec, L.; Iagnocco, A.; et al. Prevention, screening, assessing and managing of non-adherent behaviour in people with rheumatic and musculoskeletal diseases: Systematic reviews informing the 2020 EULAR points to consider. RMD Open 2020, 6, e001432. [Google Scholar] [CrossRef]
- Nijs, J.; Goubert, D.; Ickmans, K. Recognition and Treatment of Central Sensitization in Chronic Pain Patients: Not Limited to Specialized Care. J. Orthop. Sports Phys. Ther. 2016, 46, 1024–1028. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Louw, A.; Puentedura, E. Therapeutic Neuroscience Education: Teaching Patients about Pain: A guide for Clinicians; International Spine and Pain Institute: Story City, IA, USA, 2013. [Google Scholar]
- Malfliet, A.; Kregel, J.; Meeus, M.; Cagnie, B.; Roussel, N.; Dolphens, M.; Danneels, L.; Nijs, J. Applying contemporary neuroscience in exercise interventions for chronic spinal pain: Treatment protocol. Braz. J. Phys. Ther. 2017, 21, 378–387. [Google Scholar] [CrossRef]
- Nijs, J.; Malfliet, A.; Ickmans, K.; Baert, I.; Meeus, M. Treatment of central sensitization in patients with “unexplained” chronic pain: An update. Expert Opin. Pharmacother. 2014, 15, 1671–1683. [Google Scholar] [CrossRef] [PubMed]
- Moseley, G.L.; Butler, D.S. Fifteen Years of Explaining Pain: The Past, Present, and Future. J. Pain 2015, 16, 807–813. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moseley, G.; Butler, D. Explain Pain Supercharged; NOI Group Publishers: Adelaide City, Australia, 2017. [Google Scholar]
- Nijs, J.; Lluch Girbés, E.; Lundberg, M.; Malfliet, A.; Sterling, M. Exercise therapy for chronic musculoskeletal pain: Innovation by altering pain memories. Man. Ther. 2015, 20, 216–220. [Google Scholar] [CrossRef] [PubMed]
- Lluch Girbés, E.; Nijs, J.; Torres-Cueco, R.; López Cubas, C. Pain treatment for patients with osteoarthritis and central sensitization. Phys. Ther. 2013, 93, 842–851. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wijma, A.; van Wilgen, C.; Meeus, M.; Nijs, J. Clinical biopsychosocial physiotherapy assessment of patients with chronic pain: The first step in pain neuroscience education. Physiother. Theory Pract. 2016, 32, 368–384. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.; Green, S. Cochrane handbook for systematic reviews. Cochrane Collab. 2008, 5, 74–100. [Google Scholar]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Slim, K.; Nini, E.; Forestier, D.; Kwiatkowski, F.; Panis, Y.; Chipponi, J. Methodological index for non-randomized studies (MINORS): Development and validation of a new instrument. ANZ J. Surg. 2003, 73, 712–716. [Google Scholar] [CrossRef] [PubMed]
- Sydney Musculoskeletal Health. PEDro—Physiotherapy Evidence Database—PEDro Scale. 2020. Available online: https://pedro.org.au/spanish/resources/pedro-scale/ (accessed on 6 June 2020).
- Schünemann, H.; Brożek, J.; Guyatt, G.; Oxman, A. (Eds.) GRADE Handbook for Grading Quality of Evidence and Strength of Recommendations. Updated October 2013. The GRADE Working Group, 2013. Available online: https://gdt.gradepro.org/app/handbook/handbook.html (accessed on 10 December 2021).
- GRADEpro GDT: GRADEpro Guideline Development Tool [Software]. McMaster University and Evidence Prime, 2021. Available online: gradepro.org (accessed on 10 December 2021).
- Deguchi, N.; Hirakawa, Y.; Izawa, S.; Yokoyama, K.; Muraki, K.; Oshibuti, R.; Higaki, Y. Effects of pain neuroscience education in hospitalized patients with high tibial osteotomy: A quasi-experimental study using propensity score matching. BMC Musculoskelet. Disord. 2019, 20, 516. [Google Scholar] [CrossRef]
- Louw, A.; Puentedura, E.J.; Reed, J.; Zimney, K.; Grimm, D.; Landers, M.R. A controlled clinical trial of preoperative pain neuroscience education for patients about to undergo total knee arthroplasty. Clin. Rehabil. 2019, 33, 1722–1731. [Google Scholar] [CrossRef] [PubMed]
- Louw, A.; Zimney, K.; Reed, J.; Landers, M.; Puentedura, E.J. Immediate preoperative outcomes of pain neuroscience education for patients undergoing total knee arthroplasty: A case series. Physiother. Theory Pract. 2019, 35, 543–553. [Google Scholar] [CrossRef] [PubMed]
- Lluch, E.; Dueñas, L.; Falla, D.; Baert, I.; Meeus, M.; Sánchez-Frutos, J.; Nijs, J. Preoperative pain neuroscience education combined with knee joint mobilization for knee osteoarthritis. Clin. J. Pain 2018, 34, 44–52. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Xie, S.; Bao, T.; Zhu, S.; Liang, Q.; Wang, X.; Zhang, R.; Xiang, X.; Du, C.; He, C. Exercise and education for community-dwelling older participants with knee osteoarthritis: A video-linked programme protocol based on a randomised controlled trial. BMC Musculoskelet. Disord. 2021, 22, 470. [Google Scholar] [CrossRef]
- Larsen, J.B.; Skou, S.T.; Arendt-Nielsen, L.; Simonsen, O.; Madeleine, P. Neuromuscular exercise and pain neuroscience education compared with pain neuroscience education alone in patients with chronic pain after primary total knee arthroplasty: Study protocol for the NEPNEP randomized controlled trial. Trials 2020, 21, 218. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lawford, B.J.; Hinman, R.S.; Kasza, J.; Nelligan, R.; Keefe, F.; Rini, C.; Bennell, K.L. Moderators of Effects of Internet-Delivered Exercise and Pain Coping Skills Training for People with Knee Osteoarthritis: Exploratory Analysis of the IMPACT Randomized Controlled Trial. J. Med. Internet. Res. 2018, 20, e10021. [Google Scholar] [CrossRef] [Green Version]
- Saw, M.M.; Kruger-Jakins, T.; Edries, N.; Parker, R. Significant improvements in pain after a six-week physiotherapist-led exercise and education intervention, in patients with osteoarthritis awaiting arthroplasty, in South Africa: A randomised controlled trial. BMC Musculoskelet. Disord. 2016, 17, 236. [Google Scholar] [CrossRef] [Green Version]
- Bennell, K.L.; Ahamed, Y.; Jull, G.; Bryant, C.; Hunt, M.A.; Forbes, A.B.; Kasza, J.; Akram, M.; Metcalf, B.; Harris, A.; et al. Physical Therapist-Delivered Pain Coping Skills Training and Exercise for Knee Osteoarthritis: Randomized Controlled Trial. Arthritis Care Res. 2016, 68, 590–602. [Google Scholar] [CrossRef] [PubMed]
- Fernandes, L.; Storheim, K.; Sandvik, L.; Nordsletten, L.; Risberg, M.A. Efficacy of patient education and supervised exercise vs. patient education alone in patients with hip osteoarthritis: A single blind randomized clinical trial. Osteoarthr. Cartil. 2010, 18, 1237–1243. [Google Scholar] [CrossRef] [PubMed]
- Bezalel, T.; Carmeli, E.; Katz-Leurer, M. The effect of a group education programme on pain and function through knowledge acquisition and home-based exercise among patients with knee osteoarthritis: A parallel randomised single-blind clinical trial. Physiotherapy 2010, 96, 137–143. [Google Scholar] [CrossRef] [PubMed]
- Baird, C.L.; Sands, L. A pilot study of the effectiveness of guided imagery with progressive muscle relaxation to reduce chronic pain and mobility difficulties of osteoarthritis. Pain Manag. Nurs. 2004, 5, 97–104. [Google Scholar] [CrossRef] [PubMed]
- Ettinger, W.H., Jr.; Burns, R.; Messier, S.P.; Applegate, W.; Rejeski, W.J.; Morgan, T.; Shumaker, S.; Berry, M.J.; O’Toole, M.; Monu, J.; et al. A randomized trial comparing aerobic exercise and resistance exercise with a health education program in older adults with knee osteoarthritis: The Fitness Arthritis and Seniors Trial (FAST). JAMA 1997, 277, 25–31. [Google Scholar] [CrossRef] [PubMed]
- Nijs, J.; Clark, J.; Malfliet, A.; Ickmans, K.; Voogt, L.; Don, S.; Bandt, H.D.; Goubert, D.; Kregel, J.; Coppieters, I.; et al. In the spine or in the brain? Recent advances in pain neuroscience applied in the intervention for low back pain. Clin. Exp. Rheumatol. 2017, 107, 108–115. [Google Scholar]
- Louw, A.; Diener, I.; Butler, D.S.; Puentedura, E.J. The effect of neuroscience education on pain, disability, anxiety, and stress in chronic musculoskeletal pain. Arch. Phys. Med. Rehabil. 2011, 92, 2041–2056. [Google Scholar] [CrossRef] [PubMed]
- Karlsen, A.; Wetterslev, M.; Hansen, S.; Hansen, M.; Mathiesen, O.; Dahl, J. Postoperative pain treatment after total knee arthroplasty: A systematic review. PLoS ONE 2017, 12, e0173107. [Google Scholar] [CrossRef]
- Bülow, K.; Lindberg, K.; Vaegter, H.B.; Juhl, C.B. Effectiveness of Pain Neurophysiology Education on Musculoskeletal Pain: A Systematic Review and Meta-Analysis. Pain Med. 2021, 22, 891–904. [Google Scholar] [CrossRef] [PubMed]
- Watson, J.A.; Ryan, C.G.; Atkinson, G.; Williamson, P.; Ellington, D.; Whittle, R.; Dixon, J.; Martin, D.J. Inter-Individual Differences in the Responses to Pain Neuroscience Education in Adults with Chronic Musculoskeletal Pain: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. J. Pain 2021, 22, 9–20. [Google Scholar] [CrossRef] [PubMed]
- Louw, A.; Puentedura, E.; Diener, I. A descriptive study of the utilization of physical therapy for postoperative Rehabilitation in patients undergoing surgery for lumbar radiculopathy. Eur. Spine J. 2016, 25, 3550–3559. [Google Scholar] [CrossRef] [PubMed]


| Author | Year | Population and Mean Age | Intervention | Control | Pharmacological Treatment | Scales Used | Results |
|---|---|---|---|---|---|---|---|
| Deguchi, N et al. [34] | 2019 | IG: 67 (67 years); CG: 52 (63.7 years) | Rehabilitation (same as the control group) + 6 PNE sessions were carried out by a physiotherapist, with each session lasting 60 min | Rehabilitation only (weight bearing as tolerated, 6 times a week in 40- to 60- minute sessions) | NSAIDs 3 times a day postoperatively, tapered off at 3 weeks postoperatively | NRS, PCS, PSEQ | No significant effects were found in the comparison items between groups, except catastrophizing. |
| Louw, A et al. [35] | 2019 | IG: 49 (74.1 ± 9.5) 31 analyzed; CG: 54 (69.6 ± 10.6) 36 analyzed | PNE | Traditional preoperative educational program | Opioid treatment according to the determined regulation | NRS, PCS, Tampa scale, WOMAC | No differences could be found between the groups. |
| Louw, A et al. [36] | 2018 | Patients = 12 [10 women + 2 men] (68.6 ± 8.7 years) | PNE | The second group was not managed | Not specified | NRS, PCS, Tampa Scale | There were changes in favor of the PNE group. |
| Lluch et al. [37] | 2017 | IG patients: 27 (72.8 ± 5.6); CG patients: 27 (67.7 ± 7.8) | PNE + knee joint mobilization | Biomedical education + Knee joint mobilization | Not specified | CSI, PCS, Tampa Scale, WOMAC | Changes were found regarding kinesiophobia and catastrophizing for PNE. |
| Author | Scale | Pain | Scale | Catastrophizing | Scale | Kinesiophobia | Scale | Disability | Scale | Quality of Life |
|---|---|---|---|---|---|---|---|---|---|---|
| Deguchi, N et al. [34] | NRS | Without significant changes in the groups IG: Pain at rest pre 2.0 (2.6) post 1.1 (1.3) CG: pain at rest pre 1.9 (2.3) post 0.8 (1.2) | PCS | Significant effects in favor of PNE IG: pre 30.3 (6.5) post 16.9 (9.7) CG: pre 30.8 (7.7) post 20.7 (8.4) | PSEQ | No significant changes between the groups IG: pre 37.6 (10.6) post 43.4 (10.2) CG: pre 36.3 (11.1) post 38.7 (12.8) | ||||
| Louw, A et al. [35] | NRS | Significant improvement in both groups. There was a difference attributable to time (p < 0.001) with improvements in all patients. | PCS | No significant differences between the groups F (3192) = 0.209, p = 0.819, power = 0.083. (p = 0.075), yes, difference in time (p < 0.001) | Tampa Scale of Kinesiophobia | There were no significant differences between the groups F (3192) = 1.402, p = 0.245, power = 0.358 (p = 0.247) | WOMAC | There were no significant differences in the groups F (3195) = 1.501, p = 0.222, power = 0.355 | ||
| Louw, A et al. [36] | NRS | There were no significant differences between the pre- and post-intervention measures. pre PNE 5.0 IQR = 2.3–6.8 Range (0.0–8.0) post PNE 3.5 IQR = 1.0–5.0 Range (0.0–7.0) p = 0.119 | PCS | There were no significant differences between the measures. pre 3.3–27.8 (1.0–51.0) post 7.0 IQR = 3.3–15.8 Range (0.0–36.0) p = 0.081 | Tampa Scale of Kinesiophobia | A difference in favor of the PNE post intervention. pre 42.0 IQR = 38.5–44.0 Range (31.0–54.0) post 39.0 IQR = 36.0–42.5 Range (31.0–46.0) p = 0.036 | ||||
| Lluch E, et al. [37] | CSI | There were no significant differences between the groups. IG: pre 37.6 ± 17.2 post 30.3 ± 10.2 CG: pre 38.3 ± 15.6 post: 38.1 ± 15.7 | PCS | There were no significant differences between IG groups: Pre 22.6 ± 11.5 post 12.5 ± 10.3 CG: pre 25.9 ± 13.6 post 24.5 ± 13.6 | Tampa Scale of Kinesiophobia | Significant changes in favor of the PNE IG were reported pre 34.3 ± 7 post 25.9 ± 5.9 CG: pre 33.7 ± 5.6 post 33.6 ± 6.7 | WOMAC | There were no significant differences between the groups IG: pre 52.4 ± 14.6 post 41.4 ± 13.7 CG: pre 52.1 ± 18.4 post 50.1 ± 18.5 |
| Autor | Year | Type of Study | Reasons for Exclusion |
|---|---|---|---|
| Wang, L et al. [38] | 2021 | Clinical trial | It is a protocol, mention another educational technique |
| Larsen, J et al. [39] | 2020 | Clinical trial | It is a protocol |
| Lawford, B et al. [40] | 2018 | Clinical trial | it does not mention the specific technique |
| Saw MM et al. [41] | 2016 | Clinical trial | mention another educational technique |
| Bennell Kl et al. [42] | 2016 | Clinical trial | mention another educational technique |
| Fernandes L et al. [43] | 2010 | Clinical trial | mention another educational technique |
| Bezalel T et al. [44] | 2010 | Clinical trial | mention another educational technique |
| Baird CL et al. [45] | 2004 | Clinical trial | mention another educational technique |
| Ettinger WH et al. [46] | 1997 | Clinical trial | mention another educational technique |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ordoñez-Mora, L.T.; Morales-Osorio, M.A.; Rosero, I.D. Effectiveness of Interventions Based on Pain Neuroscience Education on Pain and Psychosocial Variables for Osteoarthritis: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 2559. https://doi.org/10.3390/ijerph19052559
Ordoñez-Mora LT, Morales-Osorio MA, Rosero ID. Effectiveness of Interventions Based on Pain Neuroscience Education on Pain and Psychosocial Variables for Osteoarthritis: A Systematic Review. International Journal of Environmental Research and Public Health. 2022; 19(5):2559. https://doi.org/10.3390/ijerph19052559
Chicago/Turabian StyleOrdoñez-Mora, Leidy Tatiana, Marco Antonio Morales-Osorio, and Ilem D. Rosero. 2022. "Effectiveness of Interventions Based on Pain Neuroscience Education on Pain and Psychosocial Variables for Osteoarthritis: A Systematic Review" International Journal of Environmental Research and Public Health 19, no. 5: 2559. https://doi.org/10.3390/ijerph19052559
APA StyleOrdoñez-Mora, L. T., Morales-Osorio, M. A., & Rosero, I. D. (2022). Effectiveness of Interventions Based on Pain Neuroscience Education on Pain and Psychosocial Variables for Osteoarthritis: A Systematic Review. International Journal of Environmental Research and Public Health, 19(5), 2559. https://doi.org/10.3390/ijerph19052559







