Changes in Physical Activity and Sedentary Behavior before and during the COVID-19 Pandemic: A Swedish Population Study
Abstract
:1. Introduction
2. Material and Methods
2.1. Recruitment of Participants and Data Collection
2.2. Measures
2.3. Statistical Analysis
2.3.1. Data Management
2.3.2. Analyses
3. Results
3.1. Description of the Sample
3.2. Changes in Total, Vigorous, Moderate, and Light PA
3.3. Changes in Types of PA
3.4. Changes in Sedentary Behavior
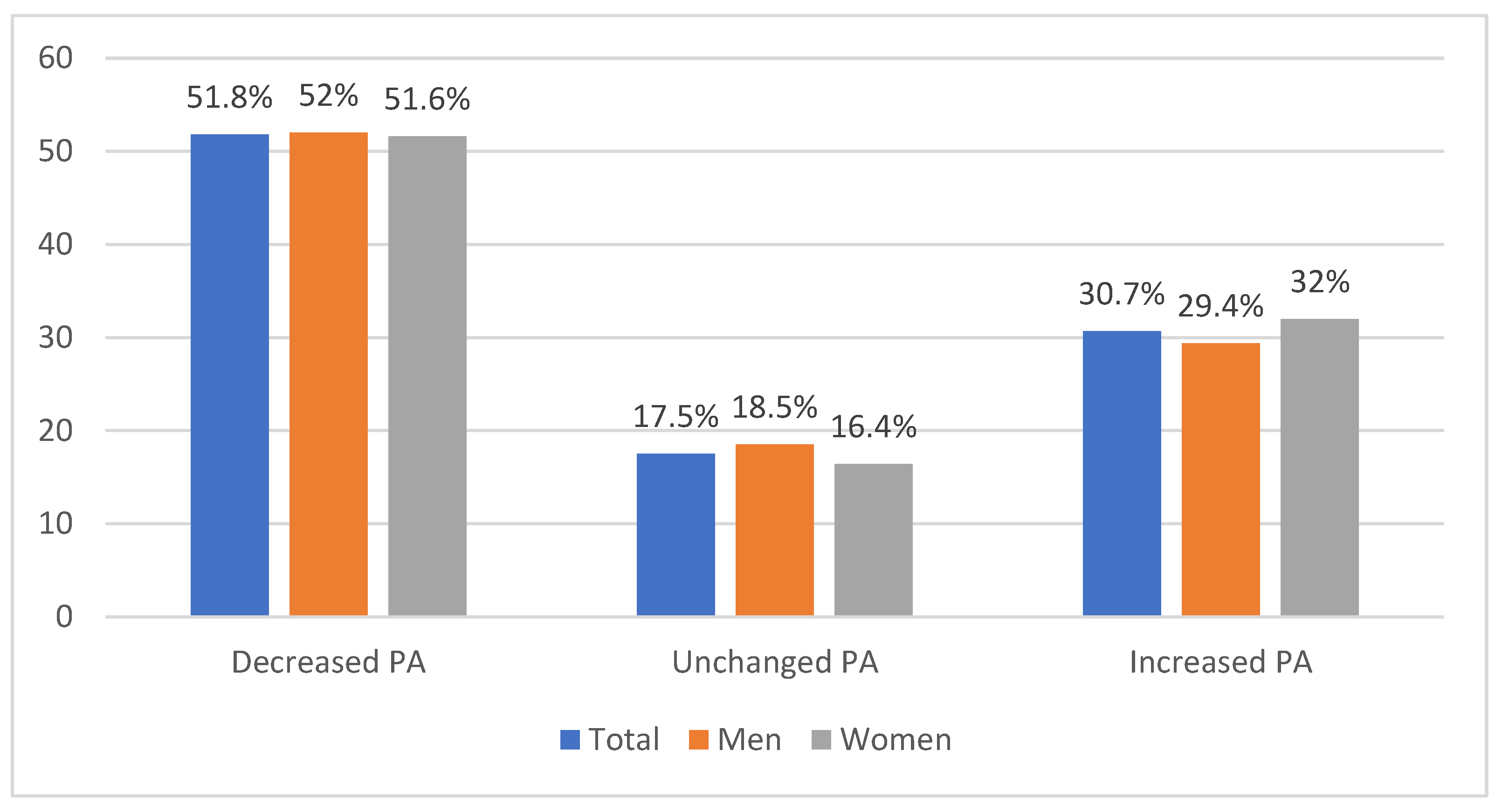
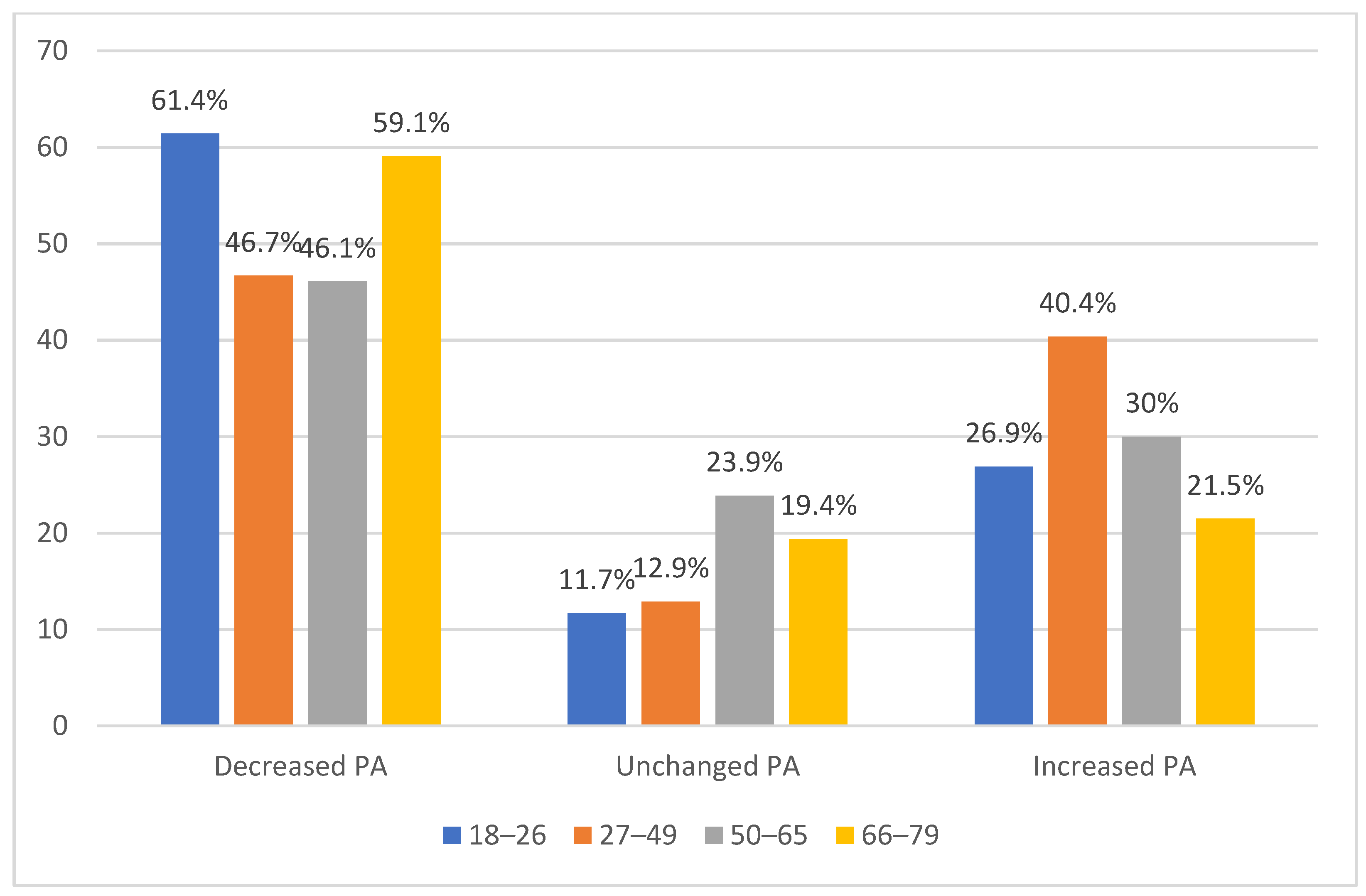
3.5. Determinants of Changes in PA
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Global Action Plan on Physical Activity 2018–2030: More Active People for a Healthier World. Available online: https://www.who.int/publications/i/item/9789241514187 (accessed on 20 January 2022).
- Guthold, R.; Stevens, G.A.; Riley, L.M.; Bull, F.C. Worldwide trends in insufficient physical activity from 2001 to 2016: A pooled analysis of 358 population-based surveys with 1·9 million participants. Lancet Glob. Health 2018, 6, e1077–e1086. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. WHO Global Status Report on Noncommunicable Diseases 2014. Available online: https://apps.who.int/iris/bitstream/handle/10665/148114/9789241564854_eng.pdf?sequence=1 (accessed on 20 January 2022).
- Tremblay, M.S.; Aubert, S.; Barnes, J.D.; Saunders, T.J.; Carson, V.; Latimer-Cheung, A.E.; Chastin, S.F.M.; Altenburg, T.M.; Chinapaw, M.J.M. Sedentary Behavior Research Network (SBRN)—Terminology consensus project process and outcome. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 75. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hagströmer, M.; Kwak, L.; Oja, P.; Sjöström, M. A 6 year longitudinal study of accelerometer-measured physical activity and sedentary time in Swedish adults. J. Sci. Med. Sport. 2015, 18, 553–557. [Google Scholar] [CrossRef] [PubMed]
- Panahi, S.; Tremblay, A. Sedentariness and health: Is sedentary behavior more than just physical inactivity? Front. Public Health 2018, 6, 258. [Google Scholar] [CrossRef] [Green Version]
- Van der Ploeg, H.P.; Hillsdon, M. Is sedentary behaviour just physical inactivity by another name? Int. J. Behav. Nutr. Phys. Act. 2017, 14, 142. [Google Scholar] [CrossRef]
- Patel, A.V.; Maliniak, M.L.; Rees-Punia, E.; Matthews, C.E.; Gapstur, S.M. Prolonged leisure time spent sitting in relation to cause-specific mortality in a large US cohort. Am. J. Epidemiol. 2018, 187, 2151–2158. [Google Scholar] [CrossRef] [Green Version]
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.P.; Chastin, S.; Chou, R.; et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef]
- World Health Organization. WHO Coronavirus (COVID-19) Dashboard. Available online: https://covid19.who.int (accessed on 20 January 2022).
- Chastin, S.F.M.; Abaraogu, U.; Bourgois, J.G.; Dall, P.M.; Darnborough, J.; Duncan, E.; Dumortier, J.; Pavón, D.J.; McParland, J.; Roberts, N.J.; et al. Effects of regular physical activity on the immune system, vaccination and risk of community-acquired infectious disease in the general population: Systematic review and meta-analysis. Sports Med. 2021, 51, 1673–1686. [Google Scholar] [CrossRef]
- Dahlen, M.; Thorbjørnsen, H.; Sjåstad, H.; von Heideken Wågert, P.; Hellström, C.; Kerstis, B.; Lindberg, D.; Stier, J.; Elvén, M. Changes in physical activity are associated with corresponding changes in psychological well-being: A pandemic case study. Int. J. Environ. Res. Public Health 2021, 18, 10680. [Google Scholar] [CrossRef]
- Mon, B.; McFall-Johnsen, M. A Third of the Global Population Is on Coronavirus Lockdown—Here’s Our Constantly Updated List of Countries and Restrictions. Available online: https://www.businessinsider.nl/countries-on-lockdown-coronavirus-italy-2020-3?international=true&r=US (accessed on 25 August 2020).
- Irwin, R.E. Misinformation and de-contextualization: International media reporting on Sweden and COVID-19. Glob. Health 2020, 16, 62. [Google Scholar] [CrossRef]
- Swedish Government. The Swedish Way: Government Policies and Practices. Available online: https://www.government.se/ (accessed on 20 January 2022).
- Tison, G.H.; Avram, R.; Kuhar, P.; Abreau, S.; Marcus, G.M.; Pletcher, M.J.; Olgin, J.E. Worldwide effect of COVID-19 on physical activity: A descriptive study. Ann. Intern. Med. 2020, 173, 767–770. [Google Scholar] [CrossRef]
- Ammar, A.; Brach, M.; Trabelsi, K.; Chtourou, H.; Boukhris, O.; Masmoudi, L.; Bouaziz, B.; Bentlage, E.; How, D.; Ahmed, M.; et al. Effects of COVID-19 home confinement on eating behaviour and physical activity: Results of the ECLB-COVID19 international online survey. Nutrients 2020, 12, 1583. [Google Scholar] [CrossRef] [PubMed]
- Elisabeth, A.L.; Karlen, S.B.-L.; Magkos, F. The effect of COVID-19-related lockdowns on diet and physical activity in older adults: A systematic review. Aging Dis. 2021, 12, 1935–1947. [Google Scholar] [CrossRef] [PubMed]
- Lindsey, B.W.; Boolani, A.; Merrigan, J.J.; Cortes, N.; Caswell, S.V.; Martin, J.R. Relationship between employment status, reported physical activity, and sitting time during COVID-19 pandemic. J. Phys. Act. Health 2021, 18, 325–328. [Google Scholar] [CrossRef]
- Runacres, A.; Mackintosh, K.A.; Knight, R.L.; Sheeran, L.; Thatcher, R.; Shelley, J.; McNarry, M.A. Impact of the COVID-19 pandemic on sedentary time and behaviour in children and adults: A systematic review and meta-analysis. Int. J. Environ. Res. Public Health 2021, 18, 11286. [Google Scholar] [CrossRef]
- Lesser, I.A.; Nienhuis, C.P. The impact of COVID-19 on physical activity behavior and well-being of Canadians. Int. J. Environ. Res. Public Health 2020, 17, 3899. [Google Scholar] [CrossRef] [PubMed]
- Eek, F.; Larsson, C.; Wisén, A.; Ekvall Hansson, E. Self-perceived changes in physical activity and the relation to life satisfaction and rated physical capacity in Swedish adults during the COVID-19 pandemic—a cross sectional study. Int. J. Environ. Res. Public Health 2021, 18, 671. [Google Scholar] [CrossRef]
- Blom, V.; Lönn, A.; Ekblom, B.; Kallings., L.V.; Väisanen, D.; Hemmingsson, E.; Andersson, G.; Wallin, P.; Stenling, A.; Ekblom, Ö.; et al. Lifestyle habits and mental health in light of the two COVID-19 pandemic waves in Sweden, 2020. Int. J. Environ. Res. Public Health 2021, 18, 3313. [Google Scholar] [CrossRef]
- Vyas, L.; Butakhieo, N. The impact of working from home during COVID-19 on work and life domains: An exploratory study on Hong Kong. Policy Des. Pract. 2020, 4, 59–76. [Google Scholar] [CrossRef]
- Constandt, B.; Thibaut, E.; De Bosscher, V.; Scheerder, J.; Ricour, M.; Willem, A. Exercising in times of lockdown: An analysis of the impact of COVID-19 on levels and patterns of exercise among adults in Belgium. Int. J. Environ. Res. Public Health 2020, 17, 4144. [Google Scholar] [CrossRef]
- Schwendinger, F.; Pocecco, E. Counteracting physical inactivity during the COVID-19 pandemic: Evidence-based recommendations for home-based exercise. Int. J. Environ. Res. Public Health 2020, 17, 3909. [Google Scholar] [CrossRef] [PubMed]
- Michie, S.; van Stralen, M.M.; West, R. The behaviour change wheel: A new method for characterising and designing behaviour change interventions. Implement. Sci. 2011, 6, 42. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gibson Miller, J.; Hartman, T.K.; Levita, L.; Martinez, A.P.; Mason, L.; McBride, O.; McKay, R.; Murphy, J.; Shevlin, M.; Stocks, T.V.A.; et al. Capability, opportunity, and motivation to enact hygienic practices in the early stages of the COVID-19 outbreak in the United Kingdom. Br. J. Health Psychol. 2020, 25, 856–864. [Google Scholar] [CrossRef] [PubMed]
- Stockwell, S.; Trott, M.; Tully, M.; Shin, J.; Barnett, Y.; Butler, L.; McDermott, D.; Schuch, F.; Smith, L. Changes in physical activity and sedentary behaviours from before to during the COVID-19 pandemic lockdown: A systematic review. BMJ Open Sport Exerc. Med. 2021, 7, e000960. [Google Scholar] [CrossRef]
- Caputo, E.L.; Reichert, F.F. Studies of physical activity and COVID-19 during the pandemic: A scoping review. J. Phys. Act. Health 2020, 17, 1275–1284. [Google Scholar] [CrossRef]
- Kavaliunas, A.; Ocaya, P.; Mumper, J.; Lindfeldt, I.; Kyhlstedt, M. Swedish policy analysis for Covid-19. Health Policy Technol. 2020, 9, 598–612. [Google Scholar] [CrossRef]
- World Medical Association. Declaration of Helsinki—Ethical Principles for Medical Research Involving Human Subjects. 2013, Adopted by the 18th WMA General Assembly, Helsinki, Finland, June 1964 (Amended by the 64th WMA General Assembly, Fortaleza, Brazil, October 2013). Available online: https://www.wma.net/policies-post/wma-declaration-of-helsinki-ethical-principles-for-medical-research-involving-human-subjects/ (accessed on 20 January 2022).
- The Swedish Research Council. Good Research Practice. Available online: https://www.vr.se/english/analysis/reports/our-reports/2017-08-31-good-research-practice.html (accessed on 20 January 2022).
- Public Health Agency of Sweden. Available online: https://www.folkhalsomyndigheten.se/smittskydd-beredskap/utbrott/aktuella-utbrott/covid-19/statistik-och-analyser/bekraftade-fall-i-sverige/ (accessed on 20 January 2022).
- Craig, C.L.; Marshall, A.L.; Sjöström, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Pratt, M.; Ekelund, U.; Yngve, A.; Sallis, J.F.; et al. International physical activity questionnaire: 12-country reliability and validity. Med. Sci. Sports Exerc. 2003, 35, 1381–1395. [Google Scholar] [CrossRef] [Green Version]
- Hurst, H.; Bolton, J. Assessing the clinical significance of change scores recorded on subjective outcome measures. J. Manip. Physiol. Ther. 2004, 27, 26–35. [Google Scholar] [CrossRef]
- Keyworth, C.; Epton, T.; Goldthorpe, J.; Calam, R.; Armitage, C.J. Acceptability, reliability, and validity of a brief measure of capabilities, opportunities, and motivations (“COM-B”). Br. J. Health Psychol. 2020, 25, 474–501. [Google Scholar] [CrossRef]
- Karolinska Institutet. Guidelines for Data Processing and Analysis of the International Physical Activity Questionnaire (IPAQ)—Short and Long Forms. Available online: http://www.ipaq.ki.se (accessed on 20 January 2022).
- Field, A. Discovering Statistics Using IBM SPSS Statistics, 4th ed.; Sage: Newcastle Upon Tyne, UK, 2013. [Google Scholar]
- Michie, S.; Rubin, G.J.; Amlot, R. Behavioural Science Must Be at the Heart of the Public Health Response to COVID-19. Available online: https://blogs.bmj.com/bmj/2020/02/28/behavioural-science-must-be-at-the-heart-of-the-public-health-response-to-covid-19/ (accessed on 20 January 2022).
- Knittle, K.; Nurmi, J.; Crutzen, R.; Hankonen, N.; Beattie, M.; Dombrowski, S.U. How can interventions increase motivation for physical activity? A systematic review and meta-analysis. Health Psychol. Rev. 2018, 12, 211–230. [Google Scholar] [CrossRef]
- Spence, J.C.; Rhodes, R.E.; McCurdy, A.; Mangan, A.; Hopkins, D.; Mummery, W.K. Determinants of physical activity among adults in the United Kingdom during the COVID-19 pandemic: The DUK-COVID study. Br. J. Health Psychol. 2021, 26, 588–605. [Google Scholar] [CrossRef] [PubMed]
- Pierce, M.; Hope, H.; Ford, T.; Hatch, S.; Hotopf, M.; John, A.; Kontopantelis, E.; Webb, R.; Wessely, S.; McManus, S.; et al. Mental health before and during the COVID-19 pandemic: A longitudinal probability sample survey of the UK population. Lancet Psychiatry. 2020, 7, 883–892. [Google Scholar] [CrossRef]
- Vindegaard, N.; Benros, M.E. COVID-19 pandemic and mental health consequences: Systematic review of the current evidence. Brain Behav. Immun. 2020, 89, 531–542. [Google Scholar] [CrossRef]
- Higgins, V.; Sohaei, D.; Diamandis, E.P.; Prassas, I. COVID-19: From an acute to chronic disease? Potential long-term health consequences. Crit. Rev. Clin. Lab. Sci. 2021, 58, 297–310. [Google Scholar] [CrossRef] [PubMed]
- Bandura, A. Self-Efficacy: The Exercise of Control; Freeman and Company: New York, NY, USA, 1997. [Google Scholar]
- Rhodes, R.E.; Janssen, I.; Bredin, S.S.D.; Warburton, D.E.R.; Bauman, A. Physical activity: Health impact, prevalence, correlates and interventions. Psychol. Health 2017, 32, 942–975. [Google Scholar] [CrossRef] [PubMed]
- Williams, S.L.; French, D.P. What are the most effective intervention techniques for changing physical activity self-efficacy and physical activity behaviour—And are they the same? Health Educ. Res. 2011, 26, 308–322. [Google Scholar] [CrossRef]
- Ashford, S.; Edmunds, J.; French, D.P. What is the best way to change self-efficacy to promote lifestyle and recreational physical activity? A systematic review with meta-analysis. Br. J. Health Psychol. 2010, 15, 265–288. [Google Scholar] [CrossRef] [Green Version]
- Meyer, J.; McDowell, C.; Lansing, J.; Brower, C.; Smith, L.; Tully, M.; Herring, M. Changes in physical activity and sedentary behavior in response to COVID-19 and their associations with mental health in 3052 US adults. Int. J. Environ. Res. Public Health 2020, 17, 6469. [Google Scholar] [CrossRef]
- Chodzko-Zajko, W.J.; Proctor, D.N.; Fiatarone Singh, M.A.; Minson, C.T.; Nigg, C.R.; Salem, G.J.; Skinner, J.S. Exercise and physical activity for older adults. Med. Sci. Sports Exerc. 2009, 41, 1510–1530. [Google Scholar] [CrossRef]
- Diaz, K.M.; Howard, V.J.; Hutto, B.; Colabianchi, N.; Vena, J.E.; Safford, M.M.; Blair, S.N.; Hooker, S.P. Patterns of sedentary behavior and mortality in U.S. middle-aged and older adults: A national cohort study. Ann. Intern. Med. 2017, 167, 465–475. [Google Scholar] [CrossRef]
- Sprod, J.; Ferrar, K.; Olds, T.; Maher, C. Changes in sedentary behaviours across the retirement transition: A systematic review. Age Ageing 2015, 44, 918–925. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Eklund, C.; Elfström, M.L.; von Heideken Wågert, P.; Söderlund, A.; Gustavsson, C.; Cederbom, S.; Thunborgh, C.; Lööf, H. The meaning of sedentary behavior as experienced by people in the transition from working life to retirement: An empirical phenomenological study. Phys. Ther. 2021, 10, pzab117. [Google Scholar] [CrossRef] [PubMed]
- Castañeda-Babarro, A.; Arbillaga-Etxarri, A.; Gutiérrez-Santamaría, B.; Coca, A. Physical activity change during COVID-19 confinement. Int. J. Environ. Res. Public Health 2020, 17, 6878. [Google Scholar] [CrossRef] [PubMed]
- Lanza, K.; Durand, C.P.; Alcazar, M.; Ehlers, S.; Zhang, K.; Kohl, H.W., III. School parks as a community health resource: Use of joint-use parks by children before and during COVID-19 pandemic. Int. J. Environ. Res. Public Health 2021, 18, 9237. [Google Scholar] [CrossRef]
- Tammelin, T.; Näyhä, S.; Laitinen, J.; Rintamäki, H.; Järvelin, M.R. Physical activity and social status in adolescence as predictors of physical inactivity in adulthood. Prev. Med. 2003, 37, 375–381. [Google Scholar] [CrossRef]
- Kerstis, B.; Giannotta, F.; Wågert, P.V.H.; Hellström, C.; Lindberg, D.; Stier, J.; Elvén, M. Changes in mental health and views on communication and activities of public institutions among Swedes during the COVID-19 Pandemic—A cross-sectional repeated measures design. Healthcare 2021, 9, 1498. [Google Scholar] [CrossRef]
- Bhopal, S.S.; Bagaria, J.; Olabi, B.; Bhopal, R. Children and young people remain at low risk of COVID-19 mortality. Lancet Child Adolesc. Health 2021, 5, e12–e13. [Google Scholar] [CrossRef]
- World Health Organization. WHO Guidelines on Physical Activity and Sedentary Behaviour. Available online: https://apps.who.int/iris/bitstream/handle/10665/336656/9789240015128-eng.pdf?sequence=1&isAllowed=y (accessed on 20 January 2022).
- Lee, P.H.; Macfarlane, D.J.; Lam, T.H.; Stewart, S.M. Validity of the international Physical Activity Questionnaire Short Form (IPAQ-SF): A systematic review. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 115. [Google Scholar] [CrossRef] [Green Version]
- Colley, R.C.; Butler, G.; Garriguet, D.; Prince, S.A.; Roberts, K.C. Comparison of self-reported and accelerometer-measured physical activity in Canadian adults. Health Rep. 2018, 29, 3–15. [Google Scholar]
- Statistics Sweden. Snabba Fakta Om Sverige. Available online: https://www.scb.se/hitta-statistik/snabba-fakta/ (accessed on 20 January 2022).
| Characteristics | n (%) | M (SD) |
|---|---|---|
| Age | 50.6 (16.6) | |
| Sex | ||
| Men | 523 (50.5) | |
| Women | 512 (49.5) | |
| Highest education | ||
| Compulsory school (9 years) | 66 (6.4) | |
| Senior high school | 421 (40.7) | |
| University | 546 (52.8) | |
| Other | 2 (0.2) | |
| Confirmed COVID-19 | ||
| Yes | 55 (5.3) | |
| Chronic disease | ||
| Yes | 180 (17.4) | |
| Occupation | ||
| Students/parental leave | 97 (9.4) | |
| Manual workers | 218 (21.1) | |
| Non-manual workers/Self-employed | 407 (39.3) | |
| Unemployed Sick leave/early retired | 65 (6.3) | |
| Retired | 248 (24.0) | |
| Cohabitation status | ||
| Married/partnership | 494 (47.7) | |
| Living with partner | 217 (21.0) | |
| One person household/single parent | 324 (31.3) | |
| Origin | ||
| Born in Sweden | 930 (92.5) |
| Total PA METs/w Mdn | Vigorous PA METs/w Mdn | Moderate PA METs/w Mdn | Light PA METs/w Mdn | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Before | During | p | Post Hoc | Before | During | p | Post Hoc | Before | During | p | Post hoc | Before | During | p | Post Hoc | |
| Total sample a | 2400 | 1960 | <0.001 | 480 | 32 | <0.001 | 480 | 240 | <0.001 | 792 | 792 | NS | ||||
| Sex a | ||||||||||||||||
| Men | 2556 | 2079 | 0.001 | 480 | 80 | 0.001 | 720 | 400 | 0.001 | 693 | 693 | NS | ||||
| Women | 2317 | 1825 | 0.001 | 480 | 0 | <0.001 | 480 | 240 | 0.001 | 792 | 808 | NS | ||||
| Difference b | NS | NS | NS | NS | ||||||||||||
| Age a | ||||||||||||||||
| 18–26 year | 2758 | 1980 | <0.001 | 960 | 320 | 0.001 | 528 | 240 | 0.001 | 693 | 660 | NS | ||||
| 27–49 year | 1920 | 1733 | <0.001 | 480 | 48 | 0.001 | 360 | 240 | 0.001 | 495 | 660 | 0.001 | ||||
| 50–65 year | 2346 | 2007 | <0.001 | 320 | 0 | 0.001 | 650 | 340 | 0.001 | 792 | 742 | NS | ||||
| 66–79 year | 3066 | 2205 | <0.001 | 320 | 0 | 0.001 | 720 | 320 | 0.001 | 1188 | 1155 | 0.05 | ||||
| Difference c | 0.001 | A > B D > B D > C | 0.03 | <0.001 | D > B D > C | <0.001 | B > D | |||||||||
| Sedentary Behavior Minutes/Week Mdn (IQR) | |||
|---|---|---|---|
| Before | During | p | |
| Total sample a | 2520 (2520) | 3150 (2100) | <0.001 |
| Sex a | |||
| Men | 2534 (2520) | 3360 (2310) | <0.001 |
| Women | 2520 (2520) | 2940 (2100) | <0.001 |
| Difference in change in sedentary behavior between men and women b | 0.05 | ||
| Age a | |||
| 18–26 year | 3360 (2310) | 4095 (2940) | 0.001 |
| 27–49 year | 3360 (2517) | 3360 (2555) | 0.001 |
| 50–65 year | 2520 (2100) | 2940 (2100) | 0.001 |
| 66–79 year | 2100 (1313) | 2310 (1680) | 0.001 |
| Difference in change in PA between age groups c | NS | ||
| Parameter | B (95% CI) | SE B | β | p |
|---|---|---|---|---|
| Step 1 | ||||
| Capability | 0.13 (0.10–0.15) | 0.01 | 0.31 | <0.001 |
| Step 2 | ||||
| Capability | 0.12 (0.09–0.15) | 0.02 | 0.29 | <0.001 |
| Opportunity | 0.01(−0.02–0.04) | 0.02 | 0.02 | NS |
| Step 3 | ||||
| Capability | 0.12 (0.09–0.15) | 0.02 | 0.30 | <0.001 |
| Opportunity | 0.01 (−0.02–0.04) | 0.02 | 0.02 | NS |
| Motivation | −0.01 (−0.03–0.02) | 0.01 | −0.02 | NS |
| Step 4 | ||||
| Capability | 0.12 (0.09–0.15) | 0.02 | 0.30 | <0.001 |
| Opportunity | 0.01 (−0.02–0.04) | 0.02 | 0.03 | NS |
| Motivation | −0.01 (−0.03–0.01) | 0.01 | −0.02 | NS |
| Age | −0.01 (−0.01–0.01) | 0.00 | −0.07 | 0.02 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Elvén, M.; Kerstis, B.; Stier, J.; Hellström, C.; von Heideken Wågert, P.; Dahlen, M.; Lindberg, D. Changes in Physical Activity and Sedentary Behavior before and during the COVID-19 Pandemic: A Swedish Population Study. Int. J. Environ. Res. Public Health 2022, 19, 2558. https://doi.org/10.3390/ijerph19052558
Elvén M, Kerstis B, Stier J, Hellström C, von Heideken Wågert P, Dahlen M, Lindberg D. Changes in Physical Activity and Sedentary Behavior before and during the COVID-19 Pandemic: A Swedish Population Study. International Journal of Environmental Research and Public Health. 2022; 19(5):2558. https://doi.org/10.3390/ijerph19052558
Chicago/Turabian StyleElvén, Maria, Birgitta Kerstis, Jonas Stier, Charlotta Hellström, Petra von Heideken Wågert, Micael Dahlen, and Daniel Lindberg. 2022. "Changes in Physical Activity and Sedentary Behavior before and during the COVID-19 Pandemic: A Swedish Population Study" International Journal of Environmental Research and Public Health 19, no. 5: 2558. https://doi.org/10.3390/ijerph19052558
APA StyleElvén, M., Kerstis, B., Stier, J., Hellström, C., von Heideken Wågert, P., Dahlen, M., & Lindberg, D. (2022). Changes in Physical Activity and Sedentary Behavior before and during the COVID-19 Pandemic: A Swedish Population Study. International Journal of Environmental Research and Public Health, 19(5), 2558. https://doi.org/10.3390/ijerph19052558








