Digital Implant Planning in Patients with Ectodermal Dysplasia: Clinical Report
Abstract
:1. Introduction
2. Case Report
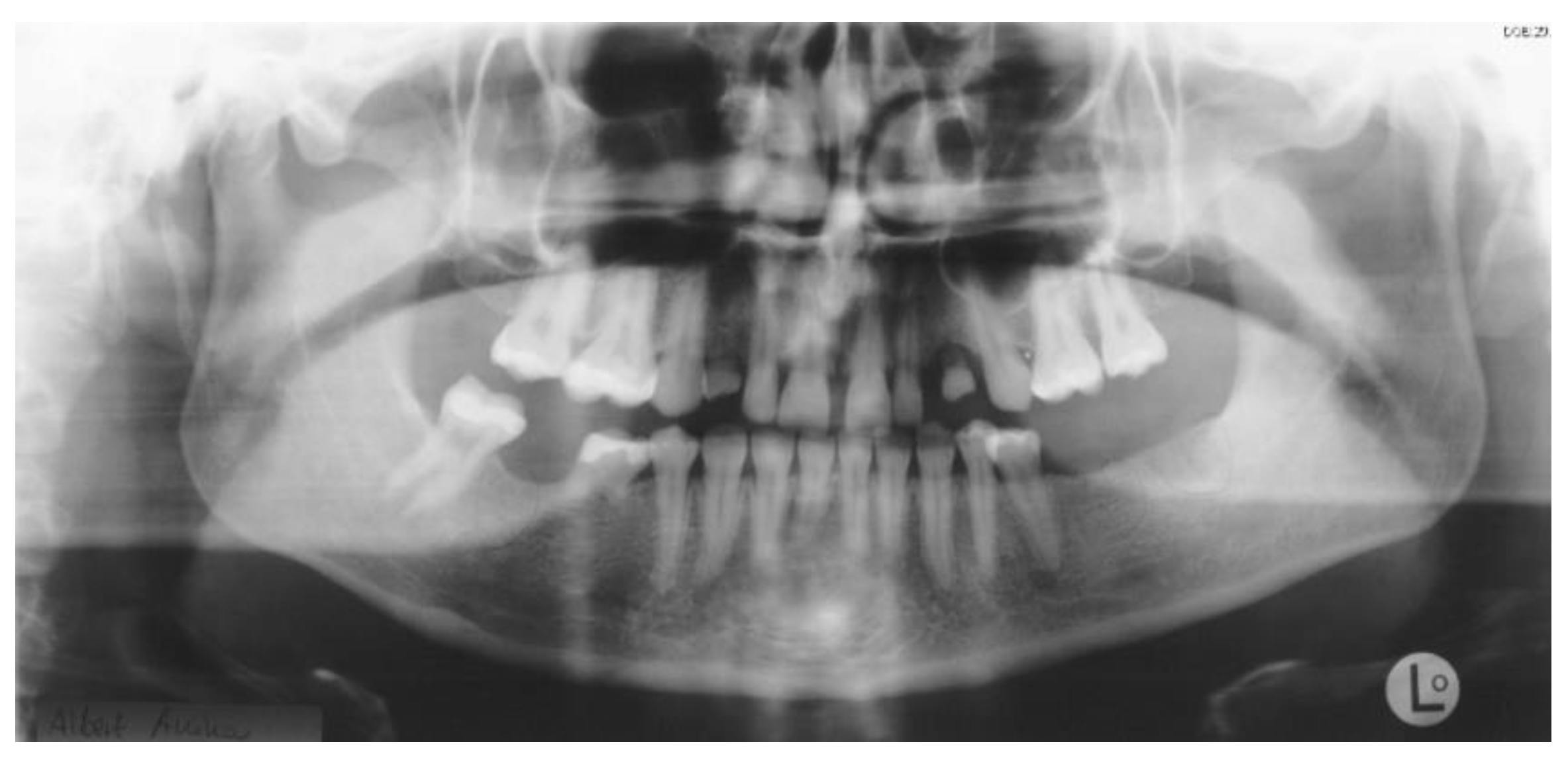
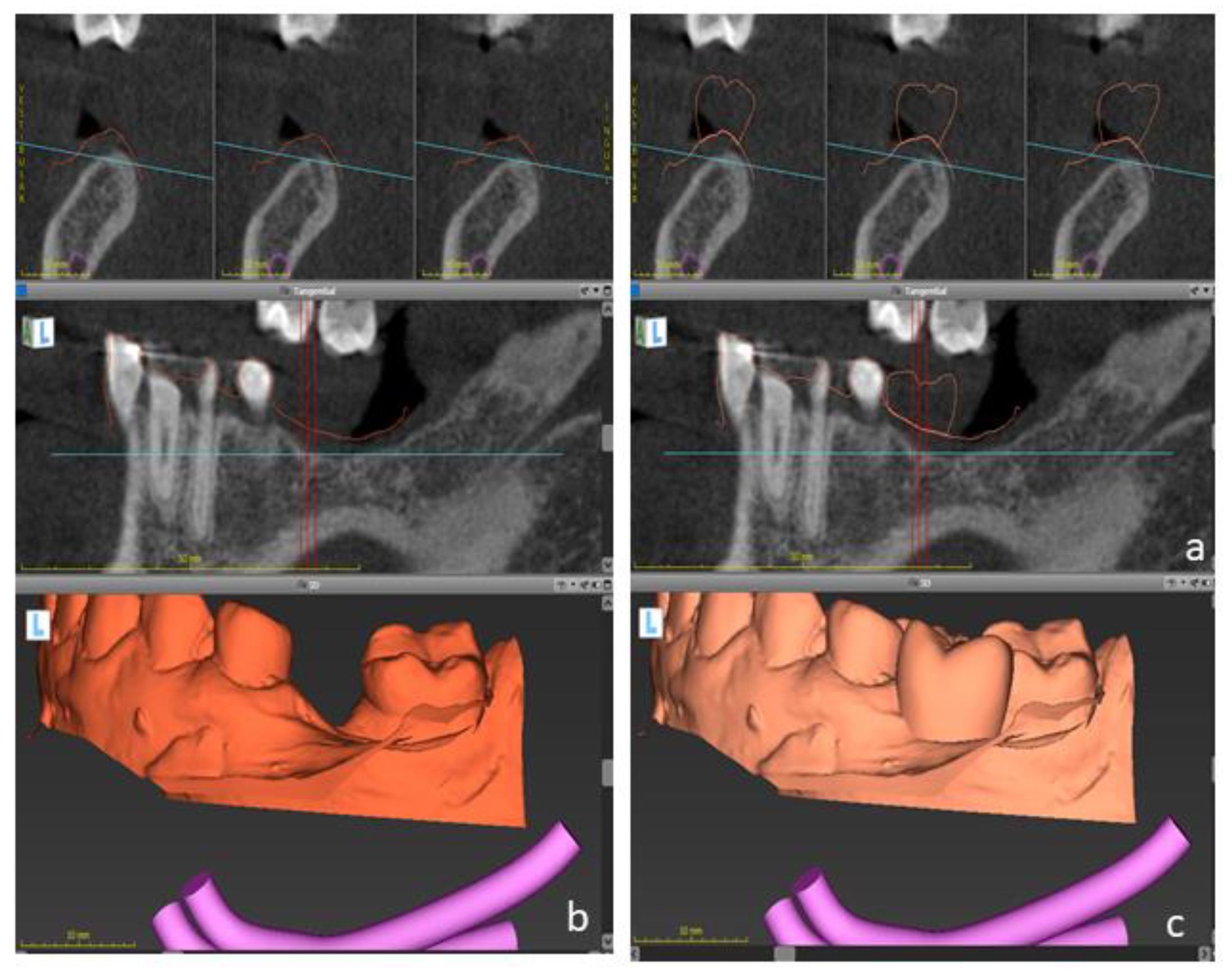
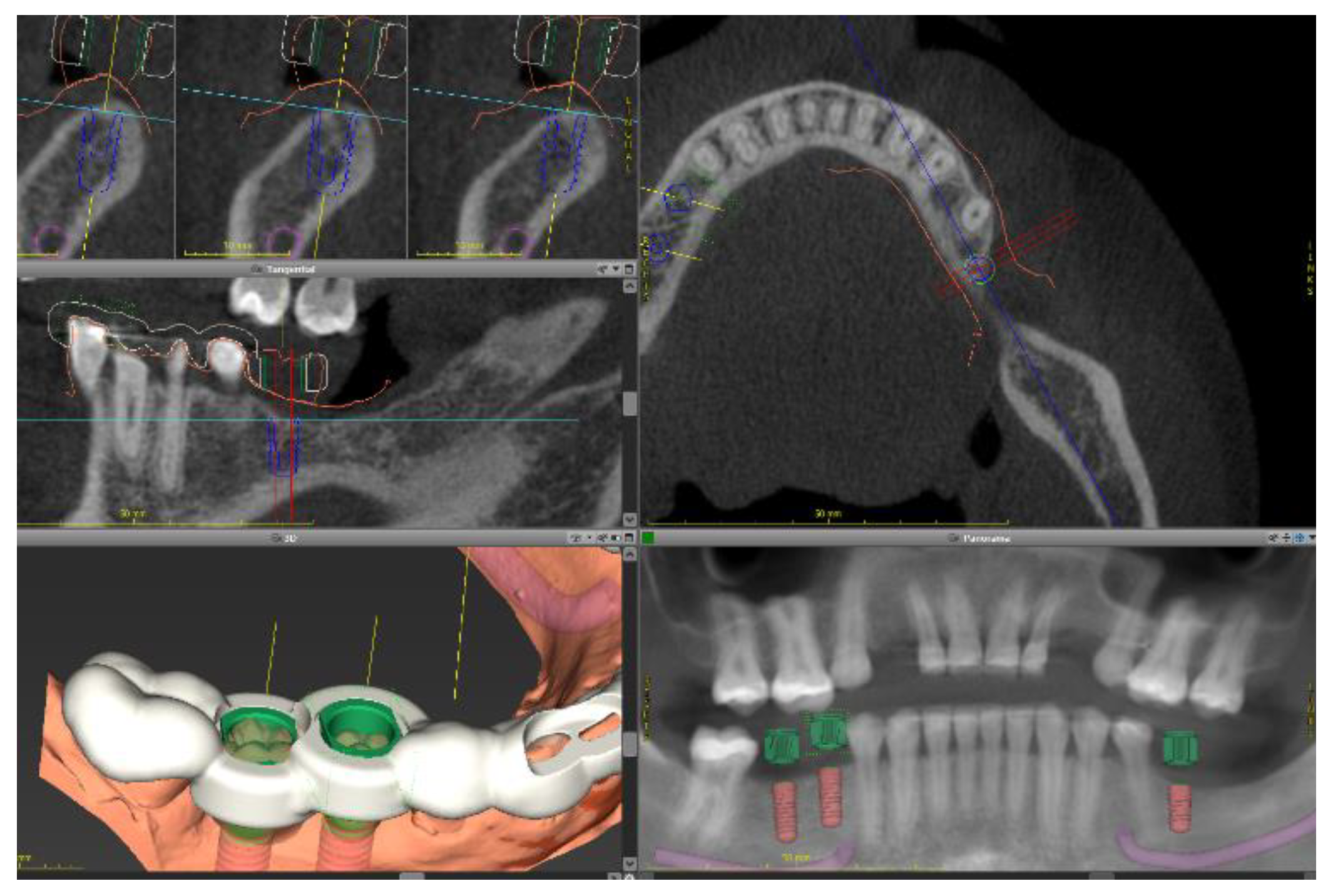
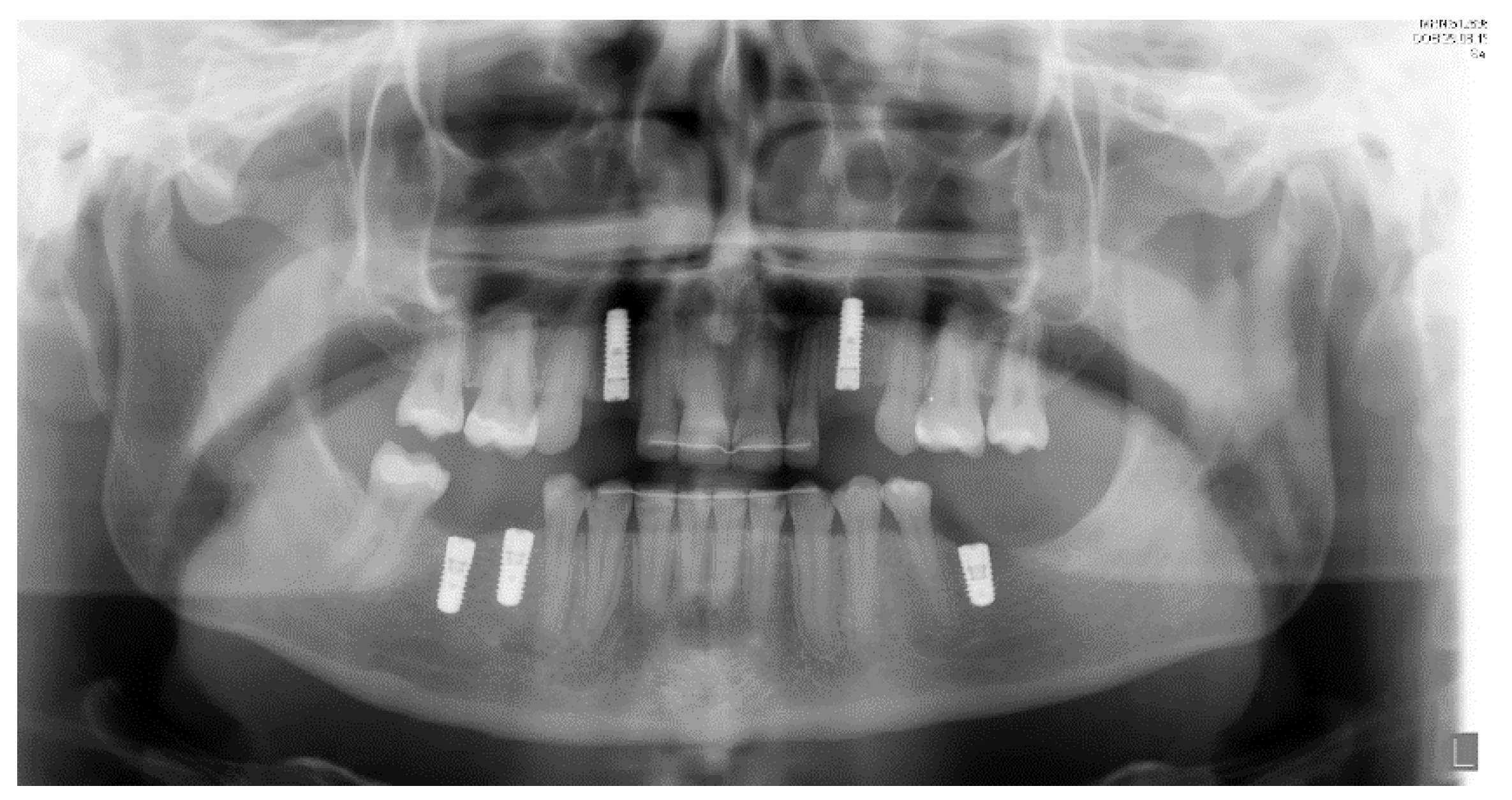
2.1. Case One
2.2. Case 2
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hanisch, M.; Sielker, S.; Jung, S.; Kleinheinz, J.; Bohner, L. Self-Assessment of Oral Health-Related Quality of Life in People with Ectodermal Dysplasia in Germany. Int. J. Environ. Res. Public Health 2019, 16, 1933. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, Y.; Tang, C. Interdisciplinary treatment with implant-supported prostheses for an adolescent with ectodermal dysplasia: A clinical report. J. Prosthet. Dent. 2019, 123, 655–660. [Google Scholar] [CrossRef] [PubMed]
- Alsayed, H.D.; Alqahtani, N.M.; Alzayer, Y.M.; Morton, D.; Levon, J.A.; Baba, N.Z. Prosthodontic rehabilitation with monolithic, multichromatic, CAD-CAM complete overdentures in an adolescent patient with ectodermal dysplasia: A clinical report. J. Prosthet. Dent. 2018, 119, 873–878. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, Y.L.; Razzoog, M.; Hammaker, S.G. Oral Care Program for Successful Long-Term Full Mouth Habilitation of Patients with Hypohidrotic Ectodermal Dysplasia. Case Rep. Dent. 2018, 2018, 4736495. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ioannidou-Marathiotou, I.; Kotsiomiti, E.; Gioka, C. The contribution of orthodontics to the prosthodontic treatment of ectodermal dysplasia: A long-term clinical report. J. Am. Dent. Assoc. 2010, 141, 1340–1345. [Google Scholar] [CrossRef] [PubMed]
- Schnabl, D.; Gerhard, S.; Biedermann, R.; Crismani, A.; Rasse, M.; Zauza, K.; Schmuth, M.; Kapferer-Seebacher, I. Dental Management and Prosthetic Rehabilitation of Patients Suffering from Hypohidrotic Ectodermal Dysplasia: A Report of Two Case Histories. Int. J. Prosthodont. 2018, 31, 552–557. [Google Scholar] [CrossRef] [PubMed]
- Schnabl, D.; Grunert, I.; Schmuth, M.; Kapferer-Seebacher, I. Prosthetic rehabilitation of patients with hypohidrotic ectodermal dysplasia: A systematic review. J. Oral Rehabil. 2018, 45, 555–570. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Terheyden, H.; Wüsthoff, F. Occlusal rehabilitation in patients with congenitally missing teeth—dental implants, conventional prosthetics, tooth autotransplants, and preservation of deciduous teeth—A systematic review. Int. J. Implant. Dent. 2015, 1, 1–25. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gonzaga, L.H.; Amorim, K.P.; Sesma, N.; Martin, W.C. Interdisciplinary rehabilitation of a patient with ectodermal dysplasia utilizing digital tools: A clinical report. J. Prosthet. Dent. 2021, S0022-3913, 30765-4. [Google Scholar] [CrossRef] [PubMed]
- Stanford, C.M.; Guckes, A.; Fete, M.; Srun, S.; Richter, M.K. Perceptions of outcomes of implant therapy in patients with ectodermal dysplasia syndromes. Int. J. Prosthodont. 2008, 21, 195–200. [Google Scholar] [PubMed]
- Liebermann, A.; Schweiger, J.; Edelhoff, D.; Schwerin, C. Innovative tooth-colored CAD/CAM polycarbonate splint design for prosthetic rehabilitation of a young ectodermal dysplasia patient with permanent tooth aplasia. Quintessence Int. 2021, 52, 694–704. [Google Scholar] [CrossRef] [PubMed]
- Hanisch, M.; Blanck-Lubarsch, M.; Kapitza, B.; Suwelack, D.; Kleinheinz, J. Interdisziplinäre kaufunktionelle Versorgung einer Patientin mit Bloch-Sulzberger-Syndrom. Implantologie 2019, 27, 295–302. [Google Scholar]
- Bohner, L.O.L.; Hanisch, M.; Kleinheinz, J.; Jung, S. Dental implants in growing patients: A systematic review. Br. J. Oral Maxillofac. Surg. 2019, 57, 397–406. [Google Scholar] [CrossRef] [PubMed]
- Bohner, L.; Wiemann, S.; Jung, S.; Kleinheinz, J.; Hanisch, M. Oral health-related quality of life in rare diseases associated with oral symptoms, diagnostic delay, and sex. Bundesgesundheitsblatt Gesund-Heitsforschung Gesundh. 2019, 62, 1406–1411. [Google Scholar] [CrossRef] [PubMed]
- Niekamp, N.; Kleinheinz, J.; Reissmann, D.R.; Bohner, L.; Hanisch, M. Subjective Oral Health-Related Quality of Life and Objective Oral Health in People with Ectodermal Dysplasia. Int. J. Environ. Res. Public Health 2020, 18, 143. [Google Scholar] [CrossRef] [PubMed]
- Hanisch, M.; Bohner, L.; Igelbrink, S.; Blanck-Lubarsch, M.; Suwelack, D.; Kleinheinz, J. Kaufunktionelle Versorgung und mundgesundheitsbezogene Lebensqualität bei ektodermalen Dysplasien. Quintessenz Implantol. 2021, 2, 203–212. [Google Scholar]







Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bohner, L.; Vinayahalingam, S.; Kleinheinz, J.; Hanisch, M. Digital Implant Planning in Patients with Ectodermal Dysplasia: Clinical Report. Int. J. Environ. Res. Public Health 2022, 19, 1489. https://doi.org/10.3390/ijerph19031489
Bohner L, Vinayahalingam S, Kleinheinz J, Hanisch M. Digital Implant Planning in Patients with Ectodermal Dysplasia: Clinical Report. International Journal of Environmental Research and Public Health. 2022; 19(3):1489. https://doi.org/10.3390/ijerph19031489
Chicago/Turabian StyleBohner, Lauren, Shankeeth Vinayahalingam, Johannes Kleinheinz, and Marcel Hanisch. 2022. "Digital Implant Planning in Patients with Ectodermal Dysplasia: Clinical Report" International Journal of Environmental Research and Public Health 19, no. 3: 1489. https://doi.org/10.3390/ijerph19031489
APA StyleBohner, L., Vinayahalingam, S., Kleinheinz, J., & Hanisch, M. (2022). Digital Implant Planning in Patients with Ectodermal Dysplasia: Clinical Report. International Journal of Environmental Research and Public Health, 19(3), 1489. https://doi.org/10.3390/ijerph19031489







