Virtual Reality Aided Therapy towards Health 4.0: A Two-Decade Bibliometric Analysis
Abstract
1. Introduction
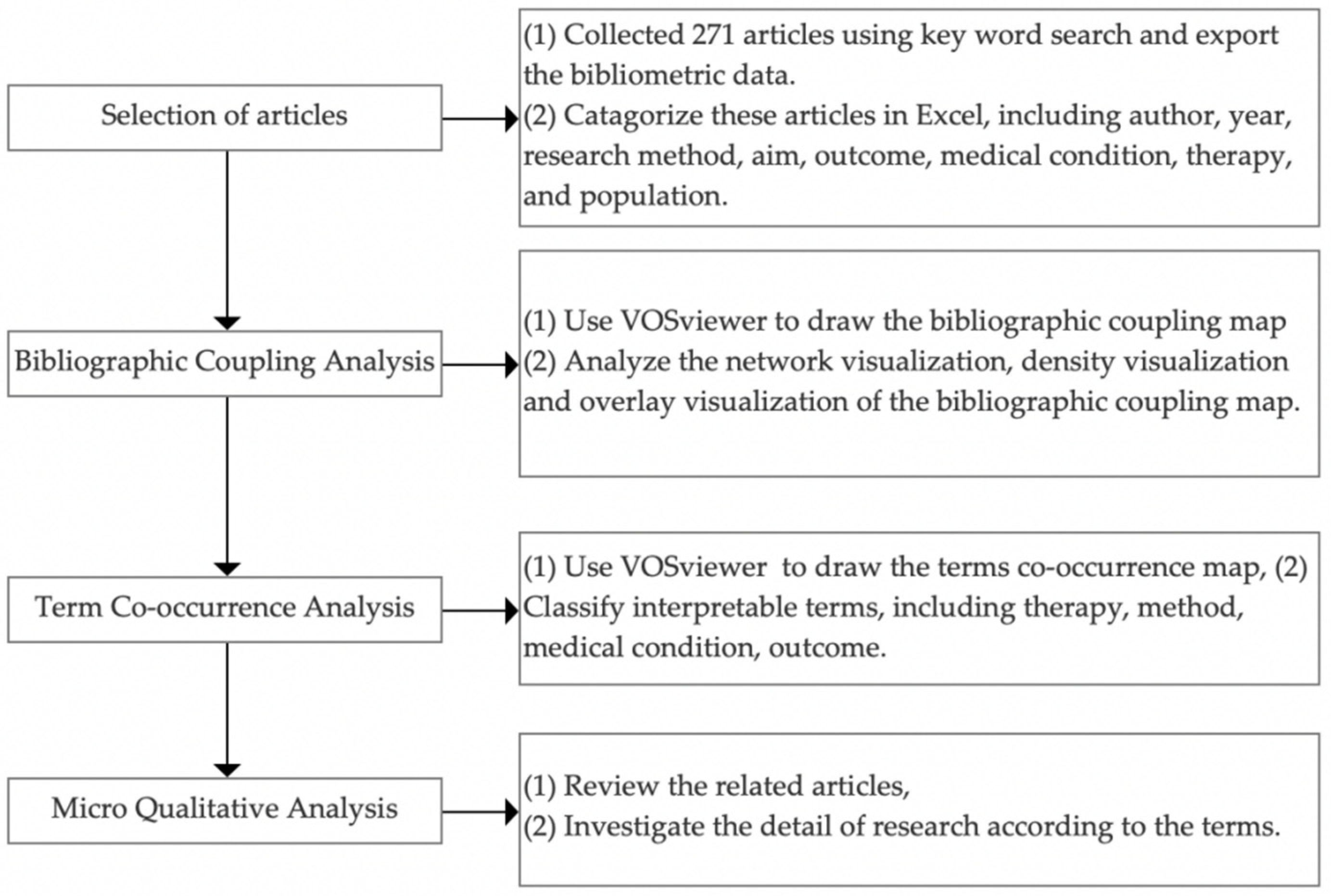
2. Materials and Methods
3. Results
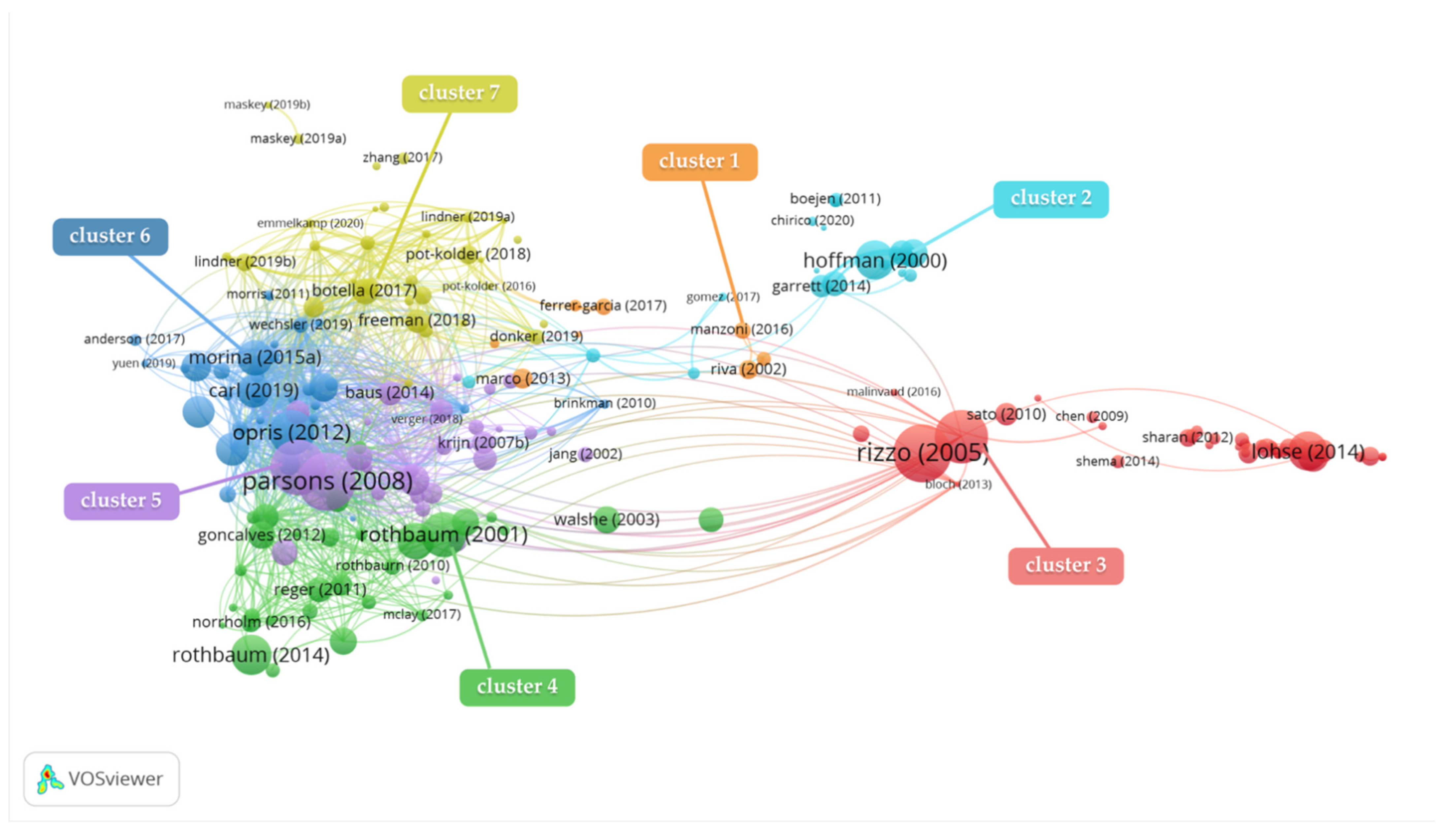
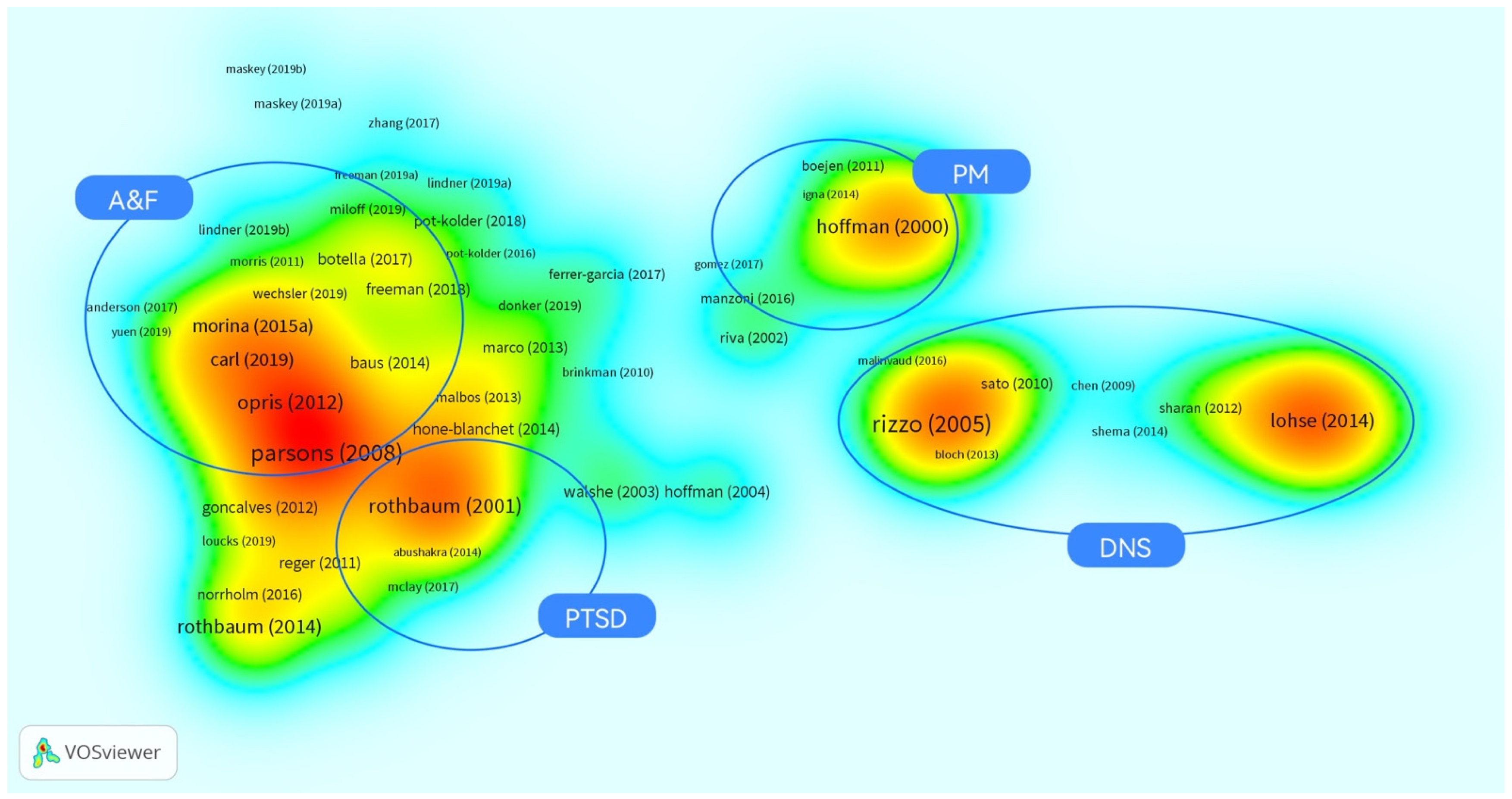
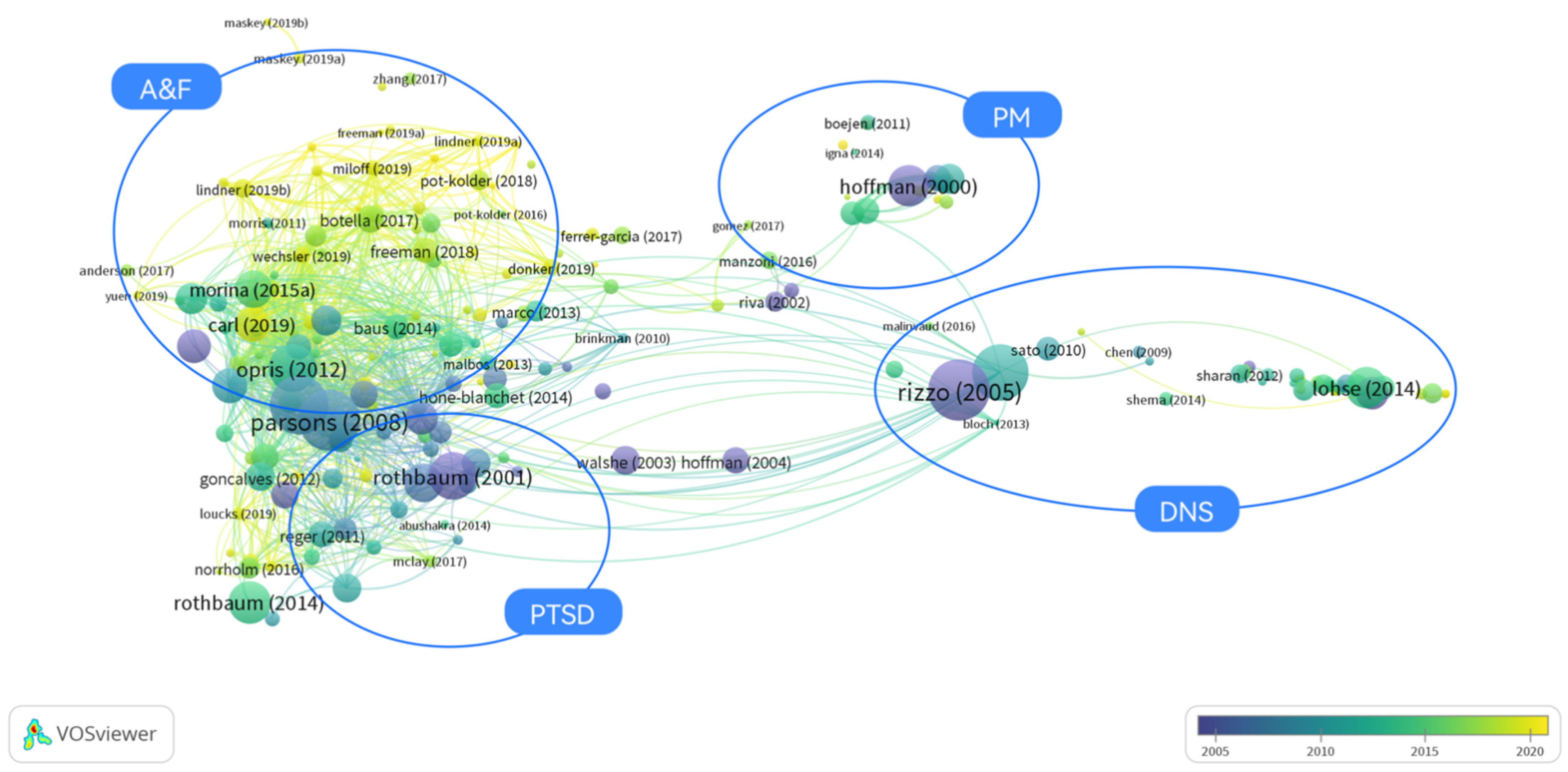
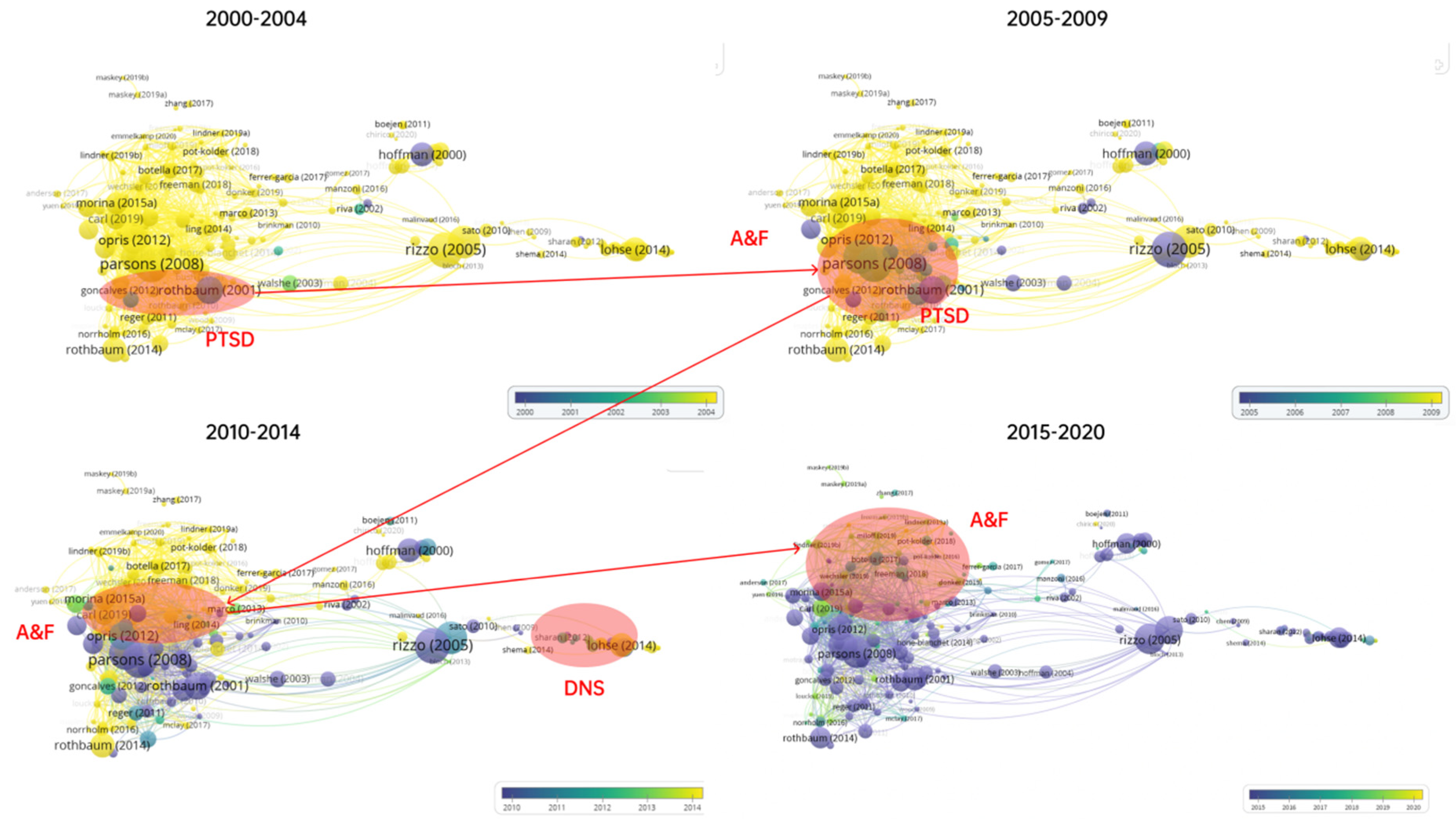
3.1. Results of the Bibliographic Coupling Analysis (BCA)
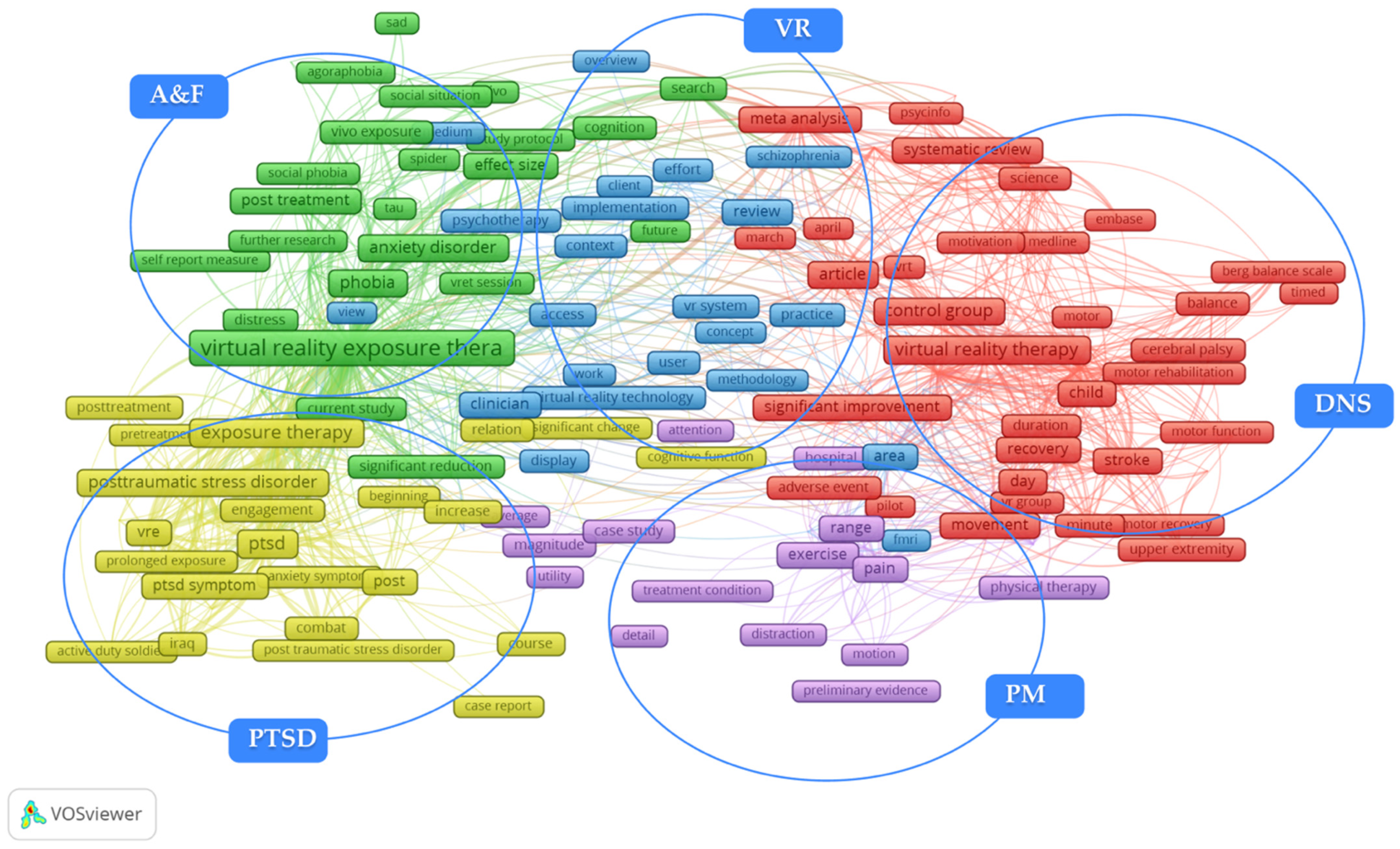
3.2. Results of Terms Co-Occurrence Analysis (TCA)
3.3. Micro Qualitative Analysis
3.3.1. Post-Traumatic Stress Disorder (PTSD)
3.3.2. Anxiety and Fear Related Disorder (A&F)
3.3.3. Diseases of the Nervous System (DNS)
3.3.4. Pain Management (PM)
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Otorkpa, D. World Health Organization (WHO) Definition of Health-Public Health 2019. Available online: https://www.publichealth.com.ng/world-health-organizationwho-definition-of-health/ (accessed on 23 August 2021).
- World Health Organization. Health in 2015: From MDGs, Millennium Development Goals to SDGs, Sustainable Development Goals; World Health Organ: Geneva, Switzerland, 2015. [Google Scholar]
- Desa, U.N. Transforming Our World: The 2030 Agenda for Sustainable Development. Available online: https://sustainabledevelopment.un.org/post2015/transformingourworld (accessed on 15 December 2021).
- Stenberg, K.; Hanssen, O.; Edejer, T.T.-T.; Bertram, M.; Brindley, C.; Meshreky, A.; Rosen, J.E.; Stover, J.; Verboom, P.; Sanders, R.; et al. Financing transformative health systems towards achievement of the health Sustainable Development Goals: A model for projected resource needs in 67 low-income and middle-income countries. Lancet Glob. Health 2017, 5, e875–e887. [Google Scholar] [CrossRef]
- Ortiz-Ospina, E.; Roser, M. Global Health. Our World Data. Available online: https://ourworldindata.org/health-meta (accessed on 15 December 2021).
- Porter, M.E. What Is Value in Health Care? N. Engl. J. Med. 2010, 363, 2477–2481. [Google Scholar] [CrossRef] [PubMed]
- Al-Jaroodi, J.; Mohamed, N.; Abukhousa, E. Health 4.0: On the Way to Realizing the Healthcare of the Future. IEEE Access 2020, 8, 211189–211210. [Google Scholar] [CrossRef] [PubMed]
- Thuemmler, C.; Bai, C. Health 4.0: Application of Industry 4.0 Design Principles in Future Asthma Management. In Health 4.0: How Virtualization and Big Data Are Revolutionizing Healthcare; Thuemmler, C., Bai, C., Eds.; Springer International Publishing: Cham, Switzerland, 2017; pp. 23–37. [Google Scholar] [CrossRef]
- Bause, M.; Esfahani, B.K.; Forbes, H.; Schaefer, D. Design for Health 4.0: Exploration of a New Area. Proc. Des. Soc. Int. Conf. Eng. Des. 2019, 1, 887–896. [Google Scholar] [CrossRef]
- Lanyi, C.S. Virtual Reality in Healthcare. In Intelligent Paradigms for Assistive and Preventive Healthcare; Ichalkaranje, N., Ichalkaranje, A., Jain, L.C., Eds.; Springer: Berlin/Heidelberg, Germany, 2006; pp. 87–116. [Google Scholar] [CrossRef]
- Chow, H.; Hon, J.; Chua, W.; Chuan, A. Effect of Virtual Reality Therapy in Reducing Pain and Anxiety for Cancer-Related Medical Procedures: A Systematic Narrative Review. J. Pain Symptom Manag. 2021, 61, 384–394. [Google Scholar] [CrossRef]
- Junaid, T. Virtual reality in Medicine and Healthcare. Available online: https://www.researchgate.net/publication (accessed on 15 December 2021).
- Cacho-Elizondo, S.; Álvarez, J.-D.L.; Garcia, V.-E. Assessing the Opportunities for Virtual, Augmented, and Diminished Reality in the Healthcare Sector. In The Digitization of Healthcare: New Challenges and Opportunities; Menvielle, L., Audrain-Pontevia, A.-F., Menvielle, W., Eds.; Palgrave Macmillan: London, UK, 2017; pp. 323–344. [Google Scholar] [CrossRef]
- Javaid, M.; Haleem, A. Virtual reality applications toward medical field. Clin. Epidemiol. Glob. Health 2020, 8, 600–605. [Google Scholar] [CrossRef]
- Aziz, H.A. Virtual Reality Programs Applications in Healthcare. J. Health Med. Inform. 2018, 9, 305. [Google Scholar] [CrossRef]
- Lindner, P.; Dagöö, J.; Hamilton, W.; Miloff, A.; Andersson, G.; Schill, A.; Carlbring, P. Virtual Reality exposure therapy for public speaking anxiety in routine care: A single-subject effectiveness trial. Cogn. Behav. Ther. 2021, 50, 67–87. [Google Scholar] [CrossRef]
- Trappey, A.; Trappey, C.V.; Chang, C.-M.; Tsai, M.-C.; Kuo, R.R.T.; Lin, A.P.C. Virtual Reality Exposure Therapy for Driving Phobia Disorder (2): System Refinement and Verification. Appl. Sci. 2020, 11, 347. [Google Scholar] [CrossRef]
- Rodríguez-Hernández, M.; Polonio-López, B.; Corregidor-Sánchez, A.-I.; Martín-Conty, J.; Mohedano-Moriano, A.; Criado-Álvarez, J.-J. Effects of Specific Virtual Reality-Based Therapy for the Rehabilitation of the Upper Limb Motor Function Post-Ictus: Randomized Controlled Trial. Brain Sci. 2021, 11, 555. [Google Scholar] [CrossRef]
- Orakpo, N.; Vieux, U.; Castro-Nuñez, C. Case Report: Virtual Reality Neurofeedback Therapy as a Novel Modality for Sustained Analgesia in Centralized Pain Syndromes. Front. Psychiatry 2021, 12. [Google Scholar] [CrossRef] [PubMed]
- Rutkowski, S.; Szczegielniak, J.; Szczepańska-Gieracha, J. Evaluation of The Efficacy of Immersive Virtual Reality Therapy as a Method Supporting Pulmonary Rehabilitation: A Randomized Controlled Trial. J. Clin. Med. 2021, 10, 352. [Google Scholar] [CrossRef] [PubMed]
- Zeng, L.; Li, Z.; Zhao, Z.; Mao, M. Landscapes and Emerging Trends of Virtual Reality in Recent 30 Years: A Bibliometric Analysis. In Proceedings of the 2018 IEEE SmartWorld, Ubiquitous Intelligence & Computing, Advanced & Trusted Computing, Scalable Computing & Communications, Cloud & Big Data Computing, Internet of People and Smart City Innovation (SmartWorld/SCALCOM/UIC/ATC/CBDCom/IOP/SCI), Guangzhou, China, 8–12 October 2018; pp. 1852–1858. [Google Scholar] [CrossRef]
- Díaz, I.A.; Torres, J.M.T.; Rodríguez, J.M.R. Bibliometric study about virtual reality applied to neurorehabilitation and its presence in scientific literature. Rev. Cuba. Inf. Cienc. Salud 2018, 29, 1–10. [Google Scholar]
- Wiederhold, B.K.; Riva, G. Virtual Reality Therapy: Emerging Topics and Future Challenges. Cyberpsychol. Behav. Soc. Netw. 2019, 22, 3–6. [Google Scholar] [CrossRef]
- Dellazizzo, L.; Potvin, S.; Luigi, M.; Dumais, A. Evidence on Virtual Reality–Based Therapies for Psychiatric Disorders: Meta-Review of Meta-Analyses. J. Med. Internet Res. 2020, 22, e20889. [Google Scholar] [CrossRef]
- Hone-Blanchet, A.; Wensing, T.; Fecteau, S. The Use of Virtual Reality in Craving Assessment and Cue-Exposure Therapy in Substance Use Disorders. Front. Hum. Neurosci. 2014, 8, 844. [Google Scholar] [CrossRef]
- Yeung, A.W.K.; Tosevska, A.; Klager, E.; Eibensteiner, F.; Laxar, D.; Stoyanov, J.; Glisic, M.; Zeiner, S.; Kulnik, S.T.; Crutzen, R.; et al. Virtual and Augmented Reality Applications in Medicine: Analysis of the Scientific Literature. J. Med. Internet Res. 2021, 23, e25499. [Google Scholar] [CrossRef] [PubMed]
- Tonkavich, M.; Sheaffer, J.; Oliver, J.; Pabich, V.; Gomez, J. Immersive Virtual Reality in Healthcare: A Systematic Mapping Review. Available online: https://scholarworks.gvsu.edu/gradshowcase/2021/occupational_therapy/2 (accessed on 15 December 2021).
- Ellegaard, O.; Wallin, J.A. The bibliometric analysis of scholarly production: How great is the impact? Science 2015, 105, 1809–1831. [Google Scholar] [CrossRef]
- Zupic, I.; Čater, T. Bibliometric methods in management and organization. Organ. Res. Methods 2015, 18, 429–472. [Google Scholar] [CrossRef]
- Cobo, M.J.; López-Herrera, A.G.; Herrera-Viedma, E.; Herrera, F. An approach for detecting, quantifying, and visualizing the evolution of a research field: A practical application to the Fuzzy Sets Theory field. J. Inform. 2011, 5, 146–166. [Google Scholar] [CrossRef]
- Small, H. Visualizing science by citation mapping. J. Am. Soc. Inf. Sci. 1999, 50, 799–813. [Google Scholar] [CrossRef]
- van Eck, N.J.; Waltman, L. Software survey: VOSviewer, a computer program for bibliometric mapping. Scientometrics 2010, 84, 523–538. [Google Scholar] [CrossRef] [PubMed]
- Liu, W. The data source of this study is Web of Science Core Collection? Not Enough Sci. 2019, 121, 1815–1824. [Google Scholar] [CrossRef]
- Kessler, M.M. Bibliographic coupling between scientific papers. Am. Doc. 1963, 14, 10–25. [Google Scholar] [CrossRef]
- Boyack, K.W.; Klavans, R. Co-citation analysis, bibliographic coupling, and direct citation: Which citation approach represents the research front most accurately? J. Am. Soc. Inf. Sci. 2010, 61, 2389–2404. [Google Scholar] [CrossRef]
- Magnuson, L. Data Visualization: A Guide to Visual Storytelling for Libraries; Rowman and Littlefield Publishers: Lanham, MD, USA, 2016; p. 111. [Google Scholar]
- Goswami, A.; Agrawal, R.K. Building intellectual structure of knowledge sharing. VINE J. Inf. Knowl. Manag. Syst. 2019, 50, 136–162. [Google Scholar] [CrossRef]
- van Eck, N.J.; Waltman, L. VOSviewer Manual. Available online: https://www.vosviewer.com/documentation/Manual_VOSviewer_1.6.8.pdf (accessed on 15 December 2021).
- ICD-11-ICD-11 for Mortality and Morbidity Statistics n.d. Available online: https://icd.who.int/browse11/l-m/en (accessed on 5 September 2021).
- Hoffman, H.G.; Patterson, D.R.; Carrougher, G.J. Use of Virtual Reality for Adjunctive Treatment of Adult Burn Pain During Physical Therapy: A Controlled Study. Clin. J. Pain 2000, 16, 244–250. [Google Scholar] [CrossRef] [PubMed]
- Rothbaum, B.O.; Hodges, L.F.; Ready, D.; Graap, K.; Alarcon, R.D. Virtual Reality Exposure Therapy for Vietnam Veterans With Posttraumatic Stress Disorder. J. Clin. Psychiatry 2001, 62, 617–622. [Google Scholar] [CrossRef]
- Myers, R.L.; Bierig, T.A. Virtual Reality and Left Hemineglect: A Technology for Assessment and Therapy. Cyberpsychol. Behav. 2000, 3, 465–468. [Google Scholar] [CrossRef]
- Bryant, R.A. Post-traumatic stress disorder: A state-of-the-art review of evidence and challenges. World Psychiatry 2019, 18, 259–269. [Google Scholar] [CrossRef]
- Kirkpatrick, H.A.; Heller, G.M. Post-Traumatic Stress Disorder: Theory and Treatment Update. Int. J. Psychiatry Med. 2014, 47, 337–346. [Google Scholar] [CrossRef] [PubMed]
- Gerardi, M.; Cukor, J.; Difede, J.; Rizzo, A.; Rothbaum, B.O. Virtual Reality Exposure Therapy for Post-Traumatic Stress Disorder and Other Anxiety Disorders. Curr. Psychiatry Rep. 2010, 12, 298–305. [Google Scholar] [CrossRef] [PubMed]
- Rothbaum, B.O.; Rizzo, A.S.; Difede, J. Virtual reality exposure therapy for combat-related posttraumatic stress disorder. In Psychiatric and Neurologic Aspects of War; Barchas, J.D., Difede, J., Eds.; Wiley Online Library: Hoboken, NJ, USA, 2010; Volume 1208, p. 126. [Google Scholar] [CrossRef]
- McLay, R.N.; McBrien, C.; Wiederhold, M.D.; Wiederhold, B.K. Exposure Therapy with and without Virtual Reality to Treat PTSD while in the Combat Theater: A Parallel Case Series. Cyberpsychol. Behav. Soc. Netw. 2010, 13, 37–42. [Google Scholar] [CrossRef] [PubMed]
- Wood, D.P.; Webb-Murphy, J.; Center, K.; McLay, R.; Koffman, R.; Johnston, S.; Spira, J.; Pyne, J.M.; Wiederhold, B.K. Combat-Related Post-Traumatic Stress Disorder: A Case Report Using Virtual Reality Graded Exposure Therapy with Physiological Monitoring with a Female Seabee. Mil. Med. 2009, 174, 1215–1222. [Google Scholar] [CrossRef]
- Gerardi, M.; Rothbaum, B.O.; Ressler, K.; Heekin, M.; Rizzo, A. Virtual reality exposure therapy using a virtual Iraq: Case report. J. Trauma. Stress 2008, 21, 209–213. [Google Scholar] [CrossRef]
- Reger, G.M.; Gahm, G.A. Virtual reality exposure therapy for active duty soldiers. J. Clin. Psychol. 2008, 64, 940–946. [Google Scholar] [CrossRef]
- Difede, J.; Cukor, J.; Jayasinghe, N.; Patt, I.; Jedel, S.; Spielman, L.; Giosan, C.; Hoffman, H.G. Virtual Reality Exposure Therapy for the Treatment of Posttraumatic Stress Disorder Following 11 September 2001. J. Clin. Psychiatry 2007, 68, 1682–1689. [Google Scholar] [CrossRef]
- Beck, J.G.; Palyo, S.A.; Winer, E.H.; Schwagler, B.E.; Ang, E.J. Virtual Reality Exposure Therapy for PTSD Symptoms After a Road Accident: An Uncontrolled Case Series. Behav. Ther. 2007, 38, 39–48. [Google Scholar] [CrossRef]
- Wood, D.P.; Murphy, J.; Center, K.; McLay, R.; Reeves, D.; Pyne, J.; Shilling, R.; Wiederhold, B.K. Combat-Related Post-Traumatic Stress Disorder: A Case Report Using Virtual Reality Exposure Therapy with Physiological Monitoring. Cyberpsychol. Behav. 2007, 10, 309–315. [Google Scholar] [CrossRef]
- Ready, D.J.; Gerardi, R.J.; Backscheider, A.G.; Mascaro, N.; Rothbaum, B.O. Comparing Virtual Reality Exposure Therapy to Present-Centered Therapy with 11 U.S. Vietnam Veterans with PTSD. Cyberpsychol. Behav. Soc. Netw. 2010, 13, 49–54. [Google Scholar] [CrossRef]
- Beidel, D.C.; Frueh, B.C.; Neer, S.M.; Bowers, C.A.; Trachik, B.; Uhde, T.W.; Grubaugh, A. Trauma management therapy with virtual-reality augmented exposure therapy for combat-related PTSD: A randomized controlled trial. J. Anxiety Disord. 2019, 61, 64–74. [Google Scholar] [CrossRef] [PubMed]
- Reger, G.M.; Smolenski, D.; Norr, A.; Katz, A.; Buck, B.; Rothbaum, B.O. Does virtual reality increase emotional engagement during exposure for PTSD? Subjective distress during prolonged and virtual reality exposure therapy. J. Anxiety Disord. 2019, 61, 75–81. [Google Scholar] [CrossRef] [PubMed]
- McLay, R.N.; Baird, A.; Webb-Murphy, J.; Deal, W.; Tran, L.; Anson, H.; Klam, W.; Johnston, S. A Randomized, Head-to-Head Study of Virtual Reality Exposure Therapy for Posttraumatic Stress Disorder. Cyberpsychol. Behav. Soc. Netw. 2017, 20, 218–224. [Google Scholar] [CrossRef] [PubMed]
- McLay, R.N.; Wood, D.P.; Webb-Murphy, J.A.; Spira, J.L.; Wiederhold, M.D.; Pyne, J.M.; Wiederhold, B.K. A Randomized, Controlled Trial of Virtual Reality-Graded Exposure Therapy for Post-Traumatic Stress Disorder in Active Duty Service Members with Combat-Related Post-Traumatic Stress Disorder. Cyberpsychol. Behav. Soc. Netw. 2011, 14, 223–229. [Google Scholar] [CrossRef] [PubMed]
- Sherrill, A.M.; Rothbaum, A.O.; McSweeney, L.B.; Rothbaum, B.O. Virtual Reality Exposure Therapy for Posttraumatic Stress Disorder. Psychiatr. Ann. 2019, 49, 343–347. [Google Scholar] [CrossRef]
- Crawford-Holland, S. Virtual Healing: Militarizing the Psyche in Virtual Reality Exposure Therapy. Telev. New Media 2017, 20, 56–71. [Google Scholar] [CrossRef]
- Botella, C.; Serrano, B.; Baños, R.M.; García-Palacios, A. Virtual reality exposure-based therapy for the treatment of post-traumatic stress disorder: A review of its efficacy, the adequacy of the treatment protocol, and its acceptability. Neuropsychiatr. Dis. Treat. 2015, 11, 2533–2545. [Google Scholar] [CrossRef] [PubMed]
- Aiken, M.P.; Berry, M.J. Posttraumatic stress disorder: Possibilities for olfaction and virtual reality exposure therapy. Virtual Real. 2015, 19, 95–109. [Google Scholar] [CrossRef]
- Motraghi, T.E.; Seim, R.W.; Meyer, E.C.; Morissette, S.B. Virtual Reality Exposure Therapy for the Treatment of Posttraumatic Stress Disorder: A Methodological Review Using CONSORT Guidelines. J. Clin. Psychol. 2014, 70, 197–208. [Google Scholar] [CrossRef]
- Bloch, F.; Rigaud, A.-S.; Kemoun, G. Virtual Reality Exposure Therapy in posttraumatic stress disorder: A brief review to open new opportunities for post-fall syndrome in elderly subjects. Eur. Geriatr. Med. 2013, 4, 427–430. [Google Scholar] [CrossRef]
- Gonçalves, R.; Pedrozo, A.L.; Coutinho, E.S.F.; Figueira, I.; Ventura, P. Efficacy of Virtual Reality Exposure Therapy in the Treatment of PTSD: A Systematic Review. PLoS ONE 2012, 7, e48469. [Google Scholar] [CrossRef] [PubMed]
- Kothgassner, O.D.; Goreis, A.; Kafka, J.X.; Van Eickels, R.L.; Plener, P.L.; Felnhofer, A. Virtual reality exposure therapy for posttraumatic stress disorder (PTSD): A meta-analysis. Eur. J. Psychotraumatol. 2019, 10, 1654782. [Google Scholar] [CrossRef] [PubMed]
- Deng, W.; Hu, D.; Xu, S.; Liu, X.; Zhao, J.; Chen, Q.; Liu, J.; Zhang, Z.; Jiang, W.; Ma, L.; et al. The efficacy of virtual reality exposure therapy for PTSD symptoms: A systematic review and meta-analysis. J. Affect. Disord. 2019, 257, 698–709. [Google Scholar] [CrossRef] [PubMed]
- Reger, G.M.; Holloway, K.M.; Candy, C.; Rothbaum, B.O.; Difede, J.; Rizzo, A.A.; Gahm, G.A. Effectiveness of virtual reality exposure therapy for active duty soldiers in a military mental health clinic. J. Trauma Stress 2011, 24, 93–96. [Google Scholar] [CrossRef]
- Walshe, D.G.; Lewis, E.J.; Kim, S.I.; O’Sullivan, K.; Wiederhold, B.K. Exploring the Use of Computer Games and Virtual Reality in Exposure Therapy for Fear of Driving Following a Motor Vehicle Accident. Cyberpsychol. Behav. 2003, 6, 329–334. [Google Scholar] [CrossRef] [PubMed]
- Loucks, L.; Yasinski, C.; Norrholm, S.D.; Maples-Keller, J.; Post, L.; Zwiebach, L.; Fiorillo, D.; Goodlin, M.; Jovanovic, T.; Rizzo, A.A.; et al. You can do that?!: Feasibility of virtual reality exposure therapy in the treatment of PTSD due to military sexual trauma. J. Anxiety Disord. 2019, 61, 55–63. [Google Scholar] [CrossRef] [PubMed]
- Dias, B.G.; Banerjee, S.B.; Goodman, J.; Ressler, K.J. Towards new approaches to disorders of fear and anxiety. Curr. Opin. Neurobiol. 2013, 23, 346–352. [Google Scholar] [CrossRef]
- De Carvalho, M.R.; Freire, R.C.; Nardi, A.E. Virtual reality as a mechanism for exposure therapy. World J. Biol. Psychiatry 2010, 11, 220–230. [Google Scholar] [CrossRef]
- Faraci, P.; Triscari, M.T.; Catalisano, D.; D’Angelo, V.; Urso, V. Effectiveness of cognitive behavioral therapy integrated with systematic desensitization, cognitive behavioral therapy combined with eye movement desensitization and reprocessing therapy, and cognitive behavioral therapy combined with virtual reality exposure therapy methods in the treatment of flight anxiety: A randomized trial. Neuropsychiatr. Dis. Treat. 2015, 11, 2591–2598. [Google Scholar] [CrossRef]
- Wallach, H.S.; Safir, M.P.; Bar-Zvi, M. Virtual Reality Cognitive Behavior Therapy for Public Speaking Anxiety. Behav. Modif. 2009, 33, 314–338. [Google Scholar] [CrossRef]
- Safir, M.P.; Wallach, H.S.; Bar-Zvi, M. Virtual Reality Cognitive-Behavior Therapy for Public Speaking Anxiety. Behav. Modif. 2012, 36, 235–246. [Google Scholar] [CrossRef] [PubMed]
- Penate, W.; Pitti, C.T.; Bethencourt, J.M.; de la Fuente, J.; Gracia, R. The effects of a treatment based on the use of virtual reality exposure and cognitive-behavioral therapy applied to patients with agoraphobia. Int. J. Clin. Health Psychol. 2008, 8, 5–22. [Google Scholar]
- Anderson, P.L.; Zimand, E.; Hodges, L.F.; Rothbaum, B.O. Cognitive behavioral therapy for public-speaking anxiety using virtual reality for exposure. Depress. Anxiety 2005, 22, 156–158. [Google Scholar] [CrossRef] [PubMed]
- David, D.; Matu, S.-A.; David, O. New Directions in Virtual Reality-Based Therapy for Anxiety Disorders. Int. J. Cogn. Ther. 2013, 6, 114–137. [Google Scholar] [CrossRef]
- Navarro-Haro, M.V.; Modrego-Alarcón, M.; Hoffman, H.G.; López-Montoyo, A.; Navarro-Gil, M.; Montero-Marin, J.; García-Palacios, A.; Borao, L.; García-Campayo, J. Evaluation of a Mindfulness-Based Intervention with and without Virtual Reality Dialectical Behavior Therapy® Mindfulness Skills Training for the Treatment of Generalized Anxiety Disorder in Primary Care: A Pilot Study. Front. Psychol. 2019, 10, 55. [Google Scholar] [CrossRef]
- Falconer, C.J.; Davies, E.B.; Grist, R.; Stallard, P. Innovations in Practice: Avatar-based virtual reality in CAMHS talking therapy: Two exploratory case studies. Child Adolesc. Ment. Health 2019, 24, 283–287. [Google Scholar] [CrossRef]
- Lindner, P.; Miloff, A.; Bergman, C.; Andersson, G.; Hamilton, W.; Carlbring, P. Gamified, Automated Virtual Reality Exposure Therapy for Fear of Spiders: A Single-Subject Trial Under Simulated Real-World Conditions. Front. Psychiatry 2020, 11, 116. [Google Scholar] [CrossRef]
- Lindner, P.; Rozental, A.; Jurell, A.; Reuterskiöld, L.; Andersson, G.; Hamilton, W.; Miloff, A.; Carlbring, P. Experiences of Gamified and Automated Virtual Reality Exposure Therapy for Spider Phobia: Qualitative Study. JMIR Serious Games 2020, 8, e17807. [Google Scholar] [CrossRef]
- Malbos, E.; Mestre, D.; Note, I.; Gellato, C. Virtual Reality and Claustrophobia: Multiple Components Therapy Involving Game Editor Virtual Environments Exposure. Cyberpsychol. Behav. 2008, 11, 695–697. [Google Scholar] [CrossRef]
- Kahlon, S.; Lindner, P.; Nordgreen, T. Virtual reality exposure therapy for adolescents with fear of public speaking: A non-randomized feasibility and pilot study. Child Adolesc. Psychiatry Ment. Health 2019, 13, 47. [Google Scholar] [CrossRef]
- Anderson, P.L.; Edwards, S.M.; Goodnight, J.R. Virtual Reality and Exposure Group Therapy for Social Anxiety Disorder: Results from a 4–6 Year Follow-Up. Cogn. Ther. Res. 2016, 41, 230–236. [Google Scholar] [CrossRef]
- Hirsch, J.A. Virtual Reality Exposure Therapy and Hypnosis for Flying Phobia in a Treatment-Resistant Patient: A Case Report. Am. J. Clin. Hypn. 2012, 55, 168–173. [Google Scholar] [CrossRef] [PubMed]
- Donker, T.; Van Klaveren, C.; Cornelisz, I.; Kok, R.N.; Van Gelder, J.-L. Analysis of Usage Data from a Self-Guided App-Based Virtual Reality Cognitive Behavior Therapy for Acrophobia: A Randomized Controlled Trial. J. Clin. Med. 2020, 9, 1614. [Google Scholar] [CrossRef] [PubMed]
- Lindner, P.; Miloff, A.; Fagernäs, S.; Andersen, J.; Sigeman, M.; Andersson, G.; Furmark, T.; Carlbring, P. Therapist-led and self-led one-session virtual reality exposure therapy for public speaking anxiety with consumer hardware and software: A randomized controlled trial. J. Anxiety Disord. 2019, 61, 45–54. [Google Scholar] [CrossRef]
- Gujjar, K.R.; van Wijk, A.; Kumar, R.; de Jongh, A. Efficacy of virtual reality exposure therapy for the treatment of dental phobia in adults: A randomized controlled trial. J. Anxiety Disord. 2019, 62, 100–108. [Google Scholar] [CrossRef]
- Donker, T.; Cornelisz, I.; Van Klaveren, C.; van Straten, A.; Carlbring, P.; Cuijpers, P.; Van Gelder, J.-L. Effectiveness of Self-guided App-Based Virtual Reality Cognitive Behavior Therapy for Acrophobia: A Randomized Clinical Trial. JAMA Psychiatry 2019, 76, 682–690. [Google Scholar] [CrossRef]
- Freeman, D.; Haselton, P.; Freeman, J.; Spanlang, B.; Kishore, S.; Albery, E.; Denne, M.; Brown, P.; Slater, M.; Nickless, A. Automated psychological therapy using immersive virtual reality for treatment of fear of heights: A single-blind, parallel-group, randomised controlled trial. Lancet Psychiatry 2018, 5, 625–632. [Google Scholar] [CrossRef]
- Moldovan, R.; David, D. One session treatment of cognitive and behavioral therapy and virtual reality for social and specific phobias. preliminary results from a randomized clinical trial. J. Evid. Based Psychother. 2014, 14, 67–83. [Google Scholar]
- Anderson, P.L.; Price, M.; Edwards, S.M.; Obasaju, M.A.; Schmertz, S.K.; Zimand, E.; Calamaras, M.R. Virtual reality exposure therapy for social anxiety disorder: A randomized controlled trial. J. Consult. Clin. Psychol. 2013, 81, 751–760. [Google Scholar] [CrossRef]
- Meyerbroeker, K.; Morina, N.; Kerkhof, G.; Emmelkamp, P. Virtual Reality Exposure Therapy Does Not Provide Any Additional Value in Agoraphobic Patients: A Randomized Controlled Trial. Psychother. Psychosom. 2013, 82, 170–176. [Google Scholar] [CrossRef]
- Malbos, E.; Rapee, R.; Kavakli, M. A controlled study of agoraphobia and the independent effect of virtual reality exposure therapy. Aust. N. Z. J. Psychiatry 2012, 47, 160–168. [Google Scholar] [CrossRef] [PubMed]
- Anderson, P.L.; Molloy, A. Maximizing the impact of virtual reality exposure therapy for anxiety disorders. Curr. Opin. Psychol. 2020, 36, 153–157. [Google Scholar] [CrossRef]
- Emmelkamp, P.M.G.; Meyerbröker, K.; Morina, N. Virtual Reality Therapy in Social Anxiety Disorder. Curr. Psychiatry Rep. 2020, 22, 32. [Google Scholar] [CrossRef] [PubMed]
- Kritikos, J.; Zoitaki, C.; Tzannetos, G.; Mehmeti, A.; Douloudi, M.; Nikolaou, G.; Alevizopoulos, G.; Koutsouris, D. Comparison between Full Body Motion Recognition Camera Interaction and Hand Controllers Interaction used in Virtual Reality Exposure Therapy for Acrophobia. Sensors 2020, 20, 1244. [Google Scholar] [CrossRef] [PubMed]
- Boeldt, D.; McMahon, E.; Mcfaul, M.; Greenleaf, W. Using Virtual Reality Exposure Therapy to Enhance Treatment of Anxiety Disorders: Identifying Areas of Clinical Adoption and Potential Obstacles. Front. Psychiatry 2019, 10, 773. [Google Scholar] [CrossRef]
- Ben-Moussa, M.; Rubo, M.; Debracque, C.; Lange, W.-G. DJINNI: A Novel Technology Supported Exposure Therapy Paradigm for SAD Combining Virtual Reality and Augmented Reality. Front. Psychiatry 2017, 8, 26. [Google Scholar] [CrossRef]
- McCann, R.A.; Armstrong, C.M.; Skopp, N.A.; Edwards-Stewart, A.; Smolenski, D.J.; June, J.D.; Metzger-Abamukong, M.; Reger, G.M. Virtual reality exposure therapy for the treatment of anxiety disorders: An evaluation of research quality. J. Anxiety Disord. 2014, 28, 625–631. [Google Scholar] [CrossRef] [PubMed]
- Ebaus, O.; Bouchard, S. Moving from Virtual Reality Exposure-Based Therapy to Augmented Reality Exposure-Based Therapy: A Review. Front. Hum. Neurosci. 2014, 8, 112. [Google Scholar] [CrossRef]
- García-García, E.S.; I Rosa-Alcázar, A.; Olivares-Olivares, P.J. Terapia de Exposición Mediante Realidad Virtual e Internet en el Trastorno de Ansiedad/Fobia Social: Una Revisión Cualitativa. Terapia Psicol. 2011, 29, 233–243. [Google Scholar] [CrossRef][Green Version]
- Bush, J. Viability of virtual reality exposure therapy as a treatment alternative. Comput. Hum. Behav. 2008, 24, 1032–1040. [Google Scholar] [CrossRef]
- Botella, C.; Fernández-Álvarez, J.; Guillén, V.; García-Palacios, A.; Baños, R. Recent Progress in Virtual Reality Exposure Therapy for Phobias: A Systematic Review. Curr. Psychiatry Rep. 2017, 19, 42. [Google Scholar] [CrossRef] [PubMed]
- Meyerbröker, K.; Emmelkamp, P. Virtual reality exposure therapy in anxiety disorders: A systematic review of process-and-outcome studies. Depress. Anxiety 2010, 27, 933–944. [Google Scholar] [CrossRef]
- Horigome, T.; Kurokawa, S.; Sawada, K.; Kudo, S.; Shiga, K.; Mimura, M.; Kishimoto, T. Virtual reality exposure therapy for social anxiety disorder: A systematic review and meta-analysis. Psychol. Med. 2020, 50, 2487–2497. [Google Scholar] [CrossRef] [PubMed]
- Carl, E.; Stein, A.T.; Levihn-Coon, A.; Pogue, J.R.; Rothbaum, B.; Emmelkamp, P.; Asmundson, G.J.; Carlbring, P.; Powers, M.B. Virtual reality exposure therapy for anxiety and related disorders: A meta-analysis of randomized controlled trials. J. Anxiety Disord. 2019, 61, 27–36. [Google Scholar] [CrossRef] [PubMed]
- Wechsler, T.F.; Kümpers, F.; Mühlberger, A. Inferiority or Even Superiority of Virtual Reality Exposure Therapy in Phobias?—A Systematic Review and Quantitative Meta-Analysis on Randomized Controlled Trials Specifically Comparing the Efficacy of Virtual Reality Exposure to Gold Standard in vivo Exposure in Agoraphobia, Specific Phobia, and Social Phobia. Front. Psychol. 2019, 10, 1758. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Álvarez, J.; Rozental, A.; Carlbring, P.; Colombo, D.; Riva, G.; Anderson, P.L.; Baños, R.M.; Benbow, A.A.; Bouchard, S.; Bretón-López, J.M.; et al. Deterioration rates in Virtual Reality Therapy: An individual patient data level meta-analysis. J. Anxiety Disord. 2019, 61, 3–17. [Google Scholar] [CrossRef] [PubMed]
- Benbow, A.A.; Anderson, P.L. A meta-analytic examination of attrition in virtual reality exposure therapy for anxiety disorders. J. Anxiety Disord. 2019, 61, 18–26. [Google Scholar] [CrossRef] [PubMed]
- Chesham, R.K.; Malouff, J.M.; Schutte, N.S. Meta-Analysis of the Efficacy of Virtual Reality Exposure Therapy for Social Anxiety. Behav. Chang. 2018, 35, 152–166. [Google Scholar] [CrossRef]
- Cardoş, R.A.; David, O.; David, D.O. Virtual reality exposure therapy in flight anxiety: A quantitative meta-analysis. Comput. Hum. Behav. 2017, 72, 371–380. [Google Scholar] [CrossRef]
- Morina, N.; Ijntema, H.; Meyerbröker, K.; Emmelkamp, P.M. Can virtual reality exposure therapy gains be generalized to real-life? A meta-analysis of studies applying behavioral assessments. Behav. Res. Ther. 2015, 74, 18–24. [Google Scholar] [CrossRef]
- Ling, Y.; Nefs, H.T.; Morina, N.; Heynderickx, I.; Brinkman, W.-P. A Meta-Analysis on the Relationship between Self-Reported Presence and Anxiety in Virtual Reality Exposure Therapy for Anxiety Disorders. PLoS ONE 2014, 9, e96144. [Google Scholar] [CrossRef] [PubMed]
- Opriş, D.; Pintea, S.; García-Palacios, A.; Botella, C.; Ştefan, S.; David, D. Virtual reality exposure therapy in anxiety disorders: A quantitative meta-analysis. Depress. Anxiety 2012, 29, 85–93. [Google Scholar] [CrossRef] [PubMed]
- Powers, M.B.; Emmelkamp, P. Virtual reality exposure therapy for anxiety disorders: A meta-analysis. J. Anxiety Disord. 2008, 22, 561–569. [Google Scholar] [CrossRef] [PubMed]
- Parsons, T.D.; Rizzo, A.A. Affective outcomes of virtual reality exposure therapy for anxiety and specific phobias: A meta-analysis. J. Behav. Ther. Exp. Psychiatry 2008, 39, 250–261. [Google Scholar] [CrossRef]
- Landowska, A.; Roberts, D.; Eachus, P.; Barrett, A. Within- and Between-Session Prefrontal Cortex Response to Virtual Reality Exposure Therapy for Acrophobia. Front. Hum. Neurosci. 2018, 12, 362. [Google Scholar] [CrossRef]
- Gujjar, K.R.; Van Wijk, A.; Sharma, R.; De Jongh, A. Virtual Reality Exposure Therapy for the Treatment of Dental Phobia: A Controlled Feasibility Study. Behav. Cogn. Psychother. 2017, 46, 367–373. [Google Scholar] [CrossRef]
- Tsai, C.-F.; Yeh, S.-C.; Huang, Y.; Wu, Z.; Cui, J.; Zheng, L. The Effect of Augmented Reality and Virtual Reality on Inducing Anxiety for Exposure Therapy: A Comparison Using Heart Rate Variability. J. Health Eng. 2018, 2018, 1–8. [Google Scholar] [CrossRef]
- Verger, A.; Malbos, E.; Reynaud, E.; Mallet, P.; Mestre, D.; Pergandi, J.-M.; Khalfa, S.; Guedj, E. Brain metabolism and related connectivity in patients with acrophobia treated by virtual reality therapy: An 18F-FDG PET pilot study sensitized by virtual exposure. EJNMMI Res. 2018, 8, 93. [Google Scholar] [CrossRef]
- Jang, D.; Ku, J.; Choi, Y.; Wiederhold, B.; Nam, S.; Kim, I.; Kim, S. The development of virtual reality therapy (VRT) system for the treatment of acrophobia and therapeutic case. IEEE Trans. Inf. Technol. Biomed. 2002, 6, 213–217. [Google Scholar] [CrossRef]
- Jiang, M.Y.; Upton, E.; Newby, J.M. A randomised wait-list controlled pilot trial of one-session virtual reality exposure therapy for blood-injection-injury phobias. J. Affect. Disord. 2020, 276, 636–645. [Google Scholar] [CrossRef]
- North, M.M.; North, S.M. The Sense of Presence Exploration in Virtual Reality Therapy. J. Univers. Comput. Sci. 2018, 24, 72–84. [Google Scholar]
- Price, M.; Anderson, P. The role of presence in virtual reality exposure therapy. J. Anxiety Disord. 2007, 21, 742–751. [Google Scholar] [CrossRef] [PubMed]
- Price, M.; Mehta, N.; Tone, E.B.; Anderson, P.L. Does engagement with exposure yield better outcomes? Components of presence as a predictor of treatment response for virtual reality exposure therapy for social phobia. J. Anxiety Disord. 2011, 25, 763–770. [Google Scholar] [CrossRef]
- Lindner, P.; Miloff, A.; Zetterlund, E.; Reuterskiöld, L.; Andersson, G.; Carlbring, P. Attitudes Toward and Familiarity with Virtual Reality Therapy Among Practicing Cognitive Behavior Therapists: A Cross-Sectional Survey Study in the Era of Consumer VR Platforms. Front. Psychol. 2019, 10, 176. [Google Scholar] [CrossRef] [PubMed]
- Schuster-Amft, C.; Eng, K.; Suica, Z.; Thaler, I.; Signer, S.; Lehmann, I.; Schmid, L.; McCaskey, M.A.; Hawkins, M.; Verra, M.; et al. Effect of a four-week virtual reality-based training versus conventional therapy on upper limb motor function after stroke: A multicenter parallel group randomized trial. PLoS ONE 2018, 13, e0204455. [Google Scholar] [CrossRef] [PubMed]
- Chauhan, A.; Kumar, N.; Saxena, S. Virtual Reality based Therapy Modules for Rehabilitation of Upper-limb Movements of Stroke Patients: A Trial Study. JSIR 2020, 79, 794–797. [Google Scholar]
- Roberts, H.; Shierk, A.; Clegg, N.J.; Baldwin, D.; Smith, L.; Yeatts, P.; Delgado, M.R. Constraint Induced Movement Therapy Camp for Children with Hemiplegic Cerebral Palsy Augmented by Use of an Exoskeleton to Play Games in Virtual Reality. Phys. Occup. Ther. Pediatr. 2021, 41, 150–165. [Google Scholar] [CrossRef]
- Jin, R.; Pilozzi, A.; Huang, X. Current Cognition Tests, Potential Virtual Reality Applications, and Serious Games in Cognitive Assessment and Non-Pharmacological Therapy for Neurocognitive Disorders. J. Clin. Med. 2020, 9, 3287. [Google Scholar] [CrossRef] [PubMed]
- Felipe, F.A.; de Carvalho, F.O.; Silva, É.R.; Santos, N.G.L.; Fontes, P.A.; de Almeida, A.S.; Garção, D.C.; Nunes, P.S.; Araújo, A.A.D.S. Evaluation instruments for physical therapy using virtual reality in stroke patients: A systematic review. Physiotherapy 2019, 106, 194–210. [Google Scholar] [CrossRef]
- Wille, D.; Eng, K.; Holper, L.; Chevrier, E.; Hauser, Y.; Kiper, D.; Pyk, P.; Schlegel, S.; Meyer-Heim, A. Virtual reality-based paediatric interactive therapy system (PITS) for improvement of arm and hand function in children with motor impairment-a pilot study. Dev. Neurorehabil. 2009, 12, 44–52. [Google Scholar] [CrossRef]
- Lohse, K.R.; Hilderman, C.G.; Cheung, K.L.; Tatla, S.; Van der Loos, H.M. Virtual Reality Therapy for Adults Post-Stroke: A Systematic Review and Meta-Analysis Exploring Virtual Environments and Commercial Games in Therapy. PLoS ONE 2014, 9, e93318. [Google Scholar] [CrossRef] [PubMed]
- Ustinova, K.I.; Perkins, J.; Leonard, W.A.; Hausbeck, C.J. Virtual reality game-based therapy for treatment of postural and co-ordination abnormalities secondary to TBI: A pilot study. Brain Inj. 2014, 28, 486–495. [Google Scholar] [CrossRef] [PubMed]
- Ni, L.T.; Fehlings, D.; Biddiss, E. Design and Evaluation of Virtual Reality–Based Therapy Games with Dual Focus on Therapeutic Relevance and User Experience for Children with Cerebral Palsy. Games Health J. 2014, 3, 162–171. [Google Scholar] [CrossRef] [PubMed]
- Bullock, K.; Won, A.S.; Bailenson, J.; Friedman, R. Virtual Reality-Delivered Mirror Visual Feedback and Exposure Therapy for FND: A Midpoint Report of a Randomized Controlled Feasibility Study. J. Neuropsychiatry Clin. Neurosci. 2020, 32, 90–94. [Google Scholar] [CrossRef]
- Yeves-Lite, A.; Zuil-Escobar, J.C.; Martínez-Cepa, C.; Romay-Barrero, H.; Ferri-Morales, A.; Palomo-Carrión, R. Conventional and Virtual Reality Mirror Therapies in Upper Obstetric Brachial Palsy: A Randomized Pilot Study. J. Clin. Med. 2020, 9, 3021. [Google Scholar] [CrossRef]
- Mekbib, D.B.; Zhao, Z.; Wang, J.; Xu, B.; Zhang, L.; Cheng, R.; Fang, S.; Shao, Y.; Yang, W.; Han, J.; et al. Proactive Motor Functional Recovery Following Immersive Virtual Reality–Based Limb Mirroring Therapy in Patients with Subacute Stroke. Neurotherapeutics 2020, 17, 1919–1930. [Google Scholar] [CrossRef]
- Sucar, L.E.; Orihuela-Espina, F.; Velazquez, R.L.; Reinkensmeyer, D.J.; Leder, R.; Hernandez-Franco, J. Gesture Therapy: An Upper Limb Virtual Reality-Based Motor Rehabilitation Platform. IEEE Trans. Neural Syst. Rehabil. Eng. 2014, 22, 634–643. [Google Scholar] [CrossRef]
- Orihuela-Espina, F.; Del Castillo, I.F.; Palafox, L.; Pasaye, E.; Sánchez-Villavicencio, I.; Leder, R.; Franco, J.H.; Sucar, L.E. Neural Reorganization Accompanying Upper Limb Motor Rehabilitation from Stroke with Virtual Reality-Based Gesture Therapy. Top. Stroke Rehabil. 2013, 20, 197–209. [Google Scholar] [CrossRef]
- Feng, H.; Li, C.; Liu, J.; Wang, L.; Ma, J.; Li, G.; Gan, L.; Shang, X.; Wu, Z. Virtual Reality Rehabilitation Versus Conventional Physical Therapy for Improving Balance and Gait in Parkinson’s Disease Patients: A Randomized Controlled Trial. Med. Sci. Monit. 2019, 25, 4186–4192. [Google Scholar] [CrossRef]
- Farr, W.J.; Green, D.; Bremner, S.; Male, I.; Gage, H.; Bailey, S.; Speller, S.; Colville, V.; Jackson, M.; Memon, A.; et al. Feasibility of a randomised controlled trial to evaluate home-based virtual reality therapy in children with cerebral palsy. Disabil. Rehabil. 2021, 43, 85–97. [Google Scholar] [CrossRef]
- Ökmen, B.M.; Aslan, M.D.; Yüzer, G.F.N.; Özgirgin, N. Effect of virtual reality therapy on functional development in children with cerebral palsy: A single-blind, prospective, randomized-controlled study. Turk. J. Phys. Med. Rehabil. 2019, 65, 371–378. [Google Scholar] [CrossRef] [PubMed]
- In, T.; Lee, K.; Song, C. Virtual Reality Reflection Therapy Improves Balance and Gait in Patients with Chronic Stroke: Randomized Controlled Trials. Med. Sci. Monit. 2016, 22, 4046–4053. [Google Scholar] [CrossRef] [PubMed]
- Park, J.-H.; Park, J.-H. The effects of game-based virtual reality movement therapy plus mental practice on upper extremity function in chronic stroke patients with hemiparesis: A randomized controlled trial. J. Phys. Ther. Sci. 2016, 28, 811–815. [Google Scholar] [CrossRef] [PubMed]
- Warnier, N.; Lambregts, S.; Van De Port, I. Effect of Virtual Reality Therapy on Balance and Walking in Children with Cerebral Palsy: A Systematic Review. Dev. Neurorehabilit. 2020, 23, 502–518. [Google Scholar] [CrossRef] [PubMed]
- Baur, K.; Schättin, A.; De Bruin, E.D.; Riener, R.; Duarte, J.E.; Wolf, P. Trends in robot-assisted and virtual reality-assisted neuromuscular therapy: A systematic review of health-related multiplayer games. J. Neuroeng. Rehabil. 2018, 15, 107. [Google Scholar] [CrossRef]
- Mekbib, D.B.; Han, J.; Zhang, L.; Fang, S.; Jiang, H.; Zhu, J.; Roe, A.W.; Xu, D. Virtual reality therapy for upper limb rehabilitation in patients with stroke: A meta-analysis of randomized clinical trials. Brain Inj. 2020, 34, 456–465. [Google Scholar] [CrossRef]
- Mohammadi, R.; Semnani, A.V.; Mirmohammadkhani, M.; Grampurohit, N. Effects of Virtual Reality Compared to Conventional Therapy on Balance Poststroke: A Systematic Review and Meta-Analysis. J. Stroke Cerebrovasc. Dis. 2019, 28, 1787–1798. [Google Scholar] [CrossRef]
- Abou, L.; Malala, V.D.; Yarnot, R.; Alluri, A.; Rice, L.A. Effects of Virtual Reality Therapy on Gait and Balance among Individuals with Spinal Cord Injury: A Systematic Review and Meta-analysis. Neurorehabilit. Neural Repair 2020, 34, 375–388. [Google Scholar] [CrossRef]
- Słyk, S.; Zarzycki, M.Z.; Kocwa-Karnaś, A.; Domitrz, I. Virtual reality in the diagnostics and therapy of neurological diseases. Expert Rev. Med. Devices 2019, 16, 1035–1040. [Google Scholar] [CrossRef]
- Bohil, C.; Alicea, B.; Biocca, F.A. Virtual reality in neuroscience research and therapy. Nat. Rev. Neurosci. 2011, 12, 752–762. [Google Scholar] [CrossRef]
- You, S.H.; Jang, S.H.; Kim, Y.-H.; Kwon, Y.-H.; Barrow, I.; Hallett, M. Cortical reorganization induced by virtual reality therapy in a child with hemiparetic cerebral palsy. Dev. Med. Child Neurol. 2005, 47, 628. [Google Scholar] [CrossRef] [PubMed]
- Saleh, S.; Fluet, G.; Qiu, Q.; Merians, A.; Adamovich, S.V.; Tunik, E. Neural Patterns of Reorganization after Intensive Robot-Assisted Virtual Reality Therapy and Repetitive Task Practice in Patients with Chronic Stroke. Front. Neurol. 2017, 8, 452. [Google Scholar] [CrossRef] [PubMed]
- Levac, D.; Missiuna, C.; Wishart, L.; DeMatteo, C.; Wright, F.V. The Motor Learning Strategy Instrument. Pediatr. Phys. Ther. 2013, 25, 53–60. [Google Scholar] [CrossRef] [PubMed]
- Samuel, G.S.; Choo, M.; Chan, W.Y.; Kok, S.; Ng, Y.-S. The use of virtual reality-based therapy to augment poststroke upper limb recovery. Singap. Med. J. 2015, 56, e127–e130. [Google Scholar] [CrossRef] [PubMed]
- Sharan, D.; Ajeesh, P.; Rameshkumar, R.; Mathankumar, M.; Paulina, R.J.; Manjula, M. Virtual reality based therapy for post operative rehabilitation of children with cerebral palsy. Work 2012, 41, 3612–3615. [Google Scholar] [CrossRef] [PubMed]
- Matijević, V.; Secić, A.; Mašić, V.; Sunić, M.; Kolak, Z.; Znika, M. Virtual reality in rehabilitation and therapy. Acta Clin. Croat. 2013, 52, 453–457. [Google Scholar] [PubMed]
- Katz, N. The Impact of Pain Management on Quality of Life. J. Pain Symptom Manag. 2002, 24, S38–S47. [Google Scholar] [CrossRef]
- Brennan, F.; Carr, D.B.; Cousins, M. Pain Management: A Fundamental Human Right. Anesth. Analg. 2007, 105, 205–221. [Google Scholar] [CrossRef]
- Gatchel, R.J.; McGeary, D.D.; McGeary, C.A.; Lippe, B. Interdisciplinary chronic pain management: Past, present, and future. Am. Psychol. 2014, 69, 119–130. [Google Scholar] [CrossRef]
- Huang, M.Y.; Scharf, S.; Chan, P.Y. Effects of immersive virtual reality therapy on intravenous patient-controlled sedation during orthopaedic surgery under regional anesthesia: A randomized controlled trial. PLoS ONE 2020, 15, e0229320. [Google Scholar] [CrossRef]
- Cimpean, A. Doctoral School Evidence-based assessment and psychological interventions A Pilot Study to Compare Cognitive Behavioral Therapy with Virtual Reality vs. Standard Cognitive Behavioral Therapy for Patients who Suffer from Cervical Cancer. J. Evid. Based Psychother. 2019, 19, 115–128. [Google Scholar] [CrossRef]
- Schmitt, Y.S.; Hoffman, H.G.; Blough, D.K.; Patterson, D.R.; Jensen, M.P.; Soltani, M.; Carrougher, G.J.; Nakamura, D.; Sharar, S.R. A randomized, controlled trial of immersive virtual reality analgesia, during physical therapy for pediatric burns. Burns 2011, 37, 61–68. [Google Scholar] [CrossRef] [PubMed]
- Garrett, B.; Taverner, T.; McDade, P.; Lalloo, C.; Jones, T. Virtual Reality as an Adjunct Home Therapy in Chronic Pain Management: An Exploratory Study. JMIR Med. Inform. 2017, 5, 17–28. [Google Scholar] [CrossRef] [PubMed]
- Hoffman, H.G.; Meyer, W.J.; Ramirez, M.; Roberts, L.; Seibel, E.J.; Atzori, B.; Sharar, S.R.; Patterson, D.R. Feasibility of Articulated Arm Mounted Oculus Rift Virtual Reality Goggles for Adjunctive Pain Control During Occupational Therapy in Pediatric Burn Patients. Cyberpsychol. Behav. Soc. Netw. 2014, 17, 397–401. [Google Scholar] [CrossRef] [PubMed]
- Faber, A.W.; Patterson, D.R.; Bremer, M. Repeated Use of Immersive Virtual Reality Therapy to Control Pain during Wound Dressing Changes in Pediatric and Adult Burn Patients. J. Burn Care Res. 2013, 34, 563–568. [Google Scholar] [CrossRef]
- Hoffman, H.G.; Patterson, D.R.; Soltani, M.; Teeley, A.; Miller, W.; Sharar, S.R. Virtual Reality Pain Control during Physical Therapy Range of Motion Exercises for a Patient with Multiple Blunt Force Trauma Injuries. Cyberpsychol. Behav. 2009, 12, 47–49. [Google Scholar] [CrossRef]
- Chirico, A.; Maiorano, P.; Indovina, P.; Milanese, C.; Giordano, G.G.; Alivernini, F.; Iodice, G.; Gallo, L.; De Pietro, G.; Lucidi, F.; et al. Virtual reality and music therapy as distraction interventions to alleviate anxiety and improve mood states in breast cancer patients during chemotherapy. J. Cell. Physiol. 2019, 235, 5353–5362. [Google Scholar] [CrossRef]
- Igna, R.; Stefan, S.; Onac, I.; Onac, I.; Ungur, R.-A.; Szentagotai-Tatar, A. Mindfulness-based cognitive-behavior therapy (mcbt) versus virtual reality (vr) enhanced cbt, versus treatment as usual for chronic back pain. a clinical trial. J. Evid. Based Psychother. 2014, 14, 229–247. [Google Scholar]
- Luo, H.; Cao, C.; Zhong, J.; Chen, J.; Cen, Y. Adjunctive virtual reality for procedural pain management of burn patients during dressing change or physical therapy: A systematic review and meta-analysis of randomized controlled trials. Wound Repair Regen. 2018, 27, 90–101. [Google Scholar] [CrossRef]
- Sharar, S.R.; Carrougher, G.J.; Nakamura, D.; Hoffman, H.G.; Blough, D.K.; Patterson, D.R. Factors Influencing the Efficacy of Virtual Reality Distraction Analgesia During Postburn Physical Therapy: Preliminary Results from 3 Ongoing Studies. Arch. Phys. Med. Rehabil. 2007, 88, S43–S49. [Google Scholar] [CrossRef]
- Ford, C.G.; Manegold, E.M.; Randall, C.L.; Aballay, A.M.; Duncan, C.L. Assessing the feasibility of implementing low-cost virtual reality therapy during routine burn care. Burns 2018, 44, 886–895. [Google Scholar] [CrossRef] [PubMed]
- Stamm, O.; Dahms, R.; Müller-Werdan, U. Virtual reality in pain therapy: A requirements analysis for older adults with chronic back pain. J. Neuroeng. Rehabil. 2020, 17, 129. [Google Scholar] [CrossRef] [PubMed]
- Morris, L.D.; A Grimmer-Somers, K.; Spottiswoode, B.; A Louw, Q. Virtual reality exposure therapy as treatment for pain catastrophizing in fibromyalgia patients: Proof-of-concept study (Study Protocol). BMC Musculoskelet. Disord. 2011, 12, 85. [Google Scholar] [CrossRef] [PubMed]
- Thurner, T.W.; Dyachenko, E.; Mironenko, A. Diffusion of new technologies in medical research: The case of virtual reality. Health Technol. 2020, 10, 1221–1227. [Google Scholar] [CrossRef]
- Huang, Y.; Huang, Q.; Ali, S.; Zhai, X.; Bi, X.; Liu, R. Rehabilitation using virtual reality technology: A bibliometric analysis, 1996–2015. Science 2016, 109, 1547–1559. [Google Scholar] [CrossRef]
- Hacmun, I.; Regev, D.; Salomon, R. The Principles of Art Therapy in Virtual Reality. Front. Psychol. 2018, 9, 2082. [Google Scholar] [CrossRef]
- Birckhead, B.; Khalil, C.; Liu, X.; Conovitz, S.; Rizzo, A.; Danovitch, I.; Bullock, K.; Spiegel, B. Recommendations for Methodology of Virtual Reality Clinical Trials in Health Care by an International Working Group: Iterative Study. JMIR Ment. Health 2019, 6, e11973. [Google Scholar] [CrossRef]
- Ökmen, B.M.; Aslan, M.D.; Çetin, F.Ç.; Yüzer, G.F.N.; Dönmez, B.K.; Özgirgin, N. Serebral Palsili Çocuklarda Sanal Gerçeklik Terapisinin Ruhsal Uyuma Etkisi. Arch. Neuropsychiatry 2013, 50, 70–74. [Google Scholar] [CrossRef]
- Department of Health. No Health without Mental Health: A Cross-Government Mental Health Outcomes Strategy for People of All Ages; The Stationery Office: London, UK, 2011; p. 5.
- Fava, G.A.; Sonino, N. Psychosomatic Medicine: Emerging Trends and Perspectives. Psychother. Psychosom. 2000, 69, 184–197. [Google Scholar] [CrossRef]
- Pereira, P.; Duarte, E.; Rebelo, F.; Noriega, P. A Review of Gamification for Health-Related Contexts. In Design, User Experience, and Usability. User Experience Design for Diverse Interaction Platforms and Environments; Marcus, A., Ed.; Springer International Publishing: Cham, Switzerland, 2014; pp. 742–753. [Google Scholar] [CrossRef]
- Menelas, B.-A.J.; Haidon, C.; Ecrepont, A.; Girard, B. Use of virtual reality technologies as an Action-Cue Exposure Therapy for truck drivers suffering from Post-Traumatic Stress Disorder. Entertain. Comput. 2018, 24, 1–9. [Google Scholar] [CrossRef]
- Lin, J.; Kelleher, C.L.; Engsberg, J.R. Developing Home-Based Virtual Reality Therapy Interventions. Games Health J. 2013, 2, 34–38. [Google Scholar] [CrossRef]
- Udara, S.; De Alwis, A. Gamification for Healthcare and Well-being. Glob. J. Med Res. 2019, 2019, 25–29. [Google Scholar] [CrossRef]
- Muangsrinoon, S.; Boonbrahm, P. Game elements from literature review of gamification in healthcare context. J. Technol. Sci. Educ. 2019, 9, 20–31. [Google Scholar] [CrossRef]
- Thomason, J. MetaHealth—How will the Metaverse Change Health Care? J. Metaverse 2021, 1, 13–14. Available online: https://dergipark.org.tr/en/pub/jmv/issue/67581/1051379 (accessed on 23 August 2021).
- Chen, D.; Zhang, R. Exploring Research Trends of Emerging Technologies in Health Metaverse: A Bibliometric Analysis. SSRN J. 2022. [Google Scholar] [CrossRef]
- Park, S.-M.; Kim, Y.-G. A Metaverse: Taxonomy, Components, Applications, and Open Challenges. IEEE Access 2022, 10, 4209–4251. [Google Scholar] [CrossRef]
- Sharma, A.; Bajpai, P.; Singh, S.; Khatter, K. Virtual Reality: Blessings and Risk Assessment. arXiv 2018, arXiv:170809540. [Google Scholar]
- Msc, S.M.N.G.; Levac, D. Barriers, Facilitators and Interventions to Support Virtual Reality Implementation in Rehabilitation: A Scoping Review. PMR 2018, 10, 1237–1251.e1. [Google Scholar] [CrossRef]
- Heydari Khajehpour, S.; Seyed Esfahani, M. The barriers of accepting Virtual Reality in Healthcare by older generation. In Proceedings of the International Society for Professional Innovation Management (ISPIM), Virtual, 10 June 2020. [Google Scholar]
- Tsekleves, E.; Cooper, R. Emerging Trends and the Way Forward in Design in Healthcare: An Expert’s Perspective. Des. J. 2017, 20, S2258–S2272. [Google Scholar] [CrossRef]
- Kellmeyer, P. Neurophilosophical and Ethical Aspects of Virtual Reality Therapy in Neurology and Psychiatry. Camb. Q. Health Ethic 2018, 27, 610–627. [Google Scholar] [CrossRef]
- Brinkman, W.-P.; Van Der Mast, C.; Sandino, G.; Gunawan, L.T.; Emmelkamp, P.M. The therapist user interface of a virtual reality exposure therapy system in the treatment of fear of flying. Interact. Comput. 2010, 22, 299–310. [Google Scholar] [CrossRef]
| Cluster | Author | Year | Research Method | Research Subject | Medical Condition | Therapy |
|---|---|---|---|---|---|---|
| 1 | Marco et al. | 2013 | Controlled study | Women | Eating disorders | Body image treatment using Virtual reality |
| Riva et al. | 2002 | Controlled study | Adult women | Eating disorders | Multidimensional virtual reality treatment | |
| Ferrer-garcia et al. | 2017 | Randomized Controlled Comparison | Adults | Eating disorders | Virtual reality cue exposure therapy | |
| 2 | Hoffman et al. | 2000 | Case study (self-report) | Adults | Burn pain | Virtual-reality-aided physical therapy |
| Schmitt et al. | 2011 | Randomized, controlled trial | Teenagers | Burn pain | Virtual-reality-aided physical therapy | |
| Hoffman et al. | 2014 | Case study | Teenagers | Burn pain | Occupational therapy with virtual reality | |
| 3 | Rizzo et al. | 2005 | SWOT analysis | Unclear | Rehabilitation | Unspecified |
| Bohil et al. | 2011 | Literature review | Unclear | Neuroscience related | Unspecified | |
| Lohse et al. | 2014 | Systematic review | Unclear | Post-stroke | Custom built virtual environments and commercially available gaming systems. | |
| 4 | Rothbaum et al. | 2001 | Open clinical trial | Vietnam combat veterans | Post-traumatic stress disorder | Virtual reality exposure therapy |
| Rothbaum et al. | 2014 | Controlled randomized clinical trial | Iraq and Afghanistan veterans | Post-traumatic stress disorder | Virtual reality exposure with drugs | |
| Difede et al. | 2007 | Controlled trial | Civilians and disaster workers | Post-traumatic stress disorder | Virtual reality exposure therapy | |
| 5 | Parsons et al. | 2008 | A meta-analysis | Unclear | Anxiety and specific phobias | Virtual reality exposure therapy |
| Powers et al. | 2008 | A meta-analysis | Unclear | Anxiety and specific phobias | Virtual reality exposure therapy | |
| Rothbaum et al. | 2006 | Controlled clinical trial | Unclear | Fear of flying | Virtual reality exposure therapy | |
| 6 | Opris et al. | 2012 | A meta-analysis | Unclear | Anxiety disorders | Virtual reality exposure therapy |
| Morina et al. | 2015 | Case study | College students | Anxiety disorders | Virtual reality exposure therapy | |
| Carl et al. | 2019 | A meta-analysis | Unclear | Anxiety disorders | Virtual reality exposure therapy | |
| 7 | Botella et al. | 2017 | Systematic review | Unclear | Phobias | Virtual reality exposure therapy |
| Freeman et al. | 2018 | Randomized trial | Adults | Fear of heights | Virtual reality cognitive intervention | |
| Lindner et al. | 2017 | Literature review | Unclear | Anxiety disorders | Virtual reality exposure therapy |
| Rank | Term | Occurrences |
|---|---|---|
| 1 | Virtual reality exposure therapy | 94 |
| 2 | Exposure therapy | 46 |
| 3 | Virtual reality therapy | 43 |
| 4 | Test | 41 |
| 5 | PTSD | 38 |
| 6 | Rehabilitation | 35 |
| 7 | Control group | 33 |
| 8 | Anxiety disorder | 31 |
| 9 | Post-traumatic stress disorder | 28 |
| 10 | Phobia | 28 |
| Medical Condition | Therapy | Method | Outcome |
|---|---|---|---|
| IRAP, combat, veteran, active duty soldier, anxiety symptom, cognitive function, post-traumatic stress, PTSD, PTSD symptom, stress disorder | Course, exposure therapy, imaginal exposure, post-treatment, pretreatment, prolonged exposure, virtual reality exposure (VRE) | Case report | Engagement, frequency, immersion, potential benefit, significant change |
| Medical Condition | Therapy | Method | Outcome |
|---|---|---|---|
| Avoidance, depressive symptom, distress, panic disorder, paranoia, phobia, public speaking anxiety, sad, social anxiety, social anxiety disorder, social phobia, social situation, specific phobia, spider | Post-treatment, pre-treatment, virtual reality cognitive, virtual reality exposure, vivo, vivo exposure, vivo exposure therapy, VR CBT, VR exposure, VR exposure therapy, VRET session | Control condition, heart rate, self-reporting | Availability, effect size, effective treatment, extent, low cost, relaxation, significant reduction, wide range |
| Medical Condition | Therapy | Method | Outcome |
|---|---|---|---|
| Adult, balance, cerebral palsy, child, children, gait, motor, motor function, motor rehabilitation, movement, stroke, upper limb | Conventional therapy, post intervention, VR therapy, VR group, VR intervention | Berg balance scale, control group, experimental group, Fugl Meyer assessment, randomized clinical trial, systematic review, meta-analysis, test | Duration, mobility, motivation, participation, performance, positive effect, significant improvement, significant result |
| Medical Condition | Therapy | Method | Outcome |
|---|---|---|---|
| Burn patient, chronic, female, pain | Attention, distraction, exercise, immersive virtual reality, physical therapy, VR session | Case study | Average, preliminary evidence, range, side effect |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, Z.; Ren, L.; Xiao, C.; Zhang, K.; Demian, P. Virtual Reality Aided Therapy towards Health 4.0: A Two-Decade Bibliometric Analysis. Int. J. Environ. Res. Public Health 2022, 19, 1525. https://doi.org/10.3390/ijerph19031525
Liu Z, Ren L, Xiao C, Zhang K, Demian P. Virtual Reality Aided Therapy towards Health 4.0: A Two-Decade Bibliometric Analysis. International Journal of Environmental Research and Public Health. 2022; 19(3):1525. https://doi.org/10.3390/ijerph19031525
Chicago/Turabian StyleLiu, Zhen, Lingfeng Ren, Chang Xiao, Ke Zhang, and Peter Demian. 2022. "Virtual Reality Aided Therapy towards Health 4.0: A Two-Decade Bibliometric Analysis" International Journal of Environmental Research and Public Health 19, no. 3: 1525. https://doi.org/10.3390/ijerph19031525
APA StyleLiu, Z., Ren, L., Xiao, C., Zhang, K., & Demian, P. (2022). Virtual Reality Aided Therapy towards Health 4.0: A Two-Decade Bibliometric Analysis. International Journal of Environmental Research and Public Health, 19(3), 1525. https://doi.org/10.3390/ijerph19031525







