The COVID-19 Pandemic Crisis and Patient Safety Culture: A Mixed-Method Study
Abstract
1. Introduction
2. Methods
2.1. Survey Instrument
2.2. Study Procedure
2.3. Ethical Permission
2.4. Statistical Analysis
3. Results
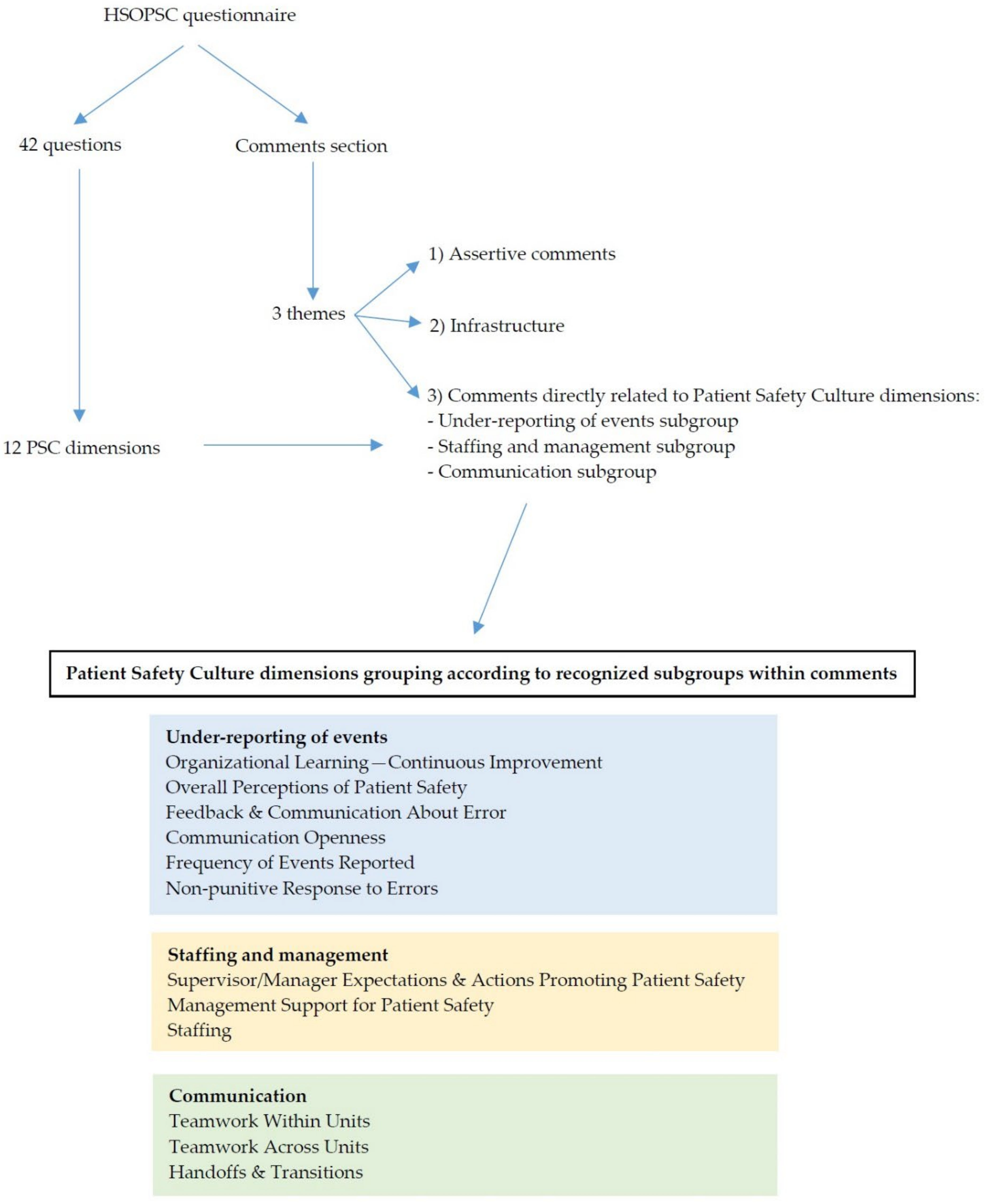
3.1. Qualitative Analysis of the Comments Sections
- In the “Assertive Comments” theme group, comments were expressed as praise for this research and acknowledgment that the patients were safe in this hospital (Table 2):“Praise for the chosen subject. We should talk about patient safety more and change attitudes. It is necessary to put emphasis on, and familiarize employees with, patient safety”;“The patients are safe in our hands”.
- The “Infrastructure” theme (Table 2) revealed concern for the infrastructure of the hospital building, its sanitation (water and power outages) and the state of its equipment. Some of the comments are expressed below and in Table 2:“I don’t consider the water drinkable—it is often brown, and it is embarrassing to explain to patients that it is potable when I wouldn’t drink it myself!”;“It was challenging to complete this survey given that the Hospital is ancient, worn out, in poor repair and further destroyed by the earthquake”;“In addition to the items examined, the hospital’s infrastructure needs to be changed to improve staff working conditions and patient safety!”; “Cribs are without fences (the bed is enclosed with room chairs if necessary), oxygen bottles without stands and insufficiently attached to the frame, so they sometimes roll over on the floor in the patient’s room, the valves on the oxygen bottles loosen and hiss as they run out of rubber, in the external staircase through which staff pass and enter, plaster is falling from the walls, brown tap water”.
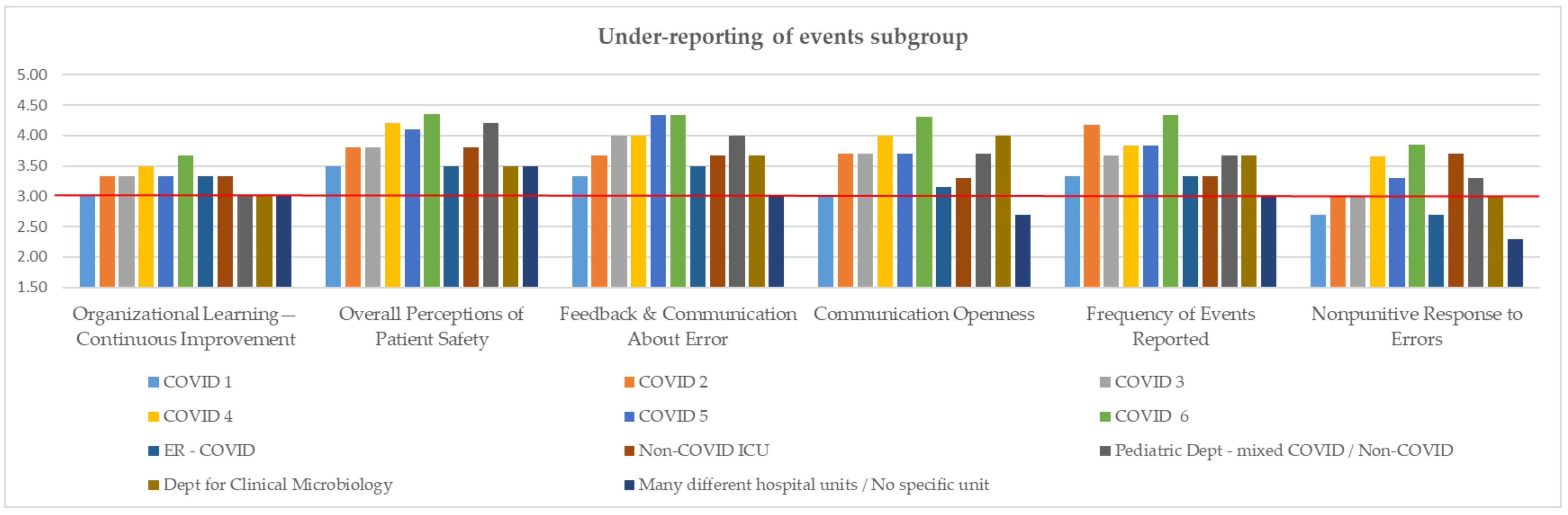
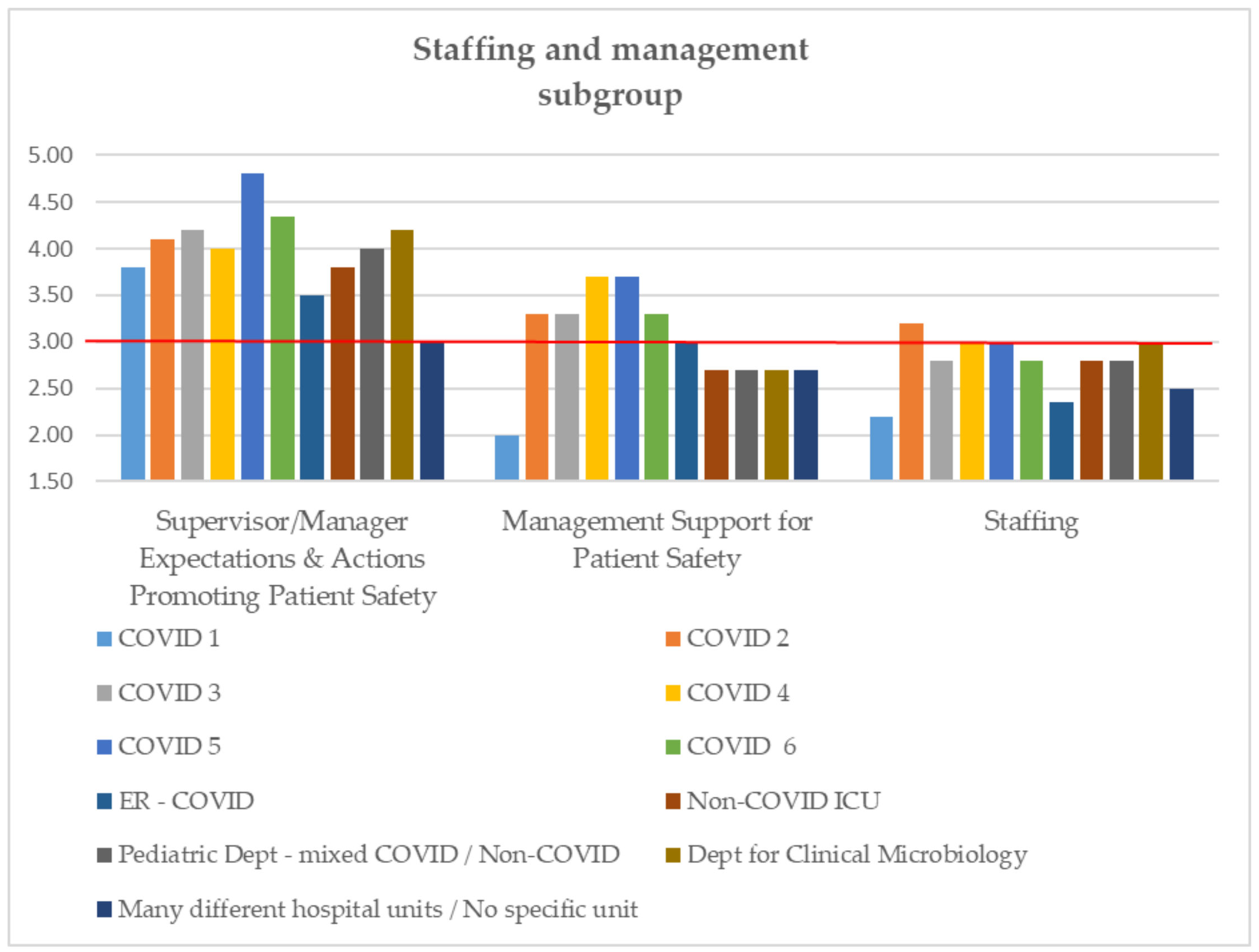
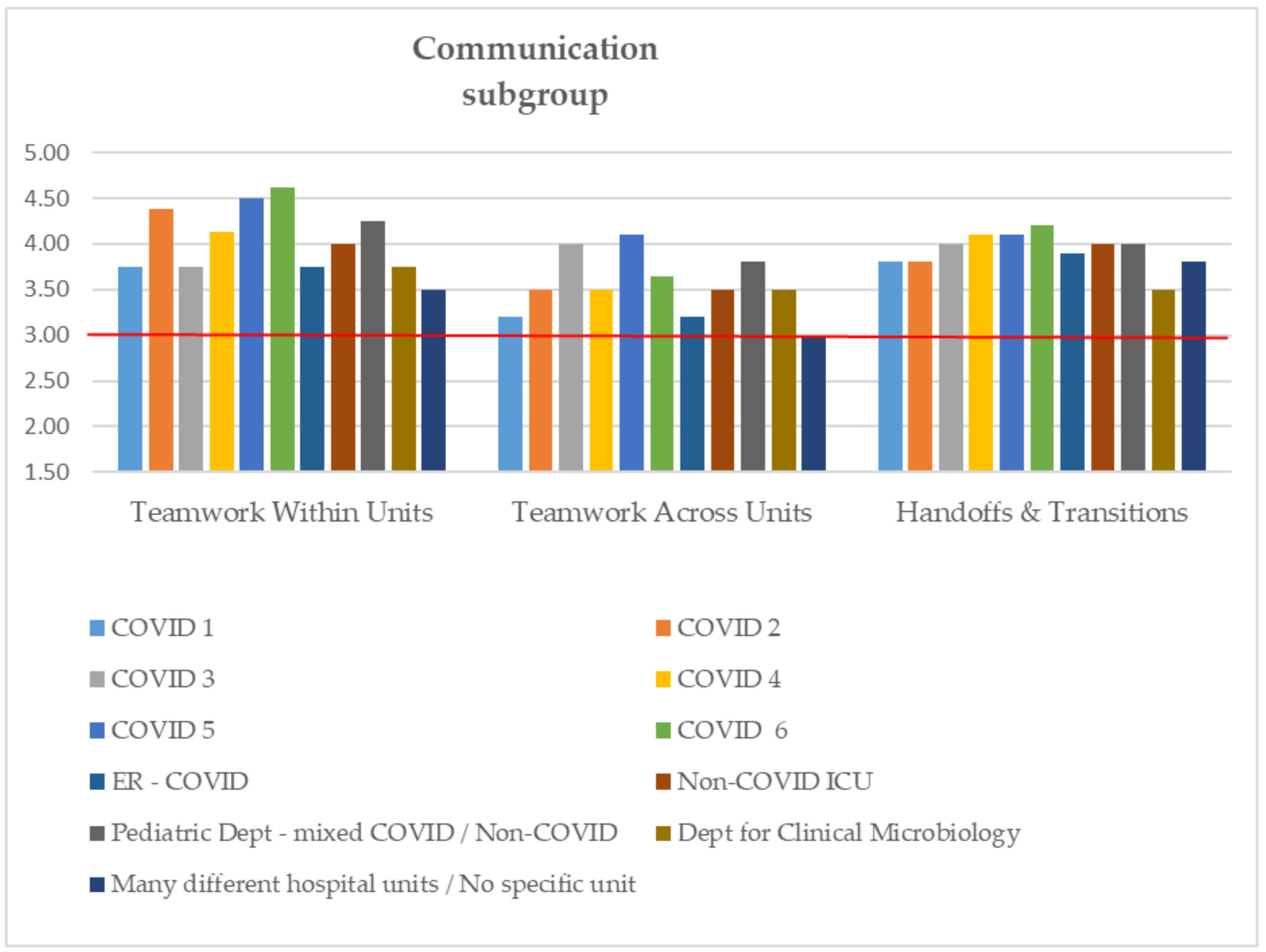
- The “Detailed Answers to Patient Safety Culture Dimensions” theme revealed three subgroups that preoccupied the participants: (1) “Under-reporting of events”, (2) “Staffing and management” and (3) “Communication” (Table 2).
“This was, and still is, the taboo theme. Instead of learning from mistakes, extracting some positive message, and changing the mode of operation, such things get hushed up, nobody is informed about them, and the staff are repeatedly warned they will be placed on their superiors’ ‘black list’”;“Systematic problem solving is not done, only solving individual cases”;
“Too few nurses, porters and auxiliary staff. We are entirely out of protection. Other institutions have security guards”;“If he had employed more nurses, patient safety would be higher, and therefore unwanted events fewer”;“A reduction in the number of patient beds in the department or an increase in the number of nurses in the shift, depending on the severity of the patients’ medical issues, would reduce the number of errors and unwanted events. The patients would be safer”.
“Better communication with epidemiologists”;“Medical findings/hospital records should be delivered by mail to the outpatient patients under a unique code”;“Inadequate communication across the department”.
3.2. Quantitative Analysis—Analysis of the PSC Dimensions Arranged in the Three Subgroups According to the “Detailed Answers to Patient Safety Culture Dimensions” Group from the Qualitative Data Analysis
3.3. Single-Question Responses
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Centers for Disease Control and Prevention. Appendix 2. Terminology. Available online: https://www.cdc.gov/infectioncontrol/guidelines/healthcare-personnel/appendix/terminology.html (accessed on 4 December 2021).
- Health Protection Surveillance Centre. Definition of a Healthcare Worker. Available online: https://www.hpsc.ie/notifiablediseases/casedefinitions/healthcareworkerdefinition/ (accessed on 4 December 2021).
- WHO. Patient Safety. Available online: https://www.euro.who.int/en/health-topics/Health-systems/patient-safety/patient-safety (accessed on 4 December 2021).
- Centers for Disease Control and Prevention; The National Institute for Occupational Safety and Health (NIOSH). Healthcare Workers. Available online: https://www.cdc.gov/niosh/topics/healthcare/default.html (accessed on 4 December 2021).
- HZJZ. Hrvatski Zavod za Javno Zdravstvo—Služba za Medicinu Rada. Profesionalne Bolesti u Republici Hrvatskoj. Available online: http://www.hzzzsr.hr/index.php/porefesionalne-bolesti-i-ozljede-na-radu/profesionalne-bolesti/profesionalne-bolesti-u-republici-hrvatskoj/ (accessed on 4 December 2021).
- Brborović, H.; Šklebar, I.; Brborović, O.; Brumen, V.; Mustajbegović, J. Development of a Croatian version of the US Hospital Survey on Patient Safety Culture questionnaire: Dimensionality and psychometric properties. Postgrad. Med. J. 2014, 90, 125–132. [Google Scholar] [CrossRef] [PubMed]
- Nieva, V.F.; Sorra, J. Safety culture assessment: A tool for improving patient safety in healthcare organizations. Qual. Saf. Health Care 2003, 12, 1117–1123. [Google Scholar] [CrossRef] [PubMed]
- Pronovost, P.; Sexton, B. Assessing safety culture: Guidelines and recommendations. Qual. Saf. Health Care 2005, 14, 231–233. [Google Scholar] [CrossRef] [PubMed]
- Culture of Safety: An Overview. Available online: https://www.ecri.org/components/HRC/Pages/RiskQual21.aspx#:~:text=Patient%20safety%20culture%20is%20the,of%20staff%20throughout%20the%20organization (accessed on 4 December 2021).
- Rangachari, P.; Woods, J.L. Preserving Organizational Resilience, Patient Safety, and Staff Retention during COVID-19 Requires a Holistic Consideration of the Psychological Safety of Healthcare Workers. Int. J. Environ. Res. Public Health 2020, 17, 4267. [Google Scholar] [CrossRef] [PubMed]
- The COVID-19 Crisis Too Few Are Talking about: Health Care Workers’ Mental Health. Available online: https://www.statnews.com/2020/04/03/the-covid-19-crisis-too-few-are-talking-about-health-careworkers-mental-health/ (accessed on 1 May 2020).
- Lai, J.; Ma, S.; Wang, Y.; Cai, Z.; Hu, J.; Wei, N.; Wu, J.; Du, H.; Chen, T.; Li, R.; et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw. Open 2020, 3, e203976. [Google Scholar] [CrossRef]
- Santarone, K.; McKenney, M.; Elkbuli, A. Preserving mental health and resilience in frontline healthcare workers during COVID-19. Am. J. Emerg. Med. 2020, 38, 1530–1531. [Google Scholar] [CrossRef]
- Bolcato, M.; Aurilio, M.T.; Aprile, A.; Di Mizio, G.; Della Pietra, B.; Feola, A. Take-Home Messages from the COVID-19 Pandemic: Strengths and Pitfalls of the Italian National Health Service from a Medico-Legal Point of View. Healthcare 2021, 9, 17. [Google Scholar] [CrossRef]
- In Fight against COVID-19, Nurses Face High-Stakes Decisions, Moral Distress. Available online: https://hub.jhu.edu/2020/04/06/covid-nursing-cynda-rushton-qa/ (accessed on 30 November 2021).
- Clark, L.; Stephens, A.F.; Liao, S.; Byrne, T.J.; Gregory, S.D. Coping with COVID-19: Ventilator splitting with differential driving pressure using standard hospital equipment. Anesthesia 2020, 75, 872–880. [Google Scholar] [CrossRef]
- Government of the Republic of Croatia. Coronavirus Protection Measures. Available online: https://vlada.gov.hr/coronavirus-protection-measures/28950 (accessed on 4 December 2021).
- Koronavirus.hr. Smjernice za Liječenje Oboljelih od COVID-19. Available online: https://www.koronavirus.hr/smjernice-za-lijecenje-oboljelih-od-covid-19/805 (accessed on 4 December 2021).
- Ministarstvo Zdravstva Republike Hrvatske. Smjernice za Liječenje Oboljelih od Koronavirusne Bolesti 2019 (COVID-19) Verzija 3 od 21. Listopada 2021. Available online: https://www.hzjz.hr/wp-content/uploads/2021/11/Smjernice-za-lije%C4%8Denje-oboljelih-od-koronavirusne-bolesti-2019-COVID-19-verzija-3-od-21-listopada-2021.-godine.pdf (accessed on 4 December 2021).
- The Great Unknown: How Many Health CareWorkers Have Coronavirus? Available online: https://www.usnews.com/news/national-news/articles/2020-04-03/how-many-health-care-workers-have-coronavirus (accessed on 30 November 2021).
- Huang, J.; Liu, F.; Teng, Z.; Chen, J.; Zhao, J.; Wang, X.; Wu, R. Care for the psychological status of frontline medical staff fighting against COVID-19. Clin. Infect. Dis. 2020, 71, 3268–3269. [Google Scholar] [CrossRef]
- Chen, Q.; Liang, M.; Li, Y.; Guo, J.; Fei, D.; Wang, L.; He, L.; Sheng, C.; Cai, Y.; Li, X.; et al. Mental health care for medical staff in China during the COVID-19 outbreak. Lancet Psychiatry 2020, 7, e15–e16. [Google Scholar] [CrossRef]
- Sani, G.; Janiri, D.; Di Nicola, M.; Janiri, L.; Ferretti, S.; Chieffo, D. Mental health during and after the COVID-19 emergency in Italy. Psychiatry Clin. Neurosci. 2020, 74, 372. [Google Scholar] [CrossRef] [PubMed]
- Jun, J.; Tucker, S.; Melnyk, B. Clinician mental health and well-being during global healthcare crisis: Evidence learned from prior epidemics for COVID-19 pandemic. Worldviews Evid. Based Nurs. 2020, 17, 182–184. [Google Scholar] [CrossRef] [PubMed]
- Shanafelt, T.; Ripp, J.; Trockel, M. Understanding and addressing sources of anxiety among health care professionals during the COVID-19 pandemic. JAMA 2020, 323, 2133–2134. [Google Scholar] [CrossRef]
- Brborović, O.; Brborović, H.; Nola, I.A.; Milošević, M. Culture of Blame—An Ongoing Burden for Doctors and Patient Safety. Int. J. Environ. Res. Public Health 2019, 16, 4826. [Google Scholar] [CrossRef]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Mesarić, J.; Mandelsamen Perica, M.; Hađić Kostrenčić, K. (Eds.) Izvješće o Neočekivanim Neželjenim Događajima za 2017. Godinu; Agencija za Kvalitetu i Akreditaciju u Zdravstvu i Socijalnoj Skrbi: Zagreb, Croatia, 2018; Available online: https://www.aaz.hr/sites/default/files/Izvjesca_NND_NDPO_2017_godina.pdf (accessed on 18 November 2021).
- Mesarić, J.; Hadžić-Kostrenčić, K.; Frketić, D. Izviješće o Radu Povjerenstva za Kvalitetu Zdravstvene Ustanove 2017. Available online: http://www.aaz.hr/sites/default/files/Izvjesce_o_radu_povjerenstva_2017.pdf (accessed on 16 November 2021).
- Denning, M.; Goh, E.T.; Scott, A.; Martin, G.; Markar, S.; Flott, K.; Mason, S.; Przybylowicz, J.; Almonte, M.; Clarke, J.; et al. What Has Been the Impact of COVID-19 on Safety Culture? A Case Study from a Large Metropolitan Healthcare Trust. Int. J. Environ. Res. Public Health 2020, 17, 7034. [Google Scholar] [CrossRef] [PubMed]
- Hooper, P.; Kocman, D.; Carr, S.; Tarrant, C. Junior doctors’ views on reporting concerns about patient safety: A qualitative study. Postgrad. Med. J. 2015, 91, 251–256. [Google Scholar] [CrossRef]
- Šklebar, I.; Mustajbegović, J.; Šklebar, D.; Cesarik, M.; Milošević, M.; Brborović, H.; Šporčić, K.; Petrić, P.; Husedžinović, I. How to Improve Patient Safety Culture in Croatian Hospitals? Acta Clin. Croat. 2016, 55, 370–380. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Brborović, H.; Brborović, O. Patient safety culture shapes presenteeism and absenteeism: A cross-sectional study among Croatian healthcare workers. Arhiv za Higijenu Rada i Toksikologiju 2017, 68, 185–189. [Google Scholar] [CrossRef]
- Health Workforce. Available online: https://www.who.int/health-topics/health-workforce#tab=tab_1 (accessed on 30 November 2021).
- United Nations University; Institute for Environment and Human Security. Five Things You Need to Know about Health Infrastructures. Available online: https://ehs.unu.edu/news/news/five-things-you-need-to-know-about-health-infrastructures.html (accessed on 4 December 2021).
- Ward, M.; Ní Shé, É.; De Brún, A.; Korpos, C.; Hamza, M.; Burke, E.; Duffy, A.; Egan, K.; Geary, U.; Holland, C.; et al. The co-design, implementation and evaluation of a serious board game ‘PlayDecide patient safety’ to educate junior doctors about patient safety and the importance of reporting safety concerns. BMC Med. Educ. 2019, 19, 232. [Google Scholar] [CrossRef]
- McCarthy, S.E.; O’Boyle, C.A.; O’Shaughnessy, A.; Walsh, G. Online patient safety education programme for junior doctors: Is it worthwhile? Ir. J. Med. Sci. 2016, 185, 51–58. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Brennan, P.A.; Davidson, M. Improving patient safety: We need to reduce hierarchy and empower junior doctors to speak up. BMJ 2019, 366, l4461. [Google Scholar] [CrossRef] [PubMed]
| Safety Culture Dimensions (Unit Level) | Questions | ||
|---|---|---|---|
| 1 | Supervisor/Manager Expectations and Actions Promoting Safety | B1 | My supervisor/manager says a good word when he/she sees a job done according to established patient safety procedures |
| B2 | My supervisor/manager seriously considers staff suggestions for improving patient safety | ||
| B3r | Whenever pressure builds up, my supervisor/manager wants us to work faster, even if it means taking shortcuts (reverse worded) | ||
| B4r | My supervisor/manager overlooks patient safety problems that happen over and over (reverse worded) | ||
| 2 | Organizational Learning—Continuous Improvement | A6 | We are actively doing things to improve patient safety |
| A9 | Mistakes have led to positive changes here | ||
| A13 | After we make changes to improve patient safety, we evaluate their effectiveness | ||
| 3 | Teamwork Within Hospital Units | A1 | People support one another in this unit |
| A3 | When a lot of work needs to be done quickly, we work together as a team to get the work done | ||
| A4 | In this unit, people treat each other with respect. | ||
| A11 | When one area in this unit gets really busy, others help out | ||
| 4 | Communication Openness | C2 | Staff will freely speak up if they see something that may negatively affect patient care |
| C4 | Staff feel free to question the decisions or actions of those with more authority | ||
| C6r | Staff are afraid to ask questions when something does not seem right (reverse worded) | ||
| 5 | Feedback and Communication About Error | C1 | We are given feedback about changes put into place based on event reports |
| C3 | We are informed about errors that happen in this unit | ||
| C5 | In this unit, we discuss ways to prevent errors from happening again | ||
| 6 | Non-punitive Response To Error | A8r | Staff feel like their mistakes are held against them (reverse worded) |
| A12r | When an event is reported, it feels like the person is being written up, not the problem (reverse worded) | ||
| A16r | Staff worry that mistakes they make are kept in their personnel file (reverse worded) | ||
| 7 | Staffing | A2 | We have enough staff to handle the workload. |
| A5r | Staff in this unit work longer hours than is best for patient care (reverse worded) | ||
| A7r | We use more agency/temporary staff than is best for patient care (reverse worded) | ||
| A14r | We work in “crisis mode,” trying to do too much, too quickly (reverse worded) | ||
| 8 | Hospital Management Support for Patient Safety | F1 | Hospital management provides a work climate that promotes patient safety |
| F8 | The actions of hospital management show that patient safety is a top priority | ||
| F9r | Hospital management seems interested in patient safety only after an adverse event happens (reverse worded) | ||
| Safety Culture Dimensions (Hospital-wide) | |||
| 9 | Teamwork Across Hospital Units | F4 | There is good cooperation among hospital units that need to work together |
| F10 | Hospital units work well together to provide the best care for patients | ||
| F2r | Hospital units do not coordinate well with each other (reverse worded) | ||
| F6r | It is often unpleasant to work with staff from other hospital units (reverse worded) | ||
| 10 | Hospital Handoffs & Transitions | F3r | Things “fall between the cracks” when transferring patients from one unit to another (reverse worded) |
| F5r | Important patient care information is often lost during shift changes (reverse worded) | ||
| F7r | Problems often occur in the exchange of information across hospital units (reverse worded) | ||
| F11r | Shift changes are problematic for patients in this hospital (reverse worded) | ||
| Outcome Measures | |||
| 11 | Frequency of Event Reporting | D1 | When a mistake is made, but is caught and corrected before affecting the patient, how often is this reported? |
| D2 | When a mistake is made, but has no potential to harm the patient, how often is this reported? | ||
| D3 | When a mistake is made that could harm the patient, but does not, how often is this reported? | ||
| 12 | Overall Perceptions of Safety | A15 | Patient safety is never sacrificed to get more work done |
| A18 | Our procedures and systems are good at preventing errors from happening | ||
| A10r | It is just by chance that more serious mistakes don’t happen around here (reverse worded) | ||
| A17r | We have patient safety problems in this unit (reverse worded) | ||
| Patient Safety Grade * | E1 | Please give your work area/unit in this hospital an overall grade on patient safety | |
| Number of Events Reported ** | G1 | In the past 12 months, how many event reports have you filled out and submitted? | |
| Themes (Groups) | Subgroups | Comments |
|---|---|---|
| Comments Directly Related to Patient Safety Culture Dimensions | Under-reporting of events | “This was, and still is, the taboo theme. Instead of learning from mistakes, extracting some positive message, and changing the mode of operation, such things get hushed up, nobody is informed about them, and the staff are repeatedly warned they will be placed on their superiors’ ‘black list’”; “Systematic problem solving is not done, only solving individual cases.” “In my opinion, adverse events are under-reported. If we want things to change, we must know what went wrong!” |
| Staffing and management | “Too few nurses, porters and auxiliary staff. We are entirely out of protection. Other institutions have security guards”; “If he had employed more nurses, patient safety would be higher, and therefore unwanted events fewer”; “A reduction in the number of patient beds in the department or an increase in the number of nurses in the shift, depending on the severity of the patients’ medical issues, would reduce the number of errors and unwanted events. The patients would be safer” | |
| Communication | “Better communication with epidemiologists”; “Medical findings/hospital records should be delivered by mail to the outpatient patients under a unique code”; “Inadequate communication across the department” | |
| Infrastructure | “I don’t consider the water drinkable—it is often brown, and it is embarrassing to explain to patients that it is potable when I wouldn’t drink it myself!”; “It was challenging to complete this survey given that the Hospital is ancient, worn out, in poor repair and further destroyed by the earthquake.”; “In addition to the items examined, the hospital’s infrastructure needs to be changed to improve staff working conditions and patient safety!”; “Occasionally there is a power outage”; “Very often, security is at stake because of the infrastructure barrier.”; “Cribs are without fences (the bed is enclosed with room chairs if necessary), oxygen bottles without stands and insufficiently attached to the frame, so they sometimes roll over on the floor in the patient’s room, the valves on the oxygen bottles loosen and hiss as they run out of rubber, in the external staircase through which staff pass and enter, plaster is falling from the walls, brown tap water” | |
| Assertive Comments | “Praise for the chosen subject. We should talk about patient safety more and change attitudes. It is necessary to put emphasis on, and familiarize employees with, patient safety”; “The patients are safe in our hands” | |
| Themes (Groups) | Subgroups | Recognized PSC Dimensions |
|---|---|---|
| Comments Directly Related to Patient Safety Culture Dimensions | Under-reporting of events | Organizational Learning—Continuous Improvement |
| Overall Perceptions of Patient Safety | ||
| Feedback & Communication About Errors | ||
| Communication Openness | ||
| Frequency of Events Reported | ||
| Non-punitive Response to Errors | ||
| Staffing and management | Supervisor/Manager Expectations & Actions Promoting Patient Safety | |
| Management Support for Patient Safety | ||
| Staffing | ||
| Communication | Teamwork Within Units | |
| Teamwork Across Units | ||
| Handoffs & Transitions | ||
| Infrastructure | Possible new PSC dimension | |
| Assertive Comments | / | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Brborović, O.; Brborović, H.; Hrain, L. The COVID-19 Pandemic Crisis and Patient Safety Culture: A Mixed-Method Study. Int. J. Environ. Res. Public Health 2022, 19, 2237. https://doi.org/10.3390/ijerph19042237
Brborović O, Brborović H, Hrain L. The COVID-19 Pandemic Crisis and Patient Safety Culture: A Mixed-Method Study. International Journal of Environmental Research and Public Health. 2022; 19(4):2237. https://doi.org/10.3390/ijerph19042237
Chicago/Turabian StyleBrborović, Ognjen, Hana Brborović, and Leonarda Hrain. 2022. "The COVID-19 Pandemic Crisis and Patient Safety Culture: A Mixed-Method Study" International Journal of Environmental Research and Public Health 19, no. 4: 2237. https://doi.org/10.3390/ijerph19042237
APA StyleBrborović, O., Brborović, H., & Hrain, L. (2022). The COVID-19 Pandemic Crisis and Patient Safety Culture: A Mixed-Method Study. International Journal of Environmental Research and Public Health, 19(4), 2237. https://doi.org/10.3390/ijerph19042237







